Abstract
Background:
Heterosexual transmission of HIV among married couples is the commonest mode of transmission seen in India. Intramarital transmission is associated with several challenges which need to be further researched.
Aim:
To study level of seroconcordance and serodiscordance among HIV positive couples and factors affecting intramarital sexual transmission in terms of safe sexual practice, and the presence of Sexually transmitted infections (STI)/circumcision.
Materials and Methods:
Ninety-one monogamous married cohabiting HIV-positive cases (index cases) attending Department of Skin and Venereology, Medical College Baroda, from January 2009 to August 2009 were studied. Their spouses were tested for HIV. A structured proforma was used to study various factors like condom use, circumcision, and the presence of sexually transmitted infections.
Results:
Ninety-one monogamous married cohabiting HIV-positive cases were included in the study and considered as index cases. There were 51 males and 40 females. On testing their spouses for HIV, both the spouses were positive in 55 couples giving rise to 60% seroconcordance rate. Out of 55 seroconcordant couples, male spouses used condom in 16 cases (29%). Out of 36 serodiscordant couples 17 male spouses (47%) used condom. Evidence of STD was observed in one of the spouses in 6 out of 55 seroconcordant couples and 6 out of 36 serodiscordant couples. Thus, out of 91 couples one of the partners was having STI in 12 couples. Overall rate of circumcision was 12.2%.
Conclusion:
The prevention of transmission of HIV to the HIV negative partner is of paramount importance. Serodiscordant couples, specially the HIV negative female partner is at higher risk. Less acceptability of condoms among married couples may be one of the factors responsible in transmission. Further studies are needed to explore other risk factors associated with HIV transmission in discordant couples.
Keywords: Circumcision, condom, HIV/AIDS, seroconcordant-discordant, STD
INTRODUCTION
In India, 2.39 million people are HIV infected of whom 87.4% are those who have acquired the infection through heterosexual transmission. Data from National AIDS Control Organization (NACO) suggest feminization of the HIV epidemic in India with 39% of cases in females; 83% of them belong to 15 to 49 years age group. More than 90% of HIV positive women are married and largely monogamous suggesting transmission within marriage as the commonest scenario. This can be influenced by factors such as condom use, the presence of sexually transmitted diseases, circumcision, etc. Understanding these factors will provide direction for future research.[1] Of these factors, STIs have significantly increased risk of HIV transmission among couples. Early diagnosis and treatment of STIs may significantly reduce the risk of HIV transmission.
Though lot is known about HIV, there are certain aspects which are yet to be understood. The factors responsible for serodiscordance (i.e., HIV positivity in only one partner) and non-transmission of HIV are poorly studied and need to be clearly established. Serodiscordance may also be explained in couples by the HIV negative individual's genetic makeup. Genetic variation in Chemokine Co-receptor 5(CCR5) co-receptor results in less effective HIV transmission. Sexual practices followed by the couple also influences sexual transmission. HIV negative individuals in discordant partnerships are at a high risk of infections and preventive interventions targeted at such individuals is the need of the hour.
OBJECTIVES
To determine seroconcordance and serodiscordance among HIV positive couples,
To study factors affecting intramarital sexual transmission in terms of condom use and the presence of STI/circumcision.
MATERIALS AND METHODS
This is an observational cross-sectional study design. The study protocol was approved by Institutional Review Boards, University of South Florida, Tampa, USA. Ninety-one consecutive couples, wherein one of the partners was diagnosed as HIV positive attending Skin and Venereal Diseases (VD) Department of Medical College Vadodara from January 2009 to August 2009 were enrolled. The partner reporting first was considered as the index case. The HIV status was confirmed by two ELISA tests. The cases were Anti-Retroviral Therapy (ART) naïve at the time of enrollment. The mode of acquisition of HIV infection was ascertained from the history. The partner was counseled for examination and assessment of HIV status. Various factors like condom use, mode of transmission. STI and circumcision were studied and their possible influence on spousal transmission was assessed. The details of marital life were enquired into.
Data management and analysis
The data were collected on pre-tested questionnaires and later entered into a Microsoft excel spreadsheet. No identifying information was recorded on either hardcopy or the excel spreadsheet. Researchers had access to only excel spreadsheet which had no identifying information. Data were analyzed using SAS software. Initially, frequencies of the variables were assessed and later cross tabulations against gender were performed. Finally, factors affecting spousal transmission were analyzed. Power calculations were done instead of sample size due to limited number of discordant couples available. The power of 80% with alpha error of 5% was considered as minimum requirements.
RESULTS
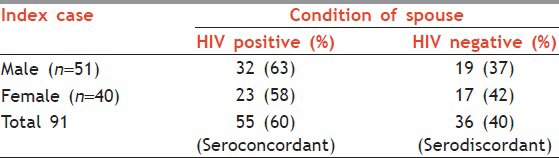
Ninety-one monogamous married cohabiting HIV-positive cases were included in the study and considered as index cases. There were 51 males and 40 females. On testing their spouses for HIV, both the spouses were positive in 55 couples giving rise to 60% seroconcordance rate. In the remaining 36 couples, one of the spouses was negative, and hence serodiscordance rate was 40% [Table 1].
Table 1.
Serostatus of spouse of index cases
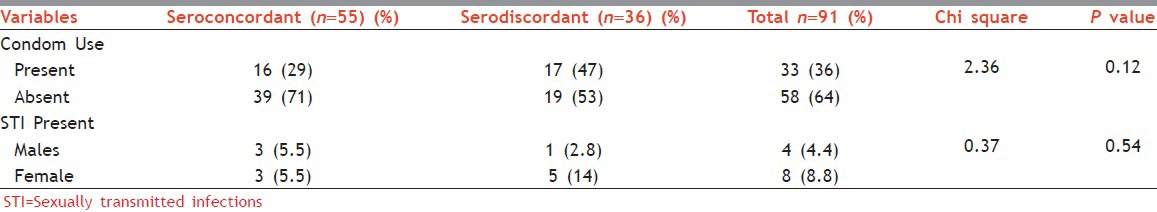
Out of 55 seroconcordant couples, male spouses used condom in 16 cases (29%). Out of 36 serodiscordant couples, 17 (47%) male spouses used condom. Evidence of STD in one of the spouses was observed in 6 couples out of 55 seroconcordant couples and 6 out of 36 serodiscordant couples. Thus, out of 91 couples, one of the partners having STI was seen among 12 couples. The difference in the condom usage and the presence of STI among seroconcordant and serodiscordant couples was not statistically significant [Table 2].
Table 2.
Variables associated with serostatus-condom use and presence of STIs
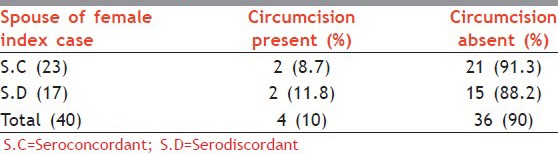
In present study, 11 (12.2%) out of 91 male spouses were circumcised. The statistical significance could not be calculated because of the small number of cases circumcised [Tables 3a and b].
Table 3a.
Variables associated with serostatus-circumcision in HIV positive males (index cases)
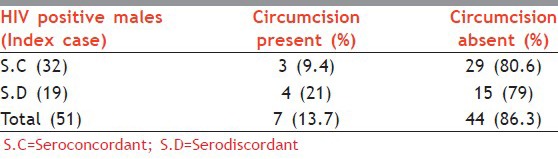
Table 3b.
Variables associated with serostatus circumcision in spouses of female index cases
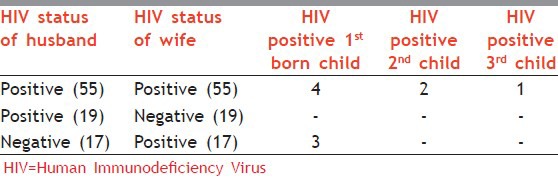
Out of 91 couples, 72 couples were with the wife being HIV positive, and therefore had potential for vertical transmission. Children of only 45 couples could be tested and 10 were positive. [Table 4]
Table 4.
HIV status of children
DISCUSSION
Heterosexual transmission is responsible for 87.4% of all HIV-1 transmissions in India.[1] The risk of HIV transmission between HIV serodiscordant married couples is highly variable and reflects the interplay between biological, genetic, immunological factors along with the various sociobehavioral factors.
Sixty percent seroconcordance may be due to late testing in index case and non-adaptation of safe sex practices [Table 1].
Forty-seven percent of serodiscordant couples in this study used condoms which were high compared to the national data of 6% (as per National Family Health Survey [NFHS-III]).[2] Whereas, only 29% of seroconcordant couples in this study use condoms which were lower than the national rate of 71% in seroconcordant couples [Table 2]. In a study conducted in South India, of 839 concordant and 996 discordant couples, discordants were more likely to use condoms with their spouses than concordant patients (49% vs. 28.8%; P = 0.01).[3] Another community-based study using a couple-based analysis to investigate the factors associated with men's use of condoms showed that concerns, such as, the importance of bearing children in a marriage, competed with protective behaviors, and undermined the use of condoms. Condom use was viewed only as a way to space births or to avoid illicit sexual activities, not as a health promotion measure.[4]
In a study in Rwanda, only 16.9% seroconcordant married co-habiting couples reported regular use of condoms; and most of the reasons reported for not using condoms related to alcohol intoxication, social and cultural beliefs as well as gender inequality. The authors pointed out that individuals infected with HIV often think that they do not have to protect themselves against re-infection/super-infection with HIV.[5]
More studies are required to study these factors responsible for low condom usage in marital sex in order to devise appropriate interventions to make use of condom as an effective preventive strategy in Indian context.
The concordant couples not using condoms can lead to certain issues like continuous exposure to fresh quantum of virus to one another including resistant/mutant strains; increased likelihood of transmitting STI; and potential of vertical transmission. While among discordant couples, non-usage of condoms poses higher chances of transmission to seronegative partner.
The evidence is strong and consistent that STIs increase chances of HIV transmission and acquisition. Overall, 12 individuals had evidence of STIs [Table 2].
Multiple studies have indicated at least a two-fold to five-fold increased risk for HIV infection among persons who have STIs, including genital ulcer diseases and non-ulcerative, inflammatory STIs. A retrospective cohort study of clients with repeat HIV tests attending a New Orleans STI clinic showed that recent syphilis or gonococci diagnosis was associated with significantly increased hazards of seroconversion (among men: Hazard ratio [HR], 4.2 [2.4-7.2]; among women: 5.0 (1.9-13.0)).[6]
A nested case-control study of 431 initially HIV-1-negative women followed prospectively for a mean duration of 2 years showed that adjusted odds ratio for seroconversion were 4.8 for gonorrhea, 3.6 for chlamydial infection, and 1.9 for trichomoniasis.[7] Because of their high prevalence and asymptomatic nature, non-ulcerative STDs may represent a considerable population-attributable risk in the transmission of HIV-1. The identification of treatable STI as risk factors for HIV-1 transmission offers an important additional strategy for the prevention of HIV/AIDS.
Overall, 11 (12.2%) males were circumcised in the present study which is very low compared to the global rate of 30% [Table 3].
A systematic review and meta-analysis by Weiss HA et al. that focused on male circumcision and heterosexual transmission of HIV in Africa showed a substantial protective effect of male circumcision on the risk for HIV infection, along with a reduced risk for genital ulcer disease.[8] After adjustment for confounding factors in the population-based studies, the relative risk for HIV infection was 44% lower in circumcised men.
Out of 91 couples in the present study, children of only 45 couples were tested, of which 10 were HIV positive. Seropositive couples try to conceive even after knowing their status because of the stigmata associated with not having children. Problems faced by HIV positive female with a discordant partner is even greater, she has to take care of herself as well as the positive child along with bearing the stigmata.
Adejuyigbe and Odebiyi in Nigeria studied on implications of parental serodiscordance on care of seropositive HIV child. The study included 51 couples of whom 27 were seroconcordant and 24 were serodiscordant (with female/mother being HIV positive). It was found that factors like discharge against medical advice, abandonment, loss to follow-up, care by the mothers alone, not being up-to-date with the immunization schedule and mortality among the children and their mothers was higher among seropositive children of serodiscordant couples when compared with children of seroconcordant parents (P < 0.05). Paternal reasons for not providing adequate care for the children from serodiscordant parents included fear of being infected, doubt of child's paternity, and waste of family resources on a ‘child who is dying’.[9]
CONCLUSION
The prevention of transmission of HIV in serodiscordant couples especially in HIV negative female partner is crucial. Adaptation of permanent methods of sterilization and less acceptability of condoms among married couples, which are seen as mere contraceptive measures and not the modes of preventing sexually transmitted diseases, may be one of the factors responsible in transmission. The protective value of circumcision is not promoted in HIV/STI prevention campaigns. The identification of treatable STIs as risk factors for HIV-1 transmission offers an important additional strategy for the prevention of HIV/AIDS.
Further studies are needed to explore other risk factors like genetic makeup, associated with HIV transmission in discordant couples. There is a testing gap as far as children of seropositive mothers are concerned.
There is indeed evidence that despite repeated exposure certain individuals appear to be protected from established infection with HIV-1 and they have been termed ‘highly exposed persistently seronegative’ (HEPS). Further studies are needed to explore risk factors like genetic makeup, viral load, innate immunity, sexual practices, and duration of exposure within intra-marital relationship, associated with HIV transmission in discordant couples.[10,11]
ACKNOWLEDGMENTS
The authors would like to thank Fogarty International Center, AIDS International Training and Research program faculty for their valuable technical support. We would also like to thank Dr. Patricia Emmanuel and Sadaf Aslam for their valuable comments and suggestions. “The project described was supported by Award Number D43TW006793 from the Fogarty International Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Fogarty International Center or the National Institutes of Health.”
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Annual report 2010-11. Department of AIDS Control. National AIDS Control Organization., Ministry of Health & Family Welfare. Government of India. [Last accessed on 2010 Nov 20]. Available from http://www.nacoonline.org/upload/REPORTS/NACO%20Annual%20Report%202010-11.pdf .
- 2.HIV Transmission in Intimate Partner Relationships in Asia. Joint United Nations Programme on HIV/AIDS (UNAIDS) 2009. [Last cited on 2010 Nov 20]. Available from: http://data.unaids.org/pub/report/2009/intimate_partners_report_en.pdf .
- 3.Kumarasamy N, Venkatesh KK, Srikrishnan AK, Prasad L, Balakrishnan P, Murugavel KG, et al. Couples at risk for HIV infection in Southern India: Characteristics of HIV-infected patients in concordant and discordant heterosexual relationships. Int J STD AIDS. 2010;21:96–100. doi: 10.1258/ijsa.2008.008418. [DOI] [PubMed] [Google Scholar]
- 4.Bhattacharya G. Promoting condom use among heterosexual married couples in India: Challenges for HIV prevention programs. Poster exhibition: The XIV international AIDS conference: Abstract no. MoPeF3917. [Last cited on 2010 Oct 12]. Available from: http://www.iasociety.org/Abstracts/A1438.aspx .
- 5.Umutesi G. Condom use among HIV seroconcordant positive couples: AIDS 2008-XVII International AIDS Conference: Abstract no. CDC0340. Available from: http://www.iasociety.org/Abstracts/A200719697.aspx .
- 6.Hanson J, Posner S, Hassig S, Rice J, Farley TA. Assessment of sexually transmitted diseases as risk factors for HIV seroconversion in a new Orleans sexually transmitted disease clinic, 1990-1998. [Last cited on 2010 Oct 10];Ann Epidemiol. 2005 15:13–20. doi: 10.1016/j.annepidem.2004.05.001. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15571989 . [DOI] [PubMed] [Google Scholar]
- 7.Laga M, Manoka A, Kivuvu M, Malele B, Tuliza M, Nzila N, et al. Non-ulcerative sexually transmitted diseases as risk factors for HIV-1 transmission in women: Results from a cohort study. AIDS. 1993;7:95–102. doi: 10.1097/00002030-199301000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Weiss HA, Quigley MA, Hayes RJ. Male circumcision and risk of HIV infection in sub-Saharan Africa: A systematic review and meta analysis. AIDS. 2000;14:2361–70. doi: 10.1097/00002030-200010200-00018. [DOI] [PubMed] [Google Scholar]
- 9.Adejuyigbe EA, Odebiyi AI. Parental HIV serodiscordance: Implications for the care of the HIV seropositive child in a resource-poor setting. AIDS Care. 2006;18:537–43. doi: 10.1080/13548500500228698. [DOI] [PubMed] [Google Scholar]
- 10.Kulkarni PS, Butera ST, Duerr AC. Resistance to HIV-1 infection: Lessons learned from studies of highly exposed persistently seronegative (HEPS) individuals. AIDS Rev. 2003;5:87–103. [PubMed] [Google Scholar]
- 11.Rowland-Jones S, Sutton J, Ariyoshi K, Dong T, Gotch F, McAdam S, et al. HIV-specific cytotoxic T-cells in HIV-exposed but uninfected Gambian women. Nat Med. 1995;1:59–64. doi: 10.1038/nm0195-59. [DOI] [PubMed] [Google Scholar]


