Abstract
Late congenital syphilis refers to the people with syphilis from the age of 2 to 30 years. We report a case of late congenital syphilis in a 9 year old girl with perforation of palate and saddle nose deformity. Kassowitz law was also observed (if a woman with untreated syphilis has series of pregnancies, the likelihood of infection of the fetus in later pregnancies becomes less). Venereal Disease Research Laboratory (VDRL) and Treponema pallidum hemagglutination (TPHA) were reactive. Computed tomography (CT) scan of paranasal sinus showed maxillary and nasal polyps. The case reported here is a rare presentation of late congenital syphilis with perforation of palate and saddle nose deformity.
Keywords: Late congenital syphilis, perforation of palate, kassowitz law
INTRODUCTION
Syphilis is an infectious disease. When present in an untreated pregnant woman, it may lead to series of miscarriage, preterm delivery, still birth, low birth weight and normal child, (known as Kassowitz law).[1] Congenital syphilis occurs in babies due to vertical transmission. It is divided into three categories: (1) early, (2) late, and (3) stigmata. Here, we report a case of late congenital syphilis presenting as palatal perforation and saddle nose deformity, also fulfilling the Kassowitz law.
CASE REPORT
A 9 year-old girl, born as the fourth child to non-consanguineous parents, was reported to our department with perforation of palate for routine Venereal Disease Research Laboratory (VDRL) screening from the ENT department. The patient had history of regurgitation of food and change of voice for the past 6 months. There was no history of trauma, loss of weight, skin lesions or fever. Also, there was no history suggestive of sexual abuse. Physical examination revealed saddle nose deformity [Figure 1] and perforation of hard palate [Figure 2]. The size of perforation was 5-mm in diameter and the edges were regular. Ophthalmic and central nervous system examination were normal. VDRL was reactive in 1:8 dilutions and was later confirmed with Treponema pallidum hemagglutination (TPHA).
Figure 1.

Patient with saddle nose deformity
Figure 2.

Intra-oral photograph of the patient showing perforation of palate
Her parents and siblings (one elder and two younger) were screened for syphilis. Parents were VDRL reactive in 1:4 dilutions, elder sibling (female, 11 years old) was VDRL reactive in 1:8 dilutions and all were confirmed with TPHA. The two younger siblings were VDRL non-reactive. Patient's father gave a history of unprotected, premarital sexual contact, with an unknown female, 14 years back. Three weeks later he developed a genital ulcer for which he was treated and the ulcer healed without any scar. Patient's mother had six deliveries. Her first male baby was delivered 12 years back which died on the same day because of seizures. The second female baby was delivered 2 years later which also died on the 10 th day due to low birth weight. Her third female child (11 years old) is the elder sibling of the patient, who had non-development of upper central incisors [Figure 3]. Her fourth child was the patient. Fifth and sixth children were clinically and serologically normal [Figure 4]. All were home deliveries without any antenatal care.
Figure 3.

Elder sibling of the patient showing absent upper central incisors
Figure 4.
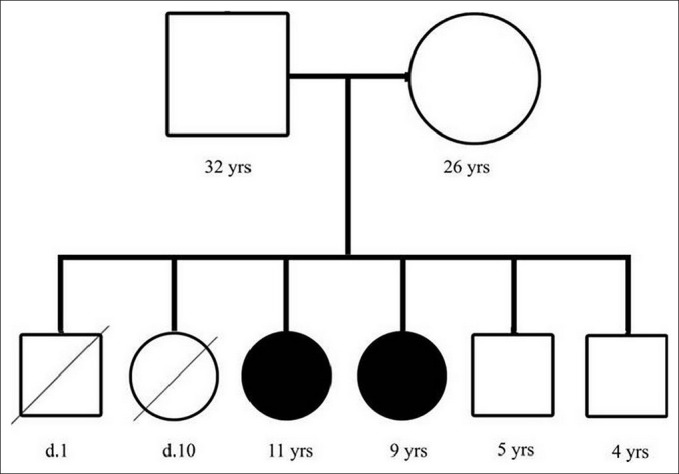
Pedigree chart showing the deceased children at day 1 and day 10 respectively, elder sibling, patient and normal children
Routine blood investigations, cerebrospinal fluid (CSF) analysis, Mantoux test, chest X-ray, X-ray skull and long bones were normal for the patient. Computed tomography (CT) scan of paranasal sinus (PNS) showed perforation of palate [Figure 5] with bilateral maxillary and nasal polyps [Figure 6]. Her parents refused for biopsy of polyps. From the above history, clinical examination and investigations, diagnosis of late congenital syphilis with stigmata was made. The patient was treated with injection benzathaine penicillin 50,000 international units/kg body weight, deep intramuscular, once weekly, for 3 weeks, after test dose. The elder sibling and parents were also treated with injection benzathaine penicillin 24 lakh international units, once weekly, for 3 weeks. They were advised to come for regular follow-up.
Figure 5.
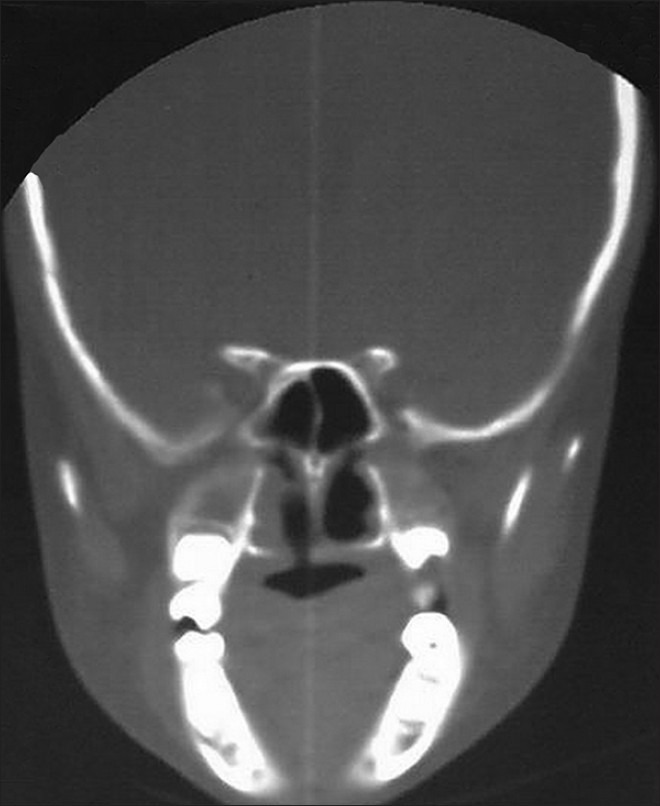
CT PNS showing the perforation of right side of hard palate
Figure 6.

CT PNS showing the bilateral maxillary and nasal polyps
DISCUSSION
In India, the incidence of congenital syphilis is reported to vary from 0.18 to 1.4%.[2,3] Only 30% are symptomatic among the infected cases.[4] Congenital syphilis is classified into early, late and stigmata types. Early congenital syphilis refers to individuals with syphilis from the first 2 years of life. The lesions of early congenital syphilis are infectious and it could be compared to the secondary stage of acquired syphilis. Common manifestations are skin rashes, mucous patches, lymphadenitis and hepato- splenomegaly. Late congenital syphilis refers to the individuals with syphilis from the age of 2 to 30 years. In most of the cases, it is asymptomatic and the diagnosis is made from the serological tests.[5] Clinical features may present as interstitial keratitis, eighth nerve deafness or clutton's joints. Stigmata are scars or deformities resulting from either early or late lesions. Stigmata resulting from early congenital syphilis are saddle nose deformity, Hutchinson's teeth, rhagades, choroid scarring and onychia. Stigmata due to late congenital syphilis are perforation of palate, corneal opacities, optic atrophy and periosteal changes of tibia.[6]
The transmission of infection to the fetus can occur at any time, but in most of the cases it occurs in utero. Once the infection enters the fetal circulation, dissemination occurs to all the tissues and elicits an inflammatory response of lymphocytes and plasma cells. The fetus may be overwhelmed by the infection and may die. If the infection is not severe, it may interfere with normal development at various stages of intra- uterine and extra- uterine life. Certain manifestations like interstitial keratitis and clutton's joints are due to hypersensitivity and not because of the direct effects of the organism. In our patient the perforation of palate was due to chronic necrosis by the localized gumma.[7] Also, the edges of palatal perforation were regular which rules out the traumatic cause. The saddle nose deformity was due to the failure of development of nasal bones. In the elder sibling the infection had affected the development of middle and lateral denticles, resulting in absence of upper central incisors.[8] Out of series of six deliveries, the patient's mother had perinatal death, neonatal death, two affected children, followed by two normal children. The above description clearly proves the Kassowitz law. Congenital syphilis could be treated either by penicillin or erythromycin, but the drug of choice is penicillin for which resistance has not been confirmed.[9]
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Purohit DM, Johnston M. Congenital syphilis. [Last updated on 2010 Sep 02, Last accessed on 2012 Mar 19]. Available from: http://www.medlink.com/medlinkcontent.asp .
- 2.Garg BR, et al. Sexually transmitted diseases in children. Indian J Sex Transm Dis. 1986;7:11–13. [Google Scholar]
- 3.Mendiratta V, et al. Congenital syphilis: A clinical profile. Indian J Sex Transm Dis. 1996;17:51–53. [Google Scholar]
- 4.Grossman KL, Rasmussen JE. Recent advances in pediatric infectious disease and their impact on dermatology. Am Acad Dermatol. 1991;24:379–389. doi: 10.1016/0190-9622(91)70057-9. [DOI] [PubMed] [Google Scholar]
- 5.Siddappa K, Ravindra K. Syphilis and nonvenereal treponematoses. In: Valia RG, Valia AR, editors. IADVL Text book and Atlas of Dermatology. Mumbai: Balani Publishing House; 2001. pp. 1390–1422. [Google Scholar]
- 6.Modi M, Sharma A, Marfatia YS, Naik E, Toney J. Late congenital syphilis with stigmata. Indian J Sex Transm Dis. 2008;29:32–33. [Google Scholar]
- 7.Bain MK, Hosseini-Ardehali M. Palatal perforations: Past and present. Two case reports and a literature review. [Last updated on September 10, 2005, Last accessed on 2012 March 24]. Available from: www.nature.com/bdj/journal/v199/n5/full/4812650a.html . [DOI] [PubMed]
- 8.King A, Nicol C, Rodin P. Venereal diseases. 4th ed. London: ELBS; 1980. Congenital syphilis; pp. 104–132. [Google Scholar]
- 9.Stamm LV, Stapleton JT, Bassford PJ., Jr In vitro assay to demonstrate high level erythromycin resistance of a clinical isolate of Treponema Pallidum. Antimicrob Agents Chemother. 1988;32:164–9. doi: 10.1128/aac.32.2.164. [DOI] [PMC free article] [PubMed] [Google Scholar]


