Abstract
OBJECTIVE
To examine the relationship of depression and survival of patients with chronic heart failure (HF) over a 12-year follow-up period.
BACKGROUND
The survival associated with depression has been demonstrated in HF patients for up to 7 years. Longer-term impact of depression on survival of these patients remains unknown.
METHODS
Prospectively conducted observational study examining adult HF patients who were admitted to a cardiology service at Duke University Medical Center between March 1997 and June 2003 and completed the Beck Depression Inventory (BDI) scale. The National Death Index was queried for vital status. Cox proportional hazards modeling was used to determine association of survival and depression.
RESULTS
During a mean follow-up of 1792.33±1372.82 days (median 1600; range 0–4683), 733 of 985 HF participants died of all causes, representing 80% of those with depression (BDI>10) and 73% of those without (p=0.01). Depression was significantly and persistently associated with decreased survival over follow-up (Hazard Ratio [HR] 1.35, 95% Confidence Interval [CI] 1.15–1.57) and was independent of conventional risk factors (HR 1.40, 95% CI 1.16–1.68). Furthermore, survival was inversely associated with depression severity (BDIcontinuous HR 1.02, 95% CI 1.006–1.025, p=0.001).
CONCLUSION
The impact of co-morbid depression during index hospitalization on significantly increased mortality of HF patients is strong and persists over12 years. These findings suggest that more investigation is needed to understand the trajectory of depression and the mechanisms underlying the impact of depression as well as to identify effective management strategies for depression of patients with HF.
Keywords: depression, cardiovascular disease, chronic disease, epidemiology
BACKGROUND
Chronic heart failure (HF) is a highly prevalent and costly disease in the U.S. Approximately 5.8 million individuals are affected in the United States, with 670,000 new cases diagnosed each year and an incidence rate of 10 per 1000 after the age of 65. Nearly 300,000 will die of HF annually and 20% die within one year of diagnosis [1]. Five-year mortality in heart failure remains high (59% in men, 45% in women) despite advances in interventions. The cost for HF has been increasing and is estimated at 39.2 billion annually [1].
More than 20% of HF patients suffer from depression [2]. Abundant evidence demonstrates a strong relationship between depression and HF [2–10]. These patients experience 2 to 3-times higher morbidity and mortality in the years following depression detection than their non-depressed counterparts [2, 8, 11]. The additional effect of depression on poor outcomes in heart failure has been demonstrated in many studies over periods from six months to seven years [6, 8, 9, 11]. With few individuals surviving past seven years and half expected to die within five, we set out to determine the association between baseline measures of depression among individuals hospitalized with HF beyond that timeline. The association of depression and survival over a 2.5 year period in this cohort was presented in 2001 [8].
METHODS
Participants
Study participants were adult patients with cardiac disease and history of HF, ages 18 years or older, who were admitted to a university-based cardiology service between March 1997 and June 2003. Eligible patients were those whose New York Heart Association (NYHA) class of HF were II or greater; who had an ejection fraction (EF) 35% or less by angiography, echocardiography, or radionuclide study; or both, and recruited consecutively following the index admission. Patients were excluded if they were pregnant, had active suicidal ideation, had planned major surgery, or were unable to provide informed consent. All study activities were approved by the institutional review board and all participants provided informed consent.
Study Variables at baseline
During the index hospitalization, all participants completed the Beck Depression Inventory (BDI). This is a self-administered, 21-item questionnaire used to screen for depression and assess the severity of depression [12]. Clinically significant depression for this study was defined as a total BDI score of ≥10. This cut-off has demonstrated diagnostic [13] and prognostic validity [4, 6–8, 14, 15]. Demographic data including age, gender, race (white vs. other), and marital status; heart failure status including EF, etiology of heart failure (ischemic vs. non-ischemic), history of coronary artery bypass graft (CABG), history of myocardial infarction (MI), and NYHA class (II vs. III/IV) were collected. Other clinical indicators included reason for index admission, diabetes status, use of selective serotonin reuptake inhibitors (SSRIs), and use of other antidepressants.
Survival Information
The National Death Index (NDI) was queried to identify the vital status of participants. The query was completed on December 29, 2009. September 19, 2009 was the date of the last death captured via the search.
Statistical Analyses
Summary statistics expressed as percentages, means, and standard deviations were used to describe demographic and clinical characteristics of participants. Bivariate associations of covariates among those without versus with clinically significant depression (BDI score <10 and ≥10, respectively) and alive versus dead were assessed using Χ2 tests for categorical and t-tests for continuous variables. Cox proportional hazards modeling was used to determine the association of depression (BDI <10 vs. BDI ≥ 10) with survival. Dose effect of depression, using BDI first as a continuous then an incrementally categorical measure (BDI scores <5, 5–9, 10–18, and ≥19) [11], on survival was also evaluated by the Cox proportional hazards model. Depressive symptoms (cognitive/affective vs. somatic/affective) [16] were assessed in the same way using the respective BDI subscales. The independent association of depression with survival was assessed in a multivariate model by adjusting for variables that were previously utilized and are recognized as common risk factors of HF prognosis [11], including age, sex, race, marital status, NYHA class, ischemic etiology of HF, history of CABG, and diagnosis of diabetes.
RESULTS
The study population consisted of 985 HF patients who provided consent. During a mean follow up of 1792.33±1372.82 days (median 1600; range 0–4683), 733 (74.4%) of the cohort patients died. Descriptive analyses of the overall study population and by depression status are given in table 1.
Table 1.
Baseline characteristics of sample overall and by depression status
| Total Sample | BDI<10 | BDI≥10 | ||
|---|---|---|---|---|
| Characteristic | Mean (SD) or N (%) | Mean (SD) or N (%) | Mean (SD) or N (%) | p-value* |
| BDI | 8.27 (7.07) | 4.68 (2.59) | 16.58 (7.16) | |
| Age | 69.07 (10.60) | 69.54 (10.17) | 67.99 (7.16) | 0.05 |
| Gender | 0.5 | |||
| Female | 368 (37.78) | 252 (37.06) | 116 (39.46) | |
| Male | 606 (62.22) | 428 (62.94) | 178 (60.54) | |
| Race | 0.7 | |||
| White | 708 (72.69) | 492 (72.35) | 216 (73.47) | |
| Other | 266 (27.31) | 188 (27.65) | 78 (26.53) | |
| Marital status | <0.001 | |||
| Married | 400 (43.96) | 312 (48.45) | 88 (32.08) | |
| Not married | 510 (56.04) | 332 (51.55) | 178 (66.92) | |
| Ejection fraction | 30.51 (12.27) | 30.84 (12.03) | 29.74 (12.79) | 0.08 |
| HF etiology | 0.3 | |||
| Ischemic | 597 (61.29) | 256 (37.65) | 121 (41.16) | |
| Non-ischemic | 377 (38.71) | 424 (62.35) | 173 (58.84) | |
| History of CABG | 0.01 | |||
| Yes | 396 (46.86) | 295 (50.26) | 104 (40.31) | |
| No | 449 (53.14) | 292 (49.74) | 154 (59.69) | |
| History of MI | 1.0 | |||
| Yes | 352 (41.66) | 243 (41.61) | 109 (41.76) | |
| No | 493 (58.34) | 341 (58.39) | 152 (58.24) | |
| NYHA score | 0.007 | |||
| <3 | 658 (67.35) | 241 (35.34) | 78 (26.44) | |
| 3 or 4 | 319 (32.65) | 441 (64.66) | 217 (73.56) | |
| Reason for admission | 0.02 | |||
| Chest pain | 186 (19.10) | 136 (20.00) | 50 (17.01) | |
| MI | 137 (14.07) | 100 (14.71) | 37 (12.59) | |
| Worsening HF | 340 (34.91) | 214 (31.47) | 126 (42.86) | |
| Arrhythmia | 97 (9.96) | 71 (10.44) | 26 (8.84) | |
| Other | 214 21.97 | 159 (23.38) | 55 (18.71) | |
| Diabetic | 0.8 | |||
| Yes | 412 (42.08) | 286 (41.81) | 126 (42.71) | |
| No | 567 (57.92) | 398 (58.19) | 169 (57.29) | |
| Taking SSRI | <0.001 | |||
| Yes | 135 (14.09) | 72 (10.76) | 63 (21.80) | |
| No | 824 (85.91) | 597 (89.24) | 226 (78.20) | |
| Other antidepressant | 0.03 | |||
| Yes | 12 (1.25) | 5 (0.75) | 7 (2.42) | |
| No | 946 (98.75) | 664 (99.25) | 282 (97.58) |
Precision of test statistic: chi-square for categorical variables or t-test for continuous variables.
Overall, 295 (30.13%) scored ≥10 on the BDI, indicating clinically significant baseline depression. The depressed and not depressed groups were similar with regards to gender, race, EF, ischemic etiology of HF, history of MI, and diagnosis of diabetes. Those who were depressed were significantly younger (67.99 vs. 69.54 years, p=0.05), more likely to be unmarried (66.92 vs. 51.55%, p<0.001), had greater NYHA class score (class III/IV: 73.56 vs. 64.66%, p=0.007), and had undergone fewer CABG procedures (40.31 vs. 50.26%, p=0.01). As expected, greater proportions of depressed individuals were prescribed SSRIs (21.80 vs. 10.76%, p<0.001) and other antidepressants (2.42 vs. 0.75%, p=0.03) than non-depressed.
Eighty percent of those with depression at baseline (BDI ≥ 10) and 73% of those without depression were deceased at follow-up (p=0.01). The patients who died had notably shorter duration of follow up (mean 974.0±1035.52 days, median 1229) than those who remained alive (mean 3460.97±753.17 days, median 3255). Those who died were also older (70.64 vs. 64.40 years, p<0.001) and had higher BDI scores (mean 8.62 vs. 7.21; p=0.01). In terms of cardiac history, they were more likely to have had HF due to ischemic etiology (65.02 vs. 50.20%, p<0.001), a history of CABG (50.15 vs. 35.90%, p<0.001), greater EF (>20; 30.68 vs. 23.27%, p=0.03), and a NYHA class III/IV (70.77 vs. 57.14%, p<0.001). They were more likely to be diabetic (45.23 vs. 32.52%, p<0.001). Baseline SSRI use was similar between those who died and survived (14.43 vs. 13.11%, p=0.6). Only 12 patients used non-SSRI antidepressants at baseline and a non-significantly higher proportion was found among the deceased (1.54% vs. 0.41%, p=0.17).
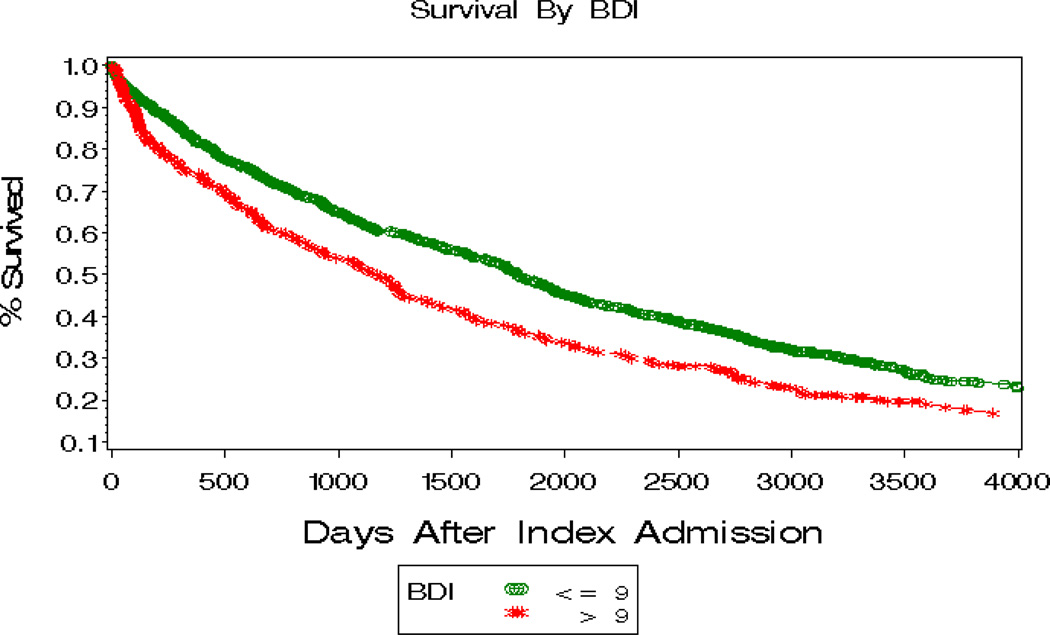
In bivariate analysis (Table 2), survival was most strongly associated with age, demonstrating a 4% increased risk for mortality with each 1-year increase in age (HR 1.04, 95% CI 1.03–1.04, p<0.001). This was followed by the NYHA class III/IV (HR 1.45, 95% CI 1.23–1.70, p<0.001), ischemic etiology of HF (HR 1.40, 95% CI 1.20–1.63, p<0.001), history of CABG (HR 1.38, 95% CI 1.18–1.61, p<0.001) and a diagnosis of diabetes (HR 1.32, 95% CI 1.14–1.52, p<0.001). Depression was significantly associated with decreased survival (HR 1.35, 95% CI 1.15–1.57, p<0.001; figure 2). Baseline EF (p=0.05) and marital status (p=0.06) were not significantly associated with mortality risk but were included in the multivariate analysis since they were identified a priori as meaningful covariates and included in previous survival analysis [8]. After adjusting for these variables (see table 2) depression (BDI<10 vs. BDI ≥10) remained highly and significantly associated with decreased survival (HR 1.40, 95% CI 1.16–1.68, p<0.001). Age, NYHA class, history of CABG, and diabetes diagnosis remained independently associated with decreased survival in the multivariate analysis.
Table 2.
Relationship of baseline characteristics to 12-year mortality during follow up period
| Univariate |
Multivariate |
|||||
|---|---|---|---|---|---|---|
| Variable | Chi-Square | HR (95% CI) | p-value | Chi-square | HR (95% CI) | p-value |
| Age | 80.26 | 1.04 (1.03–1.04) | <0.001 | 64.74 | 1.04 (1.03–1.05) | <0.001 |
| NYHA score | 20.57 | 1.45 (1.23–1.70) | <0.001 | 6.93 | 1.28 (1.07–1.55) | 0.01 |
| HF etiology | 18.85 | 1.40 (1.20–1.63) | <0.001 | 1.36 | 1.13 (0.92–1.39) | 0.2 |
| History of CABG | 16.47 | 1.38 (1.18–1.61) | <0.001 | 5.85 | 1.26 (1.05–1.52) | 0.02 |
| BDI ≥ 10 | 13.95 | 1.35 (1.15–1.57) | <0.001 | 12.77 | 1.40 (1.16–1.68) | <0.001 |
| Diabetes | 13.70 | 1.32 (1.14–1.52) | <0.001 | 10.57 | 1.32 (1.12–1.57) | 0.001 |
| Ejection fraction | 3.77 | 0.99 (0.99–1.00) | 0.05 | 13.22 | 0.99 (0.98–0.99) | <0.001 |
| Marital status | 3.50 | 0.86 (0.74–1.01) | 0.06 | 1.41 | 0.90 (0.75–1.07) | 0.2 |
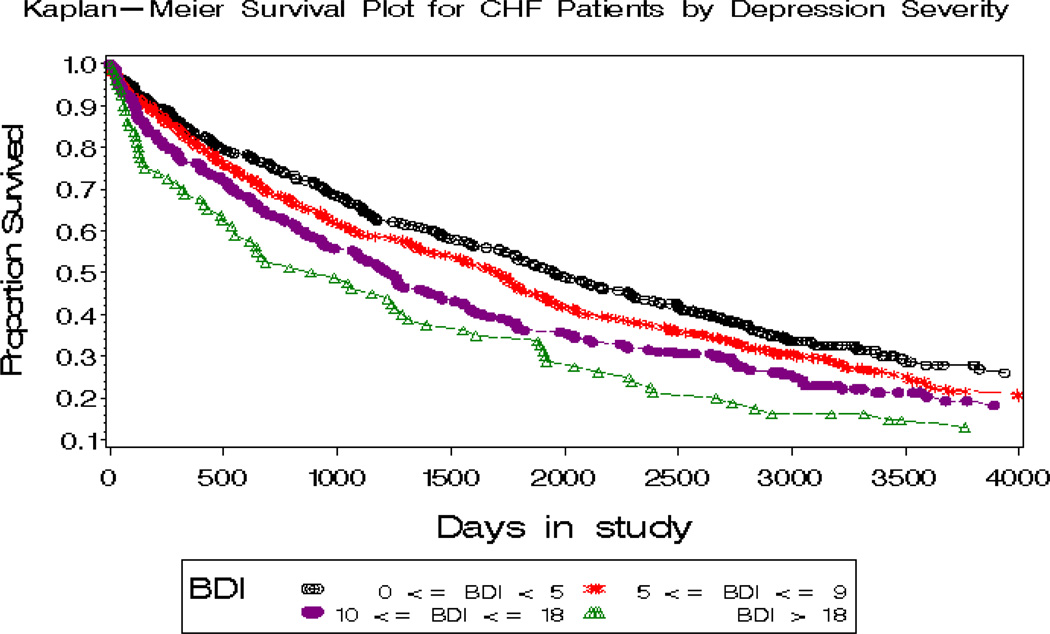
Figure 2.
Kaplan-Meier plots of survival for HF patients by depression severity
Cox Proportional analyses for the association of depression severity using BDI as continuous and categorical measure with survival demonstrate a significant dose effect of depression on increased mortality. BDI sub-scale analysis [16] revealed a significant association between survival and somatic/affective symptoms but no significant association between survival and cognitive/affective symptoms. Results of the relationship of BDI as dichotomous, categorical, continuous, and subscale scores with mortality, both unadjusted and adjusted for risk factors, are given in table 3. Kaplan Meyer survival curves for depression (BDI <10 vs. ≥10) and depression severity (categorical BDI) are shown in figures 1 and 2, respectively.
Table 3.
Relationship of BDI score with 12-year mortality during follow up period
| BDI | Unadjusted |
Adjusted* |
||||
|---|---|---|---|---|---|---|
| Chi-Square | HR (95% CI) | p-value | Chi-square | HR (95% CI) | p-value | |
| Categorical | ||||||
| <5 | -- | -- | -- | -- | -- | -- |
| 5–9 | 2.11 | 1.14 (0.96–1.36) | 0.14 | 0.06 | 1.03 (0.84–1.26) | 0.80 |
| 10–18 | 7.86 | 1.33(1.09–1.63) | 0.005 | 3.15 | 1.24 (0.98–1.58) | 0.08 |
| >18 | 14.49 | 1.69 (1.29–2.21) | <0.001 | 19.9 | 2.02 (1.48–2.76) | <0.001 |
| Continuous | 10.58 | 1.02 (1.01–1.03) | 0.001 | 13.01 | 1.02 (1.01–1.03) | <0.001 |
| Subscales | ||||||
| Cognitive/affective | 0.0005 | 1.00 (0.97–1.03) | 0.98 | 2.08 | 1.02 (0.99–1.05) | 0.15 |
| Somatic/affective | 15.68 | 1.03 (1.02–1.05) | <0.001 | 15.42 | 1.04 (1.02–1.06) | <0.001 |
Adjusted for age, ejection fraction, history of CABG, ischemic etiology of heart failure, NYHA score, diagnosis of diabetes, and marital status.
Figure 1.
Kaplan-Meier plots of survival for HF patients with a BDI ≥ 10 vs. BDI < 10
DISCUSSION
Our results demonstrate that among individuals with HF, depressive symptoms measured at one point in time significantly and substantially impact long-term survival. The results imply that a HF patient with clinically significant depressive symptoms (BDI ≥10) may have approximately 40% higher chance to die at any time over a 12-year period than HF patients without the depression. This finding is unique to the current literature in the duration of this effect: up to 12 years. This depression-related decreased survival is independent of clinical features and pertinent demographic characteristics, such as age, NYHA class, HF etiology, history of CABG, diabetes, ejection fraction, and marital status. Not surprisingly, age was most strongly associated with mortality in the current study population; however, depression was a stronger predictor than NYHA class, history of CABG, and diabetes diagnosis. This is consistent with the mortality analysis at 2.5 years in the same cohort [11]. The association between EF and survival appears reduced over time (Chi-square at 2.5 years: 9.40 and 17.35 on univariate and multivariate analyses, respectively [11]; present study: 3.77 and 13.22). In contrast, the association between BDI and survival increased (Chi-square at 2.5 years: 13.96 and 8.92 [11]; present study: 13.95 and 12.77). This shift can be understood from a clinical perspective in that improved medical management among patients with low EF could have diminished its impact on mortality while depressed individuals are less likely to receive such medical management, rehabilitation and necessary interventions [3]. Further, similar efforts to treat depression in those with HF do not seem to positively impact mortality outcomes despite improvement in symptoms [17–19].
Previously, increased mortality among depressed heart failure patients has been demonstrated in various study populations and over follow up as great as 7 years. Depression has been associated with decreased survival in heart failure patients in one study of over 90 days [3] and another study up to an average of 986 days [20]. Other studies have shown that depression was associated with increased mortality in HF patients with atrial fibrillation over three years [6] and in non-ischemic HF patients over five years [5]. In a six-year follow up study, Johansson and colleagues found that depressive symptoms trebled the risk of cardiovascular mortality and more than doubled all-cause mortality in HF patients over six years [9]. In perhaps the most appealing finding, Junger and colleagues found that the risk of mortality in heart failure conferred by depression is not only elevated compared with no depression but continues to increase over time (30 months) to achieve a HR of 8.0 [10].
Notable in these studies and in our own findings is that depression measured at one point in time continues to be associated with mortality over time. Important questions for investigation are why baseline depression remains such a strong predictor of mortality over increasingly longer follow up periods, even more so than traditional risk factors; and what impact remission or recurrence of depression might have over the course of HF. One possible explanation for the current findings is that medical management for cardiovascular disease has improved at a faster pace than the management of depression. Decreased use of HF management programs by depressed individuals may further widen the survival gap [3].
Further investigation is needed to understand potential mediators of mortality in HF for which depression may be marker or a cause. Severity of depression may fluctuate over time but depressive symptoms measured once may reflect certain psychosocial factors that persist beyond a single depressive episode, contributing to a low likelihood of depression remission, or predisposing an individual to experience a recurrent depression episode. These may include maladaptive coping strategies [21], poor mood repair responses [22], and social isolation [7]. Health behaviors such as inactivity [7, 23], engagement in outpatient disease management programs [3], and exposure to cardiac interventions [3] also mediate the effects of depression on mortality. The current study demonstrates that those with depression underwent significantly fewer bypass procedures despite having similar coronary artery disease risk profiles (i.e. ischemic etiology and diabetes diagnosis). Decreased medication adherence among depressed individuals with HF, while not yet studied, is also likely a factor given findings in other chronic and cardiac diseases [24, 25]. This evidence suggests that the depressed patients could benefit from available medical interventions as well as their non-depressed counterparts if their depression could be successfully treated, thereby allowing appropriate access to care.
Our findings have remarkable implications for treatment of depression in HF. The impact on mortality mediated by physiologic, behavioral, and psychosocial factors could, theoretically, be attenuated through depression management. Likewise, novel treatments targeting these mediators of survival in HF and depression may also prove useful. However, studies testing these hypotheses are limited. For example, while SSRIs are safe from a cardiovascular standpoint and improve depression in patients with ischemic heart disease [26–28], the only completed large trial examining the effects of sertraline in HF patients with co-morbid major depressive disorder has failed to demonstrate superiority over placebo for either depression or cardiovascular prognosis [28]. Results of this study raise speculation that depression in HF may respond differently, or prove more resistant, to pharmacological interventions. Kulcu et al. conducted a small study (N=43) that found that aerobic exercise improves depressive symptoms (BDI; p=0.004), METs (metabolic equivalent of tasks), oxygen consumption, and exercise time over 8 weeks compared to a non-exercise group [29]. This finding, coupled with those of Zuluaga and colleagues that found inactivity mediates the relationship between depression and mortality [23], suggests that behavioral activation in the form of exercise among HF patients with depression merits further study. Discerning exercise benefits from the psychosocial support afforded by such intensive treatment programs will be critical in such studies. This hypothesis was noted in post hoc analyses of SADHART, ENRICHD, and SADHART-HF, in which data indicate significant improvement of depression and improved cardiovascular prognosis from trial participation alone, independent of intervention assignment [17–19].
While evidence on the improvement of depression in HF remains equivocal, a recent small study highlights the risk of worsening depression. In this first prospective study of mortality in HF and depression, worsening depressive symptoms over 1-year follow up was associated with increased hospitalizations or death in HF patients compared to stable or improved symptoms [30].
Study Limitations
Our study has limitations. Like many previous studies, we had only one baseline measure of depressive symptoms. Therefore, we were not able to investigate whether changes in depressive symptoms may have any effect on survival. Depression status might have changed substantially over the study duration, and the relation of depression measured during the index admission to mortality might have changed accordingly, though others have not found this to be the case [31]. Antidepressant prescription data collection was limited to baseline; adherence and course of treatment were not measured at all. It is also unknown whether participants received antidepressant treatment for depression beyond the index admission which may impact overall mortality. Only limited clinical data were collected upon index admission and thus more recently studied risk factors for mortality in HF could not be examined (e.g. renal function) as these data were not collected. No biological samples were collected from participants, preventing further investigation of underlying mechanisms which might explain the long-term impact of depression in our cohort. Cause of death was not known; therefore, we cannot determine whether depression is more highly associated with either cardiovascular death or other causes of death. Furthermore, information regarding suicide in this population would further delineate the impact of the death modality.
Conclusions
Depression measured at one point in time remains highly associated with mortality in HF up to 12 years even when adjusted for conventional risk factors of HF prognosis. A simple self-administered questionnaire that can differentiate a group of HF patients who are at approximately 35–40% higher risk for dying over a 12-year period is worthy of attention. More understanding is needed for the evolution of depression, such as whether a remission or recurrence of depression drives the prognosis of HF patients, and whether a subgroup of depressive patients who are more responsive to bio-psychosocial intervention can be identified. Optimal treatment modalities for depression in HF remain poorly understood, although increased physical activity and psychosocial support appear promising. The impact of various classes of antidepressants on overall depression management, mortality, and key mediators such as inflammation require further study. Novel approaches to treating biological co-factors of the depression-mortality relationship in HF merit further study as well. Combined treatment modalities will likely be necessary to fully address the matter of depression in HF, to not only bring psychological relief to the patient, but also to reduce co-morbidities and prolong survival.
Acknowledgments
The study was partially supported by grant 5P60AG11268 from National Institute of Aging and the National Institute of Mental Health (Grant R01-MH51191), Bethesda, Maryland and Claude D. Pepper Older American Independence centers (Dr. Jiang).
Footnotes
Disclosure Statement: The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger VL, Rosamond W, Sacco R, Sorlie P, Stafford R, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J. Heart Disease and Stroke Statistics--2010 Update: A Report From the American Heart Association. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48:1527–1537. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 3.Albert NM, Fonarow GC, Abraham WT, Gheorghiade M, Greenberg BH, Nunez E, O'Connor CM, Stough WG, Yancy CW, Young JB. Depression and clinical outcomes in heart failure: an OPTIMIZE-HF analysis. Am J Med. 2009;122:366–373. doi: 10.1016/j.amjmed.2008.09.046. [DOI] [PubMed] [Google Scholar]
- 4.Azevedo A, Bettencourt P, Frioes F, Alvelos M, Abreu-Lima C, Hense HW, Barros H. Depressive symptoms and heart failure stages. Psychosomatics. 2008;49:42–48. doi: 10.1176/appi.psy.49.1.42. [DOI] [PubMed] [Google Scholar]
- 5.Faris R, Purcell H, Henein MY, Coats AJ. Clinical depression is common and significantly associated with reduced survival in patients with non-ischaemic heart failure. Eur J Heart Fail. 2002;4:541–551. doi: 10.1016/s1388-9842(02)00101-0. [DOI] [PubMed] [Google Scholar]
- 6.Frasure-Smith N, Lesperance F, Habra M, Talajic M, Khairy P, Dorian P, Roy D. Elevated depression symptoms predict long-term cardiovascular mortality in patients with atrial fibrillation and heart failure. Circulation. 2009;120:134–140. doi: 10.1161/CIRCULATIONAHA.109.851675. 3p following 140. [DOI] [PubMed] [Google Scholar]
- 7.Friedmann E, Thomas SA, Liu F, Morton PG, Chapa D, Gottlieb SS. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J. 2006;152:940 e1–940 e8. doi: 10.1016/j.ahj.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 8.Jiang W, Kuchibhatla M, Clary GL, Cuffe MS, Christopher EJ, Alexander JD, Califf RM, Krishnan RR, O'Connor CM. Relationship between depressive symptoms and long-term mortality in patients with heart failure. Am Heart J. 2007;154:102–108. doi: 10.1016/j.ahj.2007.03.043. [DOI] [PubMed] [Google Scholar]
- 9.Johansson P, Dahlstrom U, Alehagen U. Depressive symptoms and six-year cardiovascular mortality in elderly patients with and without heart failure. Scand Cardiovasc J. 2007;41:299–307. doi: 10.1080/14017430701534829. [DOI] [PubMed] [Google Scholar]
- 10.Junger J, Schellberg D, Muller-Tasch T, Raupp G, Zugck C, Haunstetter A, Zipfel S, Herzog W, Haass M. Depression increasingly predicts mortality in the course of congestive heart failure. Eur J Heart Fail. 2005;7:261–267. doi: 10.1016/j.ejheart.2004.05.011. [DOI] [PubMed] [Google Scholar]
- 11.Jiang W, Alexander J, Christopher E, Kuchibhatla M, Gaulden LH, Cuffe MS, Blazing MA, Davenport C, Califf RM, Krishnan RR, O'Connor CM. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161:1849–1856. doi: 10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- 12.Zich JM, Attkisson CC, Greenfield TK. Screening for depression in primary care clinics: the CES-D and the BDI. Int J Psychiatry Med. 1990;20:259–277. doi: 10.2190/LYKR-7VHP-YJEM-MKM2. [DOI] [PubMed] [Google Scholar]
- 13.Carney RM, Rich MW, Tevelde A, Saini J, Clark K, Jaffe AS. Major depressive disorder in coronary artery disease. Am J Cardiol. 1987;60:1273–1275. doi: 10.1016/0002-9149(87)90607-2. [DOI] [PubMed] [Google Scholar]
- 14.Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction. Impact on 6-month survival. JAMA. 1993;270:1819–1825. [PubMed] [Google Scholar]
- 15.Parissis JT, Nikolaou M, Farmakis D, Bistola V, Paraskevaidis IA, Adamopoulos S, Filippatos G, Kremastinos DT. Clinical and prognostic implications of self-rating depression scales and plasma B-type natriuretic peptide in hospitalised patients with chronic heart failure. Heart. 2008;94:585–589. doi: 10.1136/hrt.2007.117390. [DOI] [PubMed] [Google Scholar]
- 16.Linke SE, Rutledge T, Johnson BD, Vaccarino V, Bittner V, Cornell CE, Eteiba W, Sheps DS, Krantz DS, Parashar S, Bairey Merz CN. Depressive symptom dimensions and cardiovascular prognosis among women with suspected myocardial ischemia: A report from the National Heart, Lung, and Blood Institute-sponsored Women's Ischemia Syndrome Evaluation. Arch Gen Psychiatry. 2009;66:499–507. doi: 10.1001/archgenpsychiatry.2009.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carney RM, Blumenthal JA, Freedland KE, Youngblood M, Veith RC, Burg MM, Cornell C, Saab PG, Kaufmann PG, Czajkowski SM, Jaffe AS. Depression and late mortality after myocardial infarction in the Enhancing Recovery in Coronary Heart Disease (ENRICHD) study. Psychosom Med. 2004;66:466–474. doi: 10.1097/01.psy.0000133362.75075.a6. [DOI] [PubMed] [Google Scholar]
- 18.Glassman AH, Bigger JT, Jr, Gaffney M. Psychiatric characteristics associated with long-term mortality among 361 patients having an acute coronary syndrome and major depression: seven-year follow-up of SADHART participants. Arch Gen Psychiatry. 2009;66:1022–1029. doi: 10.1001/archgenpsychiatry.2009.121. [DOI] [PubMed] [Google Scholar]
- 19.Jiang W, Krishnan R, Kuchibhatla M, Cuffe MS, Martsberger C, Arias RM, O'Connor CM. Characteristics of depression remission and its relation with cardiovascular outcome among patients with chronic heart failure (from the SADHARTHF Study) Am J Cardiol. 2011;107:545–551. doi: 10.1016/j.amjcard.2010.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Faller H, Stork S, Schowalter M, Steinbuchel T, Wollner V, Ertl G, Angermann CE. Depression and survival in chronic heart failure: does gender play a role? Eur J Heart Fail. 2007;9:1018–1023. doi: 10.1016/j.ejheart.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 21.Trivedi RB, Blumenthal JA, O'Connor C, Adams K, Hinderliter A, Dupree C, Johnson K, Sherwood A. Coping styles in heart failure patients with depressive symptoms. J Psychosom Res. 2009;67:339–346. doi: 10.1016/j.jpsychores.2009.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kovacs M, Rottenberg J, George C. Maladaptive mood repair responses distinguish young adults with early-onset depressive disorders and predict future depression outcomes. Psychol Med. 2009;39:1841–1854. doi: 10.1017/S0033291709005789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zuluaga MC, Guallar-Castillon P, Rodriguez-Pascual C, Conde-Herrera M, Conthe P, Rodriguez-Artalejo F. Mechanisms of the association between depressive symptoms and long-term mortality in heart failure. Am Heart J. 2010;159:231–237. doi: 10.1016/j.ahj.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 24.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 25.Carney RM, Freedland KE, Eisen SA, Rich MW, Jaffe AS. Major depression and medication adherence in elderly patients with coronary artery disease. Health Psychol. 1995;14:88–90. doi: 10.1037//0278-6133.14.1.88. [DOI] [PubMed] [Google Scholar]
- 26.Jiang W, O'Connor C, Silva SG, Kuchibhatla M, Cuffe MS, Callwood DD, Zakhary B, Henke E, Arias RM, Krishnan R. Safety and efficacy of sertraline for depression in patients with HF (SADHART-HF): a randomized, double-blind, placebocontrolled trial of sertraline for major depression with congestive heart failure. Am Heart J. 2008;156:437–444. doi: 10.1016/j.ahj.2008.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lesperance F, Frasure-Smith N, Koszycki D, Laliberte MA, van Zyl LT, Baker B, Swenson JR, Ghatavi K, Abramson BL, Dorian P, Guertin MC. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA. 2007;297:367–379. doi: 10.1001/jama.297.4.367. [DOI] [PubMed] [Google Scholar]
- 28.O'Connor CM, Jiang W, Kuchibhatla M, Silva SG, Cuffe MS, Callwood DD, Zakhary B, Stough WG, Arias RM, Rivelli SK, Krishnan R. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-HF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol. 2010;56:692–699. doi: 10.1016/j.jacc.2010.03.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kulcu DG, Kurtais Y, Tur BS, Gulec S, Seckin B. The effect of cardiac rehabilitation on quality of life, anxiety and depression in patients with congestive heart failure. A randomized controlled trial, short-term results. Eura Medicophys. 2007;43:489–497. [PubMed] [Google Scholar]
- 30.Sherwood A, Blumenthal JA, Hinderliter A, Koch GG, Kirkwood FA, Dupree C, Bensimhon DR, Johnson KS, Trivedi R, Bowers M, Christenson RH, O'Connor C. Worsening depressive symptoms are associated with adverse clinical outcomes in patients with heart failure. J Am Coll Cardiol. 2011;57:418–423. doi: 10.1016/j.jacc.2010.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lesperance F, Frasure-Smith N, Talajic M, Bourassa MG. Five-year risk of cardiac mortality in relation to initial severity and one-year changes in depression symptoms after myocardial infarction. Circulation. 2002;105:1049–1053. doi: 10.1161/hc0902.104707. [DOI] [PubMed] [Google Scholar]