Abstract
BACKGROUND:
Traditionally regarded as a disease of the elderly, the incidence of diverticulitis of the colon has been on the rise, especially in younger cohorts. These patients have been found to experience a more aggressive disease course with more frequent hospitalization and greater need for surgical intervention.
OBJECTIVE:
To characterize factors that portend a poor prognosis in patients diagnosed with diverticulitis; in particular, to evaluate the role of demographic variables on disease course.
METHODS:
Using the Canadian Institute for Health Information Discharge Abstract Databases, readmission rates, length of stay, colectomy rates and mortality rates in patients hospitalized for diverticulitis were examined. Data were stratified according to age, sex and comorbidity (as defined by the Charlson index).
RESULTS:
In the cohort ≤30 years of age, a clear male predominance was apparent. Colectomy rate in the index admission, stratified according to age, demonstrated a J-shaped curve, with the highest rate in patients ≤30 years of age (adjusted OR 2.3 [95% CI 1.62 to 3.27]) compared with the 31 to 40 years of age group. In-hospital mortality increased with age. Cumulative rates of readmission at six and 12 months were 6.8% and 8.8%, respectively.
CONCLUSION:
In the present nationwide cohort study, younger patients (specifically those ≤30 years of age) were at highest risk for colectomy during their index admission for diverticulitis. It is unclear whether this observation was due to more virulent disease among younger patients, or surgeon and patient preferences.
Keywords: Colectomy, Diverticulitis, Hospitalization, Young onset
Abstract
HISTORIQUE :
L’incidence de la diverticulite du côlon, habituellement considérée comme une maladie des personnes âgées, est en hausse, surtout dans les cohortes plus jeunes. Ces patients présentent une évolution plus agressive de la maladie, sont hospitalisés plus souvent et ont davantage besoin d’une intervention chirurgicale.
OBJECTIF :
Caractériser les facteurs qui annoncent un mauvais pronostic chez les patients qui obtiennent un diagnostic de diverticulite, notamment évaluer le rôle des variables démographiques sur l’évolution de la maladie.
MÉTHODOLOGIE :
Les chercheurs ont utilisé la Base de données sur les congés des patients de l’Institut canadien d’information sur la santé pour examiner le taux de réhospitalisations, la durée de séjour, le taux de colectomies et le taux de mortalité des patients hospitalisés pour soigner une diverticulite.
RÉSULTATS :
Au sein de la cohorte des moins de 30 ans, les chercheurs ont remarqué une nette prédominance de sujets de sexe masculin. Le taux de colectomies dans les hospitalisations de référence, stratifiées selon l’âge, a révélé une courbe en forme de J, le taux le plus élevé s’observant chez les patients de moins de 30 ans (RR rajusté 2,3 [95 % IC 1,62 à 3,27]) par rapport à ceux des 31 à 40 ans. La mortalité en milieu hospitalier augmente avec l’âge. Le taux cumulatif de réhospitalisations au bout de six et de 12 mois s’élevait à 6,8 % et à 8,8 %, respectivement.
CONCLUSION :
Dans la présente étude nationale de cohorte, les patients plus jeunes (notamment ceux de moins de 30 ans) étaient les plus vulnérables à une colectomie pendant leur hospitalisation de référence pour soigner une diverticulite. On ne sait pas si cette observation s’explique par la nature plus virulente de la maladie chez les patients plus jeunes ou par une préférence des chirurgiens et des patients.
The incidence of diverticular disease has been on the rise in both Europe and North America (1–3). It has traditionally been regarded as a disease of the elderly; however, recent evidence suggests that diverticular disease is increasingly being recognized in younger cohorts (4,5). Overall, more than 130,000 Canadians are affected by diverticular disease and approximately 10% of these patients will require either elective or emergent hospitalization. Recurrent disease is associated with increased hospitalization, longer length of stay and increased need for surgery (3). The nature of recurrent diverticular disease plays a major role in health-related quality of life and overall national health care costs.
Younger patients have often been recognized as experiencing a more aggressive disease course with more frequent hospitalizations and greater need for surgical intervention (6,7). Previous studies have characterized the changing epidemiology of diverticular disease in the United States (3,5). In the present study, we aimed to examine Canadian trends using discharge data from the Canadian Institute for Health Information (CIHI). We hypothesized that younger males have a particularly aggressive form of diverticular disease that requires more frequent readmissions. Determining which demographic variables portend a poor prognosis will help physicians identify higher-risk patients early in the disease course and offer appropriate interventions.
METHODS
A retrospective cohort study examining data from the CIHI Discharge Abstract Databases (CIHI-DAD) was performed. All patients with a primary diagnosis of diverticular disease identified by the International Classification of Diseases and Related Health Problems – 10th Revision code of K57.2–57.9 admitted between April 1, 2007 and March 31, 2009 were included. This was considered the index hospitalization. Any hospital admissions for diverticular disease in the look-back period between April 1, 2004 and March 31, 2007 were excluded. This was performed to ensure there were no previous episodes of diverticular disease at least three years before the study period.
The CIHI-DAD contains demographic information, clinical details and administrative data on all services delivered by hospitals governed under provincial health insurance plans. Details regarding age, sex, admission diagnosis, length of stay, comorbidity measured by the Charlson index, procedures undertaken during hospitalization, vital status at discharge and type of admission (elective versus nonelective) were collected. The Charlson index has been used in many studies using administrative data to characterize and adjust for comorbidity and case mix (8). Each record within the CIHI databases contains individual anonymized patient data that enables researchers to link repeated admissions to the same patient.
The primary outcome measure was the proportion of patients who progressed to colectomy (either partial or total) during index hospitalization. For patients who did not undergo colectomy, a secondary outcome measure was the readmission rates at six and 12 months. Patients who underwent any type of colectomy during the index admission were excluded from the present analysis because they were deemed to be at higher risk of readmission given the higher likelihood of postoperative complications related to their surgery. The CIHI-DAD was searched for any subsequent admissions occuring after the index admission in the time period from April 1, 2007 to March 31, 2009. A second admission within this interval was considered a readmission. The time to readmission was defined as the number of months between the discharge date of the index hospitalization and the admission date of any subsequent admission. Readmissions occurring within six and 12 months of discharge were analyzed. Other outcome measures included in-hospital mortality rate and length of stay during index admission.
The χ2 and Fisher’s exact tests were used to compare categorical variables across groups and Student’s t test and Wilcoxon rank-sum test for continuous variables. Additionally, multiple logistic regression models were used to assess for predictors of surgery for diverticultis and death while adjusting for sex and comorbidity. Each of the 17 comorbid conditions in the Charlson index were included as predictors in the model. The adjusted ORs for the association between individual comorbid conditions and colectomy and death were derived from the beta coefficients for each of these predictors in the multiple logistic regression models. Kaplan-Meier methods were used to determine the cumulative risk of readmission, and Cox regression analysis to further control for comorbidity and other demographic factors. Adjusted HRs for readmissions associated with age were ascertained from the Cox regression models. Results were considered to be statistically significant at P<0.05.
The present study was approved by the Research Ethics Board at Mount Sinai Hospital, Toronto, Ontario. No personal health information was collected and potentially identifying data were amassed collectively and analyzed in aggregate.
RESULTS
A total of 18,711 individuals admitted for acute diverticulitis within the two-year study period who met inclusion criteria and who did not have any admissions in the previous three-year look-back period for acute diverticulitis were identified.
The mean (± SD) age was 64.0±16.5 years. Subjects were categorized into five age groups (≤30 years, 31 to 40 years, 41 to 50 years, 51 to 60 years, and >60 years) (Figure 1). Subjects were further dichotomized into two age groups (≤30 years versus >30 years). There were 328 patients who were ≤30 years of age, comprising 1.8% of the overall study population. The group comprising subjects ≤30 years of age was predominantly male (70% male), while the group >30 years of age was predominantly female (55% female).
Figure 1.
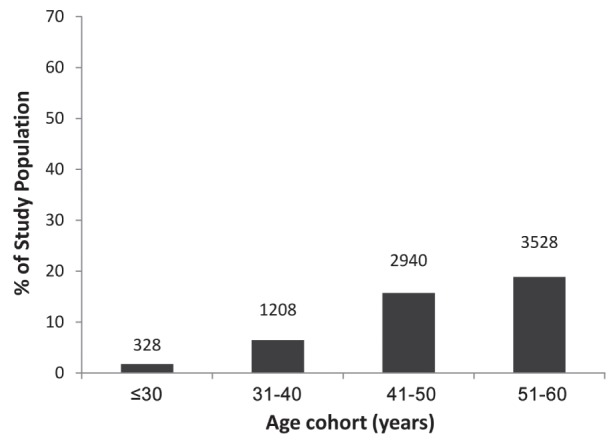
Age distribution of the study population over the five age groups. Raw numbers in each cohort appear above individual bars
The mean weighted Charlson index was 0.42±0.99. The prevalences of individual comorbidities stratified according to age group are shown in Table 1.
TABLE 1.
Distribution of individual comorbidities among age groups and their association with colectomy and death outcomes
| Comorbidity |
Age, years
|
Adjusted OR
|
||
|---|---|---|---|---|
| >30 | ≤30 | Colectomy | Death | |
| Acute myocardial infarction | 348 (1.89) | 0 (0) | 1.72 | 3.75 |
| Congestive heart failure | 451 (2.45) | 0 (0) | 1.60 | 2.54 |
| Peripheral vascular disease | 205 (1.12) | 1 (0.3) | 0.94 | 1.98 |
| Cerebrovascular disease | 174 (0.95) | 1 (0.3) | 1.06 | 4.53 |
| Dementia | 372 (2.02) | 0 (0) | 1.04 | 2.48 |
| COPD | 761 (4.14) | 2 (0.61) | 1.29 | 2.36 |
| Rheumatoid disease | 154 (0.84) | 0 (0) | 2.68 | 4.30 |
| Peptic ulcer disease | 97 (0.53) | 0 (0) | 1.81 | 1.51 |
| Mild liver disease | 91 (0.5) | 2 (0.61) | 0.70 | 3.75 |
| Moderate/severe liver disease | 18 (0.1) | 0 (0) | 4.55 | 9.60 |
| Diabetes | 1511 (8.22) | 4 (1.22) | 0.95 | 0.75 |
| Diabetes with complications | 919 (5) | 2 (0.61) | 0.95 | 1.51 |
| Hemiplegia/paraplegia | 35 (0.19) | 2 (0.61) | 1.50 | 0.63 |
| Renal disease | 515 (2.8) | 1 (0.3) | 1.19 | 2.42 |
| Cancer | 439 (2.39) | 1 (0.3) | 1.47 | 3.20 |
| Metastatic cancer | 119 (0.65) | 1 (0.3) | 2.21 | 7.90 |
| AIDS | 5 (0.03) | 0 (0) | N/A | N/A |
Data presented as n (%) unless otherwise indicated. COPD Chronic obstructive pulmonary disease; N/A Not applicable
Colectomy
The rates of colectomy during index admission stratified according to age groups are shown in Figure 2, which exhibits a J-shaped curve. Subjects ≤30 years of age who were admitted for acute diverticulitis exhibited the highest rate of large bowel resection (18%), while those in the 31 to 40 year age group had the lowest rate of resection (8%). Starting after 30 years of age, there was a increasing trend in colectomy rate until 60 years of age; thereafter, it reached a plateau of 13% and never approached the high rate observed in those ≤30 years of age. When age was dichotomized, the surgery rate among subjects ≤30 years of age was higher than that of those >30 years of age (18% versus 13%; P=0.009).
Figure 2.
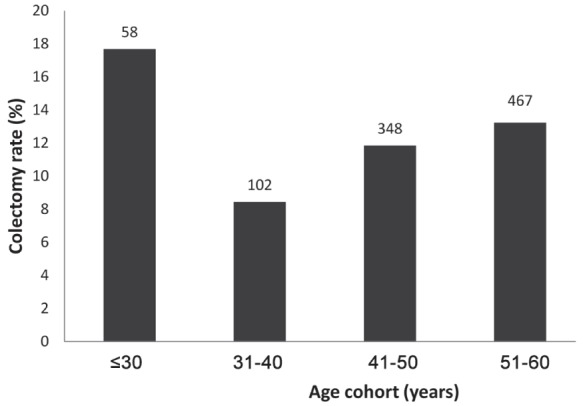
Proportion of the study population undergoing colectomy, stratified according to age cohort. Raw numbers within each group appear above individual bars
In multivariate analysis, the 31 to 40 year age group was designated the reference group because it had the lowest risk for surgery. After adjustment for sex and comorbidity, those ≤30 years of age had a greater than twofold higher risk of colectomy (adjusted OR [aOR] 2.3 [95% CI 1.62 to 3.27]) than the 31 to 40 year age group. Relative to the comparator group, the aOR for surgery for those 41 to 50 years, 51 to 60 years and >60 years were 1.48 (95% CI 1.17 to 1.87), 1.70 (95% CI 1.35 to 2.13) and 1.66 (95% CI 1.34 to 2.06), respectively. Overall, each additional comorbidity was associated with increased risk of surgery (Table 1); every incremental point in the Charlson index was associated with an aOR of 1.16 (95% CI 1.13 to 1.21). In contrast, female sex was associated with a reduced risk of surgery compared with male sex (OR 0.73 [95% CI 0.67 to 0.80). When comparing subjects ≤30 years of age with those >30 years of age, the former had a nearly 50% higher risk of colectomy (aOR 1.47 [95% CI 1.10 to 1.96]).
Mortality and readmissions
In-hospital mortality during index admission stratified according to age group is shown in Figure 3. As expected, in-hospital mortality increased with age. There were no deaths in the group ≤30 years of age. Mortality was highest among those with coexistent moderate to severe liver disease, metastatic cancer, cerebrovascular disease and rheumatoid disease (Table 1).
Figure 3.
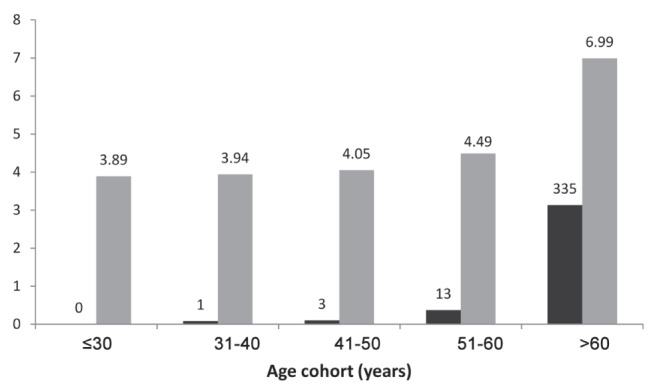
Mortality rate and length of stay in each age cohort. Black bars display the number of deaths in each group as a percent of total with raw numbers appearing above individual bars. Grey bars (with accompanying numbers) show the mean length of stay during their first hospitalization for patients in each age group who did not undergo colectomy
Readmission to hospital was subsequently examined at six and 12 months from the date of discharge. Of the 16,304 patients in the study population who did not undergo a colectomy, the cumulative rates of readmission at six and 12 months were 6.8% and 8.8%, respectively. Figure 4 shows six- and 12-month readmission rates stratified according to age group. The sex- and comorbidity-adjusted HRs for the 31 to 40 year, 41 to 50 year, and 51 to 60 year age groups were similar. The 31 to 40 year age group was defined as the reference. When compared with one another or with the reference group, both the ≤30 year (adjusted HR 0.68 [95% CI 0.44 to 1.06]) and >60 year age groups (adjusted HR 0.81 [95% CI 0.68 to 0.96]) exhibited lower risk of admissions. Women were at modestly higher risk of readmission (adjusted HR 1.10 [95% CI 1.01to 1.21]).
Figure 4.
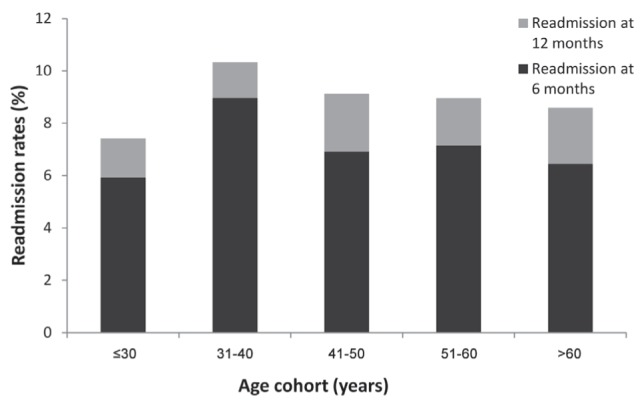
Readmission rates at six and 12 months stratified according to age cohort. For patients who did not undergo colectomy, black bars represent readmission to hospital at six months’ postdischarge. Similar data are presented for readmission at 12 months’ postdischarge
The mean length of stay for the study population that did not undergo colectomy was 5.8±9.4 days. After 40 years of age, the length of stay among those who did not undergo colectomy increased with age (Figure 3).
DISCUSSION
The present retrospective cohort study highlights that age may influence prognosis following admission for acute diverticulitis. Specifically, we showed that patients ≤30 years of age are more than twice as likely to undergo colectomy (either partial or total) compared with patients 31 to 40 years of age, despite having fewer comorbid conditions. However, younger age was not associated with higher in-hospital mortality or length of stay.
Diverticulitis has traditionally been regarded as a disease of the elderly. However, previous studies dating back to the early 1990s have demonstrated an increased rate of diverticulitis in the young, specifically those <45 years of age (3–5,9–11). Some studies have even commented on a more virulent disease course in young patients (6,12–14). The rate of diverticulitis-associated colectomy has increased among younger age groups. This trend may have reflected a growing incidence of diverticulitis in that subpopulation, resulting in more overall surgeries, but not necessarily a greater risk for surgery. Our study has demonstrated that individuals ≤30 years of age were, indeed, at higher risk for colectomy.
Potential mechanisms for such an association are not well understood. It may be that older patients inherently have more complex medical disease and that surgeons may be reluctant to operate on these individuals. Another possibility is that younger patients may be misdiagnosed as having a viral gastrointestinal illness and, therefore, not be prescribed appropriate antimicrobial therapy. As such, these patients may be more likely to progress to complications. Additionally, others have observed that the severity of first presentation is considerably worse in younger patients (6). Given that these patients have many more years of potential disease burden ahead of them, clinicians caring for these individuals may be more inclined to operate to prevent recurrent disease. Moreover, mild cases of acute diverticulitis are often treated in the outpatient setting. It is possible that physicians have a higher threshold for younger patients with acute diverticulitis but few comorbid conditions. Thus, individuals ≤30 years of age who are admitted may reflect a selection bias for younger individuals with the most severe clinical presentations.
Among younger patients with diverticulitis, many studies have documented a more aggressive disease course in men in particular (5,6,9). In our study, however, female sex was associated with an increased likelihood of readmission. The reason for this is not entirely clear. Readmission rates and data regarding length of stay were only analyzed in patients who did not undergo colectomy. Thus, it may be that more men were receiving surgery at their initial presentation whereas women were more likely to receive conservative management and were, therefore, at higher risk of recurrence. In a similar vein, the role of sex in complicated diverticulitis deserves close attention. One study found that female patients were more likely to require surgery for their diverticular disease (15). In this case series, men were significantly more likely to present with fistulizing disease or bleeding, whereas females were more likely to exhibit strictures, obstructions or perforations. On the other hand, these same male patients were more likely to progress to an operation at a younger age. Given the high one-year mortality rate associated with complicated diverticular disease, further research into potential demographic predictors of a poor disease course is needed (16). In a separate study, Kang et al (17) showed that whereas males were 15% more likely to undergo surgery, females were more likely to be admitted for diverticular disease and experienced higher age-standardized mortality rates.
Among the limitations of the present study was that our study population did not include milder cases of acute diverticulitis that may have been treated in the outpatient setting. We were not able to distinguish whether the clinical threshold for admission varied among the different age groups. Administrative data inherently do not contain laboratory, radiographic and detailed clinical data that would enable further characterization of disease severity. Furthermore, whether colectomy is performed is also influenced by patient preference. Because our study did not capture data on either disease severity or patient preference, it was not possible to distinguish the relative contributions of either factor to the higher rates of surgery in younger-onset acute diverticulitis.
SUMMARY
Our study demonstrated that diverticulitis is not a disease limited to the elderly. Incidence rates have been increasing in all age cohorts, with the fastest rise apparent in patients <40 years of age (3). Younger patients, specifically those ≤30 years of age, were more likely to undergo a colectomy. We must be cautious in attributing this observation to more aggressive disease because patient and surgeon preferences may also influence the decision to perform surgery. It is possible that surgeons may have a lower threshold to operate on very young patients (≤30 years) because acute diverticulitis is unusual in this group and because they have lower comorbidity. Further studies to understand the pathophysiological basis for this observation are warranted. Meanwhile, given such findings, clinicians should have greater index of suspicion for acute diverticulitis in younger patients and increased vigilance for complications that may require surgery.
KEY MESSAGES
Acute diverticulitis presenting in younger adults is becoming more frequent.
Younger adults presenting with acute diverticulitis undergo surgery more frequently than their older counterparts.
Younger adults, however, exhibited lower mortality and those who did not undergo surgery had lower risk of readmissions for acute diverticulitis.
Footnotes
DISCLOSURES: The authors have no finacial disclosures or conflicts of interest to declare.
REFERENCES
- 1.Masoomi H, Buchberg BS, Magno C, Mills SD, Stamos MJ. Trends in diverticulitis management in the United Statees from 2002 to 2007. Arch Surg. 2011;146:400–6. doi: 10.1001/archsurg.2010.276. [DOI] [PubMed] [Google Scholar]
- 2.Jeyarajah S, Faiz O, Bottle A, et al. Diverticular disease hospital admissions are increasing, with poor outcomes in the elderly and emergency admissions. Aliment Pharmacol Ther. 2009;30:1171–82. doi: 10.1111/j.1365-2036.2009.04098.x. [DOI] [PubMed] [Google Scholar]
- 3.Etzioni DA, Mack TM, Beart RW, Jr, Kaiser AM. Diverticulitis in the United States 1998–2005: Changing patterns of disease and treatment. Ann Surg. 2009;249:210–7. doi: 10.1097/SLA.0b013e3181952888. [DOI] [PubMed] [Google Scholar]
- 4.Acosta JA, Grebenc ML, Doberneck RC, McCarthy JD, Fry DE. Colonic diverticular disease in patients 40 years old or younger. Am Surg. 1992;58:605–7. [PubMed] [Google Scholar]
- 5.Nguyen GC, Sam J, Anand N. Epidemiological trends and geographic variation in hospital admissions for diverticulitis in the United States. World J Gastroenterol. 2011;17:1600–5. doi: 10.3748/wjg.v17.i12.1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lahat A, Menachem Y, Avidan B, et al. Diverticulitis in the young patient – is it different? World J Gastroenterol. 2006;12:2932–5. doi: 10.3748/wjg.v12.i18.2932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ambrosetti P, Robert JH, Witzig JA, et al. Acute left colonic diverticulitis in young patients. J Am Coll Surg. 1994;179:156–60. [PubMed] [Google Scholar]
- 8.Nguyen GC, Rosenberg M, Chong RY, Chong CA. Early cholecystectomy and ERCP are associated with reduced readmissions for acute biliary pancreatitis: A nationwide, population-based study. Gastrointest Endosc. 2012;75:47–55. doi: 10.1016/j.gie.2011.08.028. [DOI] [PubMed] [Google Scholar]
- 9.Schauer PR, Ramos R, Ghiatas AA, Sirinek KR. Virulent diverticular disease in young obese men. Am J Surg. 1992;164:443–8. doi: 10.1016/s0002-9610(05)81177-8. [DOI] [PubMed] [Google Scholar]
- 10.Etzioni DA, Cannom RR, Ault GT, Beart RW, Kaiser AM. Diverticulitis in California from 1995 to 2006: Increased rates of treatment for younger patients. Am Surg. 2009;75:981–5. [PubMed] [Google Scholar]
- 11.Marinella MA, Mustafa M. Acute diverticulitis in patients 40 years of age and younger. Am J Emerg Med. 2000;18:140–2. doi: 10.1016/s0735-6757(00)90004-4. [DOI] [PubMed] [Google Scholar]
- 12.Guzzo J, Hyman N. Diverticulitis in young patients: Is resection after a single attack always warranted? Dis Colon Rectum. 2004;47:1187–90. doi: 10.1007/s10350-004-0546-7. [DOI] [PubMed] [Google Scholar]
- 13.Minardi AJ, Jr, Johnson LW, Sehon JK, Zibari GB, McDonald JC. Diverticulitis in the young patient. Am Surg. 2001;67:458–61. [PubMed] [Google Scholar]
- 14.Makela J, Vuolio S, Kiviniemi H, Laitinen S. Natural history of diverticular disease: When to operate? Dis Colon Rectum. 1998;41:1523–28. doi: 10.1007/BF02237300. [DOI] [PubMed] [Google Scholar]
- 15.McConnell EJ, Tessier DJ, Wolff BG. Population-based incidence of complicated diverticular disease of the sigmoid colon based on gender and age. Dis Colon Rectum. 2003;46:1110–4. doi: 10.1007/s10350-004-7288-4. [DOI] [PubMed] [Google Scholar]
- 16.Humes DJ, West J. Role of acute diverticulitis in the development of complicated colonic diverticular disease and 1-year mortality after diagnosis in the UK: Population-based cohort study. Gut. 2012;61:95–100. doi: 10.1136/gut.2011.238808. [DOI] [PubMed] [Google Scholar]
- 17.Kang JY, Hoare J, Tinto A, et al. Diverticular disease of the colon – on the rise: A study of hospital admissions in England between 1989/1990 and 1999/2000. Aliment Pharmacol Ther. 2003;17:1189–95. doi: 10.1046/j.1365-2036.2003.01551.x. [DOI] [PubMed] [Google Scholar]


