Abstract
Objectives
Antiestrogen therapy can cause vasomotor symptoms similar to those occurring during menopause, including hot flashes. Recent studies suggest that acupuncture is effective in reducing vasomotor symptoms in patients with breast cancer receiving tamoxifen. The purpose of this study was to assess the feasibility and safety of acupuncture for treatment of hot flashes in Korean patients with breast cancer receiving antiestrogen therapy.
Design
This was a prospective single-arm observational study using before and after measurements.
Settings/location
The study was located at the East–West Medical Center at Daegu Catholic University Medical Center, Daegu, Korea.
Subjects
The subjects were 10 patients with breast cancer who were undergoing antiestrogen therapy with tamoxifen or anastrozole and who were suffering from hot flashes.
Interventions
Acupuncture was administered 3 times a week for 4 consecutive weeks, for 20±5 minutes at each session.
Outcome measures
The outcome measure was severity of hot flashes assessed by visual analogue scale (VAS) and total hot flash score.
Results
During treatment, severity of hot flashes was reduced by 70%–95% in all patients. Acupuncture significantly alleviated severity of hot flashes assessed by a visual analogue scale (F=30.261; p<0.001) as well as the total hot flash score (F=21.698; p=0.006). Four (4) weeks after the final treatment, symptoms were not aggravated.
Conclusions
Acupuncture appeared to provide effective relief from hot flashes among Korean women receiving antiestrogen therapy after surgery for breast cancer, and the effects lasted for at least 1 month after termination of treatment. A randomized controlled prospective study with a larger sample size is required to clarify the role of acupuncture in the management of hot flashes in Korean patients with breast cancer.
Introduction
Breast cancer is the second most common cancer among Korean women, and its incidence is increasing at an annual rate of 6.5%. Currently, breast cancer is the leading cause of cancer-related deaths worldwide.1,2 Besides surgery, adjuvant therapy with chemotherapy and antiestrogen therapy is conventional therapy of breast cancer. However, antiestrogen therapy is commonly associated with the side-effect of hot flashes caused by estrogen deficiency. A hot flash is characterized by a sudden rushing sensation of warmth or even intense heat spreading over various parts of the body and may severely impair quality of life.3,4 An increasing number of breast cancer survivors are undergoing antiestrogen therapy, thus relieving the symptoms of hot flashes, which made a significant impact on their quality of life.
For healthy postmenopausal women, hormone replacement therapy (HRT) has traditionally been used to alleviate symptoms, but it is contraindicated for patients with breast cancer due to the risk of recurrence of the disease or new primary breast cancer.5 The decline in prescription of HRT for treatment of hot flashes has led to increased interest in nonhormonal alternatives. Several treatment modalities including clonidine, selective serotonin reuptake inhibitors, selective norepinephrine reuptake inhibitors, and gabapentin, can be prescribed to meet this aim.6 However, many patients are noncompliant with these medications because of adverse effects. A substantial proportion of patients with breast cancer have been interested in and turn to complementary and alternative medicines for managing hot flashes and other menopausal symptoms.7,8 Acupuncture is one of the most popular forms of complementary medicines.8–10
Recent studies have suggested that acupuncture is effective in reducing vasomotor symptoms among menopausal women11–13 as well as patients with breast cancer receiving tamoxifen (Table 1).14–23 A randomized controlled trial17 reported favorable effects of acupuncture compared with sham acupuncture for hot flashes in patients with breast cancer, although another randomized controlled trial18 failed to show any such effects. Walker et al.19 compared acupuncture with venlafaxine and demonstrated that acupuncture was as effective as venlafaxine. Frisk et al.20 compared the effects of electroacupuncture with those of HRT and reported that electroacupuncture relieved vasomotor symptoms in most women with breast cancer, but that HRT was more effective.
Table 1.
Overview of Clinical Trials for the Treatment of Hot Flashes in Breast Cancer Patients
| Author(s) | Study design | Participants (n) | Intervention type (protocol) | Type of control group | Main outcomes/results |
|---|---|---|---|---|---|
| Tukmachi14 | Uncontrolled, single-arm | 22 | AT (traditional acupuncture) | None | Reduced HF frequency (p<0.001) |
| Porzio et al.15 | Uncontrolled, single-arm | 15 | AT (TCM) | None | Improved vasomotor symptoms |
| De Valois et al.16 | Uncontrolled, single-arm | 50 | AT (traditional acupuncture) | None | Reduced HF frequency (p<0.0001) |
| Hervik et al.17 | RCT | 59 | AT (TCM) | Sham AT | Intergroup: significant difference (p<0.001) Intergroup: Reduced HF frequency in AT group, both during and after treatment (p<0.001); reduced HF frequency in sham AT during treatment (p=0.01), not significant after treatment (p=0.22) |
| Deng et al.18 | RCT | 72 | AT (traditional acupuncture) | Sham AT | Intergroup: not significant Within-group: Reduced HF frequency in both groups (p<0.01) |
| Walker et al.19 | RCT | 50 | AT (not reported) | Venlafaxine | Intergroup: not significant Within-group: Reduced HF frequency in both groups (p<0.036) |
| Frisk et al.20 | RCT | 45 | EA (traditional acupuncture) | HRT | Intergroup: HRT is more effective than EA Within-group: Reduced HF frequency in both groups (p<0.05) |
| Davies et al.21 | RCT | 20 | AT (traditional acupuncture) | Sham AT | Intergroup: not significant Within-group: not reported |
| Nedstrand et al.22 | RCT | 38 | EA (classic acupuncture) | Applied relaxation | Intergroup: not reported Within-group: Reduced HF frequency in both groups (p<0.001) |
| Liljegren et al.23 | RCT | 74 | AT (traditional acupuncture) | Sham AT | Intergroup: not significant Within-group: Reduced HF frequency in both groups (p<0.001) |
AT, acupuncture; TCM, traditional Chinese medicine; RCT, randomized controlled trial; HRT, hormone replacement therapy; EA, electroacupuncture; HF, hot flash.
Acupuncture is increasingly being introduced into standard care, and is also being included in oncology clinics.24 Considering the increasing prevalence of breast cancer among Korean women,1 information on the role of acupuncture in Korean women, especially patients with breast cancer, is necessary for treating patients with hot flashes. However, there are no available data on the effectiveness of acupuncture for treatment of hot flashes in patients with breast cancer in Korea. This study was designed to assess the feasibility and safety of acupuncture for treatment of hot flashes in Korean patients with breast cancer undergoing antiestrogen therapy.
Materials and Methods
Study design
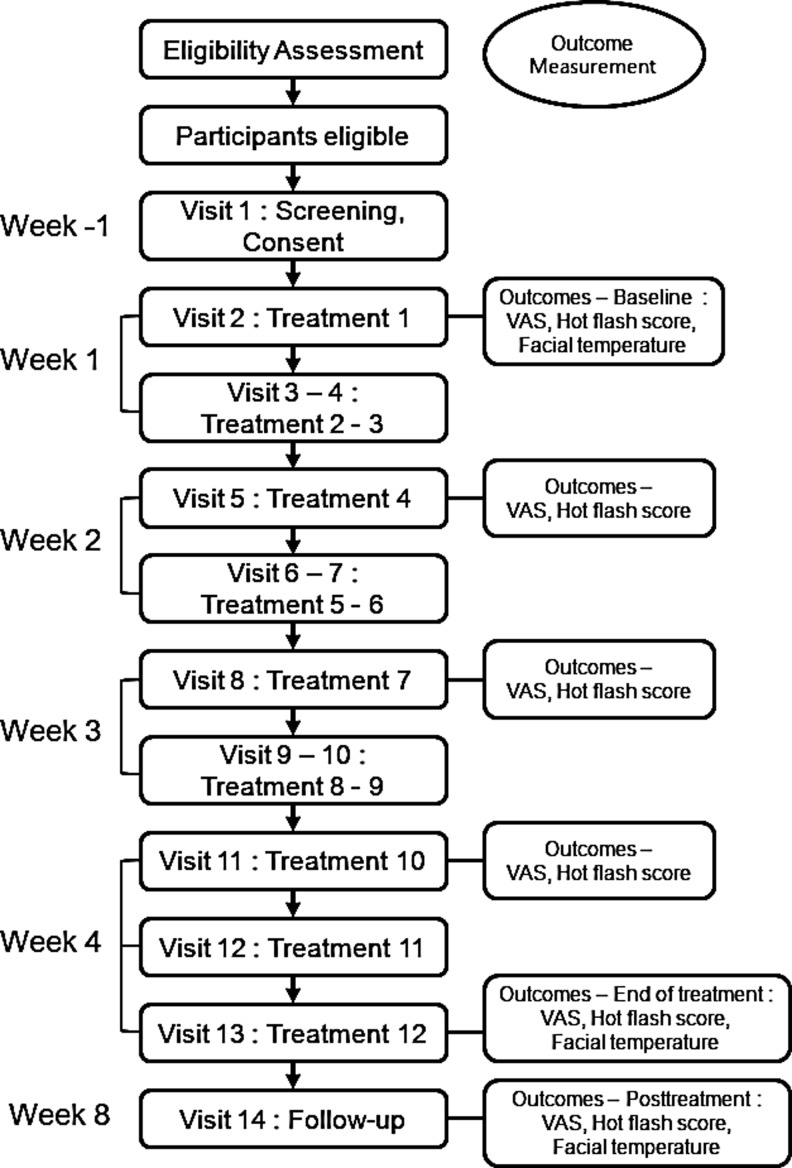
The institutional review board at Daegu Catholic University Hospital approved this study. There were no conflicts of interest for the investigators or the research staff. This was a prospective, single-arm, observational study. Participants received 12 sessions of acupuncture, delivered 3 times a week for 4 weeks. The severity of hot flashes was assessed via a visual analogue scale (VAS) and total hot flash score. Patients were evaluated 1 week before treatment commenced (baseline), once a week during treatment, and 4 weeks after the final acupuncture session. Figure 1 shows the study design.
FIG. 1.
Flow diagram of the study.
Study participants
Informed consent was obtained before participant enrollment according to a clinical trial protocol. Recruitment was performed from September 2011 through December 2012, and 10 Korean women with breast cancer were enrolled. Inclusion criteria were as follows: (1) pre- or postmenopausal status and presence of breast cancer treated with antiestrogen therapy using tamoxifen or anastrozole; (2) moderate or severe vasomotor symptoms according to the definition of the Food and Drug Administration25; (3) an average of 3 or more hot flashes per week during the 1-week period before the trial; (4) Karnofsky performance score of>60, which means ability to participate in the trial for oneself or with occasional assistance; (5) voluntary participation; (6) follow-up for the duration of the study; (7) cessation of HRT or other pharmacologic or alternative treatments for hot flashes at least 4 weeks before the trial, if such treatment were used. Exclusion criteria were as follows: (1) pharmacologic or other alternative treatment for hot flashes during the trial; (2) serious medical or psychiatric conditions making participation in the trial unsuitable; and (3) hot flashes caused by menopause without antiestrogen therapy.
Interventions
The study protocol involved 4 weeks of treatment with 3 acupuncture sessions per week. For all sessions, vital signs including blood pressure, pulse rate, and body temperature were measured before treatment. All sessions were 40 minutes long, and the acupuncture portion was 20±5 minutes in duration. Acupuncture was performed by a traditional Korean medicine (TKM) physician who was registered with the government and had at least 3 years of clinical experience in acupuncture treatment. Acupuncture points were selected according to the recommendations of TKM clinical experts26,27 and standard acupuncture textbooks.28,29 Acupuncture was applied at five acupuncture points: GV 20; M-HN-3; and bilaterally at three points including HT 8, KI 10, and LV 2.29 Table 2 shows the acupuncture point prescriptions and their anatomical position. The acupuncture needles used were sterile, disposable stainless steel needles (30×0.25 mm; Dongbang Acupuncture Inc., Chungcheongnam-do, Korea), and a total of eight needles were used. The skin was swabbed with an alcohol prep pad before acupuncture was administered. Depending on the points selected, needles were inserted 10–20 mm deep into the skin and were gently manipulated manually to obtain De Qi (needle sensation referring to pain, numbness, and distension felt around the point after the needle is inserted to a certain depth as well as the operator's sensation of tension around the needle).30 After 10 minutes, the needle positions were controlled by gentle rotation without evoking needle sensation. No electrical stimulation or other interventions were used.
Table 2.
Acupuncture Points Prescriptions and Their Therapeutic Effects with Acupuncture
|
Prescription |
|
|
|---|---|---|
| Point | Meridian | Location |
| GV 20 | Governing vessel | Midway on a line connecting the apex of both ears in a depression slightly anterior to a larger depression |
| M-HN-3 | Extra points | Midway between the medial ends of the eyebrows |
| HT 8 | Heart meridian | Between the 4th and 5th metacarpal bones |
| KI 10 | Kidney meridian | On the medial side of the knee joint between the tendons of semitendinosis and semimembranosus |
| LV 2 | Liver meridian | On the dorsum of the foot between the 1st and 2nd toes, proximal to the margin of the web at the junction of the red and white skin |
Study outcomes
The outcome measure was severity of hot flashes, which was assessed via a VAS and total hot flash score. Hot flashes were evaluated at baseline, once a week during treatment, on the final treatment day, and 4 weeks after the final acupuncture session. A self-report diary was used for data collection; this is a valid and reliable method for collecting subjective data such as patient-reported symptoms and perceptions.31 Participants were asked to document the average severity of hot flashes during the previous week using a VAS. The VAS assessment was then converted into scores ranging from 0 to 100 (0, no hot flashes; 100, severe hot flashes). Participants were also asked to record the severity of hot flashes on a scale ranging from 0 to 4 (0, none; 1, mild; 2, moderate; 3, severe; 4, very severe) as well the frequency of hot flashes per day. The total hot flash score was calculated by multiplying the frequency by the severity of hot flashes recorded in the daily diary.
Statistical analysis
Statistical analyses were performed using the SPSS statistical package, version 14.0 (SPSS Inc., Chicago, IL). A p-value of <0.05 was considered statistically significant. Using quantitative data recorded over 14 visiting days in the case report form, the mean VAS value and number of hot flashes per day were calculated for each participant, and these values were summed for all participants. For individual participants, changes in mean VAS and total hot flash scores from baseline to 4 weeks after the final acupuncture session were tested using paired t-tests. To investigate changes in the severity of hot flashes, a repeated-measures analysis of variance (ANOVA) using the VAS and total hot flash scores was performed.
Results
Participant flow
Thirty (30) women were screened for eligibility, and of these, 10 were included in the trial. All participants completed the full course of 12 acupuncture treatments. Compliance with follow-up was good, with all participants providing data for the primary endpoint. The participant flow through the trial is shown in Figure 1.
Baseline characteristics
The baseline characteristics of the participants are shown in Table 3. The mean age at baseline was 46.6 years (standard deviation [SD]=4.93; range, 38–53). Nine (9) of the 10 participants were receiving tamoxifen, and 1 participant was receiving anastrozole. The mean time since initiation of antiestrogen therapy was 19.1 months (SD=17.25; range, 2–53). No participant reported the use of dietary supplements relieving hot flashes at baseline or during the entire observation period.
Table 3.
Demographic and Clinical Characteristics at Baseline
| Variable | N (%) or mean±SD |
|---|---|
| Age (years) | 46.60±4.93 |
| Height (cm) | 159.80±4.78 |
| Weight (kg) | 66.50±11.23 |
| Menopausal status | |
| Premenopause | 8 (80) |
| Postmenopause | 2 (20) |
| Cancer treatment history | |
| Breast surgery | 10 (100) |
| Radiotherapy | 6 (60) |
| Chemotherapy | 6 (60) |
| Time taking tamoxifen or anastrozole | |
| <12 months | 4 (40) |
| 1–2 years | 4 (40) |
| 3–4 years | 1 (10) |
| >4 years | 1 (10) |
| Concurrent use of goserelin | |
| Yes | 4 (40) |
| No | 6 (60) |
| Previous use of HRT | |
| Yes | 0 (0) |
| No | 10 (100) |
SD, standard deviation; HRT, hormone replacement therapy.
Effects of acupuncture on severity of hot flashes assessed using a VAS
Changes in mean VAS score from baseline to 4 weeks after the final acupuncture session are presented in Table 4 and Figure 2. Repeated-measures ANOVA showed a significant reduction in the average VAS score for hot flash severity at the end of treatment (F=30.261, p<0.001).
Table 4.
Mean Values of VAS, Frequency, Severity and Scores of Hot Flashes from Baseline to Each Measurement Pointa
| Variables | Visit 2 | Visit 5 | Visit 8 | Visit 11 | Visit 13 | Visit 14 | F-valueb | p-Valueb |
|---|---|---|---|---|---|---|---|---|
| VAS | 71.50 (11.32) | 51.00 (16.80) | 39.00 (11.74) | 34.00 (18.38) | 23.00 (15.13) | 19.50 (13.23) | 30.261 | <0.001 |
| Frequency | 9.30 (9.72) | 3.50 (4.60) | 5.00 (6.13) | 5.10 (9.28) | 1.60 (2.41) | 1.50 (1.72) | 3.719 | 0.007 |
| Severity | 2.80 (0.79) | 1.70 (0.48) | 1.80 (0.63) | 1.60 (0.70) | 1.00 (0.47) | 1.10 (0.74) | 21.698 | <0.001 |
| Score | 31.10 (36.62) | 7.20 (9.09) | 11.60 (18.22) | 12.90 (27.81) | 1.90 (2.47) | 2.20 (2.53) | 3.825 | 0.006 |
Data are presented as mean (standard deviation).
Repeated-measures analysis of variance at visit 2, 5, 8, 11, 13, 14.
FIG. 2.
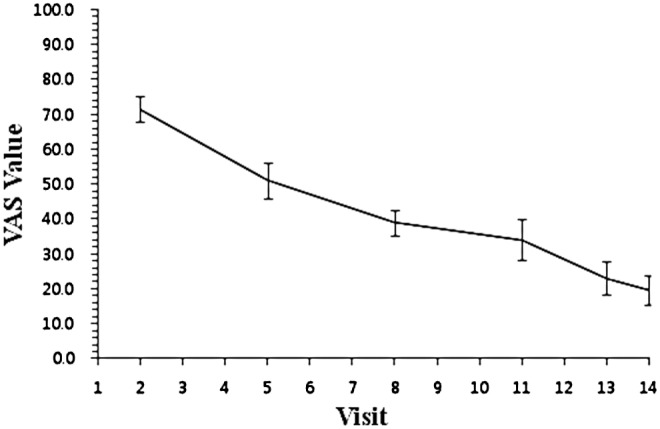
Changes in mean visual analogue scale (VAS) scores for hot flashes over time.
Effects of acupuncture on 24-hour hot flash frequency, severity, and total score
At baseline, the mean±SD 24-hour hot flash frequency was 9.30±9.72, and the mean 24-hour hot flash severity was 2.80±0.79 (Table 4). Repeated-measures ANOVA revealed a significant reduction in the average frequency, severity, and total hot flash score at the end of treatment (F=3.719, p=0.007; F=21.698, p<0.001; F=3.825, p=0.006, respectively) (Fig. 3).
FIG. 3.
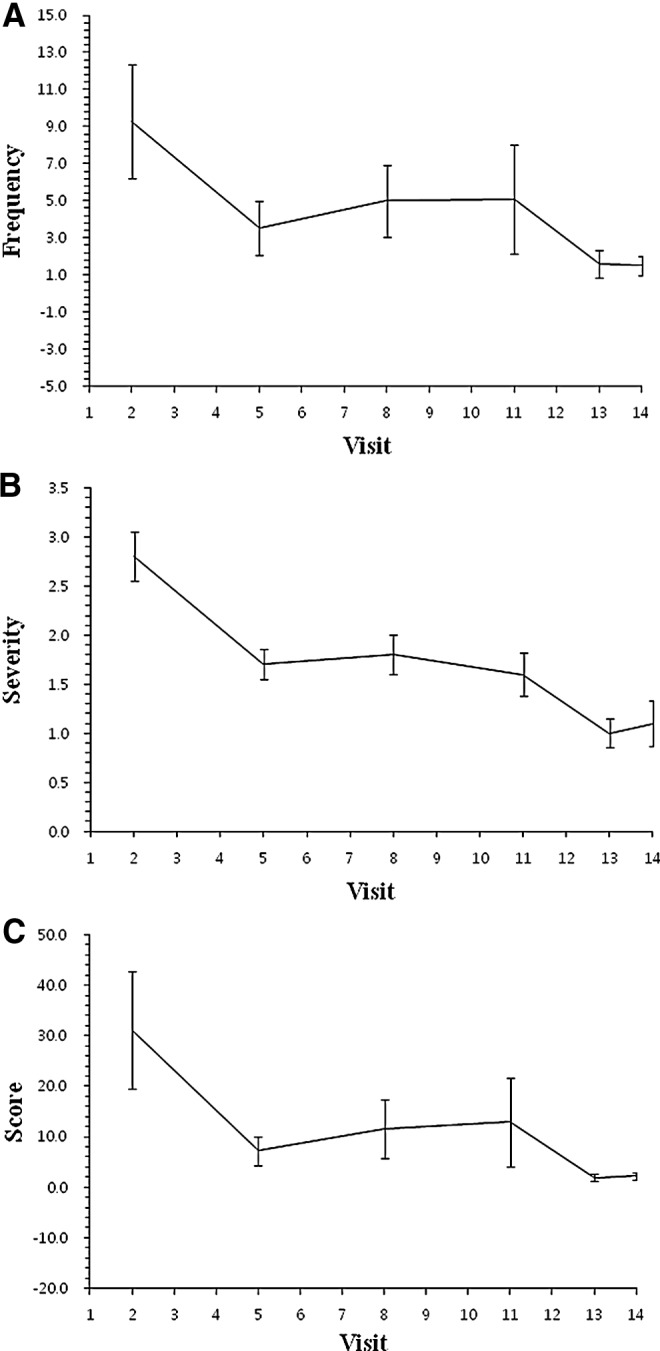
Changes in mean hot flash values per 24 hours over time. (A) Frequency, (B) severity, and (C) total hot flash score.
Safety
Acupuncture was well tolerated with few adverse events. During treatment, 1 participant experienced a skin rash that was deemed unrelated to acupuncture. No serious adverse events were reported.
Discussion
This study demonstrated that among Korean women with breast cancer, who are undergoing tamoxifen or anastrozole therapy, acupuncture reduced the mean VAS score as well as the total hot flash score for severity and frequency of hot flashes. The reduction in symptoms was maintained at week 8. These results suggest that acupuncture is a useful alternative treatment for alleviating hot flashes in patients who have breast cancer and who are receiving antiestrogen therapy, and are consistent with the results of previous studies.14–23
Recent studies have reported that acupuncture is effective in reducing vasomotor symptoms in patients who have breast cancer and who are receiving tamoxifen,16–22 but there is no consensus on the optimum treatment frequency or the duration of acupuncture in these patients. The duration of acupuncture treatment in this study was 4 weeks, which is a relatively short period compared to that in previous studies (range, 4–12 weeks).16–22 The earlier beneficial effects in the current study may be due to the cumulative effects that arise from multiple acupuncture sessions within a short period32 or from placebo effects generated by frequent exposure to treatment administration.33 These findings suggest that the effects of acupuncture are not influenced by longer treatment duration. Further study is required to determine the optimum frequency and duration of acupuncture for the treatment of hot flashes in patients with breast cancer.
Various acupoints were used in previous studies, including both standardized and individualized acupuncture therapy.16–22 In this study, five acupuncture points were selected with the functions of nourishing the Kidneys, cooling Heat, and calming the mind because patients with breast cancer generally tend to display disease patterns such as Liver Qi Stagnation and Blood Heat due to Yin insufficiency (Table 1).27,28 Acupuncture consists of inserting needles into acupuncture points, either by manipulation or by applying electric pulses or other appliances. The acupuncture protocol was selected based on the five-phase acupuncture method using five inductive points in TKM, which is different from the Traditional Chinese Medicine (TCM). In TKM, the acupuncture works by applying acupuncture to the 12 meridians and 5 inductive points.27,34,35 Each inductive point is assigned to Wood, Fire, Earth, Metal, Water of the five phases with the characteristics of each elements, whereas eight principles in TCM includes Interior and Exterior, Hot and Cold, Full and Empty, Yin and Yang.36 These inductive points represent the flow of Qi inside the 12 meridians using the flow of Water as metaphor.30 Therefore, acupuncture applied to an appropriate point of specific element can alleviate the symptoms, even though the acupuncture point is not near the body part causing symptoms.
Hot flashes are considered to be a classical sign of menopausal symptoms and can be measured via self-report. Although self-reports of hot flashes are generally considered to be acceptable for assessment, women with hot flashes tend to under-report hot flashes, resulting in high specificity but low sensitivity of subjective measurement.37 There are several studies to compare subjective and objective method for assessing hot flashes.37–39 Carpenter et al.37 and Otte et al.38 assessed hot flash frequency using self-report and sternal skin conductance monitoring, and the findings indicated dissimilarities between subjective and objective measures. Kim et al.39 assessed hot flashes by using Mexameter, Skin Thermometer, Corneometer, and Laser Doppler Perfusion Imager objectively, and results indicated weak correlation between subjective and objective measurements of hot flashes. Although previous studies show no objective measures of changes in hot flashes,37–39 the authors tried to include objective measure to explain the phenomena of hot flashes. On the basis of the findings that the subjective sensation of Heat is the predominant feature of a hot flash, infrared thermography was used. Thermography findings from a small group of patients have provided objective evidence that menopausal flushing is associated with an increase in skin temperature.40 The current study measured facial temperature during hot flash episode and analyzed the temperature differences between high and low temperature areas to compare the change in skin temperature before and after acupuncture treatment across individuals. However, the relationship between differences in facial temperature and hot flashes was dissimilar at each measurement point from baseline to the end of the study, which is consistent with the results of previous studies.37–39
Acupuncture is a relatively safe treatment modality.30,41 In previous studies,18–20 no reported adverse events were serious enough to warrant concern. Several studies have shown additional benefits of acupuncture, including improvements in emotional and physical well-being,16,19,22 and increased sex drive in some women.19 Reported adverse events were slight bleeding or bruising at the needle site.18 In the present study, there were no serious adverse effects, which is comparable with the findings of previous studies.
The present study had several limitations. First, the study consisted of a small sample and was conducted at a single acupuncture clinic. The participants were treated by a single acupuncturist (Kwon) who was also the investigator. Therefore, the relatively small, selective sample limits the ability to apply the results to the general population. Second, the design of the study is not optimal. The study was a single-arm, observational study without a control group. Without a placebo or proper control group, the beneficial effects of acupuncture can be overestimated. A large, double-blind, randomized, controlled trial is required to provide reliable evidence. Third, the follow-up period after the treatment may not have been of sufficient duration. Although the effects of acupuncture were maintained at a 4-week follow-up in this study, long-term follow-up results are required to clarify the efficacy of acupuncture, because the duration of the intervention was shorter than those of previous studies.18–20,22 Finally, a validated measure of hot flashes was not included in this study. It would be helpful if objective measurements of changes in hot flashes were available, as facial temperature measured by infrared thermography failed to show reliable results in this study.
Despite these limitations, to the best of the authors' knowledge, this is the first study to show the feasibility and safety of acupuncture for the treatment of hot flashes in Korean patients with breast cancer who are undergoing antiestrogen therapy. The results of this study showed a mean reduction of >60% in hot flashes, which is comparable to the results of previous studies.13,16,17 Furthermore, this study was performed with a standardized algorithm of TKM, which allows for replication in future biomedical studies, and suggests that TKM may be a viable treatment for women with chemotherapy-induced menopause-related hot flashes. This study's results provide important preliminary data indicating that acupuncture is a good alternative treatment for hot flashes among patients with breast cancer in Korea.
Conclusions
The present results showed the feasibility and safety of acupuncture for the treatment of hot flashes in Korean patients with breast cancer receiving antiestrogen therapy. These findings suggest that acupuncture is a useful alternative treatment for alleviation of facial flashes in patients with breast cancer who are undergoing antiestrogen therapy. A randomized, controlled, prospective study with a larger sample size is required to clarify the efficacy of acupuncture for such patients in Korea.
Acknowledgements
This study was supported by a grant of the Ministry of Health and Welfare, Republic of Korea (Project No: 20-11-0-090-091-3000-3033-320).
Disclosure Statement
The authors declare that no competing financial interests exist.
References
- 1.Korea Central Cancer Registry. Seoul: Ministry of Health and Welfare; 2010. Annual Report of Cancer Statistics in Korea in 2008; p. 25. [Google Scholar]
- 2.Kohler B. Ward E. McCarthy BJ, et al. Annual Report to the nation on the status of cancer, 1975–2007, featuring tumors of the brain and other nervous system. J Natl Cancer Inst. 2011;103:714–736. doi: 10.1093/jnci/djr077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kronenberg F. Hot flashes: Phenomenology, quality of life, and search for treatment options. Exp Gerontol. 1994;29:319–336. doi: 10.1016/0531-5565(94)90012-4. [DOI] [PubMed] [Google Scholar]
- 4.Carpenter JS. Andrykowski MA. Cordova M, et al. Hot flashes in post menopausal women treated for breast carcinoma: Prevalence, severity, correlates, management, and relation to quality of life. Cancer. 1998;82:1682–1691. [PubMed] [Google Scholar]
- 5.Holmberg L. Andersson H. HABITS (hormonal replacement therapy–is it safe?), A randomized comparison trial stopped. Lancet. 2004;363:453–455. doi: 10.1016/S0140-6736(04)15493-7. [DOI] [PubMed] [Google Scholar]
- 6.Sassarini J. Lumsden MA. Hot flushes: Are there effective alternatives to estrogen? Menopause Int. 2010;16:81–88. doi: 10.1258/mi.2010.010007. [DOI] [PubMed] [Google Scholar]
- 7.Molassiotis A. Fernandez-Ortega P. Pud D, et al. Use of complementary and alternative medicine in cancer patients: A European survey. Ann Oncol. 2005;16:655–663. doi: 10.1093/annonc/mdi110. [DOI] [PubMed] [Google Scholar]
- 8.Richardson MA. Sanders T. Palmer JL, et al. Complementary/alternative medicine use in a comprehensive cancer center and the implications for oncology. J Clin Oncol. 2000;18:2505–2514. doi: 10.1200/JCO.2000.18.13.2505. [DOI] [PubMed] [Google Scholar]
- 9.Daley A. MacArthur C. McManus R, et al. Factors associated with the use of complementary medicine and non-pharmacological interventions in a symptomatic menopausal women. Climacteric. 2006;9:336–346. doi: 10.1080/13697130600864074. [DOI] [PubMed] [Google Scholar]
- 10.Kronenberg F. Fugh-Berman A. Complementary and alternative medicine for menopausal symptoms: A review of randomized, controlled trials. Ann Intern Med. 2002;137:805–813. doi: 10.7326/0003-4819-137-10-200211190-00009. [DOI] [PubMed] [Google Scholar]
- 11.Avis NE. Legault C. Coeytaux RR, et al. A randomized, controlled pilot study of acupuncture treatment for menopausal hot flashes. Menopause. 2008;15:1070–1078. doi: 10.1097/gme.0b013e31816d5b03. [DOI] [PubMed] [Google Scholar]
- 12.Vincent A. Barton DL. Mandrekar JN, et al. Acupuncture for hot flashes: A randomized, sham-controlled clinical study. Menopause. 2007;14:45–52. doi: 10.1097/01.gme.0000227854.27603.7d. [DOI] [PubMed] [Google Scholar]
- 13.Wyon Y. Wijma K. Nedstrand E. Hammar M. A comparison of acupuncture and oral estradiol treatment of vasomotor symptoms in postmenopausal women. Climacteric. 2004;7:153–164. doi: 10.1080/13697130410001713814. [DOI] [PubMed] [Google Scholar]
- 14.Tukmachi E. Treatment of hot flushes in breast cancer patients with acupuncture. Acupunct Med. 2000;18:22–27. [Google Scholar]
- 15.Porzio G. Trapasso CT. Martelli S, et al. Acupuncture in the treatment of vasomotor symptoms in postmenopausal women taking Tamoxifen. Tumori. 2002;88:128–130. doi: 10.1177/030089160208800209. [DOI] [PubMed] [Google Scholar]
- 16.De Valois BA. Young TE. Robinson N, et al. Using traditional acupuncture for breast cancer-related hot flashes and night sweats. J Altern Complement Med. 2010;16:1047–1057. doi: 10.1089/acm.2009.0472. [DOI] [PubMed] [Google Scholar]
- 17.Hervik J. Mjåland P. Acupuncture for the treatment of hot flashes in breast cancer patients, a randomized, controlled trial. Breast Cancer Res Treat. 2009;116:311–316. doi: 10.1007/s10549-008-0210-3. [DOI] [PubMed] [Google Scholar]
- 18.Deng G. Vickers A. Yeung S. Cassileth B. Randomized, controlled trial of acupuncture for the treatment of hot flashes in breast cancer patients. J Clin Oncol. 2007;25:5584–5590. doi: 10.1200/JCO.2007.12.0774. [DOI] [PubMed] [Google Scholar]
- 19.Walker EM. Rodriguez AI. Ball RM, et al. Acupuncture versus venlafaxine for the management of vasomotor symptoms in patients with hormone receptor-positive breast cancer: A randomized controlled trial. J Clin Oncol. 2010;28:634–640. doi: 10.1200/JCO.2009.23.5150. [DOI] [PubMed] [Google Scholar]
- 20.Frisk J. Carlhall S. Kallstrom AC, et al. Long-term follow-up of acupuncture and hormone therapy on hot flushes in women with breast cancer: A prospective, randomized, controlled multicenter trial. Climacteric. 2008;11:166–174. doi: 10.1080/13697130801958709. [DOI] [PubMed] [Google Scholar]
- 21.Davies FM. The effect of acupuncture treatment on the incidence and severity of hot flushes experienced by women following treatment for breast cancer: A comparison of traditional and minimal acupuncture. Eur J Cancer. 2001;37:S438–S438. [Google Scholar]
- 22.Nedstrand E. Wijma K. Wyon Y. Hammar M. Vasomotor symptoms decrease in women with breast cancer randomized to treatment with applied relaxation or electro-acupuncture: A preliminary study. Climacteric. 2005;8:243–250. doi: 10.1080/13697130500118050. [DOI] [PubMed] [Google Scholar]
- 23.Liljegren A. Gunnarsson P. Landgren BM, et al. Reducing vasomotor symptoms with acupuncture in breast cancer patients treated with adjuvant tamoxifen: A randomized controlled trial. Breast Cancer Res Treat. 2012;135:791–798. doi: 10.1007/s10549-010-1283-3. [DOI] [PubMed] [Google Scholar]
- 24.Johnstone PA. Polston GR. Niemtzow RC. Martin PJ. Integration of acupuncture into the oncology clinic. Palliat Med. 2002;16:235–239. doi: 10.1191/0269216302pm540oa. [DOI] [PubMed] [Google Scholar]
- 25.Miller HG. Li RM. Measuring hot flashes: Summary of a National Institutes of Health workshop. Mayo Clin Proc. 2004;79:777–771. doi: 10.4065/79.6.777. [DOI] [PubMed] [Google Scholar]
- 26.Kim DI. Roh JJ. Choi MS, et al. A clinical trial to assess the efficacy of acupuncture on hot flashes in postmenopausal women. Korean J Oriental Med. 2007;28:74–85. [Google Scholar]
- 27.Association of Korean Oriental Medicine. Seoul: Association of Korean Oriental Medicine; 1998. Oriental Medicine of Korea. [Google Scholar]
- 28.Deadman P. Baker K. Al-khafaji M. Ann Arbor, MI: Cushing Mallory; 2001. A Manual of Acupuncture: Journal of Chinese Medicine Publications. [Google Scholar]
- 29.Ahn YK Meridianology Series. Seoul: Seongbosa; 1886. [Google Scholar]
- 30.Kaptchuk TJ. Acupuncture: Theory, efficacy, and practice. Ann Intern Med. 2002;136:374–383. doi: 10.7326/0003-4819-136-5-200203050-00010. [DOI] [PubMed] [Google Scholar]
- 31.Richardson A. The health diary: An examination of its use as a data collection method. J Adv Nurs. 1994;19:782–791. doi: 10.1111/j.1365-2648.1994.tb01151.x. [DOI] [PubMed] [Google Scholar]
- 32.Ezzo J. Berman B. Hadhazy VA, et al. Is acupuncture effective for the treatment of chronic pain? A systematic review. Pain. 2000;86:217–225. doi: 10.1016/S0304-3959(99)00304-8. [DOI] [PubMed] [Google Scholar]
- 33.De-Craen AJ. Moerman DE. Heisterkamp SH, et al. Placebo effect in the treatment of duodenal ulcer. Br J Clin Pharmacol. 1999;48:853–860. doi: 10.1046/j.1365-2125.1999.00094.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee BY. Lariccia PJ. Newberg AB. Acupuncture in theory and practice part I: Theoretical basis and physiologic effects. Hosp Physician. 2004;40:11–18. [Google Scholar]
- 35.Napadow V. Ahn A. Longhurst J, et al. The status and future of acupuncture mechanism research. J Altern Complement Med. 2008;14:861–869. doi: 10.1089/acm.2008.SAR-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Macioca G. New York: Churchill Livingstone; 1994. The Practice of Chinese Medicine. [Google Scholar]
- 37.Carpenter JS. Monahan PO. Azzouz F. Accuracy of subjective hot flush reports compared with continuous sterna skin conductance monitoring. Obstet Gynecol. 2004;104:1322–1326. doi: 10.1097/01.AOG.0000143891.79482.ee. [DOI] [PubMed] [Google Scholar]
- 38.Otte JL. Flockhart D. Storniolo AM, et al. Comparison of subjective and objective hot flash measures over time among breast cancer survivors initiating aromatase inhibitor therapy. Menopause. 2009;16:653–629. doi: 10.1097/gme.0b013e3181a5d0d6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim HJ. Leem KH. Kim MH. Correlation between subjective and objective measurement of climacteric women's hot flashes. J Korean Acad Nurs. 2010;40:765–774. doi: 10.4040/jkan.2010.40.6.765. [DOI] [PubMed] [Google Scholar]
- 40.Sturdee DW. Reece BL. Thermography of menopausal hot flushes. Maturitas. 1979;1:201–205. doi: 10.1016/0378-5122(79)90009-4. [DOI] [PubMed] [Google Scholar]
- 41.Birch S. Hesselink JK. Jonkman FAM, et al. Clinical research on acupuncture. Part 1. What have reviews of the efficacy and safety of acupuncture told us so far? J Altern Complement Med. 2004;10:468–480. doi: 10.1089/1075553041323894. [DOI] [PubMed] [Google Scholar]