Abstract
Objective
To determine the frequency and effects of nosocomial respiratory viral infections (RVIs) in premature neonates, including those who may be asymptomatic.
Study design
We performed a year-long surveillance for RVIs in infants <33 weeks gestational age admitted to 2 Syracuse neonatal intensive care units. Infants were enrolled within 3 days of neonatal intensive care unit admission and were sampled for RVIs until discharge using a multiplex polymerase chain reaction assay capable of detecting 17 different respiratory viruses or subtypes.
Results
Twenty-six of 50 prematurely born infants (52%) tested positive for a respiratory virus at least once during their birth hospitalization. Testing positive for a respiratory virus was significantly associated with longer length of stay (70 days vs 35 days, P = .002) and prolonged ventilatory support (51 vs 13 days, P = .002). Infants who tested positive for a respiratory virus during their birth hospitalization had more than twice the rate of developing bronchopulmonary dysplasia (P < .05).
Conclusion
Nosocomial RVIs were frequent in our study population, despite the absence of clinical indicators of illness. Length of hospital stay was significantly longer and a diagnosis of bronchopulmonary dysplasia was more common in infants who had respiratory viruses detected.
Keywords: BPD, Bronchopulmonary dysplasia; GA, Gestational age; hMPV, Human metapneumovirus; MRSA, Methicillin-resistant Staphylococcus aureus; NICU, Neonatal intensive care unit; PCR, Polymerase chain reaction; PIV, Parainfluenzavirus; RSV, Respiratory syncytial virus; RVI, Respiratory viral infection
Recent work has challenged the widely-held assumption that newborns in neonatal intensive care units (NICUs) are protected from infections present in the community. Outbreaks of common respiratory viruses among hospitalized infants have been described, including influenza virus, respiratory syncytial virus (RSV), coronavirus, parainfluenzavirus (PIV), adenovirus, enterovirus, and rhinovirus.1, 2, 3, 4, 5, 6, 7, 8 In most of these published studies, virus detection was ascertained only in symptomatic infants. In others, surveillance for respiratory virus pathogens was initiated only after an outbreak was established. Of note, respiratory viral infections (RVIs) were detected in minimally symptomatic and even asymptomatic infants when widespread screening was instituted during outbreaks.3 Moreover, premature infants often have atypical symptoms of infection, such as feeding difficulty, periodic breathing, or apnea.8, 9, 10 Reports of NICU outbreaks generally have focused on a single infectious agent, and studies extending to multiple viruses are hampered by the technical limitations associated with routine assays such as antigen detection and virus culture. Recent developments in multiplex polymerase chain reaction (PCR) testing permit rapid, sensitive testing for multiple viruses from a single specimen, including viruses for which culture is unavailable and/or unreliable or for which rapid antigen assays do not exist. In this study, we report the results of a year-long surveillance study in 2 NICUs in Syracuse, New York, in which infants’ nasopharyngeal specimens were tested for 17 different viruses in longitudinal fashion from birth to discharge.
Methods
We performed a prospective, observational study of premature infants in 2 NICUs in Syracuse, NY, during 1 calendar year (2009). Infants were eligible if they were born at less than 33 weeks, 0 days gestational age (GA), and were available for enrollment within 3 days of arrival in the NICU, which included transfer from another facility or following hospital birth. Neonates with medical and surgical diagnoses were included. GA was determined by menstrual dates and confirmed by ultrasound. Infants were excluded if they had a known or suspected immune deficiency, or were born to a human immunodeficiency virus-positive mother. After obtaining informed consent, nasopharyngeal specimens were collected using flocked swabs (Copan Diagnostics, Inc, Corona, California) from each infant by study personnel trained in the proper procedure for obtaining a nasopharyngeal specimen (including intubated infants to ensure sample consistency) within 3 days of birth and on a regular twice weekly (Monday/Thursday) schedule thereafter until discharge. Sampling was deferred on a particular day if the procedure was deemed to place the infant at risk. Specimens were placed in 1.5 mL universal transport media (Copan) and frozen at −70°C prior to testing with the xTAG respiratory viral panel (RVP; Luminex Molecular Diagnostics, Inc, Toronto, Ontario, Canada). RVP is a multiplex PCR assay that detects influenza A H1, H3, and nonspecific; influenza B; RSV A and B; PIV 1, 2, 3, and 4; coronavirus 229E, NL63, HKU-1, and OC43; rhinovirus/enterovirus; adenovirus; and human metapneumovirus (hMPV). Clinical and demographic data were collected from the medical records. At each sampling timepoint, the use of mechanical ventilation and percent of inspired oxygen was recorded, along with the results of any microbiologic testing performed for appropriate clinical purposes. Clinical events (episodes of oxygen desaturation, bradycardia, or apnea) were recorded daily according to the existing criteria being used routinely by the nursing staff in both NICUs. To qualify as an event, the aforementioned change had to persist for longer than 20 seconds. Oxygen saturation below 88% and a heart rate below 100 beats per minute were the cutoff points used for desaturation and bradycardia events, respectively. Clinical deteriorations were defined as a sustained (lasting 3 days) increase in daily oxygen desaturation events from the prior baseline rate, an increase in oxygen requirement (as judged by the current inhaled oxygen concentration required for stable oxygen saturations, excluding transient desaturations associated with feeding), or an increased level of respiratory support (moving from nasal cannula to continuous positive airways pressure, or to intubation or mechanical ventilation). A diagnosis of bronchopulmonary dysplasia (BPD) was made if an infant required supplemental oxygen at 36 weeks post-conceptional age.
The 2 NICUs in the study were a level 3 unit with a daily average census of approximately 12 infants, and a level 4 regional center with a daily average census of approximately 55 infants. Throughout the study period, each NICU operated under its usual infection control procedures: all staff employed an extended hand and arm scrub on arrival to the unit, and standard precautions were in place at all times. All direct patient contact by medical staff required gloves. Contact precautions also were in place (gown and glove) for patients known to be colonized or infected with methicillin-resistant Staphylococcus aureus (MRSA). MRSA screening by PCR was performed on all patients at the regional center on a weekly basis. All children (age 17 years and younger) were excluded from the units and adult visitors were excluded if ill. Parents who had respiratory symptoms were discouraged from visiting but allowed to visit if they wore gowns, gloves, and a surgical mask. In the regional center NICU, twin and triplet births were separated into different nursing areas. No healthcare personnel were aware of the results of the respiratory virus detection tests during the study.
Statistical comparisons between groups were performed using Fisher exact test or Student t test as appropriate. Time to infection was calculated as the interval between birth date and infection date for the first infection and the interval between previous and current infection dates for repeated infections. The marginal effects of several variables, including NICU units, sex, GA, and birth weight on time to infection were presented by Kaplan-Meier infection-free probability curves and tested by Log-rank test. A Cox proportional hazards regression model was further fitted to examine the effect of each covariate, adjusting the effect of other covariates. A random-effect term was included to adjust the dependence among the multiple observations from the same infant. The proportional hazards assumption and possible outliers were visually examined through Schoenfeld and deviance residual plots. A path model, focusing on the direct and indirect effects of infection on the hospital stay, was proposed and confirmed by using SAS v. 9.2 PROC CALIS (SAS Institute, Cary, North Carolina) under which the algorithm was optimized via a Quasi-Newton method. Statistical significance was defined at a level of P = .05.
The research was approved by the Institutional Review Boards of St. Joseph’s Hospital Health Center and Crouse Irving Memorial Hospital, both of Syracuse, NY (Institutional Review Board for the Protection of Human Subjects #2008.147 and #2008.4657, respectively).
Results
Approximately one-half of the parents approached for the study consented to enrollment. The most common reason given for refusal was a concern for an additional procedure on a very small baby, which may have skewed our population towards enrolling neonates of later GA. Fifty infants were enrolled into the study; 27 (54%) were male. The average GA was 28 weeks (range 24 to 32). Eighteen infants (36%) had GA <28 weeks. The average duration of birth hospitalization was 54.6 days. Twenty-five infants (50%) were intubated at some time during hospitalization, for a mean of 12.5 days. Twenty-eight infants (56%) required supplemental oxygen at some time during hospitalization, and 17 (34%) met criteria for diagnosis of BPD. Eleven infants were enrolled from the level 3 NICU, and 39 were from the level 4 regional NICU. One infant died.
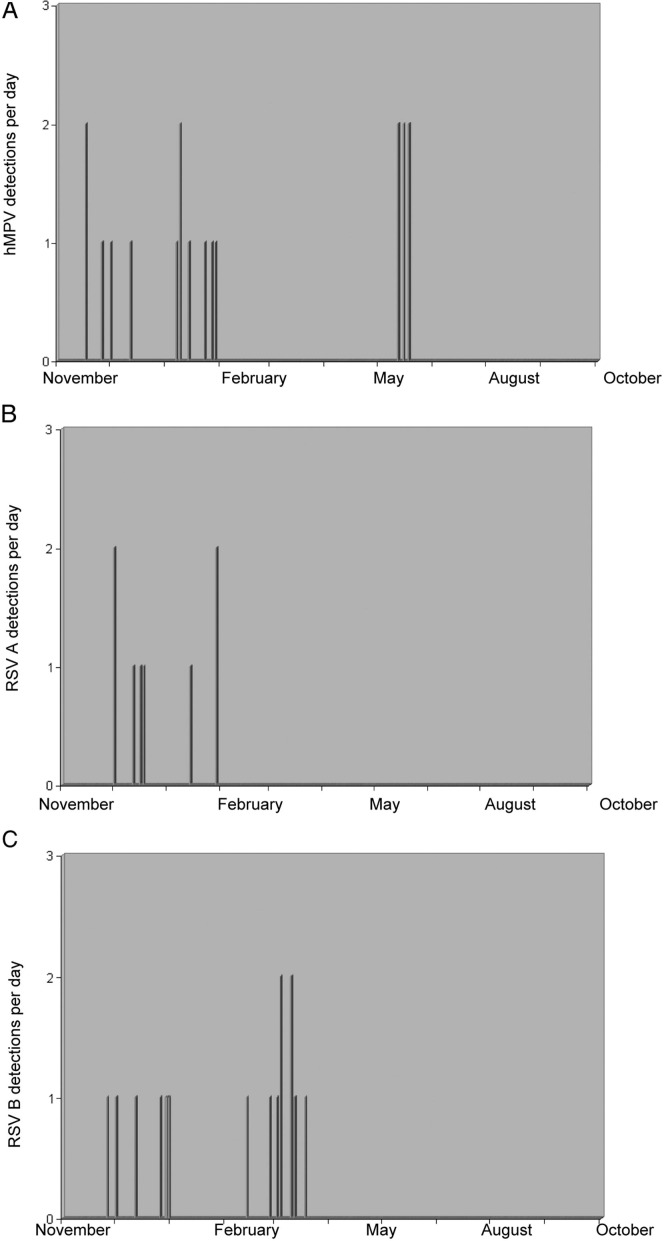
A total of 708 specimens were obtained and tested from the 50 patients over the 52-week period, for an average of 13.6 specimens per week. No weeks were missed but the level of enrollment varied throughout the year—at any 1 time, the number of active patients from the level 3 NICU varied between 0 and 4, and at the level 4 NICU between 2 and 8. Sixty-six of 708 specimens tested positive for at least 1 respiratory virus; 26 neonates (52%) were positive for a respiratory virus on at least 1 occasion. The mean time to detection of the first positive sample was 24 days (range 0-92). For each infected patient, an average of 2.5 swabs were positive during their hospital stay (range 1-13). Viruses detected in the 26 positive patients were PIV3 (13 patients), hMPV (9 patients), RSV-B (8 patients), RSV-A (7 patients), PIV-2 (7 patients), entero/rhinovirus (7 patients), and influenza B (4 patients). Eighteen samples (28% of the positive swabs) included more than 1 virus, and some infants were positive for different viruses at different times. There was evidence of seasonality of detection of particular viruses, with clusters observed (Figure 1 ). Fourteen patients had sequentially positive specimens for the same virus, with specimens positive over a range of 3-13 days; however, because we obtained specimens only twice weekly, an accurate determination of duration cannot be made. Sequential detection of hMPV, RSV B, PIV 3, and enterovirus/rotavirus occurred.
Figure 1.
Seasonality of 3 respiratory virus detection: A, hMPV, B, RSV A, and C, RSV B.
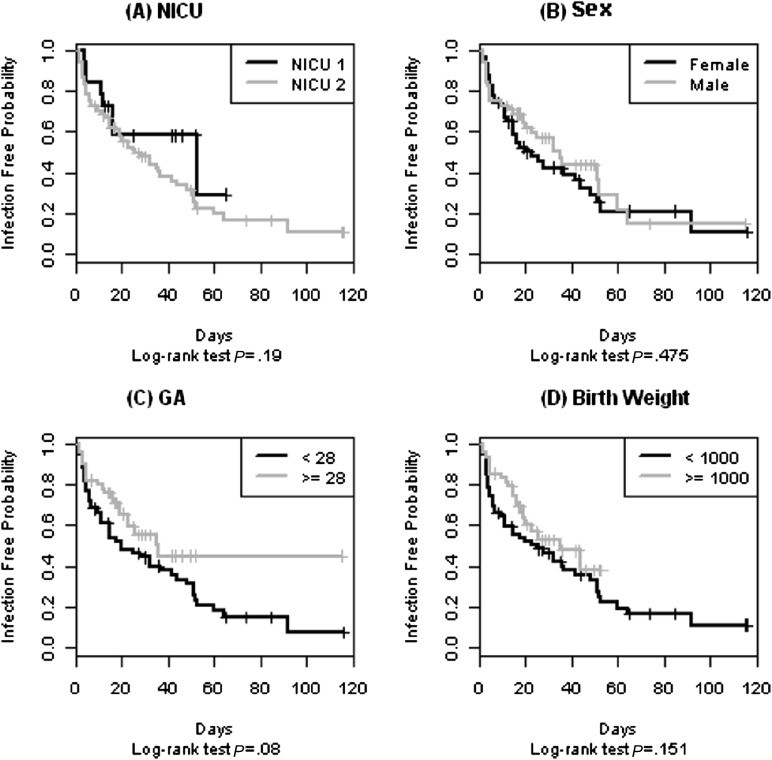
Kaplan-Meier curves were created reflecting location, sex, GA, and birth weight in order to identify potential predictors of infection. The rate for RVIs was similar between the 2 NICUs (5 of 11 from NICU 1, and 21 of 39 from NICU 2, P = .74). The Kaplan-Meier curves comparing each location for sex, birth weights, or GA were not significantly different statistically (Figure 2; available at www.jpeds.com), and the data from each NICU, therefore, were aggregated for comparison of infected and uninfected infants.
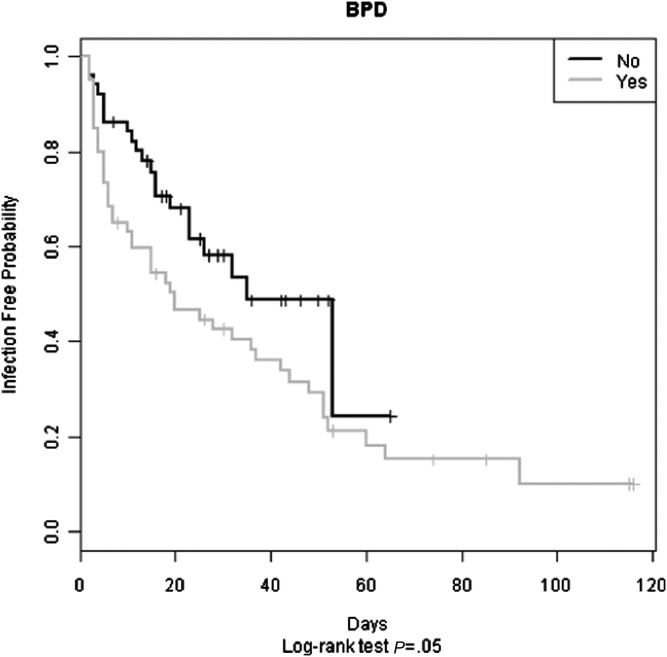
Clinical comparisons between infected and uninfected infants are shown in Table I . Infected infants compared with uninfected infants had a longer average length of stay (70 days vs 35 days, P = .002), need for intubation (17 of 26 infected infants vs 7 of 24 uninfected infants, P = .01), average duration of intubation (19 days vs 5 days, P = .03), and duration of supplemental oxygen requirement (51 days vs 13 days, P = .002). Nineteen of the 26 infected infants required supplemental oxygen at some point during their hospitalization, compared with 9 of the 24 uninfected infants (P = .006). Seventeen infants required oxygen at an adjusted GA of 36 weeks (the criteria for diagnosis of BPD); 12 of the 17 were among the virus-infected infants and the remaining 5 were uninfected. The probability of acquiring infection was significantly higher for infants diagnosed with BPD (P < .05; Figure 3; available at www.jpeds.com).
Table I.
Clinical comparison of virus-infected and uninfected infants
| Infected n = 26 | Infection-free n = 24 | P value | |
|---|---|---|---|
| Clinical characteristics | |||
| GA (mean) | 28.0 wk | 29.4 wk | .10 |
| Birth weight (mean) | 1213 g | 1441 g | .30 |
| Average length of stay | 70 d | 35 d | .002∗ |
| Average duration of intubation | 19 d | 5 d | .03∗ |
| Supplemental oxygen | n = 19 (73%) | n = 9 (38%) | .02∗ |
| Average duration of oxygen use | 51 d | 13 d | .002∗ |
| BPD (O2 at 36 wk) | n = 12 (46%) | n = 5 (21%) | .05∗ |
| Clinical events | |||
| Apnea (mean) | 0.19 | 0.38 | .0015∗ |
| Bradycardia (mean) | 1.37 | 1.32 | .74 |
| Desaturation (mean) | 7.09 | 3.90 | <.0001∗ |
| Clinical deteriorations | 38 | 8 | .0001∗ |
P ≤ .05 calculated by unpaired t test.
Supplemental oxygen requirements also were higher in the infected cohort. We identified only a single timepoint when 1 uninfected infant required an inhaled concentration of oxygen above 50%, an event that occurred at 36 separate timepoints in the infected group.
A Cox proportional hazards model showed modestly significant effects of GA after adjusting for the effect of NICU units and sex (Table II; available at www.jpeds.com). At each NICU, an infant with lower GA was more likely to be infected. The effect of birth weight in the Cox model was reversed compared with the marginal effect seen in Kaplan-Meier analysis, but 1 child with massive hydrocephalus had a very high birth weight for GA, which skewed the model. When this outlier was removed, the data points tended to cluster with no clear trend (data not shown).
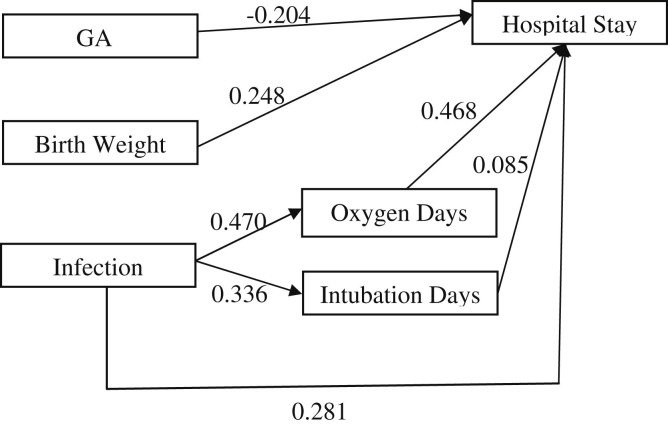
We proposed a path model to determine whether virus infection directly extended length of hospital stay or whether this effect was mediated by the need for intubation and oxygen use. The model was confirmed in SAS using covariance analysis of linear structural equations. The effect of RVI on length of stay appeared to be mediated partially through effects on the respiratory system, as there were significant standardized indirect effects of infection on length of stay (P = .001). When 2 outliers were excluded (1 infant who died on day of life 1, another who was discharged to an outlying hospital and lost to follow-up), infection was significantly correlated to length of stay through both direct (P < .003) and indirect (P < .0005) effects (Figure 4; available at www.jpeds.com).
Table I shows clinical events in infected and uninfected infants. On average, infected infants had nearly double the number of desaturation events compared with the uninfected cohort (7.1 episodes/d vs 3.9 episodes/d, P < .0001). Episodes of bradycardia were the same between the 2 groups, and there were significantly fewer apnea events among infected infants. This latter finding may have been due to the confounding factor that infected infants were more likely being mechanically ventilated, which precluded apnea.
Most infants were evaluated for bacterial infection at the time of birth, and again later at the discretion of the clinical team. A total of 118 blood cultures were obtained from the 50 study patients. Significantly more cultures were obtained from the virus-infected infants than from virus-uninfected infants (70 vs 38, P = .008). Eleven cultures were positive for bacteria from 6 of the virus-infected infants compared with 6 positive bacterial cultures from 4 of the virus-uninfected infants (23.1% of virus-infected infants had a positive culture, compared with 16.7% of virus-uninfected infants (P = .73 by Fisher exact test). Of the 11 positive bacterial cultures in infants infected with a viral pathogen, some were repeatedly positive for the same organism. In addition, 1 virus-infected infant had 2 separate blood cultures positive for coagulase-negative Staphylococcus and Klebsiella, and another had 3 separate cultures positive for Klebsiella sp, MRSA, and Candida sp. The 6 positive blood cultures from infants who never had a virus detected occurred in 4 infants, with 2 sets being repeatedly positive for Staphylococcus epidermidis. All clinical deteriorations and clinical events noted in study patients were reviewed, and changes in respiratory support were associated with coincident oxygen desaturation events. Compared with virus-infected infants, uninfected infants displayed few clinical deteriorations beyond the first few days of life; 38 clinical deteriorations occurred in 26 infected infants vs 8 clinical deteriorations in 24 uninfected infants. During 27 (71%) clinical deteriorations, RVI was detected simultaneously. All 14 episodes of sequential detections of RVIs were associated with clinical deteriorations. Additionally, 7 of the 11 positive blood cultures in the virus-infected group were associated with deteriorations. Specific details for each neonate with RVI detections are shown in Table III (available at www.jpeds.com).
Discussion
We documented unsuspected and clinically unrecognized RVIs among premature neonates during their birth hospitalizations. The detection of viral nucleic acid from the respiratory tract of asymptomatic or minimally symptomatic infants (none of the infants were evaluated for RVI by the NICU clinicians) raises the question of whether these events represent true infection. In the absence of data documenting seroconversion, our observation documenting 14 instances of prolonged serial detection suggest ongoing virus replication rather than transient carriage. Moreover, of the viruses included in the detection panel, only adenovirus is known to persist in the nasopharynx, although respiratory viruses have been detected in asymptomatic older children. Detection of viral nucleic acids in nasopharyngeal secretions in our study correlated significantly and directly with several specific negative outcomes, raising the possibility of a causal relationship. Additionally, our findings suggest the need for enhanced virus surveillance and optimized infection control.
Although outbreaks of RVIs in NICUs have been described, this study confirms the importance of systematic surveillance in detecting infections that otherwise would be unrecognized. Premature neonates with RVIs can display atypical symptoms or can have no overt, recognizable symptoms. However, the detection of RVIs within a NICU can have profound clinical implications. Infants with detectable RVIs, even those without overt symptoms, required more supplemental oxygen, had a high likelihood of mechanical ventilation, required longer durations of oxygenation, and were hospitalized longer. Persistent detection of virus was associated with clinical deteriorations. In addition, there was a higher rate of BPD in the virus-infected population, an observation worthy of further study. The expression and release of pro-inflammatory cytokines in the lung have been implicated in the etiology of BPD,11 in association with chorioamnionitis,12 and prolonged mechanical ventilation.13, 14 Nosocomial RVIs may exacerbate inflammation attributable to positive pressure ventilation, prematurity, and/or supplemental oxygen therapy, and may contribute to the development of chronic lung disease of prematurity. The effect of RVI on length of stay appeared to be mediated through effects on the respiratory system. Path analysis and linear regression analysis of our data showed significant direct and indirect effects of infection on length of stay.
Prolonged hospitalization is a risk-factor for nosocomial infection, supported by the finding in our study that the average length of time until first detecting an RVI was 24 days. Pre-existing lung disease may predispose infants to infection, as endotracheal intubation and feeding tubes (both markers of clinically compromised infants) have been previously identified as risk factors for acquisition of RVI.15 Additionally, multiple interventions by nursery and respiratory therapy personnel may increase opportunities for acquisition.
A limitation of our study is that it only covered 1 calendar year and a relatively small number of neonates. The potential for cross-contamination of specimens was limited by collection of samples in separate sealed containers using universal precautions. Laboratory contamination was limited by using dedicated, trained personnel and strict sample identification identical to that employed for our hospital’s clinical laboratory. Sample containers remained sealed from collection until laboratory RNA extraction. To ensure a consistent sample set throughout the year, the collection schedule was adhered to as much as reasonably practical with exceptions made only for times when an infant could not be tested safely, and repeated attempts were made as soon as possible. There were no weeks when specimen collection did not occur. A limitation of our study is the difficulty in proving that detection of an RVI is due to ongoing viral replication. Seroconversion data might support this supposition, but this testing was not performed. In addition, the association between detection of an RVI and prolonged hospitalization, increased requirements for oxygenation and respiratory support, and a higher rate of BPD does not prove causation.
We documented transmission of respiratory pathogens to premature neonates during their birth hospitalization despite presumed vigilance related to infection control practices in these high-risk settings. These practices included the use of barriers (gowns and gloves), hand washing before and after each patient contact, the use of masks for anyone with respiratory symptoms, and the exclusion of all children. During this study, we did not explore the sources of infection; however, most of the infants had contact only with their parents and the healthcare personnel. We noted that several twin infants had identical viruses detected at the same time, despite being in separate nursing areas. Our findings highlight the limitations of current infection control practices and raise questions as to whether the presence or sequelae of these infections justify more intensive monitoring of infections and assessment of strategies of prevention and control.
Footnotes
Funded by the Children’s Miracle Network of New York (to J.D. and N.B.) and the National Institute of Allergy and Infectious Diseases, Division of Intramural Research (Z01-AI000943 to H.R.). The authors declare no conflicts of interest.
Appendix.
Table II.
Results from the Cox regression model
| Variable | Risk ratio | P value |
|---|---|---|
| NICU | 1.4645 | .389 |
| Sex (male) | 0.8466 | .558 |
| GA (wk) | 0.8524 | .046 |
| Birth weight (g) | 1.0006 | .036 |
Table III.
Unique data on infected infants and viruses detected
| Study ID | NICU | GA | Virus(es) | Deteriorations total | RVI at time of event | Bacterial infection at time of event | Days of O2 | BPD |
|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 31 | hMPV, EV/RV | 0 | 0 | 0 | 0 | No |
| 2 | 1 | 26 | hMPV∗, EV/RV | 1 | 1 | 1 | 64 | No |
| 7 | 1 | 32 | PIV2, PIV3 | 0 | 0 | 0 | 0 | No |
| 8 | 1 | 32 | PIV2, PIV3 | 0 | 0 | 0 | 0 | No |
| 9 | 1 | 32 | PIV2, PIV3 | 0 | 0 | 0 | 9 | No |
| 13 | 2 | 32 | hMPV, EV/RV | 0 | 0 | 0 | 0 | No |
| 15 | 2 | 27 | RSV A∗, RSV B, PIV3, | 1 | 1 | 0 | 145 | Yes |
| 16 | 2 | 25 | RSV A, EV/RV | 2 | 2 | 0 | 65 | No |
| 17 | 2 | 25 | RSV B∗, PIV3∗, Flu B | 3 | 2 | 0 | 73 | Yes |
| 19 | 2 | 25 | PIV2, PIV3 | 3 | 2 | 2 | 75 | Yes |
| 20 | 2 | 31 | RSV A | 1 | 1 | 0 | 4 | No |
| 21 | 2 | 31 | hMPV, EV/RV | 0 | 0 | 0 | 0 | No |
| 23 | 2 | 24 | RSV B∗, PIV2, PIV3 | 3 | 2 | 0 | 106 | Yes |
| 24 | 2 | 24 | RSV B∗, hMPV∗, PIV2, PIV3, EV/RV∗ | 3 | 3 | 0 | 121 | Yes |
| 25 | 2 | 24 | RSV B∗ | 2 | 2 | 0 | 86 | Yes |
| 27 | 2 | 24 | RSV A, RSV B | 4 | 2 | 1 | 93 | Yes |
| 28 | 2 | 29 | Flu B, PIV3, hMPV∗, RSV A | 2 | 2 | 0 | 45 | Yes |
| 29 | 2 | 27 | RSV A | 0 | 0 | 0 | 1 (Died) | No |
| 30 | 2 | 30 | RSV A, hMPV | 0 | 0 | 0 | 0 | No |
| 31 | 2 | 31 | PIV2, PIV3 | 1 | 1 | 0 | 0 | No |
| 37 | 2 | 28 | Flu B, PIV3 | 1 | 1 | 0 | 26 | No |
| 38 | 2 | 27 | RSV B, Flu B, PIV3 | 1 | 1 | 0 | 133 | Yes |
| 39 | 2 | 26 | RSV B∗ | 2 | 1 | 0 | 70 | Yes |
| 41 | 2 | 32 | PIV3, EV/RV∗ | 1 | 1 | 1 | 2 | No |
| 43 | 2 | 25 | hMPV∗ | 3 | 1 | 2 | 69 | Yes |
| 44 | 2 | 29 | hMPV∗ | 4 | 1 | 0 | 130 | Yes |
EV/RV, enterovirus/rotavirus.
Sequential detection of the same virus. Some deterioration events were temporally associated with both RVI and a positive bacterial culture.
Figure 2.
Probability of remaining free of viral infection over time was not significantly different based on: A, location, B, sex, C, GA above or below 28 weeks, and D, birth weight above or below 1000 g. P values calculated by Log-rank test.
Figure 3.
Infants with a diagnosis of BPD at 36 weeks (labeled as “Yes”) had a greater probability of acquiring viral infection compared with infants without BPD (labeled as “No”). P values calculated by Log-rank test.
Figure 4.
Path analysis of the effects of viral infection after adjusting for other possible confounders on length of stay for 48 infants (excluding 2 outliers). Numbers represent linear path coefficients. The covariance and random error terms are not shown.
References
- 1.Diniz E.M., Vieira R.A., Ceccon M.E., Ishida M.A., Vaz F.A. Incidence of respiratory viruses in preterm infants submitted to mechanical ventilation. Rev Inst Med Trop (Sao Paulo) 2005;47:37–44. doi: 10.1590/s0036-46652005000100007. [DOI] [PubMed] [Google Scholar]
- 2.Gagneur A., Sizun J., Vallet S., Legr M.C., Picard B., Talbot P.J. Coronavirus-related nosocomial viral respiratory infections in a neonatal and pediatric intensive care unit: a prospective study. J Hosp Infect. 2002;51:59–64. doi: 10.1053/jhin.2002.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cunney R.J., Bialachowski A., Thornley D., Smaill F.M., Pennie R.A. An outbreak of influenza A in a neonatal intensive care unit. Infect Control Hosp Epidemiol. 2000;21:449–454. doi: 10.1086/501786. [DOI] [PubMed] [Google Scholar]
- 4.Halasa N.B., Williams J.V., Wilson G.J., Walsh W.F., Schaffner W., Wright P.F. Medical and economic impact of a respiratory syncytial virus outbreak in a neonatal intensive care unit. Pediatr Infect Dis J. 2005;24:1040–1044. doi: 10.1097/01.inf.0000190027.59795.ac. [DOI] [PubMed] [Google Scholar]
- 5.Singh-Naz N., Willy M., Riggs N. Outbreak of parainfluenza virus type 3 in a neonatal nursery. Pediatr Infect Dis J. 1990;9:31–33. doi: 10.1097/00006454-199001000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Singh-Naz N., Brown M., Ganeshananthan M. Nosocomial adenovirus infection: molecular epidemiology of an outbreak. Pediatr Infect Dis J. 1993;12:922–925. [PubMed] [Google Scholar]
- 7.Faden H., Wynn R.J., Campagna L., Ryan R.M. Outbreak of adenovirus type 30 in a neonatal intensive care unit. J Pediatr. 2005;146:523–527. doi: 10.1016/j.jpeds.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 8.Forster J., Schumacher R.F. The clinical picture presented by premature neonates infected with the respiratory syncytial virus. Eur J Pediatr. 1995;154:901–905. doi: 10.1007/BF01957502. [DOI] [PubMed] [Google Scholar]
- 9.Hall C.B., Kopelman A.E., Douglas R.G., Jr., Geiman J.M., Meagher M.P. Neonatal respiratory syncytial virus infection. N Engl J Med. 1979;300:393–396. doi: 10.1056/NEJM197902223000803. [DOI] [PubMed] [Google Scholar]
- 10.Vieira R.A., Diniz E.M., Vaz F.A. Clinical and laboratory study of newborns with lower respiratory tract infection due to respiratory viruses. J Matern Fetal Neonatal Med. 2003;13:341–350. doi: 10.1080/jmf.13.5.341.350. [DOI] [PubMed] [Google Scholar]
- 11.Ambalavanan N., Carlo W.A., D’Angio C.T., McDonald S.A., Das A., Schendel D. Cytokines associated with bronchopulmonary dysplasia or death in extremely low birth weight infants. Pediatrics. 2009;123:1132–1141. doi: 10.1542/peds.2008-0526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paananen R., Husa A.K., Vuolteenaho R., Herva R., Kaukola T., Hallman M. Blood cytokines during the perinatal period in very preterm infants: relationship of inflammatory response and bronchopulmonary dysplasia. J Pediatr. 2009;154:39–43. doi: 10.1016/j.jpeds.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 13.Huang H.C., Yang M.Y., Huang C.B., Yang K.D. Profiles of inflammatory cytokines in bronchoalveolar lavage fluid from premature infants with respiratory distress disease. J Microbiol Immunol Infect. 2000;33:19–24. [PubMed] [Google Scholar]
- 14.Corso A.L., Pitrez P.M., Machado D.C., Stein R.T., Jones M.H. TNF-alpha and IL-10 levels in tracheobronchial lavage of ventilated preterm infants and subsequent lung function. Braz J Med Biol Res. 2007;40:569–576. doi: 10.1590/s0100-879x2007000400016. [DOI] [PubMed] [Google Scholar]
- 15.Valenti W.M., Clarke T.A., Hall C.B., Menegus M.A., Shapiro D.L. Concurrent outbreaks of rhinovirus and respiratory syncytial virus in an intensive care nursery: epidemiology and associated risk factors. J Pediatr. 1982;100:722–726. doi: 10.1016/s0022-3476(82)80571-4. [DOI] [PubMed] [Google Scholar]