Abstract
Background and objective
The promotion of therapeutic adherence is considered as an integral component of pharmaceutical care practice and patient healthcare. It has been shown that despite effective methods of treatment, 50% of diabetic patients fail to achieve satisfactory glycemic control, which leads to accelerated development of complications and increased mortality. Clinical experience indicates that no improvement of metabolic control is possible without patients’ adherence to medications. This study sought to examine the rate of medication adherence and different factors affecting it among Type 2 diabetic patients in Egypt.
Methods
A total of 226 Type 2 diabetic patients who fulfilled the inclusion criteria were recruited in the current study. Adherence to the treatment was evaluated during patients’ hospitalization in the Outpatient Clinics of Internal Medicine Department at University of Mansoura, Egypt. The medication adherence has been assessed during a personal interview with each patient using a multiple-choice graded questionnaire.
Results
In the study population, the adherence rates to medication, dietary/exercise and appointment were observed to be suboptimal. The most important social factors that were significantly affecting adherence rate to the prescribed oral hypoglycemic agent(s) included marital status (P < 0.01), family support (P < 0.01), and socio-economical level (P < 0.01). Other patient factors that were significantly affecting therapeutic adherence were patient knowledge about the disease (P < 0.01), patients’ beliefs and motivation about prescribed drugs (P < 0.01), and regularity of patients’ self monitoring of blood glucose level (P < 0.01). Among drug factors which found to affect significantly the rate of medication adherence are the number of drugs taken (P < 0.05), complexity of drug regimen (P < 0.01), and the presence of drug side effects (P < 0.01). Economical factor played an equally important role. Direct and indirect care costs in relation to patients’ income were significantly affecting the rate of adherence to medication (P < 0.01).
Conclusions
An improvement with the adherence to oral hypoglycemic agent(s) may be achieved through continuing patient education about diabetes, improvement of patients’ economical levels as well as a reduction in the cost of medication. Pharmaceutical companies have to be involved and pharmacists have to be payed for helping chronically ill patients to take their medicines correctly for improving clinical outcomes.
Keywords: Therapeutic adherence, Drug compliance, T2DM, Oral hypoglycemic agents, Pharmaceutical care
1. Introduction
Diabetes mellitus (DM) is one of the most common noncommunicable diseases, and its epidemic proportion has placed it at the forefront of public health challenges currently facing the world (WHO, 2003). In the Eastern Mediterranean Region, there has been a rapid increase in the incidence of DM, consisting mainly of Type 2 (T2DM). Much of this increase occurs in developing countries and results from population ageing, unhealthy diet, obesity and a sedentary lifestyle. It is now the fourth leading cause of death in this region (Diabetes atlas, 2003). Despite of the advances in understanding of the disease and its management, the morbidity and mortality rate are in rise (Paulose, 2000; Rickles et al., 2010). Non-adherence or non-compliance, poverty, lack of knowledge and poor follow ups are the main factors observed in poor glycemic control (Kalyango et al., 2008). Individuals with poor management of diabetes are at a greater risk of developing long-term micro- and macro-vascular complications that lead to the damage of end organs such as kidney, heart, brain and eyes, affects the direct and indirect health care costs and overall quality of life (Maddigan et al., 2005). Optimal glucose control can be achieved through strict adherence to medications, diet, and life style modifications that in turn minimizes long-term complications (Schectman-Joel et al., 2002; Rickles et al., 2010).
Around a quarter of patients do not take their medicines as prescribed. The promotion of medication adherence is an important component of pharmaceutical care practice (Arun et al., 2008). Medication adherence or the older term, drug compliance, is defined as the extent to which a person’s medication use behavior coincides with medical or health advice; and persistence as the duration of time from initiation to discontinuation of therapy (Cramer et al., 2008). For patients with T2DM, “behavior” is taking oral hypoglycemic agents (OHAs) and/or insulin injections, following diets, performing home blood glucose monitoring and making several lifestyle changes (Odegard and Capoccia, 2007). It has been demonstrated that only about 50% of T2DM patients comply with long-term treatment (Donnan et al., 2002).
After several decades of research, it was concluded that medication non-adherence is due to many factors including lack of adequate knowledge about medication and treatment goals, beliefs about the medication, complex regimens that are difficult to manage, side effects, and costs associated with medications (Martin et al., 2005; Osterberg and Blaschke, 2005). There are several types of non-adherence. Therapeutic or medication non-adherence which includes failure to have the prescription dispensed or renewed, omission of doses, errors of dosage, incorrect administration, errors in the time and frequency of administration, and premature discontinuation of the drug regimen. A second type of non-adherence is dietary/exercise non-adherence in which the patient fails to follow the diet and exercise recommendations. A third type is the appointment non-adherence in which the patient fails to show up at the clinics for the scheduled check up (Clark and Forwell, 2000). The consequences of medication non-adherence may not only be dangerous for patient’s health, but also dramatically increase the financial costs of public health services (Muszbek et al., 2008). The healthcare providers, inclusive of physician, pharmacist (hospital and community pharmacists), and nurses play an equally important role in achieving patient adherence to diabetic treatment regimens (Vermeire et al., 2005).
Several methods are used to measure therapeutic adherence. Indirect methods, like self reports and interviews with patient, are the simplest and most common methods for measuring medication adherence (Girerd et al., 2001). Pill counts method is also used to assess medication adherence in medical drug trials, by measuring the difference between the number of doses initially dispensed and the number remaining in the container (Rudd et al., 1998). The achievement of treatment goals might also be used to assess medication adherence, especially when the drug therapy is associated with a successful outcome like normal blood glucose levels. Computerized compliance monitors are the most recent and reliable methods, like the Medication Event Monitoring System (MEMS). The system consists of microprocessor placed in the cap of the medication container, every time the patient removes the cap; the time and date are recorded. Other modern technology is the mobile computing and communications technology embodied in the modern cell phone device which can be employed to improve the lives of diabetes patients by giving them better tools for self-management and improving the rate of medication adherence (Hedtke, 2008). Direct methods of measuring therapeutic adherence like measuring drug concentration or biological markers in the patients’ biological fluids, could also be used (Liu et al., 2002).
Few studies about patient adherence to OHAs in Arab Countries have been published. Most of these studies were carried out in Saudi Arabia. One study was performed at Al-Manhal primary health care center, aimed at identifying determinants of compliance among diabetic patients attending that clinic (Khattab et al., 1999). Other study has been conducted in Palestine aiming to study the effect of “polypharmacy” and “frequency of drug dosing” on the rate of compliance among diabetic and hypertensive patients (Sweileh et al., 2003). The third study was performed to study the rate of compliance among patients with DM and hypertension (Sweileh et al., 2005). A recent study was performed to gather data on current practices in the management of patients with T2DM in Saudi Arabia and to evaluate the degree of compliance with international guidelines (Al-Elq, 2009). Of the various methods available for assessing compliance, self reports and interviews with patients were the simplest and most common methods for measuring medication adherence (Girerd et al., 2001). On the other hand, it is established that adherence rates to treatment are bad in chronic illnesses. Nevertheless, data on medication adherence among diabetics are scarce (Beziea et al., 2006). The studies so far have generally evaluated medication adherence and its effects on metabolic control of diabetes, while factors affecting medication adherence itself have been analyzed less frequently (Schectman-Joel et al., 2002). For the previous reasons and due to the limited body of evidence regarding this important health and economic issue in the Egyptian population, we conducted this research study whose aim was to investigate the variability in the rate of medication adherence among Type 2 diabetic patients. This may lead to a clear understanding about poor glycemic control among these patients as well as for a strict and successful management of this chronic illness in the future.
2. Materials and methods
2.1. Patients’ characteristics
From November 2007 to March 2008, a total 226 patients were recruited in the current study. These patients were randomly selected from the Outpatient Clinics of Internal Medicine Department at Specialized Medical Hospital at University of Mansoura, Egypt. No patient was repeated. Patients’ consent was obtained according to the regulations of the Ministry of Health in Egypt. Patients were informed that personal information will never be disclosed to a third party.
Inclusion criteria for all participants were: patients ⩾18 years of age, who had been diagnosed with T2DM at least 1 year earlier, who received oral hypoglycemic medication (sulphonylurea or/and biguanide), who did not use insulin or suffer from chronic complications, and consented to participate in the study.
2.2. Assessment of medication adherence
The adherence was assessed during a personal interview with each patient using a structured questionnaire addressing the following aspects: (i) socio-demographic patient profile; (ii) level of knowledge about diabetes mellitus disease and its complications; (iii) access to and use of medicines, patients’ beliefs and motivation about OHA(s), patient-health care provider relationship, regularity of monitoring of blood glucose level, number of drug taken, drug regimen, experience side effects, and direct and indirect care costs in relation to patient income; (iv) assessment of patient adherence to medication using the Measure Treatment Adherence (MTA) Scale developed by Delgado and Lima (2001). This method was used before more frequently to measure patient compliance with drug treatment (Lopes et al., 2008). The MTA Scale, a variation of the Morisky-Green Test with seven questions, was used to assess patient behavior patterns associated with the use of medicines (Morisky et al., 1986). The MTA Scale consists of the following questions: (1) Have you ever forgotten to take your medicines? (2) Were you careless at times about taking your medicines? (3) When you felt better, did you sometimes stop taking your medicines? (4) Sometimes, if you felt worse, did you stop taking your medicines? (6) Have you ever discontinued treatment because you ran out of pills? (7) Have you ever stopped taking your medicines for any reason other than a medical advisory? The MTA Scale allows answers from “always” to “never,” with scores ranging from 1 to 4 points. The highest values indicate the highest level of compliance with drug treatment; (v) assessment of patient adherence to diet restrictions, exercise, and appointment for regular checkup in the clinics. All questions were read to the participant, and the answers were recorded by a pharmacist or a physician. Patients collecting more than 75% of the highest points were considered in the good adherence group. Patients collecting less than 50% of the points were considered in the non-adherence group and finally patients collecting between 50% and 75% of the points were considered in the poor/partial adherence group.
2.3. Data management and statistical analysis
Computer software GraphPad InStat version 3.00, GraphPad Software, San Diego, California, USA was used to analyze the data obtained from the questionnaire. Chi-square test and contingency coefficient test were used to analyze the significant correlations between adherence rate and the tested factors. For certain two variables, when P value is less than 0.05, there is a statistically significant relationship between the two variables.
3. Results
From a total of 417 patients who were clinically examined during the study period in the Department of Internal Medicine in Specialized Medical Hospital, Mansoura University, Mansoura, Egypt, only 226 patients (54.2%) fulfilled the inclusion criteria within the study period. The social characteristics of the selected group of patients and their demographic data are summarized in Table 1.
Table 1.
A correlation between patients’ socio-demographic characteristics and adherence rate to treatment with oral hypoglycemic agents.
| Variables | N (%) | Number of patients (%) in different categories |
Chi-square | P value | ||
|---|---|---|---|---|---|---|
| 226 (100) | Good adherence (N = 88) | Fair/poor adherence (N = 101) | Non-adherence (N = 37) | |||
| Gender | ||||||
| Male | 129 (57.1) | 42 (32.5) | 63 (48.8) | 24 (18.7) | 5.214 | 0.07 |
| Female | 97 (42.9) | 46 (47.5) | 38 (39.1) | 13 (13.4) | ||
| Age (years) | ||||||
| Young group (18–40) | 56 (24.8) | 29 (51.8) | 23 (41.1) | 4 (7.1) | 7.981 | 0.09 |
| Middle-age group (41–60) | 138 (61.0) | 50 (36.2) | 62 (44.9) | 26 (18.9) | ||
| Elderly group (⩾60) | 32 (14.2) | 9 (28.1) | 16 (50.0) | 7 (21.9) | ||
| Marital status | ||||||
| Single/widowed/divorced | 82 (36.3) | 18 (21.9) | 42 (51.2) | 22 (26.8) | 19.361 | <0.01⁎⁎ |
| Married | 144 (63.7) | 70 (48.6) | 59 (41.0) | 15 (10.4) | ||
| Educational status | ||||||
| No formal education (illiterate/basic) | 29 (12.8) | 7 (24.1) | 14 (48.3) | 8 (27.6) | 5.492 | 0.24 |
| School level education (middle level) | 81 (35.8) | 30 (37.0) | 38 (47.0) | 13 (16.0) | ||
| University level education or more (high level) | 116 (51.4) | 51 (43.9) | 49 (42.2) | 16 (13.85) | ||
| Family support | ||||||
| Present | 134 (59.3) | 64 (47.7) | 51 (38.1) | 19 (14.2) | 10.786 | <0.01⁎⁎ |
| Absent | 92 (40.7) | 24 (26.1) | 50 (54.4) | 18 (19.5) | ||
| Socio-economical level | ||||||
| High | 12 (5.3) | 8 (66.6) | 2(16.6) | 2(16.6) | 21.389 | <0.01⁎⁎ |
| Middle | 58 (25.7) | 34 (58.6) | 15 (25.8) | 9 (15.6) | ||
| Low | 156 (69.0) | 46 (29.4) | 84 (53.8) | 26 (16.6.) | ||
| Place of residence | ||||||
| City | 136 (60.1) | 57 (41.9) | 61(44.8) | 18 (13.2) | 2.830 | 0.243 |
| Village | 90 (39.9) | 31 (34.4) | 40 (44.4) | 19 (23.3) | ||
∗Significance difference between good, poor and non-adherence categories according to different variables at (P < 0.05 using Chi-square test).
High significance difference at (P < 0.01).
Several factors were found to have significant effects on the rate of medication adherence (Table 2).
Table 2.
Factors affecting rate of medication adherence in Type 2 diabetic patients.
| Variables | N (%) | Number of patients (%) in different categories |
Chi-square | P value | ||
|---|---|---|---|---|---|---|
| 226 (100) | Good adherence (N = 88) | Fair/Poor adherence (N = 101) | Non-adherence (N = 37) | |||
| Patient knowledge | ||||||
| Rich/adequate | 86 (38.0) | 46 (53.5) | 22 (25.6) | 18 (20.9) | 20.654 | <0.01⁎⁎ |
| Poor | 140 (62.0) | 42 (30.0) | 79 (56.4) | 19 (13.6) | ||
| Patients’ beliefs and motivation about OHAs | ||||||
| Good | 101 (44.7) | 64 (63.3) | 25 (24.8) | 12 (11.9) | 46.477 | <0.01⁎⁎ |
| Weak | 125 (55.3) | 24 (19.2) | 76 (60.8) | 25 (20.0) | ||
| Patient-health care provider relationship | ||||||
| Good communication | 132 (58.4) | 59 (44.7) | 55 (41.7) | 18 (13.6) | 4.803 | 0.09 |
| Poor communication | 94 (41.6) | 29 (30.9) | 46 (48.9) | 19 (20.2) | ||
| Monitoring of blood glucose level | ||||||
| Regular | 65 (28.7) | 43 (66.1) | 15 (23.1) | 7 (10.7) | 28.643 | <0.01⁎⁎ |
| Irregular | 161 (71.3) | 45 (27.9) | 86 (53.5) | 30 (18.6) | ||
| Number of drug taken | ||||||
| Monotherapy | 87 (38.5) | 41 (47.1) | 39 (44.8) | 7 (8.1) | 9.340 | <0.05⁎ |
| Combination therapy | 46 (22.3) | 16 (34.8) | 22 (47.9) | 8 (17.3) | ||
| Polypharmacy | 93 (41.2) | 31 (33.3) | 40 (43.1) | 22 (23.6) | ||
| Drug regimen | ||||||
| Complex | 118 (52.2) | 31 (26.3) | 56 (47.5) | 31(26.2) | 16.665 | <0.01⁎⁎ |
| Simple | 108 (47.8) | 57 (52.8) | 33 (30.6) | 18 (16.6) | ||
| Experience side effects | ||||||
| Present | 137 (60.6.) | 38 (27.7) | 74 (54.1) | 25 (18.2) | 18.725 | <0.01⁎⁎ |
| Absent | 89(39.4) | 50 (56.1) | 27 (30.4) | 12 (13.5) | ||
| Direct and indirect care cost s in relation to patient income | ||||||
| Adequate | 97 (42.9) | 56 (57.7) | 32 (33.0) | 9 (9.3) | 25.844 | <0.01⁎⁎ |
| Inadequate | 129 (57.1) | 32 (24.8) | 69(53.5) | 28 (21.7) | ||
Significance difference between good, poor and non-adherence categories according to different variables at (P < 0.05 using Chi-square test).
High significance difference at (P < 0.01).
The overall rate of medication adherence, dietary/exercise adherence, and appointment adherence among the patients population was found to be suboptimal and non-acceptable (Fig. 1).
Figure 1.
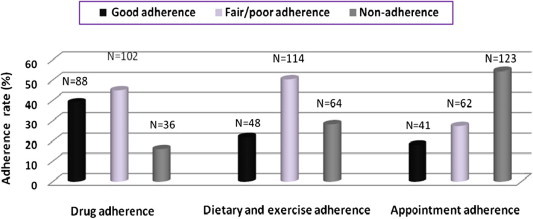
Overall adherence rate among Type 2 diabetic patients.
4. Discussion
Poor adherence to medication seems to be a significant barrier to attainment of positive clinical or therapeutic outcomes among Type 2 diabetic patients in both developed and developing countries (Adisa et al., 2009). It has been reported that, in general, diabetic patients are non-adherent to their treatment and only a small number of diabetic patients were found adherent or compliant with all aspects of diabetic care (Kurtz, 1990). This is in agreement with the current research study as it was noted that only 38.9%, 21.1% and 18.4% of all patients were belonging to the good category of adherence to drug, dietary/exercise and to the appointment for regular fellow up, respectively. The others were ranging between the poor to the non-adherence categories. Unfortunately, there is no published data yet regarding adherence to OHAs in Egypt in order to compare with these results.
Our results have also shown that therapeutic adherence was significantly affected by different patient-centered factors like marital status, family support, socio-economical level, patients’ knowledge about the diabetes mellitus disease, patients’ beliefs and motivation about OHAs, and patient self monitoring of blood glucose level. Also, it was shown that drug-related factors like number of medication therapy taken, complexity of drug regimen, presence of drug side effects, and finally cost of treatment significantly affect the rate of adherence to OHAs. On the other hand, a non-significant higher rate of medication was found in females than in males.
Married patients showed significant higher rate of therapeutic adherence (48.6%) than single, widowed or divorced ones (21.9%). Marital status might influence patients’ compliance with medication positively. The help and support from a spouse could be the reason why married patients were more compliant to medication than single patients (Cooper et al., 2005).
The effect of the education factor on the degree of adherence to medication was not surprising in our patient population. More educated people tend to appreciate and understand the consequences of non-adherence. Thus the degree of adherence was increased but none significantly with increasing level of education. Illiterate patients cannot read or distinguish their medications which increase the risk of errors and nonadherence. Illiteracy might negatively affect patients’ medical knowledge (Sweileh et al., 2005).
Support provided by family also played a beneficial role in enhancing adherence (Kasznicki et al., 2007). The general findings from different research articles showed that patients who had emotional support and help from family members, or healthcare providers were more likely to be adherent to the treatment (Seol and Min, 2005; Voils et al., 2005). The social support helps patients in reducing negative attitudes to treatment having motivation and remembering to implement the treatment as well.
The effect of age and gender were obvious but also non-significant in our results. The effect of gender on the rate of adherence to medication in other research studies is contradictory. Female patients were found by some researchers to have better adherence (Lertmaharit et al., 2005), while some studies suggested otherwise (Hertz et al., 2005). In addition, some studies could not find a relationship between gender and adherence to medication (Senior et al., 2004).
Moreover, a non-significant lower rate of drug compliance was found in elderly patients (28.1%) and middle-aged group (36.2%) than younger group of patients (51.8%). With increasing age, the degree of adherence decreases for several reasons. For example, most of the elderly patients have memory problems related to age or due to dementia or Alzheimer’s disease. Furthermore, most elderly patients have vision and hearing problems that might increase the potential of mistakes in taking medications. Another problem with elderly is that most of them have several diseases and take several drugs at the same time which might be confusing to most elderly patient. These general characteristics are common among elderly patients in most societies and that is why similar findings were made in other countries by other researchers (Norell, 1985; Sweileh et al., 2005).
Our results confirm that one of the most important factor contributing to adherence to OHAs was the level of patients’ knowledge about the disease, its causes, principles of drug therapy and complications of drug therapy as well as patients’ beliefs and motivation about OHAs. Patients who had low motivation to change behaviors or take medication are believed to have poor compliance (Spikmans et al., 2003).
Patient’s knowledge about their disease and treatment is not always adequate. Some patients lack understanding of the role their therapies play in the treatment (Ponnusankar et al., 2004); others lack knowledge about the disease and consequences of poor adherence (Gascon et al., 2004); or lack understanding of the value of clinic visits (Lawson et al., 2005). Some patients thought that the need for medication was intermittent, so they stopped the drug to see whether medication was still needed (Bender and Bender, 2005). For these reasons, patient education is very important to enhance adherence to OHAs.
A healthy relationship is based on patients’ trust in prescribers and empathy from the prescribers, pharmacists and nurses. Studies have found that adherence to medication is good when healthcare providers are emotionally supportive, giving reassurance or respect, and treating patients as an equal partner (Lawson et al., 2005).
Self management behavior with emphasis on regular monitoring of blood glucose found to be low (28.7%) among our patients population. Many of our diabetes patients were not aware of self monitoring of blood glucose level at home (SMBG) or lack financial support to buy the apparatus for regular and prompt detection of fluctuations in their blood glucose levels. This finding was in conformity with the report of a study in US where many diabetes patients in US were reported never to have monitored their blood glucose levels (Harris et al., 1993). The absence of established guidelines on SMBG and lack of its perceived importance by patients, as well as, the cost of the blood glucose monitoring device especially in a developing country like Egypt, may have accounted for the low level of awareness among patients. Though practice of SMBG does not necessarily mean that patient is adherent with prescribed treatment recommendations but it may be an indication of active commitment of patient to his/her diabetes management.
The results also showed clearly an inverse relationship between the rate of adherence to OHAs and the number of drug therapy in patient’s population. The rate of non-adherence jumps from 8.1% to 17.3% and 23.6 % when the number of medications is increased from one oral OHA (sulphonylurea or biguanide) to two drugs for treatment of diabetes (combination therapy like a sulphonylurea with a biguanide) or more than two for treatment of diabetes and other disease problems (polypharmacy like T2DM and hypertension), respectively. These results are in agreement with the findings in other research study (Sweileh et al., 2003).
Complex treatment is believed to threaten the patient’s compliance. Our results showed that the rate of adherence to OHAs was increased from (26.3%) in patients who took multiple daily dosing (MDD) to the double (52.8%) in patients who took once daily dosing (ODD) indicating that in Type 2 diabetic patients, once daily dosing is the best. This is in agreement with the findings of other researchers who found that the rate of compliance decreased as the number of daily doses increased (Iskedjian et al., 2002). Thus, simplifying the medication dosing frequency could improve the adherence markedly.
Side effects of OHAs like loss of appetite, nausea, diarrhea and intestinal discomfort were mentioned by our diabetic patients and were considered as a part of the factors contributing to medication nonadherence. This confirmed the findings in the literature that reported that the side effects of medication may be a significant factor that can affect diabetes patients’ long-term adherence to treatment programs (Jayant et al., 2000).
A significant higher rate of adherence to OHAs (57.7%) was observed in patients who exhibited adequate healthcare costs in relation to their income or full coverage health insurance compared with the others who did not have (24.8%). Financial variables especially the direct and indirect costs associated with a prescribed regimen and restricted access to therapy have been found by several studies to influence patients’ commitment to medication adherence in developing countries (Ohene-Buabeng et al., 2004; Adisa et al., 2009). A number of studies found that patients who had no insurance cover (Kaplan et al., 2004; Choi-Kwon et al., 2005), or who had low income (Mishra et al., 2005) were more likely to be non-adherent to treatment.
Aerobic exercise and restricted food was reported to be part of the recommended non-drug management of diabetes mellitus disease (Hensrud, 2001). It was obvious from our results that the rate of non-adherence to appointment for regular checkup of the patients at clinics is much higher (54.4%) than non-adherence to dietary restriction and applying aerobic exercise (28.3%) and to medication (15.9%). The overall adherence to medication, diet restriction/aerobic exercise and to appointment was found to be suboptimal. These results were also observed in other research studies (Spikmans et al., 2003).
5. Conclusions
Our study population of patients with T2DM has demonstrated unsatisfactory adherence to OHAs, dietary/exercise and even appointment to show up at the clinics for the scheduled check up. An improvement with medication adherence may be achieved through continuing patient education about the disease, improvement of patients’ socio-economical levels, encouraging patients to monitor their blood glucose level regularly, simplifying drug regimen with decreasing the number of drug taken as can as possible as well as reducing in the medication cost which is considered as a new strategy of Ministry of Health in Egypt nowadays. This strategy aimed to optimize medication costs for the majority of chronically ill patients and this may give a sound regarding adherence to medication in the near future. Our recommendations for future works are to use validated adherence measures, e.g., Medication Adherence Reports Scale (MARS) and to run other methods concurrently for assessment of therapeutic adherence, e.g., pill counts for a comparison study. Moreover, it is very important to conduct a research on a larger sample population and from different clinical settings and areas but this will require a good budget for a financial support. Further research studies should emphasize the importance of effective patient-health care provider communication in overcoming some of the barriers to therapeutic compliance.
6. Conflict of interest
We declare that there is no conflict of interest on this research study. The research study did not receive funds or support from any source.
Acknowledgements
We would like to express our appreciation to all members in the Department of Internal Medicine, Faculty of Medicine, University of Mansoura, Mansoura, Egypt for their continuous help and our deepest thanks to all patients who participated in this work.
Contributor Information
Mohamed E.E. Shams, Email: mshamspharma@gmail.com, mshamspharma@yahoo.com, http://www.biomedexperts.com/Profile.bme/1284993/Mohamed_Shams.
Enaase A.M.E. Barakat, Email: dr_enaas@hotmail.com.
References
- Adisa R., Alutundu M.B., Fakeye T.O. Factors contributing to nonadherence to oral hypoglycemic medications among ambulatory type 2 diabetes patients in Southwestern Nigeria. Pharm. Pract. (Internet) 2009;7:163–169. doi: 10.4321/s1886-36552009000300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Elq A.H. Current practice in the management of patients with type 2 diabetes mellitus in Saudi Arabia. Saudi Med. J. 2009;30:1551–1556. [PubMed] [Google Scholar]
- Arun K., Murugan R., Rajesh Kanna M., Rajalakshmi S., Kalaiselvi R., Komathi V. The impact of pharmaceutical care on the clinical outcome of diabetes mellitus among a rural patient population. Int. J. Diabetes Dev. Ctries. 2008;28:15–18. doi: 10.4103/0973-3930.41981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender B.G., Bender S.E. Patient-identified barriers to asthma treatment adherence. Responses to interviews, focus groups, and questionnaires. Immunol. Allergy Clin. North Am. 2005;25:107–130. doi: 10.1016/j.iac.2004.09.005. [DOI] [PubMed] [Google Scholar]
- Beziea Y., Molinaa M., Hernandezb N., Batistaa R., Nianga S., Huetb D. Therapeutic compliance. A prospective analysis of various factors involved in the adherence rate in type 2 diabetes. Diabetes Metab. 2006;32:611–616. doi: 10.1016/S1262-3636(07)70316-6. [DOI] [PubMed] [Google Scholar]
- Choi-Kwon S., Kwon S.U., Kim J.S. Compliance with risk factor modification: early-onset versus late-onset stroke patients. Eur. Neurol. 2005;54:204–211. doi: 10.1159/000090710. [DOI] [PubMed] [Google Scholar]
- Clark W.F., Forwell L. Patient compliance with drug therapy for diabetic nephropathy. Can. Med. Assoc. J. 2000;162:1553–1560. [PMC free article] [PubMed] [Google Scholar]
- Cooper C., Carpenter I., Katona C. The AdHOC study of older adults’ adherence to medication in 11 countries. Am. J. Geriatr. Psychiatry. 2005;13:1067–1076. doi: 10.1176/appi.ajgp.13.12.1067. [DOI] [PubMed] [Google Scholar]
- Cramer J., Roy A., Burrell A., Anuja R., Burrell A., Fairchild C., Fuldeore M., Ollendorf D., Wong P. Medication compliance and persistence. Terminology and definitions. Value Health. 2008;11:44–47. doi: 10.1111/j.1524-4733.2007.00213.x. [DOI] [PubMed] [Google Scholar]
- Delgado A., Lima M. Contributo para a validação concorrente de uma medidade de adesão aos tratamentos. Psicologia, Saúde & Doenças. 2001;2:81–100. [Google Scholar]
- Diabetes Atlas, second ed. International Diabetes Federation, Brussels, 2003.
- Donnan P.T., MacDonald T.M., Morris A.D. Adherence of prescribed oral hypoglycaemic medication in a population of patients with type 2 diabetes: a retrospective cohort study. Diabetes Med. 2002;19:279–284. doi: 10.1046/j.1464-5491.2002.00689.x. [DOI] [PubMed] [Google Scholar]
- Gascon J.J., Sanchez-Ortuno M., Llor B. Treatment compliance in hypertension study group. Why hypertensive patients do not comply with the treatment: results from a qualitative study. Fam Pract. 2004;21:125–130. doi: 10.1093/fampra/cmh202. [DOI] [PubMed] [Google Scholar]
- Girerd X., Hanon O., Anagnostopoulos K., Ciupek C., Mourad J., Consoli S. Assessment of antihypertensive compliance using a self-administered questionnaire: development and use in a hypertension clinic. Pressed Med. 2001;30:1044–1048. [PubMed] [Google Scholar]
- Harris M.I., Cowie C.C., Howie L.J. Self monitoring of blood glucose by adults with diabetes in the United States population. Diabetes Care. 1993;16:1116–1123. doi: 10.2337/diacare.16.8.1116. [DOI] [PubMed] [Google Scholar]
- Hedtke P.A. Can wireless technology enable new diabetes management tools? J. Diabetes Sci. Technol. 2008;2:127–130. doi: 10.1177/193229680800200118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hensrud D.D. Dietary treatment and long-term weight loss and maintenance in type 2 diabetes. Obes. Res. 2001;9:348–353. doi: 10.1038/oby.2001.141. [DOI] [PubMed] [Google Scholar]
- Hertz R.P., Unger A.N., Lustik M.B. Adherence with pharmacotherapy for type 2 diabetes: a retrospective cohort study of adults with employersponsored health insurance. Clin. Ther. 2005;27:1064–1073. doi: 10.1016/j.clinthera.2005.07.009. [DOI] [PubMed] [Google Scholar]
- Iskedjian M., Einarson T.R., MacKeigan L.D. Relationship between daily dose frequency and adherence to antihypertensive pharmacotherapy: evidence from a meta-analysis. Clin. Ther. 2002;24:302–316. doi: 10.1016/s0149-2918(02)85026-3. [DOI] [PubMed] [Google Scholar]
- Jayant D., Lawrence B., Richard G. Factor influencing patient acceptability of diabetes treatment regimens. Clin. Diabetes. 2000;l8:2–12. [Google Scholar]
- Kalyango J., Owino E., Nambuya A. Non-adherence to diabetes treatment at Mulago Hospital in Uganda: prevalence and associated factors. Afr. Health Sci. 2008;8:67–73. [PMC free article] [PubMed] [Google Scholar]
- Kaplan R.C., Bhalodkar N.C., Brown E.J. Race, ethnicity, and sociocultural characteristics predict noncompliance with lipid-lowering medications. Prev. Med. 2004;39:1249–1255. doi: 10.1016/j.ypmed.2004.04.041. [DOI] [PubMed] [Google Scholar]
- Kasznicki J., Głowacka A., Drzewoski J. Type 2 diabetic patients compliance with drug therapy and glycaemic control. Diabetologia Doświadczalna i Kliniczna. 2007;7:199–203. [Google Scholar]
- Khattab M.S., Abolotouh M.A., Khan M.Y., Humaidi M.A., Al-Khaldi Y.M. Compliance and control of diabetes in a family practice setting, Saudi Arabia. East Mediterr. Health J. 1999;4:755–765. [PubMed] [Google Scholar]
- Kurtz M.S. Adherence to diabetic regimens: empirical status and clinical applications. Diabetes Educ. 1990;16:50–56. doi: 10.1177/014572179001600112. [DOI] [PubMed] [Google Scholar]
- Lawson V.L., Lyne P.A., Harvey J.N. Understanding why people with type 1 diabetes do not attend for specialist advice. A qualitative analysis of the views of people with insulin-dependent diabetes who do not attend diabetes clinic. J. Health Psychol. 2005;10:409–423. doi: 10.1177/1359105305051426. [DOI] [PubMed] [Google Scholar]
- Lertmaharit S., Kamol-Ratankul P., Sawert H. Factors associated with compliance among tuberculosis patients in Thailand. J. Med. Assoc. Thai. 2005;88:149–156. [PubMed] [Google Scholar]
- Liu H., Kaplan A.H., Wenger N.S. Measuring patient adherence. Ann. Intern. Med. 2002;137:72–73. doi: 10.7326/0003-4819-137-1-200207020-00024. [DOI] [PubMed] [Google Scholar]
- Lopes N., Zanini A.C., Casella-Filho A., Chagas A.C.P. Metabolic syndrome patient compliance with drug treatment. Clinics. 2008;63:573–580. doi: 10.1590/S1807-59322008000500002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddigan S.L., Feeny D.H., Johnson J.A. Health related quality of life deficits associated with diabetes and co morbidities in a Canadian national population health survey. Qual. Life Res. 2005;14:1311–1320. doi: 10.1007/s11136-004-6640-4. [DOI] [PubMed] [Google Scholar]
- Martin L., Williams S., Haskard K., DiMatteo M.R. The challenge of patient adherence. Ther. Clin. Risk Manage. 2005;1:189–199. [PMC free article] [PubMed] [Google Scholar]
- Mishra P., Hansen E.H., Sabroe S. Socio-economic status and adherence to tuberculosis treatment: a case-control study in a district of Nepal. Int. J. Tuberc. Lung Dis. 2005;9:1134–1139. [PubMed] [Google Scholar]
- Morisky D.E., Green L.W., Levine D.M. Concurrent and predictive validity of self-reported measure of medication adherence. Med. Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- Muszbek N., Brixner D., Benedict A., Keskinaslan A., Khan Z.M. The economic consequences of noncompliance in cardiovascular disease and related conditions: a literature review. Int. J. Clin. Pract. 2008;62:338–351. doi: 10.1111/j.1742-1241.2007.01683.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norell S.E. Memory and medication compliance. J. Clin. Hosp. Pharm. 1985;10:107–109. doi: 10.1111/j.1365-2710.1985.tb00723.x. [DOI] [PubMed] [Google Scholar]
- Odegard P., Capoccia K. Medication taking and diabetes: a systematic review of the literature. Diabetes Educ. 2007;33:1014–1029. doi: 10.1177/0145721707308407. [DOI] [PubMed] [Google Scholar]
- Ohene-Buabeng K., Motowel L., Plange-Rhule J. Unaffordable drug prices: the major cause of noncompliance with hypertensive medication in Ghana. J. Pharm. Sci. 2004;7:350–352. [PubMed] [Google Scholar]
- Osterberg L., Blaschke T. Adherence to medication. N. Engl. J. Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- Paulose K. Disease awareness study in diabetic patients. Asian J. Diabetes. 2000;2:15–19. [Google Scholar]
- Ponnusankar S., Surulivelrajan M., Anandamoorthy N. Assessment of impact of medication counseling on patients’ medication knowledge and compliance in an outpatient clinic in South India. Patient Educ. Couns. 2004;54:55–60. doi: 10.1016/S0738-3991(03)00193-9. [DOI] [PubMed] [Google Scholar]
- Rickles N., Brown T., McGivney M., Snyder M., White K. Adherence. A review of education, research, practice, and policy in the United States. J. Pharm. Pract. (Internet) 2010;8:1–17. doi: 10.4321/s1886-36552010000100001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd P., Byyny R.L., Zachary V., LoVerde M.E., Mitchell W.D., Titus C., Marshall G. Pill count measures of compliance in a drug trial: variability and suitability. Am. J. Hypertens. 1998;1:309–312. doi: 10.1093/ajh/1.3.309. [DOI] [PubMed] [Google Scholar]
- Schectman-Joel M., Nadakarni-Mohan M., Voss-John D. The association between diabetes metabolic control and drug adherence in an indigent population. Diabetes Care. 2002;25:1015–1021. doi: 10.2337/diacare.25.6.1015. [DOI] [PubMed] [Google Scholar]
- Senior V., Marteau T.M., Weinman J. Self-reported adherence to cholesterol-lowering medication in patients with familial hypercholesterolaemia: the role of illness perceptions. Cardiovasc. Drugs Ther. 2004;18:475–481. doi: 10.1007/s10557-004-6225-z. [DOI] [PubMed] [Google Scholar]
- Seol M.A., Min S.K. Development of a structural model explaining medication compliance of persons with schizophrenia. Yonsei Med J. 2005;46:331–340. doi: 10.3349/ymj.2005.46.3.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spikmans F.J., Brug J., Doven M.M. Why do diabetic patients not attend appointments with their dietitian? J. Hum. Nutr. Diet. 2003;16:151–158. doi: 10.1046/j.1365-277x.2003.00435.x. [DOI] [PubMed] [Google Scholar]
- Sweileh W., Aker O., Hamooz S. Effect of polypharmacy and frequency of drug dosing” on rate of compliance among diabetic and hypertensive patients: a survey study in Palestine. An-Najah Univ. J. 2003;17:155–165. [Google Scholar]
- Sweileh W., Aker O., Hamooz S. Rate of compliance among patients with diabetes mellitus and hypertension. An-Najah Univ. J. 2005;19:2–11. [Google Scholar]
- The World Health Report, 2003. Shaping the Future. World Health Organization, Geneva.
- Vermeire, E., Wens, J., Van Royen, P., Biot, Y., Hearnshaw, H., Lindenmeyer, A., 2005. Interventions for improving adherence to treatment recommendations in people with type 2 diabetes mellitus. Cochrane Database Syst. Rev. 18, CD003638. [DOI] [PMC free article] [PubMed]
- Voils C.I., Steffens D.C., Flint E.P. Social support and locus of control as predictors of adherence to antidepressant medication in an elderly population. Am. J. Geriatr. Psychiatry. 2005;13:157–165. doi: 10.1176/appi.ajgp.13.2.157. [DOI] [PubMed] [Google Scholar]


