Abstract
INTRODUCTION
Post traumatic diaphragmatic hernia is very often missed particularly in polytrauma patients. We present case of an isolated post traumatic diaphragmatic hernia with strangulation, a very rare finding.
PRESENTATION OF CASE
A 35 year old man presented with features of intestinal obstruction with past history of a seemingly trivial blunt thoracic injury 15 years back. Findings of X-ray abdomen and chest with high leukocyte count raised suspicion of obstructed diaphragmatic hernia which on exploration revealed obstructed diaphragmatic hernia with gangrenous bowel segment.
DISCUSSION
Blunt injury of diaphragm is relatively common and is considered as a marker of severe trauma and it can clinically be occult as other violent injuries may mask and disguise its initial clinical presentation1 resulting in late presentation with obstruction and/or rarely strangulation. An early diagnosis of the condition is prudent to avoid morbidity and mortality associated with late presentations.
CONCLUSION
In a patient of intestinal obstruction with history of even trivial throraco- abdominal injury, diagnosis of diaphragmatic hernia should be kept in mind.
Keywords: Strangulation, Traumatic diaphragmatic hernia
1. Introduction
Post traumatic diaphragmatic hernia, a rare condition, may occur after blunt/penetrating injuries and usually is associated with multiple traumatic injuries. The incidence of diaphragmatic hernia in patients with multiple traumatic injuries is around 0.8–5%.2,9,11–13 In spite of rising incidence of traumatic diaphragmatic hernias, the diagnosis is frequently missed due to lack of typical symptoms and/or due to other major injuries resulting in late presentation of the condition with increased morbidity and mortality.1 An isolated diaphragmatic blunt trauma injury is rare.9,10 We report a case of an undiagnosed left diaphragmatic hernia presenting as acute intestinal obstruction, with strangulation of small intestine, 15 years after trauma.
2. Presentation of case
A 35 year old male presented to the surgical emergency with complaint of diffuse abdominal pain with distension and constipation for 15 days. He developed obstipation with multiple episodes of bilious vomiting 2 days prior to presentation. Patient had history of blunt chest trauma 15 years back which was managed conservatively. Patient did not have any other major abdominal/limb injury at that time. There was history of chronic alcohol intake and smoking for past 10 years. There was no history of dyspnea, fever and jaundice.
On examination, abdomen was distended, non-tender, with no guarding and rigidity and was resonant on percussion. On auscultation there were absent bowel sounds with decreased breath sound in the left lower lung zone. Rest parameters were within normal limits.
On investigation, X-ray abdomen erect showed multiple air-fluid levels and chest radiograph showed bowel loops in the left lower lung zone with multiple air fluid levels (Fig. 1). Total leukocyte count was 14,800/μl. Rest parameters were normal. On nasogastric tube aspiration, feculent fluid was aspirated.
Fig. 1.
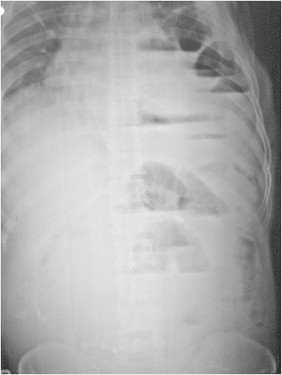
X ray abdomen and chest.
On exploration, there were enormously dilated bowel loops. Distal ileum as well as transverse colon (near splenic flexure) was seen herniating into left hemi-diaphragmatic defect with irregular margins of size 5 cm× 2 cm, with strangulation of herniated ileum (Figs. 2 and 3). Around 1.5 ft of distal ileal herniated loop was found to be gangrenous which was resected and anastomosed, herniated transverse colon was normal. The defect was repaired without mesh, in two layers: diaphragm with polypropylene 1-0 interrupted, and peritoneum with polyglactin 3-0 continuous sutures and a chest drain was placed in the left hemi-thorax.
Fig. 2.
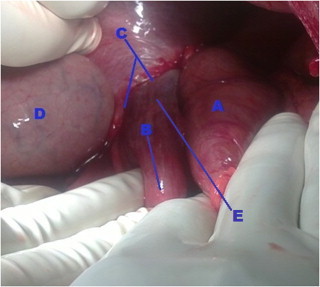
Intra operative view. (A) Herniated transverse colon; (B) herniated small intestine; (C) left hemi-diaphragmatic defect; (D) stomach; (E) gangrenous portion of herniated small intestine.
Fig. 3.
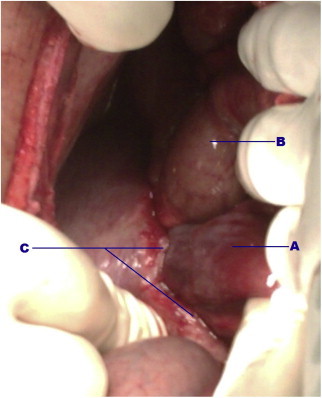
Intra operative view. (A) Herniated small intestine; (B) herniated transverse colon; (C) left hemi-diaphragmatic defect.
Patient was perioperatively managed with Inj. Ceftriaxone 1 g I.V. BD, Inj. Amikacin 500 mg I.V. BD, and Inj. Metronidazole 500 mg I.V. TDS till 5 days post op.
Post operatively patient's recovery was uneventful and chest drain was removed after 4 days. Histopathology report showed mucosal ulcerations covered with fibrinosuppurative exudation along focal areas of gangrenous change. Mesentery showed thrombosed vessels and acute and chronic non-specific inflammation.
3. Discussion
Post traumatic diaphragmatic hernia is displacement of intra-abdominal organs into chest through a pathological aperture in the diaphragm as a result of trauma. Because post traumatic diaphragmatic hernia does not always have hernial sac, some authors use the term “false hernia.” However, the presence or absence of a hernia sac has only a little impact on the clinical course and medical tactics, and the term “post traumatic diaphragmatic hernia” is generally accepted in the medical literature.4
It is believed that diaphragmatic injury occurs in 5% of patients with multiple traumatic injuries. Among diaphragmatic injuries due to blunt trauma, 70% occur on the left side primarily because the right diaphragm is protected by the liver. Post traumatic diaphragmatic hernia results from blunt trauma injuries such as motor vehicle accidents in 80% cases. Penetrating injuries such as stab wounds and gunshot wounds are associated with rest 20% cases.2
Interestingly, respiratory or abdominal symptoms following diaphragmatic hernia may manifest long after injury and delay in diagnosis >10 years is not uncommon.2 There has been report of a traumatic diaphragmatic hernia remaining asymptomatic for 40 years.3 Missed diaphragmatic injuries may occur due to delayed rupture or due to delayed detection. In delayed rupture, the muscle is devitalized at the time of initial injury and acts as a barrier to herniation temporarily only to give away later.5 According to the duration of the injury, traumatic diaphragmatic rupture can be categorized into three groups: early/acute, i.e. immediately or within 14 days post injury; latent, diagnosed after acute injury but before obstruction/strangulation; late where diagnosis is established after obstruction or strangulation sets in.1 When diaphragmatic injuries cannot be recognized in the acute phase of the trauma, the affected structures may be strangulated into the thorax, and therefore, the mortality rate may increase from 20 to 80%.6
Tube thoracostomy, for management of associated hemothorax or pneumothorax should be carried out with caution in those patients suspected of having diaphragmatic injury, to avoid further trauma to the herniated abdominal viscera.14 Surgical repair is the treatment of choice in all diaphragmatic hernias.
Clinical diagnosis of a ruptured hemi-diaphragm is difficult but may be suggested by the presence of audible bowel sounds, absent breath sounds on the affected side and respiratory distress. On a chest radiograph, the diagnostic criteria suggestive of a ruptured diaphragm are the presence of bowel loops in the chest, a nasogastric tube above the diaphragm and a markedly elevated hemi-diaphragm.7
Approximately 23–73% of traumatic diaphragmatic ruptures will be detected by initial chest radiograph, with an additional 25% found with subsequent films.8 Chest radiographic findings that indicate traumatic rupture include
-
1.
abdominal contents in the thorax, with or without signs of focal constriction (“collar sign”),
-
2.
nasogastric tube seen in the thorax,
-
3.
elevated hemi-diaphragm (>4 cm higher on left vs. right) and
-
4.
distortion of diaphragmatic margin.
When the clinical and chest radiographic findings suggest a diaphragmatic injury, appropriate contrast gastrointestinal studies may be helpful as conclusive diagnostic tools. The nasogastric tube may be helpful, but a forceful attempt to pass the tube should be avoided. During exploratory laparotomy, meticulous inspection and palpation of entire diaphragm is mandatory in trauma cases.6
4. Conclusion
A diagnosis of diaphragmatic hernia must be kept in mind in patients with thoraco-abdominal trauma by giving due attention to chest radiograph and CT if necessary to avoid delayed presentations associated with increased morbidity and mortality.
Conflict of interest statement
None.
Funding
None.
Ethical approval
I have obtained a written and informed consent from the patient.
Author contributions
Dr. Shailesh Kumar: study concept & design and approval. Dr. Santosh Kumar: analysis and interpretation of data. Dr. Shubhendu bhaduri: analysis and interpretation of data. Dr. Sumit More: writing and drafting article. Dr. Priyadarshi Dikshit: writing and drafting article.
References
- 1.Petrone P., Leppaniemi A., Inaba K., Soreide K., Asensio J.A. Diaphragmatic injuries: challenges in the diagnosis and management. Trauma. 2007;9:227–236. [Google Scholar]
- 2.Jeyarajah R., Harford W.V. Sliesenger and Fordtran's gastrointestinal and liver disease. 8th ed. Saunders, Elsevier; 2006. Abdominal hernias and gastric volvulus. p. 477–81. [Google Scholar]
- 3.Dexter J.R., Gold P.M. Acute onset of dyspnoea associated with colonoscopy. Journal of the American Medical Association. 1980;244:1239–1240. [PubMed] [Google Scholar]
- 4.Crandall M., Popowich D., Shapiro M., West M. Posttraumatic hernias: historical overview and review of the literature. The American Surgeon. 2007;73(9):845–850. [PubMed] [Google Scholar]
- 5.Yilmaz M., Isik B., Ara C., Yilmaz S., Kutlu R., Kocak O. Gastric perforation during chest tube placement for acute diaphragmatic rupture and review of the literature. Injury Extra. 2006;37:71–75. [Google Scholar]
- 6.Shetty P., Selvaraju K. A rare case of isolated blunt traumatic diaphragmatic rupture. WebmedCentral Gastrointestinal Surgery. 2010;1(11):WMC001183. [Google Scholar]
- 7.Gelman R., Mirvis S.E., Gens D. Diaphragmatic rupture due to blunt trauma: sensitivity of plain chest radiographs. American Journal of Roentgenology. 1991;156:51–57. doi: 10.2214/ajr.156.1.1898570. [DOI] [PubMed] [Google Scholar]
- 8.Sliker C. Imaging of diaphragm injuries. Radiologic Clinics of North America. 2006;44:199–211. doi: 10.1016/j.rcl.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 9.Rashid F., Chakrabarty M.M., Singh R., Iftikhar S.Y. A review on delayed presentation of diaphragmatic rupture. World Journal of Emergency Surgery. 2009;4(August):32. doi: 10.1186/1749-7922-4-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ward R.E., Flynn T.C., Clark W.P. Diaphragmatic disruption secondary to blunt abdominal trauma. Trauma. 1981;21:35–38. doi: 10.1097/00005373-198101000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Schumpelick V., Steinau G., Schluper I., Prescher A. Surgical embryology and anatomy of the diaphragm with surgical applications. Surgical Clinics of North America. 2000;80:213–239. doi: 10.1016/s0039-6109(05)70403-5. [DOI] [PubMed] [Google Scholar]
- 12.Chughtai T., Ali S., Sharkey P., Lins M., Rizoli S. Update on managing diaphragmatic rupture in blunt trauma: a review of 208 consecutive cases. Canadian Journal of Surgery. 2009;52:177–181. [PMC free article] [PubMed] [Google Scholar]
- 13.Nishijima D., Zehbtachi S., Austin R.B. Acute posttraumatic tension gastrothorax mimicking acute tension pneumothorax. American Journal of Emergency Medicine. 2007;25:734–736. doi: 10.1016/j.ajem.2006.12.019. [DOI] [PubMed] [Google Scholar]
- 14.Akhtar M.S., Beg M.H., Kumar A. Isolated traumatic giant diaphragmatic hernia mimicking a haemopneumothorax: a report of two cases. The Indian Journal of Chest Diseases & Allied Sciences. 2012;54:259–326. [Google Scholar]


