Abstract
INTRODUCTION
Malignant paratesticular tumours are rare. We report a case of paratesticular malignant mesothelioma in a patient who had excision of an adenomatoid tumour on the same site in 2 occasions previously.
PRESENTATION OF CASE
A middle aged man who had an adenomatoid tumour excised from his left hemiscrotum fifteen years previously was referred with a suspicious left epididymal lump. This was followed up sonographically for 2 years until it showed signs of enlargement and testicular invasion; it was then managed with radical orchidectomy. The histology showed paratesticular epithelioid malignant mesothelioma. The patient was referred to the Oncologists for further management.
DISCUSSION
Paratesticular tumours are commonly benign. Scrotal ultrasonography is the preferred diagnostic imaging method. Paratesticular malignant mesotheliomas are very rare and appear to have poor prognosis. The optimal adjuvant treatment post radical orchidectomy is not established yet. In our case there is suggestion of possible malignant transformation from previous adenomatoid tumour.
CONCLUSION
In recurrent paratesticular tumours the clinicians should question the possibility of malignant transformation and manage these cases accordingly.
Keywords: Paratesticular tumour, Mesothelioma, Adenomatoid tumour
1. Introduction
Malignant paratesticular tumours are rare clinical entities with heterogenous pathogenesis and behaviour. We report a case of paratesticular malignant mesothelioma which developed on the site of previously excised epididymal adenomatoid tumour.
2. Presentation of case
A 55 year-old patient was referred to the Urology clinic due to a palpable lump in the left hemiscrotum in 2009. He had previously had excision of a left epididymal adenomatoid tumour in 1993 and further exploration and excision of recurrent adenomatoid tumour on the same site in 1997.
On this presentation he complained of a small palpable lump on the top of his left testis which was intermittently painful and has grown in size over the previous 12 months. He had no other significant medical history. On clinical examination a small tender hard lesion was felt on the left epididymal head. On subsequent ultrasound scan a hyperechoic lobular area (1.6 cm in diameter) was noted on the left epididymal head with a normal ipsilateral testicle (Fig. 1). The differential diagnosis included a recurrent adenomatoid tumour or rarer clinical entities such as sarcoma, adenocarcinoma or mesothelioma.
Fig. 1.

Scrotal ultrasound scan demonstrating a hyperechoic area on the left epididymalhead with a normal left testicular parenchyma.
The patient was offered exploration of the left hemiscrotum and excision of the lesion but he refused as he was concerned of possible chronic scrotal pain. Thus a decision was made to keep the lesion under surveillance with 6-monthly clinical and sonographic evaluation.
The lesion did not change in morphology or size in the following sequential scans for approximately 2 years, until there was marginal increase in its size (2 cm in diameter) and finding of high attenuation areas in the parenchyma of the left testicle (Fig. 2). Due to the suggestion of infiltration to the testicle the patient was offered and agreed to undergo left radical orchidectomy. The pre-operative testicular tumour markers were normal.
Fig. 2.

Scrotal ultrasound scan demonstrating a marginal increase on the left epididymalhead hyperechoic lesion and high attenuation areas in the left testicular parenchyma.
Pathologically the lesion was reported as a paratesticular epithelioid malignant mesothelioma involving the epididymis, the tunica vaginalis and superficially infiltrating the adjacent testicle. Macroscopically the tumour gave a white and firm appearance to the epididymis and microscopically it had a solid and focal tubulopapillary pattern with numerous psammoma bodies. There was no sarcomatoid component or lymphovascular permeation. The immunohistochemistry demonstrated positive staining for CK5/6, WT1, BerEP4, CK7 and focally positive staining for Calretinin and LeuMl (Fig. 3).
Fig. 3.
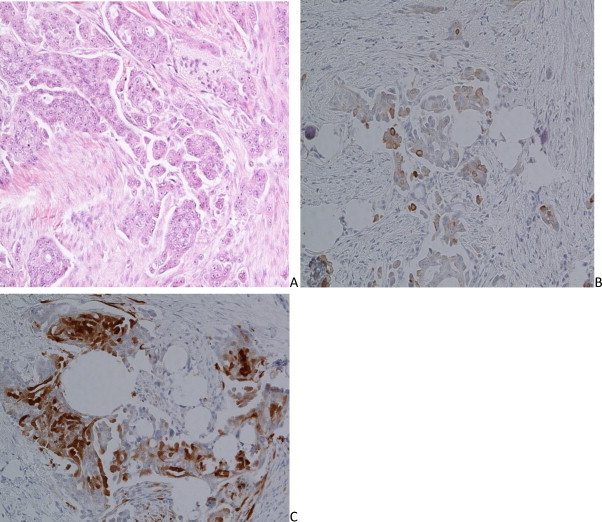
Histopathologic examination of the specimen.
The patient made an uneventful recovery and was referred to the regional Oncology team for further management.
3. Discussion
Paratesticular tumours arise from the structures surrounding the testicles including the epididymis, tunica albuginea, tunica vaginalis and the spermatic cord structures. The vast majority of them (70–78%)1,2 are benign with the commonest being the adenomatoid tumours.1 Clinical features of a painful or painless mass do not help to distinguish a benign from a malignant lesion.2 Scrotal ultrasonography remains the primary imaging method; generally benign tumours appear as hyperechoic homogenous masses and malignant tumours as either homogeneously hypoechoic or have a heterogeneous pattern.3,4 Local surgical excision is the treatment for the benign paratesticular tumours.1 Local recurrences have been reported but no malignant transformation has been reported till now.
Malignant paratesticular tumours are rare; the commonest are sarcomas.1 Paratesticular malignant mesotheliomas are even rarer entities which usually present in patients between ages 55 and 75 years.5 Previous exposure to asbestos is considered as a risk factor.5,6 Patients usually present with a palpable scrotal mass or recurrent hydrocoele; in most cases the diagnosis is made intra-operatively due to lack of pathognomonic clinical and sonographic characteristics.1,5 Radical orchidectomy is considered as the first line therapy. In cases of previous scrotal violation (i.e. scrotal exploration or epididymectomy for chronic scrotal pain) excision of ipsilateral hemiscrotum at the time of radical orchidectomy has been advocated.7 The optimal adjuvant treatment is yet to be confirmed; Open retroperitoneal lymph node dissection with therapeutic intend has been reported in a case of metastatic disease.8 Staging laparoscopic lymph node dissection has also been performed.7 Adjuvant radiotherapy or chemotherapy is generally advised.5 However strict recommendations on the role of adjuvant therapy or staging laparoscopy cannot be made due to limited available evidence.7 The tumour's histological pattern and differentiation seems to play an important role in the prognosis.9 The median overall survival so far has been calculated to 24 months.10
In our case we report the diagnosis of a paratesticular mesothelioma which was excised from the area of a previously excised benign paratesticular tumour. This could potentially represent malignant transformation. To our knowledge this has not been published so far in the literature.
4. Conclusion
In those cases of recurrent paratesticular tumours (previously diagnosed as benign) the clinicians cannot continue to assume that the pathology will be benign again. As the clinical behaviour of the paratesticular tumours has not been completely understood we advocate a long term follow-up for the patients who had a benign paratesticular tumour excised.
Conflict of interest statement
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
I can confirm that the authors of this manuscript have made substantial contributions to all of the following: the conception and design of the study, drafting the article or revising it critically for important intellectual content, final approval of the version to be submitted. The Guide for authors has been read. I can also confirm that we had no writing assistance and have no other person to acknowledge. I can also confirm that this manuscript, has not been previously published and that the manuscript is not under consideration elsewhere.
References
- 1.Khoubehi B., Mishra V., Ali M., Motiwala H., Karim O. Adult paratesticular tumours. BJU International. 2002;90(November (7)):707–715. doi: 10.1046/j.1464-410x.2002.02992.x. [DOI] [PubMed] [Google Scholar]
- 2.Lioe T.F., Biggart J.D. Tumours of the spermatic cord and paratesticular tissue. A clinicopathological study. British Journal of Urology. 1993;71(May (5)):600–606. doi: 10.1111/j.1464-410x.1993.tb16033.x. [DOI] [PubMed] [Google Scholar]
- 3.Fields J.M., Russell S.A., Andrew S.M. Ultrasound appearances of a malignant mesothelioma of the tunica vaginalis testis. Clinical Radiology. 1992;46:128–130. doi: 10.1016/s0009-9260(05)80318-6. [DOI] [PubMed] [Google Scholar]
- 4.Vick C.V., Bird K.I.J., Rosenfield A.T., Viscomi G.N., Taylor K.J.W. Scrotal masses with uniform hyperechoic pattern. Radiology. 1983;148:209–211. doi: 10.1148/radiology.148.1.6856837. [DOI] [PubMed] [Google Scholar]
- 5.Plas E., Riedl C.R., Pfluger H. Malignant mesothelioma of the tunica vaginalis testis. Review of literature and assessment of prognostic parameters. Cancer. 1998;83:2437–2446. doi: 10.1002/(sici)1097-0142(19981215)83:12<2437::aid-cncr6>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 6.Vijayan S, Carr R, Strachan J. Primary and secondary mesothelioma of the tunica vaginalis: a comparative case study. Bjui.org. http://dx.doi.org/10.1002/BJUIw-2011-127-web.
- 7.Esen T., Acar O., Peker K., Sarman K., Musaoglu A., Tefekli A. Malignant mesothelioma of the tunica vaginalis: presenting with intermittent scrotal pain and hydrocele. Case Reports in Medicine. 2012;2012:189170. doi: 10.1155/2012/189170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith J.J., Malone M.J., Geffin J., Silverman M.L., Libertino J. A retroperitoneal lymph node dissection in malignant mesothelioma of tunica vaginalis testis. Journal of Urology. 1990;144(5):1242–1243. doi: 10.1016/s0022-5347(17)39706-9. [DOI] [PubMed] [Google Scholar]
- 9.Brimo F., Illei P.B., Epstein J.I. Mesothelioma of the tunica vaginalis: a series of eight cases with uncertain malignant potential. Modern Pathology. 2010;23(August (8)):1165–1172. doi: 10.1038/modpathol.2010.113. [DOI] [PubMed] [Google Scholar]
- 10.Jones M.A., Young R.H., Scully R.E. Malignant mesothelioma of the tunica vaginalis. A clinicopathologic analysis of 11 cases with review of the literature. American Journal of Surgical Pathology. 1995;19:815–825. doi: 10.1097/00000478-199507000-00010. [DOI] [PubMed] [Google Scholar]


