Abstract

Purpose
Minimally invasive or “minimal access surgery” (MAS) is being utilized with increasing frequency to reduce approach-related morbidity in the lumbar spine. This paper describes our minimal access technique for posterior bilateral transforaminal lumbar interbody fusion (TLIF) and spinal instrumentation in a patient with high-grade spondylolisthesis grade (Myerding Grade III) with 5-year follow-up.
Methods
A 24-year-old lady presented with mechanical back pain and left leg L5 radiculopathy. On examination, she was a thin lady with an obvious step deformity in the lower lumbar spine and otherwise, a normal neurological examination. Imaging showed a grade III isthmic L5–S1 spondylolisthesis with foraminal stenosis and focal kyphotic alignment of 20° [slip angle (SA) = 70°]. Conservative measures had failed, and a decision was made to proceed with a MAS-TLIF approach.
Results
The estimated blood loss was less than 100 ml, operating time 150 min, and post-operative hospital stay was 4 days. Post-operatively the patient had significant improvement of back and radicular pain. Improvement in ODI was substantial and sustained at 5 years. A solid fusion was achieved at 8 months. The slip percentage improved from 68 % (pre-op) to 28 % (post-op) and the focal alignment to 20° lordosis (SA = 110°).
Conclusions
A MAS approach for selected patients with a mobile high-grade spondylolisthesis is feasible, safe and clinically effective, with the added benefit of reduced soft-tissue disruption. Our result of this technique suggests that the ability to correct focal deformity, and achieve excellent radiographic and clinical outcome is similar to the open procedure.
Keywords: High-grade spondylolisthesis, Minimally invasive, Spinal instrumentation
Case report
A 24-year-old fashion design student presented with mechanical back pain and left leg L5 radiculopathy. The patient had been very active as a ballet dancer for 15 years and was also an avid snowboarder. She first noticed some minor back pain as far back as 8 years ago, but in the last 4 years her back pain and left leg pain had increased. On examination, she was a thin lady with an obvious step deformity in the lower lumbar spine and otherwise, a normal neurological examination.
Diagnostic imaging section
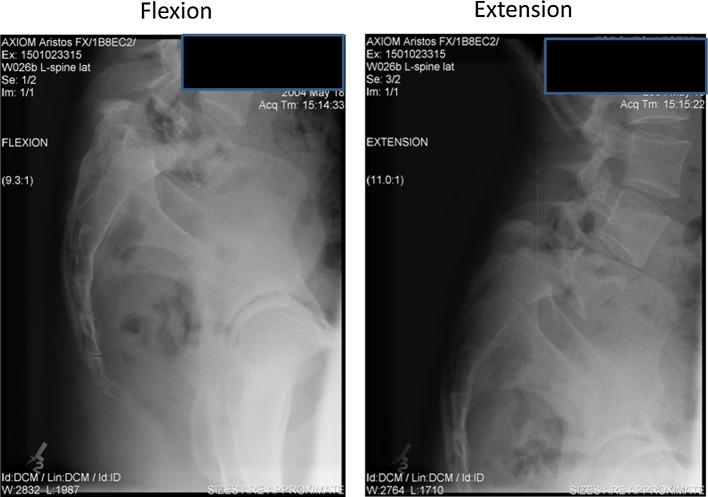
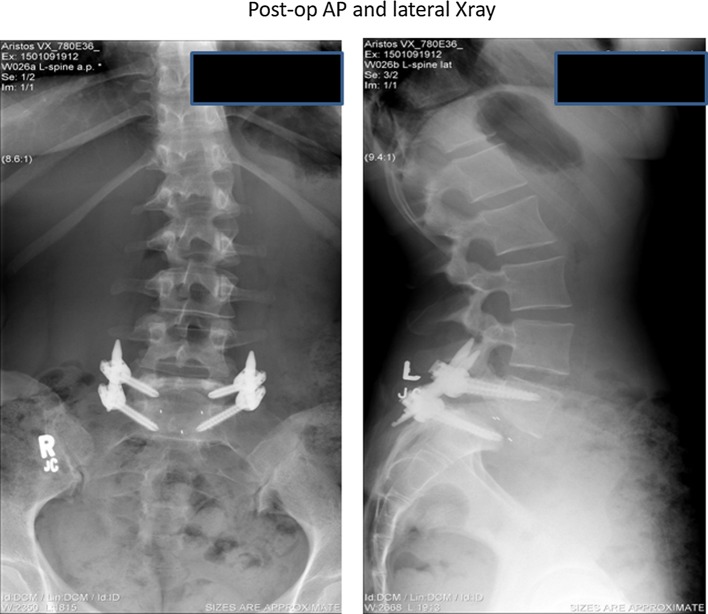
Imaging, including dynamic films (Fig. 1), showed a grade III isthmic L5–S1 spondylolisthesis with foraminal stenosis (left worse than right) and a 20° focal kyphotic alignment or lumbosacral slip angle (SA) = 70° (Fig. 2). The lumbosacral SA is the angle formed by a line drawn parallel to the superior aspect of the L5 vertebra and a line drawn perpendicular to the posterior aspect of the body of the first sacral vertebra (normal range 90–110°) [1]. Conservative measures had failed, and a decision was made to proceed with minimal access surgery (MAS), involving decompression, interbody fusion [transforaminal lumbar interbody fusion–(TLIF)] and instrumented stabilization.
Fig. 1.
Pre-operative flexion–extension views of our patient with a grade III isthmic L5–S1 spondylolisthesis
Fig. 2.
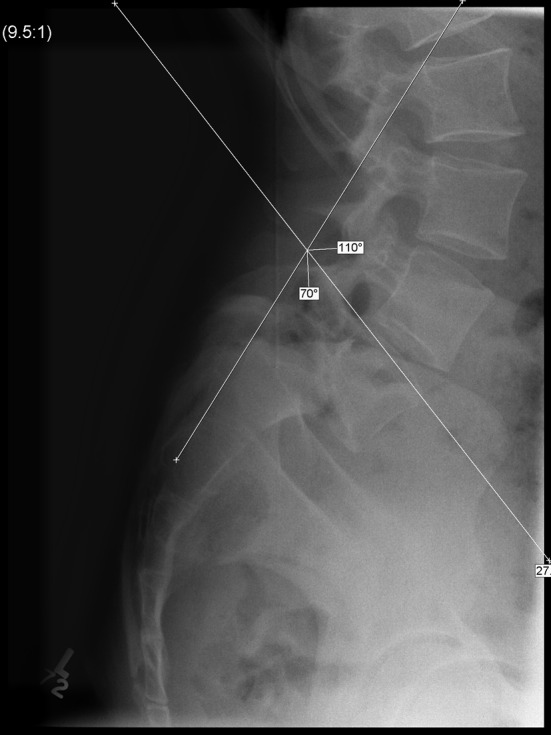
Pre-operative standing lateral radiograph showing a lumbosacral slip angle of 70°
Historical review, epidemiology, diagnosis, pathology, differential diagnosis
Isthmic spondylolisthesis is a common spinal entity that exists in up to 7–8 % of the population [2]. It can cause disabling mechanical low back pain and/or radicular leg pain [2]. Surgical treatment of spondylolisthesis in adults frequently consists of decompression of neural structures combined with instrumented fusion using pedicle screws and bone graft. High-grade (Myerding Grade III–IV) spondylolisthesis is often associated with dysplastic or congenitally anomalous spinal anatomy and complex three-dimensional deformity [3–6]. Consequently, surgical treatment, particularly when considering instrumentation, is very technically demanding and often necessitates the use of intra-operative imaging such as a fluoroscope.
More recently, in an effort to further reduce operative morbidity, minimally invasive posterior fusion techniques have been introduced. These techniques essentially utilize a muscle splitting approach with specialized retractors and instruments to perform standard open procedures in a less invasive manner [7–11].
The objective of this report is to describe our technique with the use of a minimally invasive or perhaps more appropriately termed “less invasive or minimal access surgery” for a grade III isthmic spondylolisthesis.
Rationale for treatment and evidence based literature
Many patients with high-grade spondylolisthesis suffer from mechanical low back pain with or without radicular leg pain. The radicular pain is caused by either nerve root compression and/or traction of nerve roots especially, the L5 nerve roots [12]. Treatment of high-grade spondylolisthesis is a controversial subject, but most surgeons consider surgical treatment for patients with severe mechanical back and/or radicular pain after adequate conservative treatment. Which surgical treatment is appropriate for this condition is also a matter of some disagreement and a detailed discussion about different surgical treatments is outside the scope of this paper.
In brief, due to significant focal kyphosis, high-grade slips are typically associated-high-shear stresses at with the lumbosacral junction. In addition the slipped vertebra is often difficult to access for instrumentation or bone grafting. These factors result in a significantly higher risk of non-union and instrumentation (if used) failure. A variety of surgical options have been utilized to reduce the non-union rate such as extension of the in situ fusion one or two levels above the slip, specialized lumbo-sacral instrumentation (transvertebral screw fixation, intrasacral rod, and iliac wing fixation), and/or reduction techniques [11–18]. It is sufficient to say that these different techniques have individual and combined merit in the treatment of this anatomically complex condition. Due to variable anatomical and clinical presentation, an individualized treatment plan based on the patients’ specific anatomical and clinical characteristics, the surgeons experience and the available supporting literature is appropriate.
The rationale for a minimally invasive surgical technique is to reduce the approach-related muscular morbidity and it is imperative that it is clinically as effective as the more conventional open procedure, and ultimately superior with respect to peri-operative pain, recovery, and patient satisfaction if it is to be widely accepted. Over the last decade, posterior minimal access spinal surgery has gained significant momentum [19–21].
Whilst many studies have reported radiographic outcome following surgery for high-grade spondylolisthesis, objective outcome scores are lacking. Lamberg and colleagues [22] performed long-term analysis on different techniques for uninstrumented fusion for high-grade slips in adolescents. They reported a mean ODI of 9.7 (postero-lateral fusion group), 8.9 (anterior fusion group) and 3.0 (circumferential group) at an average follow-up of 17.2 years. The mean ODI in our patient improved from 62 % to a mean of 22 % at 5 years follow-up. However, in the absence of pre-operative scores in the aforementioned study, and a different patient population (i.e. the majority of literature on high-grade spondylolisthesis involves a pediatric population) any comparison is to be cautiously interpreted. A reduction of 40 % in our ODI scores reflects a substantial clinical improvement in our case [23]. Our estimated blood loss (EBL) (less than 100 ml), operating time (150 min) and post-operative hospital stay (4 days) are comparable to Shufflebarger and Geck’s study [24] of a Gill distraction, PLIF and posterior instrumentation in adolescent high-grade isthmic dysplastic spondylolisthesis (EBL 650 ml, OR time 3.6 h and post-op hospital stay of 6 days). However, the chronic changes that have occurred within a much older adult population make direct surgical comparison difficult. For example, within the senior author’s institution, for low-grade spondylolisthesis there is a greater than 500 ml difference in EBL between open and MIS fusion [25]. This is consistent with the recent study by Goyal [26], where the authors reported an average EBL of 1,092 ml in a series of 13 patients undergoing open TLIF for mid to high-grade isthmic spondylolisthesis. Regarding length of stay (LOS), comparison from a socialised health system to that of different system (e.g. private) is not valid. The LOS for this high-grade patient is the same as for our low-grade spondylolisthesis MIS fusions which is in turn 3 days shorter compared to open [25].
Radiographic comparisons, however, are more comparable. The slip percentage in our patient improved from a pre-op 68 % to 28 % at 5 years follow-up. This radiographic improvement is similar to reports from open techniques. Goyal et al. [26], found an average anterolisthesis improvement from 51 % to 17 % at final follow-up (average 21.5 months) with instrumented reduction and TLIF.
There were no neurological or structural complications in our patient comprising of single level pathology without atypical features. Furthermore, clinical and radiographic success achieved with mono-segmental fusion compared to multi-level open procedures described in the Goyal series [26]. A possible explanation for this is that the paramedian approach gives better access to the L5 pedicle enabling a more medial anatomic screw trajectory and the screw sizes were maximized after reduction. In addition this approach provides significantly less muscle retraction and morbidity [27–29], that has been shown to have positive effects on post-operative trunk muscle performance and hence possibly improved local dynamic stability [29].
For high-grade cases, where pedicular anatomy is not suitable for safe pedicle instrumentation or dysplastic lumbo-sacral anatomy would preclude a reasonable expectation of safe partial reduction, more conventional open techniques are employed. Furthermore, if a rigid listhesis is noted pre-operatively or intra-operatively, more conventional open means of reduction (if required) and/or multilevel fixation should be utilized. If attempted through the technique described herein, the 3-cm paramedian incisions can be expanded to enable a more traditional Wilste approach and utilization of open release (bony or soft-tissue) and instrumentation techniques as required. It must be noted that the senior author has significant experience in both open and MAS surgery and would not recommend this technique for a novice surgeon with early experience in MAS surgery.
Procedure
The general posterior techniques for a MAS approach have been previously described in the literature [7, 8]. The following is a technical description as it applies to high-grade spondylolisthesis. The patient was positioned on a radiolucent spine table with a hyper extended posture. In order to reduce radiation exposure, our preference is to use C-arm fluoroscopy in combination with two-dimensional image-guided navigation for localization, pedicle screw placement and disc preparation [9]. Use of this technique has been previously described and is not the focus of this paper [7–10] and will be referred to as “imaging” for the remainder of the manuscript (i.e. technique can be preformed with or with out computer assistance).
Firstly, 3-cm paramedian incisions are made 4–5 cm from the midline (a more lateral starting point is utilized for larger patients) over the affected level. The underlying lumbosacral and paraspinal muscle fascia is split in line with the incision and blunt finger dissection identifies the intermuscular plane between multifidus and longissimus muscles. The appropriate facet is identified and confirmed with imaging. A MAS retractor is then placed directly over the facet (we use the Quadrant™ or MetRx fixed 22 mm tubular Retractors, Medtronic–Sofamor Danek, Memphis, TN, USA). As these surgeries are performed at a university teaching center, an operating microscope is used for illumination and to allow visualization for the entire team. Alternatively, loupes and a fiberoptic light source can be used.
The muscular attachment to the facet is released and the bony facet is completely exposed using a monopolar cautery. Using a series of bayoneted-long spinal instruments (MetRx™) as well as osteotomes bilateral facetectomies are performed through the MAS operative corridors as per an open TLIF or a posterior lumbar interbody fusion (PLIF). For grade III or IV high-grade listhesis, a bilateral facetectomy approach is used, otherwise a unilateral facetectomy approach is used for lower grades. For higher grade listhesis, the exiting and traversing nerve roots are both exposed (neurolysis is performed as required) and protected.
For high-grade spondylolisthesis cases the exiting nerve root is typically directly over the disc space. This necessitates, working a little more inferior and medial compared to a standard TLIF with some retraction of the traversing root (i.e. disc entry is somewhere between a TLIF and PLIF). Disc entry is also difficult due to the degree of spondylolisthesis, complete disc space collapse and formation of posterior traction osteophyte at the caudal vertebrae. Entry into the disc space was performed by a fluoroscopically guiding a 6 mm osteotome or thin/sharp distraction blade line up just above and parallel to the caudal pedicle (annulus-endplate junction) and endplate respectively. The osteotome/distraction blade is driven through the base of osteophyte into the disc space until the tip is at least 1-cm beyond the posterior aspect of the cephalad translated vertebrae. It is then rotated 90° to its taller dimension and left in situ until the contralateral disc space is entered (see distraction below). These techniques enable the annulus and the overlying nerve to be simultaneously lifted away. The annulus is left as a flap that protects the exiting root throughout the case. This initial distraction facilitates the contralateral disc space exposure and entry.
The procedure is then repeated on the other side through a similar 3 cm paramedian incision. Sequential distraction of the disc space is then carried out with intradiscal distraction blades until adequate tension of the annulus is felt or a maximum size implant that is safely passable within the confines of the neural exposure is reached [11]. During distraction an aggressive bilateral discectomy is performed, including release of the posterolateral annulus and osteotomy of the anterior cephalad endplate. The latter is performed with live fluoroscopic images. Symmetric disc space distraction reliably corrects focal sagittal or coronal deformity and typically results in partial correction of the listhesis by one grade. The goal in such a patient with high-grade spondylolisthesis is to correct the focal kyphosis and to reduce translation to a minimum of grade I to enable safe placement of the interbody devices (i.e. adequate anterior to posterior coverage of the implant by both endplates).
Spondylolisthesis reduction screws (Legacy, Medtronic–Sofamor Danek, Memphis, TN, USA) were then placed with imaging assistance in the cephalad vertebrae and standard multi-axial screws (7.5 mm diameter, bicortical screws at S1) in the caudal vertebrae. Compared to a midline approach, the paramedian approach facilitates easier access to the L5 pedicles screw entry point and provides the ideal trajectory (Fig. 2). The rod is placed and the caudal screw is locked with the cephalad portion of the rod 1–1.5 cm above the base of the cephalad screw. The reduction is performed with the use of spondylolisthesis screws with the distraction blades in situ. The blades act as parallel tracts to slide the translated vertebrae back on the stable vertebrae. Once adequate reduction is achieved, the screws are locked and the procedure is continued as below.
One distractor as well as the corresponding rod and the ipsilateral cartilaginous endplate were removed. Morselized, local autogenous bone graft is packed anteriorly. Adequate bone graft to fill the cages and disc space is usually obtained from the decompression; if more is required then it can be obtained from further removal of the lamina and base of the spinous process. In our case, the off-label use of recombinant bone morphogenic protein two (rhBMP2, Infuse, Medtronic–Sofamor Danek, Memphis, TN, USA) was also used. A small kit was utilized with the absorbable collagen sponges (ACS) placed inside the cages. No posterolateral bone grafting was performed.
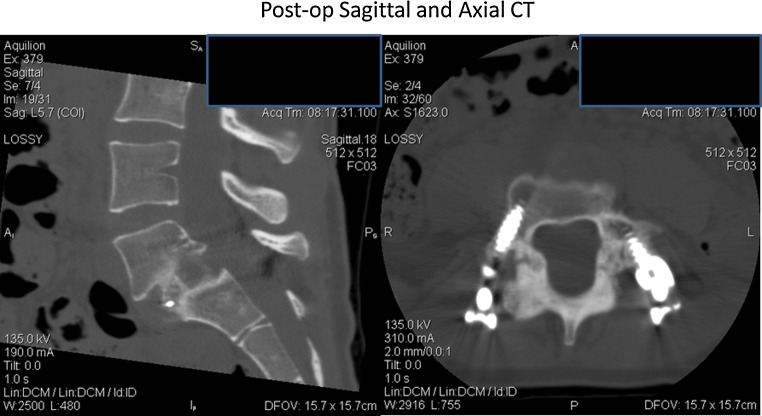
The appropriate size interbody device is then placed with its profile orientated such that the smallest amount of neural retraction is performed. A lordotic shaped device is preferred to improve focal sagittal disc space alignment. Due to possible loosening of the reduction screw during the reduction process, the cephalad screw is replaced by a larger diameter screw (5.5 mm diameter screw is placed initially and replaced with a 6.5- or 7.5-mm screw as tolerated). The process is then repeated on the contra-lateral side. The final screws and interbody graft are shown in Fig. 3 and mid-sagittal and axial CT scan (Fig. 4) shows that a complete laminectomy was not done (i.e. we performed bilateral facetectomy leaving the remaining upper lamina L5). Appropriate hemostasis is ensured and a layered (muscular and lumbosacral fascia) closure is performed. The EBL was less than 100 ml, operating time 150 min, and post-operative hospital stay was 4 days.
Fig. 3.
Post-operative AP and lateral radiographs with instrumentation in situ
Fig. 4.
Post-operative mid-sagittal and axial CT showing that the upper part of the L5 lamina was intact
Procedure imaging section
Fig. 5.
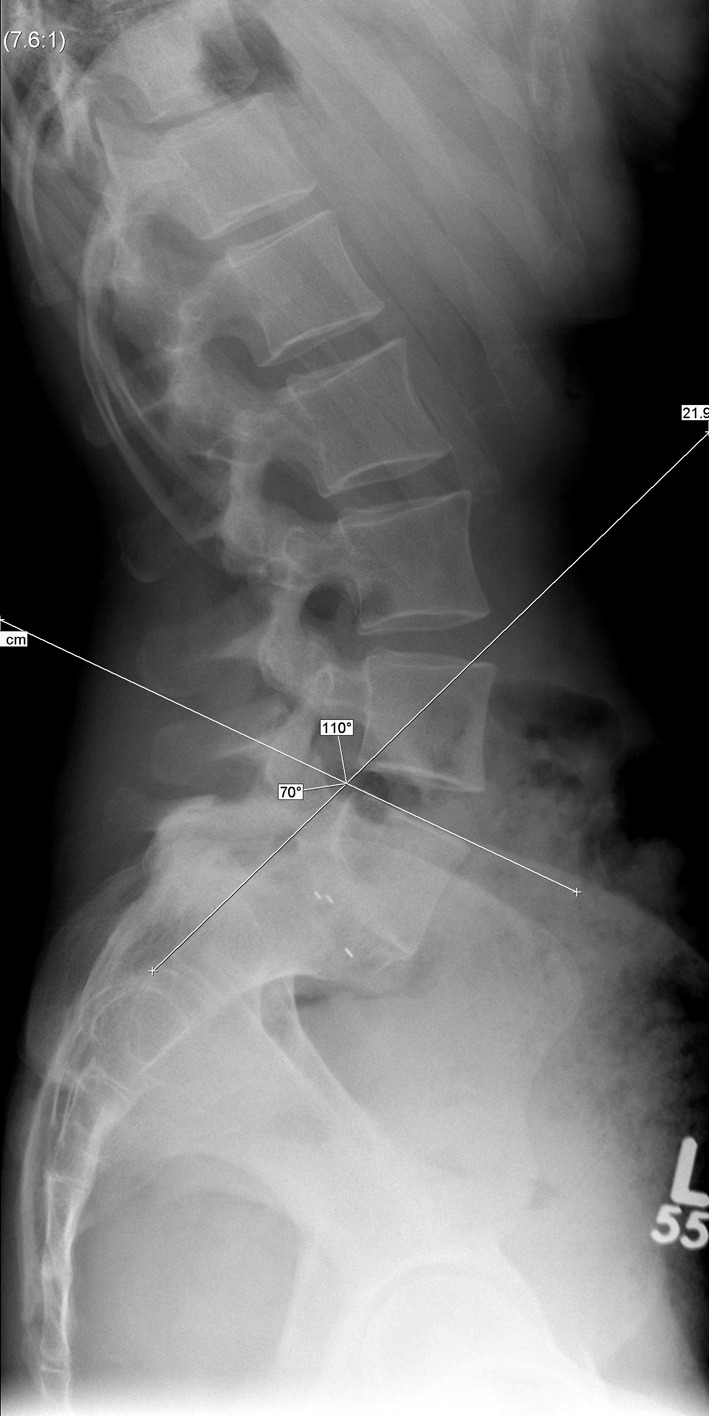
The slip percentage improved from 68 % (pre-op) to 28 % (post-op), and the slip angle from 70° (20° kyphotic) to 110° (20° lordotic). She had the pedicle screws/rods removed at the 1-year stage due to prominence and continues to do well at 5 years with maintained radiographic alignment and complete ossification of the disc space
Outcome
Post-operatively, our patient recovered well with significant improvement of back pain (pre-op VAS 8/10, 1-year post-op 3/10, 2-year post-op 5/10, 5-year post-op 3/10), radicular leg pain (pre-op VAS 8/10, 1-year post-op 2/10, 2-year post-op 2/10, 5-year post-op 0/10) and ODI (pre-op 62 %, 1-year post-op 38 %, 2-year post-op 32 %, 5-year post-op 22 %)—these improvements were substantial and sustained at 5 years. Both the X-rays and CT scan showed good placements of the screws in the appropriate positions. Intradiscal bridging bone was noted on routine CT at 8 months (senior author as a routine performs a CT scan at 6 months for assessment of fusion). The slip percentage improved from 68 % (pre-op) to 28 % (post-op), and the slip angle, by 40° [70° (20° kyphotic from neutral) pre-op to 110° (20° lordotic) post-op] (Fig. 5). She had the pedicle screws/rods removed at the 1-year stage due to prominence and continues to do well at 5 years with maintained radiographic alignment (Fig. 5).
In conclusion, a minimal access reduction and fusion technique is feasible, safe and clinically effective for selected adults with mobile high-grade spondylolisthesis. We have used this technique in at least another four patients. Furthermore, our results suggest that for highly selected cases, a less invasive technique can adequately correct focal deformity and achieve radiographic fusion rates similar to reported results from open techniques.
Conflict of interest
Yoga Raja Rampersaud is a consultant for Medtronic.
References
- 1.Boxall D, Bradford DS, Winter RB, Moe JH. Management of severe spondylolisthesis in children and adolescents. J Bone Joint Surg. 1979;61A(4):479–495. [PubMed] [Google Scholar]
- 2.Molinari RW. Adult isthmic spondylolisthesis. Curr Opin Orthop. 2002;13(3):178–183. doi: 10.1097/00001433-200206000-00004. [DOI] [Google Scholar]
- 3.Curylo LJ, Edwards C, DeWald RW. Radiographic markers in spondyloptosis: implications for spondylolisthesis progression. Spine. 2002;27:2021–2025. doi: 10.1097/00007632-200209150-00010. [DOI] [PubMed] [Google Scholar]
- 4.Hanson DS, Bridwell KH, Rhee JM, Lenke LG. Correlation of pelvic incidence with low- and high-grade isthmic spondylolisthesis. Spine. 2002;27:2026–2029. doi: 10.1097/00007632-200209150-00011. [DOI] [PubMed] [Google Scholar]
- 5.Molinari RW, Bridwell KH, Lenke LG, et al. Complications in the surgical treatment of pediatric high-grade, isthmic dysplastic spondylolisthesis. A comparison of three surgical approaches. Spine. 1999;24:1701–1711. doi: 10.1097/00007632-199908150-00012. [DOI] [PubMed] [Google Scholar]
- 6.Myerding HW. Spondylolisthesis: surgical treatment and results. Surg Gynecol Obstet. 1932;54:371–377. [Google Scholar]
- 7.Rampersaud YR, Gurgo RD (2008) Mini-open posterior lumbar interbody fusion for deformity. In: Mummaneni, Lenke, Haid (eds) Spinal deformity: a guide to surgical planning and management, Chap 35. Quality Medical Publishing, Inc., St. Louis, pp 721–748
- 8.Schwender JD, Holly LT, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech. 2005;18(Suppl):S1–S6. doi: 10.1097/01.bsd.0000132291.50455.d0. [DOI] [PubMed] [Google Scholar]
- 9.Ravi B, Zahrai A, Rampersaud R. Clinical accuracy of computer-assisted two-dimensional fluoroscopy for the percutaneous placement of lumbosacral pedicle screws. Spine (Phila Pa 1976) 2011;36(1):84–91. doi: 10.1097/BRS.0b013e3181cbfd09. [DOI] [PubMed] [Google Scholar]
- 10.Rampersaud YR, Pik JH, Salonen D, Farooq S. Clinical accuracy of fluoroscopic computer-assisted pedicle screw fixation: a CT analysis. Spine (Phila Pa 1976) 2005;30(7):E183–E190. doi: 10.1097/01.brs.0000157490.65706.38. [DOI] [PubMed] [Google Scholar]
- 11.Sears W. Posterior lumbar interbody fusion for lytic spondylolisthesis: restoration of sagittal balance using insert-and-rotate interbody spacers. Spine J. 2005;5(2):161–169. doi: 10.1016/j.spinee.2004.05.256. [DOI] [PubMed] [Google Scholar]
- 12.Petraco DM, Spivak JM, Cappadona JG, et al. An anatomic evaluation of L5 nerve stretch in spondylolisthesis reduction. Spine. 1996;21:1133–1138. doi: 10.1097/00007632-199605150-00002. [DOI] [PubMed] [Google Scholar]
- 13.Cunningham BW, Lewis SJ, Long J, et al. Biomechanical evaluation of lumbosacral reconstruction techniques for spondylolisthesis: an in vitro porcine model. Spine. 2002;27:2321–2327. doi: 10.1097/00007632-200211010-00004. [DOI] [PubMed] [Google Scholar]
- 14.Jackson RP, McManus AC. The iliac buttress. A computed tomographic study of sacral anatomy. Spine. 1993;18:1318–1328. doi: 10.1097/00007632-199308000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Kuklo TR, Bridwell KH, Lewis SJ, et al. Minimum 2-year analysis of sacropelvic fixation and L5–S1 fusion using S1 and iliac screws. Spine. 2001;26:1976–1983. doi: 10.1097/00007632-200109150-00007. [DOI] [PubMed] [Google Scholar]
- 16.Lebwohl NH, Cunningham BW, Dmitriev A, et al. Biomechanical comparison of lumbosacral fixation techniques in a calf spine model. Spine. 2002;27:2312–2320. doi: 10.1097/00007632-200211010-00003. [DOI] [PubMed] [Google Scholar]
- 17.Mazda K, Khairouni A, Pennecot GF, Bloch J. The ideal position of sacral transpedicular endplate screws in Jackson’s intrasacral fixation. An anatomic study of 50 sacral specimens. Spine. 1998;23:2123–2126. doi: 10.1097/00007632-199810010-00017. [DOI] [PubMed] [Google Scholar]
- 18.Minamide A, Akamaru T, Yoon ST, et al. Transdiscal L5–S1 screws for the fixation of isthmic spondylolisthesis: a biomechanical evaluation. J Spinal Disord Tech. 2003;16:144–149. doi: 10.1097/00024720-200304000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Oppenheimer JH, DeCastro I, McDonnell DE. Minimally invasive spine technology and minimally invasive spine surgery: a historical review. Neurosurg Focus. 2009;27(3):E9. doi: 10.3171/2009.7.FOCUS09121. [DOI] [PubMed] [Google Scholar]
- 20.Peng CW, Yue WM, Poh SY, Yeo W, Tan SB. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976) 2009;34(13):1385–1389. doi: 10.1097/BRS.0b013e3181a4e3be. [DOI] [PubMed] [Google Scholar]
- 21.Kasis AG, Marshman LA, Krishna M, Bhatia CK. Significantly improved outcomes with a less invasive posterior lumbar interbody fusion incorporating total facetectomy. Spine (Phila Pa 1976) 2009;34(6):572–577. doi: 10.1097/BRS.0b013e3181973e35. [DOI] [PubMed] [Google Scholar]
- 22.Lamberg T, Remes V, Helenius I, Schenzka D, Seitsalo S, Poussa M. Uninstrumented in situ fusion for high-grade childhood and adolescent isthmus spondylolisthesis: long-term outcome. J Bone Joint Surg Am. 2007;89(3):512–518. doi: 10.2106/JBJS.E.00545. [DOI] [PubMed] [Google Scholar]
- 23.Glassman SD, Copay AG, Berven SH, Polly DW, Subach BR, Carreon LY. Defining substantial clinical benefit following lumbar spine arthrodesis. J Bone Joint Surg Am. 2008;90(9):1839–1847. doi: 10.2106/JBJS.G.01095. [DOI] [PubMed] [Google Scholar]
- 24.Shufflebarger HL, Geck MJ. High grade isthmic dysplastic spondylolisthesis. Spine. 2005;30(6 Suppl):S42–S48. doi: 10.1097/01.brs.0000155583.55856.f9. [DOI] [PubMed] [Google Scholar]
- 25.Rampersaud YR, Gray R, Lewis SJ, Massicotte EM, Fehlings MG. Cost-utility analysis of posterior minimally invasive fusion compared with conventional open fusion for lumbar spondylolisthesis. SAS J. 2011;5:29–35. doi: 10.1016/j.esas.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goyal N, Wimberley DW, Hyatt A, Zeiller S, Vaccaro AR, Hilibrand AS, Albert TJ. Radiographic and clinical outcomes after instrumented reduction and transforaminal lumbar interbody fusion of mid and high-grade isthmic spondylolisthesis. J Spinal Disord Tech. 2009;22(5):321–327. doi: 10.1097/BSD.0b013e318182cdab. [DOI] [PubMed] [Google Scholar]
- 27.Tsutsumimoto T, Shimogata M, Ohta H, Misawa H. Mini-open versus conventional open posterior lumbar interbody fusion for the treatment of lumbar degenerative spondylolisthesis: comparison of paraspinal muscle damage and slip reduction. Spine (Phila Pa 1976) 2009;34(18):1923–1928. doi: 10.1097/BRS.0b013e3181a9d28e. [DOI] [PubMed] [Google Scholar]
- 28.Kim KT, Lee SH, Suk KS, Bae SC. The quantitative analysis of tissue injury markers after mini-open lumbar fusion. Spine (Phila Pa 1976) 2006;31(6):712–716. doi: 10.1097/01.brs.0000202533.05906.ea. [DOI] [PubMed] [Google Scholar]
- 29.Kim DY, Lee SH, Chung SK, Lee HY. Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine (Phila Pa 1976) 2005;30(1):123–129. doi: 10.1097/01.brs.0000157172.00635.3a. [DOI] [PubMed] [Google Scholar]