Abstract
This study examined the relationship between the traditional masculine norms (“status,” “toughness” and “antifemininity”) of 296 ethnically and racially diverse, young men transitioning to fatherhood and substance use (smoking, alcohol, marijuana, hard drugs) and health behaviors (diet, exercise). Participants were recruited from urban obstetric clinics in the Northeast United States. Logistic and multiple regression equations were constructed to examine the relationship between masculine norms and health behaviors. Moderator effects were also examined. Masculine norm “status” was most endorsed and “antifemininity” was least endorsed. African American young men had higher masculine norm scores than Latino and Whites. Different masculine norms were associated with health-promoting and health-undermining behaviors. Different racial groups who had higher scores on some masculine norms were more likely to engage in either health-promoting or health-undermining behaviors when compared with other ethnic groups in this study. These results observed different relationships between the traditional masculine norms measured and the substance use and health behaviors of diverse, young men transitioning to fatherhood. This may have implications for intervention strategies and future research.
Keywords: masculinity, young fathers, health behaviors, substance use
Masculinity and health behaviors have been described as incompatible (Courtenay, 2002). Males experience greater pressure to endorse gendered social prescriptions, and ethnic minority individuals experience significant challenges as they negotiate their masculine identities (Courtenay, 2000a, 2000b; Emslie, Ridge, Ziebland, & Hunt, 2006; Wade, 2008). Masculinities have also been associated with health outcomes for men, including less help seeking, asking fewer questions in health settings, involvement in less preventive health care, and involvement in more health-undermining behaviors (Courtenay, 2002; McKelley & Rochlen, 2010). Although these studies look at behaviors that have been reported to affect the medical visit or care, they do not address the health behaviors that men engage in daily life (Courtenay, 2000a; Lee & Owens, 2002; Mahalik, Burns, & Syzdek, 2007; Mankowski & Maton, 2010). The relationship between masculine norms and health requires some consideration of the theories that link the two and integrate their meaning for diverse young men.
Masculine Norms and Health: A Conceptual Model
Traditional masculinity or hegemonic masculinity has generally been conceptualized to represent the way that men are to behave, including things done and role expectations. Traditional masculinity has also been described as being available only to a subset of men (i.e., White men; Courtenay, 2000a, 2000b). Nevertheless, all men are required, socially, to position themselves to it. Within this positioning, traditional masculinity is legitimized through its subjugation of women and other subordinate masculinities (e.g., gay men; Connell & Messerschmidt, 2005). This definition represents a static view of what constitutes masculinity. Researchers (Courtenay, 2000a; Galdas et al., 2005; Mahalik et al., 2007; Mankowski & Maton, 2010; Wade, 2008) have highlighted a shift in the understanding of traditional masculinity, from one that is not static but dynamic and that can differ across social situations (Connell & Messerschmidt, 2005). Simply stated, there are multiple traditional masculinities that may differentially relate to health behaviors. The shape of these masculinities includes striving toward competition, success, and power (e.g., status), being tough and aggressive (e.g., toughness), and the rejection of anything stereotypically feminine (e.g., antifemininity; Mankowski & Maton, 2010; O’Neil, Helms, Gable, David, & Wrightsman, 1986). In some instances, masculine norms that include being tough and rejecting feminine stereotypes (i.e., toughness and antifemininity) may be thought of as having a negative relationship with help-seeking behaviors. However, it is possible that other norms such as status (striving for success and power) may serve to promote healthy behaviors in some instances. Although not exhaustive, these examples represent some of the most examined traditional masculine norms. Masculine norms also have relevance for young, diverse, expecting fathers, who, because of their impending role change, may find their masculine identity in the process of redefinition.
There are a number of factors that have been identified and described as affecting the health of men. Most notable are the traditional masculine norms reinforced through the gender socialization experiences of men (Courtenay, 2000a, 2000b). Studies have documented a relationship between these masculine norms and high-risk sexual behaviors (Barker & Ricardo, 2005), parenting (Marsiglio & Pleck, 2005), violence toward intimate partner (Anderson, 2005), use of health-promoting behaviors (e.g., asking question during the medical visit and seeking preventive care; Mahalik, Lagan, & Morrison, 2006), and alcohol abuse (McCreary, Newcomb, & Sadava, 1999). There is also some evidence that not all masculine norms have negative relationships with health-promoting behaviors. Some (see Levant, 2008) argue that men’s can do attitude (i.e., toughness) may be health promoting. Furthermore, others (see Mankowski & Maton, 2010) argue that masculinity in its various forms and their traits may be used to facilitate positive adaptation.
Little research has explored how masculine norms affect health behaviors across races. The intersection of race and gender is particularly relevant to health and health-related behavior. Minority men have been described as having higher age-adjusted mortality and death rates for several preventable causes in the United States and experience more burden of preventable morbidity and mortality (Anonymous, 1990; Braveman & Egerter, 2008; Cohen et al., 1991; Cooper, 1993; Fullilove et al., 1999; Greenberg & Schneider, 1994; Heron, 2011; McCord & Freeman, 1990; Ravenell et al., 2008; Treadwell & Ro, 2003; Williams & Collins, 2002).
Fatherhood may be an important time to understand health behaviors because it represents a significant transition in the lives of young men and may be an important catalyst to behavior change. When compared with young men who have not fathered a child, the evidence suggests that the transition to fatherhood may negatively affect the health of young men and that these effects may extend past pregnancy, negatively affecting their parenting behaviors (Bartlett, 2004; Buist, Morse, & Durkin, 2003; Condon, Boyce, & Corkindale, 2004). Fewer studies exist about the negative health outcomes for diverse adolescent and young fathers. Studies that have examined their health functioning report increased substance use, delinquency, and other health-undermining behaviors when compared with their same-aged peers who are not fathers (Lane & Clay, 2000; Weinman, Buzi, & Smith, 2005; Weinman, Smith, & Buzi, 2002).
Traditional masculinity affects the health beliefs, practices, and resources accessed by men (Courtenay, 2002; Mahalik, Good, & Englar-Carlson, 2003). Understanding how the endorsed masculine norms and the consequences of these norms on the health and well-being of young men transitioning to adulthood and parenthood is important. Young adulthood is a unique period when traditional masculinity is being constructed and reconstructed. We propose to address an important gap in the literature: How do traditional masculine norms affect the health behaviors of young fathers? Given that toughness, antifemininity, and status are the most referenced masculine norms reviewed in research and theoretical thinking about masculinity and there are reliable measures of these three norms, we hypothesized that the masculine norms of “toughness” and “antifemininity” will be negatively related to health behaviors whereas the masculine norm “status” will promote positive health behaviors. Second, we hypothesize that race will moderate the relationship between these traditional masculine norms and health behaviors, with Black and Latino men more strongly endorsing these norms.
Method
Study Sample and Procedures
Data for this study come from a longitudinal study of young expectant fathers and their pregnant adolescent partners. Between July 2007 and February 2011, 296 young expectant fathers were recruited from their partners’ referrals who were recruited at obstetrics and gynecology clinics in four university-affiliated hospitals in Connecticut. Potential participants were screened and, if eligible, research staff explained the study in detail and answered any questions.
Inclusion criteria included (a) the pregnant partner is in the second or third trimester of pregnancy at time of baseline interview; (b) age at least 14 years, at time of the interview; (c) in a romantic relationship with the mother of the baby; (d) report being the biological parent of the unborn baby; (e) partner also agrees to participate in the study; and (f) able to speak English or Spanish. The mother’s age was the index criteria for inclusion in this study. As a result, there was no maximum limit for the inclusion of the fathers in this study. Because this was a longitudinal study we used an initial run-in period as part of eligibility criteria where participants were deemed ineligible if they could not be recontacted after screening and before their estimated due date. Both the young mothers and the fathers needed to consent to be a part of the study in order to be enrolled.
A research staff member, at the baseline appointment, obtained written informed consent. The men completed structured interviews via audio computer-assisted self-interviews. Participation was voluntary and confidential, and did not influence the provision of health care or social services. All procedures were approved by the Yale University Human Investigation Committee and by institutional review boards at study clinics. Participants were reimbursed $25 each for their effort.
Of 413 eligible men, 296 (72.2%) enrolled in the study. Those who agreed to participate had partners of greater gestational age (p = .03). Participation did not vary by any other prescreened demographic characteristic (e.g., age, race, income; all p > .05). Data reported are from the baseline assessments of the 296 male participants.
The majority of participants were African American (48.6%) or Hispanic (36.5%), with 14.9% White/Other race. Average age was 21.3 years (SD = 4.1; range = 15-25 years). A total of 8.8% of the young men were married and mean gestational age of their pregnant partner was 29.1 weeks. Across the three race groups (African Americans, Latinos, and Whites/Other) there were no age differences. Differences, however, were observed in their mean household income (F = 5.51; p < .01) with Latinos having significantly less income than Whites.
Measures
Masculine ideology was measured using the Masculine Role Norms Scale (Thompson & Pleck, 1986). Male role norms were assessed by respondents’ agreement or disagreement with 25 belief statements about men’s expected behavior. Each statement was scored on a 7-point Likert-type scale ranging from 1 (strongly disagree) to 7 (strongly agree). This scale measures three masculine norms: “Status” (11 items), “Toughness” (8 items), and “Antifemininity” (7 items). The statements attended to the belief that men should acquire skills that warrant respect and admiration, become mentally and physically tough, and avoid anything feminine. Reliability analyses identified that one item (It is good to teach a boy to cook) on the “antifemininity” norms factor had a low item-total correlation and was dropped from the scale. Reliability for the “status” norm factor was very good (α = .90) and adequate for the “toughness” norms factor (α = .74) and “antifemininity” norms factor (α = .77).
Healthy behavior was measured by examining the respondents’ response to behavioral questions about their exercise, eating, alcohol, and substance use.
Exercise behavior was measured using two items from the WAVE assessment on activity (Gans et al., 2003). Two questions were adapted from the WAVE assessment tool, with the prefix “In the average week how often do you.” Participants were asked how often they do moderate activity (e.g., walking briskly, jogging, swimming, biking, dancing, etc.) and lifestyle activities (e.g., taking the stairs instead of the elevator, walking to the store instead of driving, etc.). Responses ranged from never, 1 to 2 days, 3 to 4 days, 5 6 days and every day. Responses were summed to form a total score. Given that it was a two-item measure, alpha was not calculated.
Eating habits were assessed using questions from the Rapid Eating and Activity Assessment for Patients (REAP; Gans et al., 2003). This measure has moderately high rankings on usefulness, ease, practicality, and helpfulness. It has excellent test–retest reliability and is correlated with other measures and intake of nutrients (Gans et al., 2003; Gans et al., 2006). Participants indicated on a 5-point scale ranging from never to every day how often in an average week they performed each diet-related activity. Two subscales were created with two items each: eating fruits and vegetables (fruits, vegetables), and eating junk food (fried food, fast food).
Alcohol and substance use were measured using the Recreational Drug Use Scale (Halkitis & Parsons, 2002). This measure, which has been reliably used in other settings, measures any use in the past 3 months for each substance: alcohol, cigarettes, marijuana, and hard drugs (e.g., crack, heroin, methamphetamines, and other hard drugs; Greenwood et al., 2001; Halkitis & Parsons, 2002).
Data Analysis
Frequencies and means were conducted to describe the sample. To examine the effects of race, controlling for age and income, on the three masculinity subscales a profile analysis using repeated measures ANOVA was conducted. Race was considered a between-subjects variable and the subscales of masculinity as a within-subjects variable. We controlled for age, income, and education.
To assess the effects of the masculinity subscales on health behaviors, controlling for demographics a series of regression analyses were conducted. For the categorical variables of any substance use in the past 3 months (alcohol, smoking, marijuana, and hard drug use) logistic regression analyses were conducted. For the continuous variables of exercise and eating fruits and vegetables, and eating junk food, linear regressions were conducted.
Finally, to assess the possible moderating effect of race, race by masculinity subscales were entered one at a time. Significant interactions were added to the final model. Simple effects were conducted to interpret significant interactions.
Results
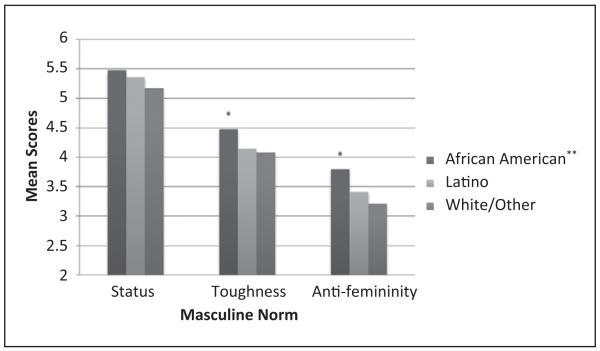
Results of the profile analysis observed significant differences between the three masculine norms, F = 5.96, p = .003 with the highest scores for “status” and the lowest scores for “antifemininity” (see Figure 1). There was a significant masculine norm by race interaction indicating that the masculinity profiles differed by race (F = 2.56, p = .038). African Americans had higher levels of endorsement of the masculine norms “toughness” and “antifemininity” than Latino and White/Other (p < .05) males. There were no significant differences between Latino and White/Other males on their levels of endorsement of the masculine norm “toughness” and “antifemininity.” There were no differences between racial groups on the endorsement of the masculine norm “status” (see Figure 1).
Figure 1. Masculinity norms by race.
*p < .05. **p < .01.
A series of logistic and multiple regression equations were completed to evaluate how masculinity predicted health behaviors. Higher endorsement of the masculine norm “toughness” was significantly related to drinking, marijuana use, hard drug use, and eating junk food. It also approached significance for smoking and exercise. A higher level of endorsement of the masculine norm “status” was significantly related to the absence of marijuana use and eating fruits and vegetables. Increased endorsement of this norm approached significance for predicting the absence of using alcohol or hard drugs. Finally, higher levels of the masculine norm “antifemininity” was significantly related to less exercise and junk food consumption (see Tables 1 and 2).
Table 1.
Logistic Regression Analysis of Masculine Norms Predicting Substance Use
| Predictor | β | SE β | Wald’s χ2 | df | p | eβ(odds ratio) |
|---|---|---|---|---|---|---|
| Alcohol use by masculine norms | ||||||
| Constant | −2.587 | 1.025 | 6.369 | 1 | .012 | 0.075 |
| Status | −0.245 | 0.131 | 3.469 | 1 | .063 | 0.78 |
| Toughness | 0.545 | 0.158 | 11.932 | 1 | .001 | 1.725 |
| Antifemininity | −0.096 | 0.130 | 0.540 | 1 | .463 | 0.909 |
| Likelihood ratio test: χ2 = 13.964, df = 3, p = .003 | ||||||
| Cigarette use by masculine norms | ||||||
| Constant | −2.310 | 0.987 | 5.470 | 1 | .019 | 0.099 |
| Status | −0.072 | 0.129 | 0.311 | 1 | .577 | 0.931 |
| Toughness | 0.278 | 0.148 | 3.538 | 1 | .060 | 1.321 |
| Antifemininity | −0.042 | 0.126 | 0.113 | 1 | .737 | 0.958 |
| Likelihood ratio test: χ2 = 4.227, df = 3, p = .238 | ||||||
| Marijuana use by masculine norms | ||||||
| Constant | −0.512 | 0.962 | 0.283 | 1 | .595 | 0.599 |
| Status | −0.269 | 0.134 | 4.030 | 1 | .045 | 0.764 |
| Toughness | 0.314 | 0.156 | 0.406 | 1 | .044 | 1.370 |
| Antifemininity | −0.020 | 0.131 | 0.025 | 1 | .876 | 0.980 |
| Likelihood ratio test: χ2 = 11.974, df = 4, p = .018 | ||||||
| Hard drug use by masculine norms | ||||||
| Constant | −4.923 | 1.983 | 6.163 | 1 | .013 | 0.007 |
| Status | −0.550 | 0.295 | 3.476 | 1 | .062 | 0.577 |
| Toughness | 0.847 | 0.359 | 5.555 | 1 | .018 | 2.333 |
| Antifemininity | 0.072 | 0.275 | 0.069 | 1 | .793 | 1.075 |
| Likelihood ratio test: χ2 = 8.014, df = 3, p = .046 | ||||||
Table 2.
Masculinities Predicting Health-Promoting Behaviors
| Eating Fruits and Vegetables; B | Eating Junk Food; B | Exercise; B | |
|---|---|---|---|
| Covariates | |||
| Race | |||
| African | Rrference | Rrference | Rrference |
| American | |||
| Hispanic | −.137 (.131) [−.394, .120] | −.051 (.106) [−.157, .259] | −.185 (.155) [−.489, .120] |
| White/Other | .082 (.178) [−.268, .433] | −.484 (.144)** [.200, .768] | −.269 (.211) [−.684, .146] |
| Masculinity norms | |||
| Status | .154 (.062)* [.035, .274] | −.014 (.049) [−.111, .083] | .07 (.07) [−.072, .211] |
| Toughness | −.106 (.070) [−.243, .032] | .197 (.057)** [.085, .308] | .15 (.08)† [−.010, .316] |
| Antifemininity | −.030 (.061) [−.149, .090] | −.104 (.049)* [−.201, −.008] | −.19 (.07)** [−.333, −.051] |
p < .10.
p < .05.
p < .01
p < .001.
Next, we assessed whether race modified these effects. Results identified significant interactions with race and masculine norms on smoking and marijuana use. There was a significant race by masculine norm “status” interaction, χ2(df = 2) = 8.57, p = .01, on smoking. Simple effects observed that higher masculine norm “status” related to less smoking for African American (odds ratio [OR] = 0.53, confidence interval [CI] = [0.34, 0.845], p = .007) but not Latino (OR = 1.23, CI = [0.79, 1.96], p = .31) and White/Other young men (OR = 1.59, CI = [0.68, 3.75], p = .29). There was a significant race by masculine norm “status” effect interaction, (χ2(df = 2) = 6.89, p = .03, on marijuana use. Simple effects observed that masculine norm “status” related to less marijuana use for African American (OR = 0.53, CI = [0.33, 0.83], p = .006) but not Latino (OR = .92, CI = [0.60, 1.40], p = .69) and White/Other young men (OR = 1.51, CI = [0.61, 3.76], p = .38).
Results also observed significant interactions with race and masculine norms on eating junk food. There was a significant race by masculine norm “antifemininity” interaction (F = 3.71, p = .03). Simple effects identified that masculine norm “antifemininity” related to less junk food consumption for Latino (β = −.35, p = .001) but not African American (β = −.03, p = .77) and White/Other (β = −.16, p = .46) young men.
Discussion
This study sought to examine how the masculine norms of “status,” “toughness,” and “antifemininity” related to substance use and health behaviors for a diverse group of young men transitioning into fatherhood. Consistent with extant theories on masculinities and health (Addis & Mahalik, 2003; Courtenay, 2000b; Mankowski & Maton, 2010) this research supported the idea that some masculinities were more related to negative health behaviors. In this research, the masculine norm “toughness” was related to more negative health behaviors. This result appears to suggest that young men who endorse the idea that a man is to be emotionally, physically, and mentally tough may also engage in health-undermining behaviors. These health behaviors may further complicate their experience and have long-term health implications.
Whereas the masculine norm “toughness” related to negative health behaviors for these diverse young men, other masculine norms were found to be protective. The masculine norm “status” was protective against substance use and related to the consumption of more fruits and vegetables for this diverse sample of young men transitioning into fatherhood. This observation seems to suggest that for those young men who adhered to the views that a man needs to be successful in his work and family life may engage in protective health behaviors to provide a positive role model and example. This was even more pronounced for the young, expecting, African American fathers. For this group, their endorsement of masculine norm “status” resulted in less smoking and marijuana use than their Latino and White counterparts. This may be associated with a greater acceptance of the schemas that associate their masculine norm “status” with being a productive citizen, something that cannot be achieved if one is actively involved in substance use and other health-undermining behaviors. This is a promising finding for the African American sample in this study and supports previous research that demonstrates that masculinities can and may play a protective role in some contexts (Addis & Mahalik, 2003; Mankowski & Maton, 2010; Wade, 2008).
The findings of this study suggest that the masculine norm “antifemininity” was not related to most of the substance use and health behaviors examined in this study except for exercise. Those who endorsed more antifeminine norms were less likely to exercise. Furthermore, because of the interaction, Latino young men who endorsed higher masculine norms “antifemininity” reported less junk food consumption. This too is an important observation. Closer analyses of these results are warranted. Understanding how the adherence to the views that behaviors that could be interpreted as “feminine” result in less exercise and less junk food consumption would advance our intervention strategies for young men. Possible explanations may include the view that “real men”—men who do ’not engage in women’s work or activities, do ’not need to engage in activities such as exercise. Making links like the one described through research would help clarify how masculinities, such as “antifemininity” and health-promoting behaviors are cognitively linked.
Unique, however, to these findings were the way each masculine norm examined had complex relationships to health behaviors. Specifically, endorsement of the masculine norm “toughness” was mostly related to substance use. It was, however, also related to exercise. In addition, the masculine norm “antifemininity” was related to less exercise and less junk food consumption. These observations support the view that although masculinities do not confer only risks or rewards, they may simultaneously confer both (Levant, 2008). Understanding what are the ways that the positive health outcomes are supported by adherence to these views and disentangling them from the negative health consequences may help us better understand and develop more effective and targeted interventions.
Finally, the research presented supports the notion that young men of color, and more specifically, African American young men, may adhere to these scripts at a rate higher than that of their Latino and White counterparts. This observation raises questions about the unique meaning for African American young men, and men of color more specifically, given that they cannot, according to more hegemonic notions of masculinity, achieve the coveted ideal masculine role (Courtenay, 2000a; Sabo & Gordon, 1995; Sabol, Coulton, & Polousky, 2004; Wade, 2008). Although this observation is true, researchers (see Courtenay, 2000a) have argued that because of their social status young men of color may endorse the masculine norms they deem valued more rigidly than their White counterparts who have access to other means of enacting their masculinity. This sample was composed predominantly of young men of color. The results also raise questions about the relationship between their impending fatherhood status, masculinities, and behaviors that may undermine their current and long-term health. Understanding how stressors, such as fatherhood, affect the health and long-term health behaviors of men would be important as they mark this important transition. Longitudinal studies to observe masculinity as young men, and men in general, transition into fatherhood and other important developmental transitions would help answer these questions.
Limitations
Although the results presented only give small window into the role of masculinities and health for young expecting fathers, there are some limitations that need to be examined and addressed. First, we used a cross-sectional approach. This strategy does not allow us to characterize the temporal relationship between the observations presented. Longitudinal studies may help us better characterize these relationships for diverse young men who are about to be fathers. Second, this information was also collected through self-report, which in turn increases the probability of socially desirable responding. We used audio computer-assisted self-interview to reduce the likelihood of social desirability. Third, we cannot generalize these observations to young men who are not transitioning into fatherhood, choose to end the relationship with their pregnant partners, and not residing in urban settings. Finally, given that 28% of eligible participants did not enroll in the study, there may be masculine norm and health differences in the nonparticipant group that were not measured.
Implications
The impact of masculinity and health was present for this sample of expecting fathers. Given the role transition occurring, this may be an opportune time to develop the coping strategies, provide support, and expand how they conceptualize what it means to be a man. Consideration of the role of social modeling, community expectations, and peer influence cannot be ignored, given their developmental status. We should also not lose sight of the main goal, which is to increase the short- and long-term health of young expecting fathers and its implications for their children (Fiscella, 2010). Helping the young men model with their partners more preventive health behaviors may have a positive impact beyond their health. There have been a number of calls for strategies to engage fathers whose partners are pregnant, prenatally and postnatally. Teaching health behaviors within a masculine consistent framework can have implications for the functioning of the young men in fulfilling their roles and help to support their pregnant partners in their efforts to be healthy for their unborn child. Research into disentangling the health-promoting and health-undermining aspects of masculinities would also aid in the development of gendered protocols focused on men.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Supported by a grant to Dr. Trace Kershaw from the National Institutes of Mental Health (1R01MH075685) and a diversity supplement grant to Dr. Derrick Gordon (1R01MH075685-S1). Additional support from the Center for Interdisciplinary Research on AIDS (5P30MH062294).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Addis ME, Mahalik JR. Men, masculinity, and the contexts of help seeking. American Psychologist. 2003;58:5–14. doi: 10.1037/0003-066x.58.1.5. [DOI] [PubMed] [Google Scholar]
- Anderson KL. Theorizing gender in intimate partner violence research. Sex Roles. 2005;52:853–865. [Google Scholar]
- Anonymous Excess mortality in Harlem [Comment letter] New England Journal of Medicine. 1990;322:1606–1607. doi: 10.1056/NEJM199005313222213. [DOI] [PubMed] [Google Scholar]
- Barker G, Ricardo C. Young men and the construction of masculinity in sub-Saharan Africa: Implications for HIV/AIDS, conflict and violence. World Bank; Washington, DC: 2005. [Google Scholar]
- Bartlett EE. The effects of fatherhood on the health of men: A review of the literature. Journal of Men’s Health & Gender. 2004;1:159–169. doi:10.1016/j.jmhg.2004.06.004. [Google Scholar]
- Braveman P, Egerter S. Overcoming obstacles to health. Robert Wood Johnson Foundation; Princeton, NJ: 2008. [Google Scholar]
- Buist A, Morse CA, Durkin S. Men’s adjustment to fatherhood: Implications for obstetric health care. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2003;32:172–180. doi: 10.1177/0884217503252127. doi:10.1177/0884217503252127. [DOI] [PubMed] [Google Scholar]
- Cohen MA, Aladjem A, Horton A, Lima J, Palacios A, Hernandez I, Mehta P. How can we combat excess mortality in Harlem: A one day survey of substance abuse in adult general care. International Journal of Psychiatry in Medicine. 1991;21:369–378. doi: 10.2190/PL2W-DGB6-MAWH-V8F0. [DOI] [PubMed] [Google Scholar]
- Condon JT, Boyce P, Corkindale CJ. The First-Time Fathers Study: A prospective study of the mental health and wellbeing of men during the transition to parenthood. Australian and New Zealand Journal of Psychiatry. 2004;38:56–64. doi: 10.1177/000486740403800102. [DOI] [PubMed] [Google Scholar]
- Connell RW, Messerschmidt JW. Hegemonic masculinity: Rethinking the concept. Gender & Society. 2005;19:829–859. [Google Scholar]
- Cooper RS. Health and the social status of blacks in the United States. Annals of Epidemiology. 1993;3:137–144. doi: 10.1016/1047-2797(93)90126-o. [DOI] [PubMed] [Google Scholar]
- Courtenay WH. Constructions of masculinity and their influence on men’s well-being: A theory of gender and health. Social Science & Medicine. 2000a;50:1385–1401. doi: 10.1016/s0277-9536(99)00390-1. [DOI] [PubMed] [Google Scholar]
- Courtenay WH. Engendering health: A social constructionist examination of men’s health beliefs and behaviors. Psychology of Men & Masculinity. 2000b;1:4–15. [Google Scholar]
- Courtenay WH. A global perspective on the field of men’s health: An editorial. International Journal of Men’s Health. 2002;1:1–13. [Google Scholar]
- Emslie C, Ridge D, Ziebland S, Hunt K. Men’s accounts of depression: Reconstructing or resisting hegemonic masculinity? Social Science & Medicine. 2006;62:2246–2257. doi: 10.1016/j.socscimed.2005.10.017. [DOI] [PubMed] [Google Scholar]
- Fiscella K. Breaking the cycle of poverty and poor health: Paediatricians can make a difference. Acta Paediatrica. 2010;99:648–650. doi: 10.1111/j.1651-2227.2010.01704.x. [DOI] [PubMed] [Google Scholar]
- Fullilove RE, Fullilove MT, Northridge ME, Ganz ML, Bassett MT, McLean DE, McCord C. Risk factors for excess mortality in Harlem. Findings from the Harlem Household Survey. American Journal of Preventive Medicine. 1999;16(3 Suppl.):22–28. doi: 10.1016/s0749-3797(98)00146-9. [DOI] [PubMed] [Google Scholar]
- Galdas PM, Cheater FM, Marshall P. Men and health help-seeking behaviour: Literature review. Journal of Advanced Nursing. 2005;49:616–623. doi: 10.1111/j.1365-2648.2004.03331.x. [DOI] [PubMed] [Google Scholar]
- Gans KM, Risica PM, Wylie-Rosett J, Ross EM, Strolla LO, McMurray J, Eaton CB. Development and evaluation of the nutrition component of the Rapid Eating and Activity Assessment for Patients (REAP): A new tool for primary care providers. Journal of Nutrition Education and Behavior. 2006;38:286–292. doi: 10.1016/j.jneb.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Gans KM, Ross E, Barner CW, Wylie-Rosett J, McMurray J, Eaton C. REAP and WAVE: New tools to rapidly assess/discuss nutrition with patients. Journal of Nutrition. 2003;133:556S–562S. doi: 10.1093/jn/133.2.556S. [DOI] [PubMed] [Google Scholar]
- Greenberg M, Schneider D. Violence in American cities: Young black males is the answer, but what was the question? Social Science & Medicine. 1994;39:179–187. doi: 10.1016/0277-9536(94)90326-3. [DOI] [PubMed] [Google Scholar]
- Greenwood GL, White EW, Page-Shafer K, Bein E, Osmond DH, Paul J, Stall RD. Correlates of heavy substance use among young gay and bisexual men: The San Francisco Young Men’s Health Study. Drug and Alcohol Dependence. 2001;61:105–112. doi: 10.1016/s0376-8716(00)00129-0. doi:10.1016/s0376-8716(00)00129-0. [DOI] [PubMed] [Google Scholar]
- Halkitis PN, Parsons JT. Recreational drug use and HIV-risk sexual behavior among men frequenting gay social venues. Journal of Gay & Lesbian Social Services. 2002;14(4):19–38. [Google Scholar]
- Heron M. Deaths: Leading causes for 2007. National Vital Statistics Reports. 2011;59(8):1–96. [PubMed] [Google Scholar]
- Lane TS, Clay CM. Meeting the service needs of young fathers. Child & Adolescent Social Work Journal. 2000;17:35–54. [Google Scholar]
- Lee C, Owens RG. The psychology of men’s health. Open University Press; Buckingham, England: 2002. [Google Scholar]
- Levant RF. How do we understand masculinity? An editorial. Psychology of Men & Masculinity. 2008;9:1–4. doi:10.1037/1524-9220.9.1.1. [Google Scholar]
- Mahalik JR, Burns S, Syzdek M. Masculinity and perceived normative health behaviors as predictors of men’s health behaviors. Social Science & Medicine. 2007;64:2201–2209. doi: 10.1016/j.socscimed.2007.02.035. [DOI] [PubMed] [Google Scholar]
- Mahalik JR, Good GE, Englar-Carlson M. Masculinity scripts, presenting concerns, and help seeking: Implications for practice and training. Professional Psychology: Research and Practice. 2003;34:123–131. [Google Scholar]
- Mahalik JR, Lagan H, Morrison JA. Health behaviors and masculinity in Kenyan and U.S. male college students. Psychology of Men & Masculinity. 2006;7:191–202. [Google Scholar]
- Mankowski ES, Maton KI. A community psychology of men and masculinity: Historical and conceptual review. American Journal of Community Psychology. 2010;45:73–86. doi: 10.1007/s10464-009-9288-y. [DOI] [PubMed] [Google Scholar]
- Marsiglio W, Pleck JH. Fatherhood and masculinities. In: Kimmel MS, Hearn J, Connell RW, editors. Handbook of studies on men and masculinities. Sage; Thousand Oaks, CA: 2005. pp. 249–269. [Google Scholar]
- McCord C, Freeman HP. Excess mortality in Harlem [Comparative study] New England Journal of Medicine. 1990;322:173–177. doi: 10.1056/NEJM199001183220306. [DOI] [PubMed] [Google Scholar]
- McCreary DR, Newcomb MD, Sadava SW. The male role, alcohol use, and alcohol problems: A structural modeling examination in adult women and men. Journal of Counseling Psychology. 1999;46:109–124. [Google Scholar]
- McKelley RA, Rochlen AB. Conformity to masculine role norms and preferences for therapy or executive coaching. Psychology of Men & Masculinity. 2010;11:1–14. [Google Scholar]
- O’Neil JM, Helms BJ, Gable RK, David L, Wrightsman LS. Gender-role conflict scale: College men’s fear of femininity. Sex Roles. 1986;14:335–350. [Google Scholar]
- Ravenell JE, Whitaker EE, Johnson WE, Jr., Ravenell JE, Whitaker EE, Johnson WE., Jr. According to him: Barriers to healthcare among African-American men’. Journal of the National Medical Association. 2008;100:1153–1160. doi: 10.1016/s0027-9684(15)31479-6. [DOI] [PubMed] [Google Scholar]
- Sabo DF, Gordon DF, editors. Men’s health and illness: Gender, power, and the body. Sage; Thousand Oaks, CA: 1995. [Google Scholar]
- Sabol W, Coulton C, Polousky E. Measuring child maltreatment risk in communities: A life table approach. Child Abuse & Neglect. 2004;28:967–983. doi: 10.1016/j.chiabu.2004.03.014. doi:http://dx.doi.org/10.1016/j.chiabu.2004.03.014. [DOI] [PubMed] [Google Scholar]
- Thompson EH, Pleck JH. The structure of male role norms. American Behavioral Scientist. 1986;29:531–543. doi:10.1177/000276486029005003. [Google Scholar]
- Treadwell HM, Ro M. Poverty, race, and the invisible men. American Journal of Public Health. 2003;93:705–707. doi: 10.2105/ajph.93.5.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade JC. Masculinity ideology, male reference group identity dependence, and African American men’s health-related attitudes and behaviors. Psychology of Men & Masculinity. 2008;9:5–16. [Google Scholar]
- Weinman ML, Buzi RS, Smith PB. Addressing risk behaviors, service needs, and mental health issues in programs for young fathers. Families in Society. 2005;86:261–266. [Google Scholar]
- Weinman ML, Smith PB, Buzi RS. Young fathers: An analysis of risk behaviors and service needs. Child & Adolescent Social Work Journal. 2002;19:437–453. [Google Scholar]
- Williams DR, Collins C, editors. U.S. socioeconomic and racial differences in health. Jossey-Bass; San Francisco, CA: 2002. [Google Scholar]