Abstract
Purpose
The purpose of this retrospective study was to examine the association of facet tropism and progressive facet arthrosis (PFA) after lumbar total disc replacement (TDR) surgery using ProDisc-L®.
Methods
A total of 51 segments of 42 patients who had undergone lumbar TDR using ProDisc-L® between October 2003 and July 2007 and completed minimum 36-month follow-up period were retrospectively reviewed. The changes of facet arthrosis were categorized as non-PFA and PFA group. Comparison between non-PFA and PFA group was made according to age, sex, mean follow-up duration, grade of preoperative facet arthrosis, coronal and sagittal prosthetic position and degree of facet tropism. Multiple logistic regression analysis was also performed to analyze the effect of facet tropism on the progression of facet arthrosis.
Results
The mean age at the surgery was 44.43 ± 11.09 years and there were 16 males and 26 females. The mean follow-up period was 53.18 ± 15.79 months. Non-PFA group was composed of 19 levels and PFA group was composed of 32 levels. Age at surgery, sex proportion, mean follow-up period, level of implant, grade of preoperative facet arthrosis and coronal and sagittal prosthetic position were not significantly different between two groups (p = 0.264, 0.433, 0.527, 0.232, 0.926, 0.849 and 0.369, respectively). However, PFA group showed significantly higher degree of facet tropism (7.37 ± 6.46°) than that of non-PFA group (3.51 ± 3.53°) and p value was 0.008. After adjustment for age, sex and coronal and sagittal prosthetic position, multiple logistic regression analysis revealed that facet tropism of more than 5° was the only significant independent predictor of progression of facet arthrosis (odds ratio 5.39, 95 % confidence interval 1.251–19.343, p = 0.023).
Conclusions
The data demonstrate that significant higher degree of facet tropism was seen in PFA group compared with non-PFA group and facet tropism of more than 5° had a significant association with PFA after TDR using ProDisc-L®.
Keywords: Facet tropism, Progressive facet arthrosis, Lumbar total disc replacement, ProDisc-L®
Introduction
Although lumbar total disc replacement (TDR) is known for its advantage of motion preservation, several authors have indicated that kinematic changes in quality and quantity of motion following TDR could affect adversely on facet joint at index segment and consequently lead to the progression of facet joint arthrosis (PFA) [1–5]. For this reason, significant facet disease has been considered as one of the ten primary contraindications to TDR [6], and Bertagnoli et al. [7] also suggested that osteoarthritic change of facet joint was poor indication to disc arthroplasty.
Facet tropism is defined as asymmetry in both the facet joint angles [8]. It is postulated that when tropism exists, asymmetric axial rotation of motion segment would occur [9, 10] and many authors suggested that this anatomic difference of facet angle was a predisposing factor for the development of diverse pathology including disc disease, spondylolisthesis and facet degeneration [9, 11, 12].
So far, most of previous studies have focused on the relationship between facet tropism and degenerative spinal disease as already mentioned above, while there has been no study dealing with the association between facet tropism and PFA after lumbar TDR surgery as far as we know.
We hypothesized that if artificial disc was designed to provide a symmetric axial rotatory movement and if it was implanted at both coronally and sagittally proper position, asymmetric loading caused by facet tropism will significantly affect on the fate of facet joint after lumbar TDR surgery. To verify this, we present our result obtained from retrospective study focusing on the association of facet tropism and PFA after lumbar TDR surgery.
Materials and methods
Forty-four patients who underwent lumbar TDR surgery for degenerative disc disease (DDD) between October 2003 and July 2007 and could be followed for at least 36 months were enrolled in this study. All patients underwent lumbar TDR using ProDisc-L® (Synthes Spine, West Chester, PA, USA) by single surgeon (C.K. Park). The exclusion criteria included spondylolysis, spondylolisthesis, spinal stenosis, advanced facet arthrosis, osteoporosis, prior fusion, obesity, pseudoarthrosis, scoliosis and deficient posterior element.
Plain radiograph was obtained preoperatively, postoperative immediately and at the final follow-up. CT scan was used to evaluate change of facet arthrosis both before surgery and at the final follow-up.
Four grades of facet joint arthrosis were defined using the Pathria grading system [13] which was based on the findings of CT scan, preoperatively and at the time of minimum 36 months follow-up. The interpretation and grading of facet arthrosis were assigned to a clinical fellow who was completely unaware of any information of this study. The PFA was defined as the increase in the degeneration grade of the facet joints after TDR and the all segments were divided into two groups, non-PFA group and PFA group. Between these two groups, comparisons of age at surgery, sex proportion, mean follow-up duration, level of implant, grade of preoperative facet arthrosis, coronal and sagittal prosthetic position and difference of facet angles were made and analyzed.
Preoperatively, the facet joint angle relative to the sagittal plane at index level was measured on the axial CT images using the method described by Noren et al. [12] (Fig. 1). Axial CT scan images that bisected the intervertebral disc were obtained. On an axial image, two lines were made, one was reference line that passed through the center of the disc and the base of the spinous process and the other was facet line that connected the two points, the anteromedial and posterolateral margin of the superior articular facet. Then, the difference between the right and left facet angle of each segment was calculated. For this study, we defined facet tropism as the bilateral angle difference greater than 5° as in Noren et al.’s study [12] and grouped into two groups, non-facet tropism and facet tropism group.
Fig. 1.

Axial CT scan image shows the method of facet angle measurement. A reference line (A) was drawn between the center of the disc and the base of the spinous process. Right and left facet line (B and B′, respectively) passed through the two points, the anteromedial and posterolateral margin of the superior articular facet. The angle between the reference line and the facet line was measured for each side of spine (a and b)
On postoperative radiographic image, the sagittal and coronal positions of prosthesis were assessed. The position of the prosthesis in the coronal plane was defined as the ratio of the distance between the center of the lower keel and the nearer lateral margin of the upper endplate to the whole distance of the upper endplate in the caudal vertebra in anteroposterior projection of radiograph (Fig. 2A) and categorized into two groups according to the ratio (midline group <0.025, off the midline group >0.025). The position of the prosthesis in the sagittal plane was defined as the ratio of the distance between the posterior margin of the upper endplate and the posterior margin of the prosthesis divided by the length of the upper endplate of the caudal vertebral body (Fig. 2B) and these ratios were classified into two groups (anterior group <0.100, posterior group >0.100).
Fig. 2.
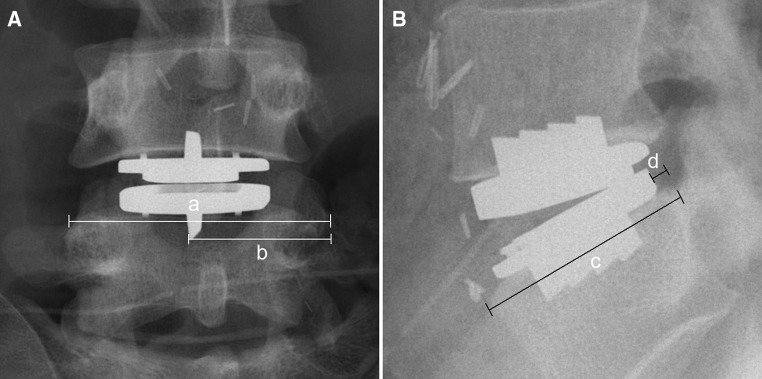
Line drawn on a plain radiograph showing the radiographic determination for defining the prosthesis position on the coronal and sagittal plane. The a and b represent the width of the upper endplate of the caudal vertebral body and the distance between the center of lower keel and the nearer lateral margin of the upper endplate of the caudal vertebra, respectively. The relative prosthesis position on frontal plane was defined as the ratio of the difference of a/2 and b and a; ((a/2 − b)/a). The position of the prosthesis in the sagittal plane was defined as the ratio of the distance between the posterior margin of the upper endplate and the posterior margin of the prosthesis divided by the length of the upper endplate of the caudal vertebral body (d/c)
Radiologic measurements were obtained on a digital radiographic image displayed on a Picture Archiving and Communication Systems (PACS) terminal (Marosis 2003, Seoul, Korea), and the facet angle and the position of prosthesis were measured using an automated program of the PACS computer software.
The data were analyzed using SPSS for Windows (version 18.0.0; SPSS Inc., USA). In the comparison between non-PFA and PFA group, χ2 test was used for categorical variable and t test for continuous variables. Multiple logistic regression analysis was used to analyze the associations between PFA and facet tropism while adjusted for age, sex, level of implant and coronal and sagittal position. Based on odds ratio and confidence interval from regression analysis, relative risk of facet tropism on PFA after TDR surgery and adequacy of sample size would be evaluated.
In prior to analyze, each factor was converted into a categorical variable (age: more than 40 or not, coronal position: midline and off the midline group, sagittal position: anterior and posterior group, facet tropism: more than 5° or not) except for sex and level of implant. The data were expressed as mean and standard deviation (mean ± SD) and the result was considered statistically significant if the p value was <0.05.
Results
The patient population was composed of 16 males (38.1 %) and 26 females (61.9 %). The mean age was 44.43 ± 11.09 years (range 24–69 years) and the mean duration of follow-up was 53.18 ± 15.79 months. Nine patients underwent two levels of TDR surgery and totally 51 implanted segments were analyzed. Twenty-four cases of TDR (47.0 %) were performed at the level of L4–5 and there were 27 cases of TDR (52.9 %) at L5/S1 level. The mean angle of facet tropism at L4–5 level was 5.60 ± 4.44° and 6.26 ± 6.91° at L5–S1 level, which showed no statistically significant difference (p = 0.703).
In the overall population, the mean value of Pathria’s grade increased from 0.25 ± 0.48, preoperatively to 1.27 ± 1.09 at the time of final follow-up, which showed statistically significant increase (p = 0.000) and the mean degree of facet tropism was 5.93 ± 5.83°.
Non-PFA group was composed of 19 levels (37.3 %) and PFA group was composed of 32 levels (62.7 %). The results of comparisons between non-PFA and PFA groups (Table 1) showed no differences in mean age at surgery (p = 0.264), sex proportion (p = 0.433), mean follow-up duration (p = 0.527), and level of implant (p = 0.232). Preoperative facet arthrosis (Pathria grade) was not significantly different (p = 0.926) between two groups as well. Both the ratio of coronal and sagittal position of prosthesis did not show significant differences (p = 0.849, 0.369) between two groups; however, the mean degree of facet tropism in PFA group (7.37 ± 6.46°) was significantly higher than that of non-PFA group (3.51 ± 3.53°, p = 0.008).
Table 1.
Comparison between non-PFA and PFA groups
| Non-PFA group (19 levels) | PFA group (32 levels) | p value | |
|---|---|---|---|
| Age at surgery (years) | 42.16 ± 10.64 | 45.78 ± 11.30 | 0.264 |
| Sex (male/female) | 8/11 | 10/22 | 0.433 |
| Mean F/U duration (months) | 51.51 ± 11.99 | 54.17 ± 17.78 | 0.527 |
| Level of implant (L4–5/L5–S1) | 11/8 | 13/19 | 0.232 |
| Preoperative facet arthrosisa | 0.26 ± 0.45 | 0.25 ± 0.50 | 0.926 |
| Coronal position (ratio) | 0.02 ± 0.01 | 0.02 ± 0.02 | 0.849 |
| Sagittal position (ratio) | 0.10 ± 0.05 | 0.11 ± 0.05 | 0.369 |
| Facet tropism (°) | 3.51 ± 3.53 | 7.37 ± 6.46 | 0.008b |
aPathria grading system
bp < 0.05
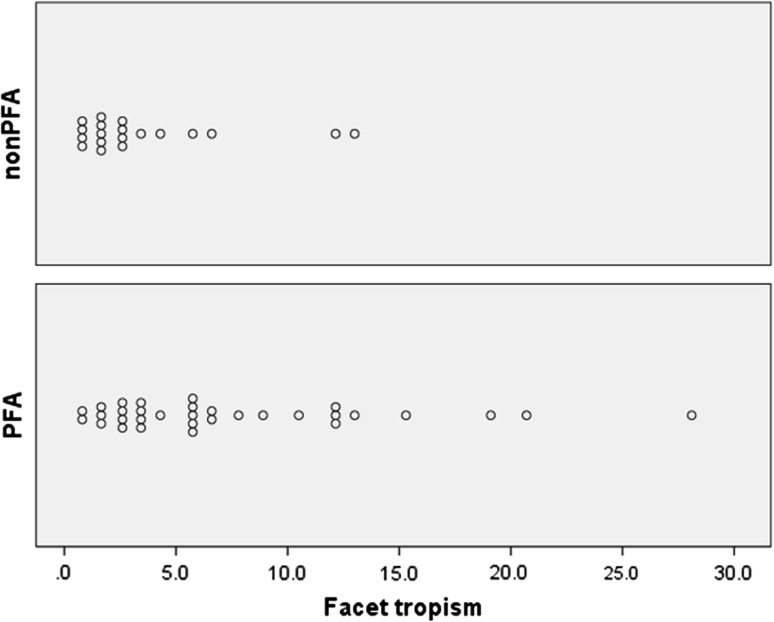
The distribution of measured angle of facet tropism in both non-PFA and PFA groups was shown in Fig. 3. While the over the half of values of facet tropism in PFA group were distributed over the 5.0°, the most of values in non-PFA group were distributed on x axis of lesser than 5.0°.
Fig. 3.
Graph showing the distribution of measured angle of facet tropism in both non-PFA and PFA groups
Table 2 shows the results of the multivariate analysis of the association between PFA and facet tropism, while adjusting for age, sex, level of implant and coronal and sagittal position. In the present study, after adjustment for age, sex, level of implant and coronal and sagittal position, facet tropism of more than 5° was significantly associated with PFA (OR 5.39, 95 % CI 1.25–19.34; p = 0.023).
Table 2.
Associations between facet tropism and PFA by multiple logistic regression analysis (adjusted for age, sex, coronal and sagittal position and level of implant)
| Variablesa | Progression of facet arthrosis | ||
|---|---|---|---|
| OR | 95 % CI | p value | |
| Age | 0.69 | 0.07–6.53 | 0.715 |
| Sex | 3.12 | 0.31–32.25 | 0.310 |
| Coronal position | 0.49 | 0.12–1.93 | 0.535 |
| Sagittal position | 0.66 | 0.18–2.36 | 0.466 |
| Level of implant | 2.59 | 0.69–9.60 | 0.154 |
| Facet tropism | 5.39 | 1.25–19.34 | 0.023 |
OR odds ratio, CI confidence interval
aFor each variable, below 40 years, male, coronally midline group, sagittally posterior group, level of L5–S1 and facet tropism lesser than 5.0° were taken as the reference
Discussion
The progression of facet arthrosis after TDR surgery has been known as one of negative side effects [1, 3, 14, 15] and considered as a reason for unsatisfactory pain relief even after successful implantation [16]. Shim et al. [3], in their comparative study of two kinds of prosthesis (CHARITE vs. ProDisc), reported 36.4 and 32 % of the facet degeneration in the CHARITE and ProDisc group, respectively. Siepe et al. [4] described the results of implantation of the ProDisc from 93 patients with 53.4 months of follow-up and reported 20.0 % of the facet degeneration. In the current study, the data revealed high prevalence of PFA observed in 26 patients (59.1 %) and 32 levels (62.7 %) compared with previous published studies [3, 4]. One possible explanation for this result could be that in our study, CT scan was used to assess the change of facet joint arthrosis rather than MR imaging. Owing to precise demonstration of osseous details, CT was believed to be more sensitive than MR imaging in the depiction of joint space narrowing and subchondral sclerosis [17] and that would seem to induce a high occurrence rate of PFA in the present study.
Regarding the clinical significance of facet tropism, highly controversial debates have existed surrounding the question of whether or not there was any significant relationship between facet tropism and the development of disc degeneration and degenerative spondylolisthesis [9, 10, 12, 18]. In addition, relations between facet tropism and facet arthrosis have been contentious issue as well [19, 20]. Grogan et al. [19], in their study with 21 cadavers, insisted that lumbar facet joint tropism did not accelerate facet joint degeneration. However, small number of specimens, smaller number of facet tropism (10 out of 104 facet joints) and not taking into account the level where facet tropism was exhibited were major limitations of their study. In the present study, there was no statistically significant difference of facet arthrosis according to the level of implant, however, individuals with PFA after TDR surgery showed statistically higher degree of facet tropism than individuals without PFA and this result was in agreement with Kong et al. [20] study.
There are various criteria of determining facet tropism. Noren et al. [12] defined facet asymmetry as a bilateral angle difference greater than 5° and some authors [18, 21] defined facet asymmetry as a bilateral angle difference greater than 1 standard deviation. We defined facet tropism to be bilateral angular asymmetry greater than 5° which was adopted from the definition of previous study [12] and according to the findings in the distribution of measured angle of the facet tropism, the most of angle of facet tropism in non-PFA group was less than 5° while the majority of PFA group distributed over the 5°.
Various factors seem to be related with PFA after TDR. The prevalence of facet arthrosis was 24 % in patients below the age of 40, however, this number increased to 44.7 % for patients above the age of 40 and these data supported the possibility of age as a attributable factor for the development of PFA after TDR [4].
Park et al. [2] followed 41 segments of TDR using ProDisc in 32 patients for 32.2 months, and reported that PFA after TDR was related to female gender and the malposition of prosthesis on coronal plane. They explained that the female was susceptible to facet arthrosis owing to high prevalence of osteoporosis, and asymmetric movement of the disc by improper position of prosthesis could cause uneven facet loading.
Not only proper position of coronal side but also sagittally well-positioned prosthesis has important implications to the facet joint as well. Dooris et al. [14] reported that when the prosthesis was implanted anteriorly, lordosis increased and the loads of facet joint were 2.5 times greater. Based on these results, they concluded that anteriorly improperly placed prosthesis could cause facet arthrosis and dysfunction.
It was reported that the ROM at the L5–S1 is lower than at other levels for the ProDisc-L® prosthesis [22] due to its firm stabilization by the iliolumbar ligaments, and theoretically, a hypermobile motion segment might contribute to the degeneration of the facet joints. Although there was no statistical relationship between PFA and the level of implantation in this study, it is important to consider the development of facet degeneration depending on its related levels of facet tropism [20].
The aforementioned variables such as age, sex, position of prosthesis and level of implantation can play a role as a confounding factor in determining the factors associated with PFA after TDR. In this study, adjusting these factors, multivariate analysis revealed that only facet tropism of more than 5° had a significant association with PFA after TDR. One possible explanation for this result could be that the combination of altered biomechanics of implanted segment and predisposing morphological joint configuration, that is facet tropism, leads to or accelerates the development of facet instability and degeneration. To implant disc prosthesis, resection of both anterior longitudinal ligament (ALL) and anterior annulus is required. As a direct result of loss of these structures, a significant increases in range of axial rotation and facet loading would occurred [23, 24], and a motion segment where disc prosthesis was implanted became vulnerable to rotatory instability. By nature, the role of facet joint is to limit the axial rotation and maintain the stability of motion segment [25], however, with asymmetry of facet joint, uneven rotatory movement would occur [10] and that would be more worsened by absence of ALL and anterior annulus after prosthesis implantation and accordingly, accelerate or give birth to the development of PFA after TDR.
Many studies have suggested that pathologic condition of facet joint was one of the contraindications to TDR surgery [6, 7]. However, as far as we know, there has been no study investigating the association between inherent anatomic variations of facet joint, such as facet tropism and PFA after TDR surgery. Although this study revealed statistically significant associations between facet tropism and PFA after TDR surgery, we thought that it is premature and hasty to conclude facet tropism of more than 5° could be one of the contraindications to lumbar TDR surgery. To verify this, randomized designed, larger sample sized study with various prostheses will be required.
There were several limitations to the current study. First, this is a retrospective not randomized study. Second, methodologically, there were no considerations for inter- or intra-observer reliability and this might cause lack of reliability and accuracy in this study. However, a third party who was not informed with the purpose and hypothesis of this study interpreted the change of facet joint arthrosis and this would minimize the chances of bias and could acquire its reliability. Lack of consideration about single or multi-level implantation of TDR is the third limitation of current study. Finally, confidence interval of multivariate analysis was too wide (CI 1.25–19.34), although p value was <0.05. We assume that a low lumber of cases (n = 51) underpowered our study. In the future, prospective analysis with a larger number of patients being remedied its limitations should be conducted.
Conflict of interest
None.
References
- 1.van-Ooij A, Oner FC, Verbout AJ. Complications of artificial disc replacement: a report of 27 patients with the SB Charité disc. J Spinal Disord. 2003;16:369–383. doi: 10.1097/00024720-200308000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Park C, Ryu K, Jee W. Degenerative changes of discs and facet joints in lumbar total disc replacement using ProDisc II: minimum two-year follow-up. Spine (Philadelphia, Pa 1976) 2008;33:1755–1761. doi: 10.1097/BRS.0b013e31817b8fed. [DOI] [PubMed] [Google Scholar]
- 3.Shim CS, Shin H, Kang HS, Choi W, Jung B, Choi G, Ahn Y, Lee S, Lee HY (2007) Charite versus ProDisc: a comparative study of a minimum 3-year follow-up 32(9):1012–1018 [DOI] [PubMed]
- 4.Siepe CJ, Zelenkov P, Sauri Barraza J, Szeimies U, Grubinger T, Tepass A, Stbler A, Mayer MH. The fate of facet joint and adjacent level disc degeneration following total lumbar disc replacement: a prospective clinical, X-ray, and magnetic resonance imaging investigation. Spine (Philadelphia, Pa 1976) 2010;35:1991–2003. doi: 10.1097/BRS.0b013e3181d6f878. [DOI] [PubMed] [Google Scholar]
- 5.Lemaire J, Carrier H, Sariali EW, Sari Ali EF, Skalli W, Lavaste F. Clinical and radiological outcomes with the Charité artificial disc: a 10-year minimum follow-up. J Spinal Disord. 2005;18:353–359. doi: 10.1097/01.bsd.0000172361.07479.6b. [DOI] [PubMed] [Google Scholar]
- 6.Huang RC, Lim MR, Girardi FP, Cammisa FP. The prevalence of contraindications to total disc replacement in a cohort of lumbar surgical patients. Spine (Philadelphia, Pa 1976) 2004;29:2538–2541. doi: 10.1097/01.brs.0000144829.57885.20. [DOI] [PubMed] [Google Scholar]
- 7.Bertagnoli R, Kumar S. Indications for full prosthetic disc arthroplasty: a correlation of clinical outcome against a variety of indications. Eur Spine J. 2002;11:S131–S136. doi: 10.1007/s00586-002-0428-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brailsford JF. Deformities of the lumbosacral region of the spine. Br J Surg. 1929;16:562–627. doi: 10.1002/bjs.1800166405. [DOI] [Google Scholar]
- 9.Boden SD, Riew KD, Yamaguchi K, Branch TP, Schellinger D, Wiesel SW. Orientation of the lumbar facet joints: association with degenerative disc disease. J Bone Joint Surg Am. 1996;78:403–411. doi: 10.2106/00004623-199603000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Cyron BM, Hutton WC. Articular tropism and stability of the lumbar spine. Spine (Phila Pa 1976) 1980;5:168–172. doi: 10.1097/00007632-198003000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Berlemann U, Jeszenszky DJ, Bhler DW, Harms J. Facet joint remodeling in degenerative spondylolisthesis: an investigation of joint orientation and tropism. Eur Spine J. 1998;7:376–380. doi: 10.1007/s005860050093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noren R, Trafimow J, Andersson GB, Huckman MS. The role of facet joint tropism and facet angle in disc degeneration. Spine (Phila Pa 1976) 1991;16:530–532. doi: 10.1097/00007632-199105000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Pathria M, Sartoris DJ, Resnick D. Osteoarthritis of the facet joints: accuracy of oblique radiographic assessment. Radiology. 1987;164:227–230. doi: 10.1148/radiology.164.1.3588910. [DOI] [PubMed] [Google Scholar]
- 14.Dooris AP, Goel VK, Grosland NM, Gilbertson LG, Wilder DG. Load-sharing between anterior and posterior elements in a lumbar motion segment implanted with an artificial disc. Spine (Philadelphia, Pa 1976) 2001;26:E122–E129. doi: 10.1097/00007632-200103150-00004. [DOI] [PubMed] [Google Scholar]
- 15.Lemaire JP, Skalli W, Lavaste F, Templier A, Mendes F, Diop A, Sauty V, Laloux E. Intervertebral disc prosthesis. Results and prospects for the year 2000. Clin Orthop Relat Res. 1997;337:64–76. doi: 10.1097/00003086-199704000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Liu J, Ebraheim NA, Haman SP, Shafiq Q, Karkare N, Biyani A, Goel VK, Woldenberg L. Effect of the increase in the height of lumbar disc space on facet joint articulation area in sagittal plane. Spine (Philadelphia, Pa 1976) 2006;31:E198–E202. doi: 10.1097/01.brs.0000206387.67098.a0. [DOI] [PubMed] [Google Scholar]
- 17.Leone A, Aulisa L, Tamburrelli F, Lupparelli S, Tartaglione T. The role of computed tomography and magnetic resonance in assessing degenerative arthropathy of the lumbar articular facets. Radiol Med (Torino) 1994;88:547–552. [PubMed] [Google Scholar]
- 18.Vanharanta H, Floyd T, Ohnmeiss DD, Hochschuler SH, Guyer RD. The relationship of facet tropism to degenerative disc disease. Spine (Phila Pa 1976) 1993;18:1000–1005. doi: 10.1097/00007632-199306150-00008. [DOI] [PubMed] [Google Scholar]
- 19.Grogan J, Nowicki BH, Schmidt TA, Haughton VM. Lumbar facet joint tropism does not accelerate degeneration of the facet joints. AJNR Am J Neuroradiol. 1997;18:1325–1329. [PMC free article] [PubMed] [Google Scholar]
- 20.Kong MH, He W, Tsai Y, Chen N, Keorochana G, Do DH, Wang JC. Relationship of facet tropism with degeneration and stability of functional spinal unit. Yonsei Med J. 2009;50:624–629. doi: 10.3349/ymj.2009.50.5.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ko HY, Park BK. Facet tropism in lumbar motion segments and its significance in disc herniation. Arch Phys Med Rehabil. 1997;78:1211–1214. doi: 10.1016/S0003-9993(97)90334-8. [DOI] [PubMed] [Google Scholar]
- 22.Kim D, Ryu K, Kim M, Park C. Factors influencing segmental range of motion after lumbar total disc replacement using the ProDisc II prosthesis. J Neurosurg Spine. 2007;7:131–138. doi: 10.3171/SPI-07/08/131. [DOI] [PubMed] [Google Scholar]
- 23.Demetropoulos CK, Sengupta DK, Knaub MA, Wiater BP, Abjornson C, Truumees E, Herkowitz HN. Biomechanical evaluation of the kinematics of the cadaver lumbar spine following disc replacement with the ProDisc-L prosthesis. Spine (Philadelphia, Pa 1976) 2010;35:26–31. doi: 10.1097/BRS.0b013e3181c4eb9a. [DOI] [PubMed] [Google Scholar]
- 24.Rundell SA, Auerbach JD, Balderston RA, Kurtz SM. Total disc replacement positioning affects facet contact forces and vertebral body strains. Spine (Philadelphia, Pa 1976) 2008;33:2510–2517. doi: 10.1097/BRS.0b013e318186b258. [DOI] [PubMed] [Google Scholar]
- 25.Adams MA, Hutton WC. The mechanical function of the lumbar apophyseal joints. Spine (Phila Pa 1976) 1983;8:327–330. doi: 10.1097/00007632-198304000-00017. [DOI] [PubMed] [Google Scholar]