Abstract
INTRODUCTION
Anastomotic leakage is a severe complication after colorectal surgery which causes substantial morbidity and mortality and impairs the oncologic and functional outcomes. The incidence rate varies in the literature from 4% to 26%. Diagnosis is difficult. Clinical presentation and time management are closely related to prognosis. If subcutaneous emphysema is an obvious clinical sign, its etiology is complex to determine, particularly in the post-operative course of colorectal surgery.
PRESENTATION OF CASE
We report our experience in the management of a patient with early colorectal anastomotic leakage after left colectomy, whose only physical sign was subcutaneous emphysema of thorax, neck and face. This presentation is not described to date. Emergency CT-scan with injection of contrast revealed a pneumoperitoneum with extradigestive air in the pelvis, pneumomediastinum and subcutaneous emphysema. Suture, drainage and defunctioning ileostomy have been performed in emergency with good results. The subcutaneous emphysema resolved spontaneously without specific treatment.
DISCUSSION
There are many differential diagnoses of subcutaneous emphysema and its etiology is potentially lethal. This case is original by the clinical manifestation of anastomotic leakage in the immediate post-operative course of colorectal surgery; this presentation is not described to date.
CONCLUSION
Isolated subcutaneous emphysema after left colectomy should suggest first a post-intubation tracheal wound. This case shows that an anastomotic leakage must be evocated and eliminated in order to provide the best outcome for these patients.
Keywords: Subcutaneous emphysema, Left colectomy, Pneumomediastinum, Pneumoperitoneum, Anastomotic leakage, Colorectal surgery, Tracheal rupture
1. Introduction
Anastomotic leakage is a severe complication after colorectal surgery, which causes substantial morbidity and mortality and impairs the oncologic and functional outcomes.1 Its rate varies in the literature from 4% to 26%. Its diagnosis is difficult, and the clinical presentation and time management are closely related to prognosis. The median time to diagnosis of anastomotic leak is 7 days. Classic clinical features at the time of diagnosis are fever, tachycardia, abdominal pain and occlusion.2 If subcutaneous emphysema is an obvious clinical sign, its etiology is complex to determine, particularly in the post-operative course of colorectal surgery. We report a case of early colorectal anastomotic leakage after elective left colectomy, whose only physical sign was sub-cutaneous emphysema of thorax, neck and face.
2. Presentation of case
A 73-year-old man with no medical history presented a sigmoid Lieberkuhnien adenocarcima revealed by melaena. His performance status was maintained. Staging of the tumor was negative. An elective laparoscopic left colectomy with end-to-end colorectal anastomosis was performed mechanically. We had to convert to median laparotomy due to difficulties of exposure. The anastomosed colon was diverticular. The anastomosis was without tension. The intraoperative test with methylene blue and air at the end of the operation were negative. There were no difficulties during intubation (Cormack 1, easy intubation). Immediate post-operative evolution was favorable.
On day 4, clinical examination revealed large subcutaneous emphysema of the thorax, the neck and the face (Fig. 1). He had no fever, no dyspnea, no sign of sepsis, no pain and the gases were absent. Since the intervention we noted a persistent inflammatory syndrome with hyperleukocytosis (12,000 mm−3) and CRP increased at 200 mg/l. An injected computed tomography in emergency revealed a pneumoperitoneum with presence of extradigestive air in the pelvis (Fig. 2) and in the subphrenic region (Fig. 3), pneumomediastinum and subcutaneous emphysema of thorax, neck and face (Figs. 4 and 5). There was no intra-abdominal effusion, or aspect of peritonitis on the scanner. The rectal opacification made the diagnosis of an anastomotic leakage with contrast leaking lateralized to the right (Figs. 6 and 7). Emergency surgical treatment was decided. Exploratory relaparotomy confirmed the anastomotic fistula on the right side (1 cm) and the absence of peritonitis with a clean pelvis. The fistula was sutured and drained for irrigation and washing. Defunctioning ileostomy was crafted. Adequate empiric antibiotic with tazocilline and aminoglycoside was introduced and the patient was monitored in intensive care unit for 5 days. The post-operative evolution was uneventful. The subcutaneous emphysema persisted until the tenth day after surgery and resolved spontaneously without specific treatment. Drainage ablation was performed on day 15 after CT control which showed no pelvic collection, no anastomotic leakage after rectal opacification and confirmed resorption of subcutaneous emphysema, pneumomediastinum and pneumoperitoneum. There was no complication due to the ileostomy. The patient was discharged 17 days after surgery. The intestinal continuity restoration was delayed due to pulmonary embolism at 1 month. Closure of the ileostomy was performed at the 3rd month after a new rectal opacification confirming the absence of residual fistula. Tumor staging was pT3N0M0. There was no adjuvant treatment. The follow-up at one, three and six month after ileostomy closure did not reveal functional outcomes or recurrence of the tumor.
Fig. 1.

Large subcutaneous emphysema.
Fig. 2.
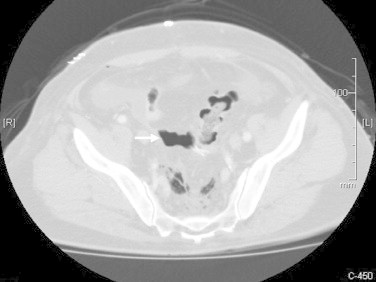
Pelvic pneumoperitoneum.
Fig. 3.
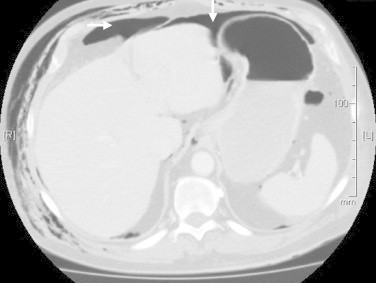
Subphrenic pneumoperitoneum.
Fig. 4.

Subcutaneous emphysema, pneumoperitoneum and pneumomediastinum.
Fig. 5.

Subcutaneous emphysema, pneumoperitoneum and pneumomediastinum.
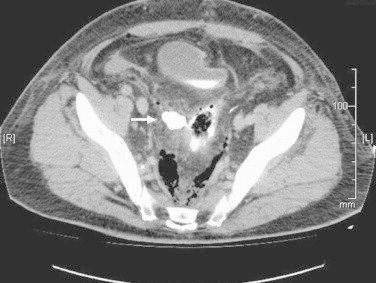
Fig. 6.

Rectal opacification and anastomotic leakage on the right side.
Fig. 7.
Rectal opacification and anastomotic leakage on the right side.
3. Discussion
Subcutaneous emphysema is frequently seen in emergency. There are many differential diagnoses and its etiology may be potentially lethal. It is common after chest trauma, it can also be iatrogenic or infectious as part of a necrotizing fasciitis requiring prompt diagnosis. This case is original by the clinical manifestation of anastomotic leakage in the immediate post-operative course of colorectal surgery; this presentation is not described to date. In the literature, only a few cases of subcutaneous emphysema due to rectal or colonic perforation have been reported, most often associated with gastrointestinal symptoms. Similar cases have been described after rectal barotraumas, pelvic trauma,3 perforation due to fecaloma4,5 or rectal tumor.6 Several cases of perforation with emphysema have been reported following high and low endoscopy, the occurrence of emphysema being facilitated by air insufflation.7,8 We found a case of emphysema of the thigh secondary to rectal perforation after prostatic irradiation, managed initially by the orthopedic surgeons, with a significant diagnosis delay concerning the rectal injury.9
The key feature of this case results from the isolated subcutaneous emphysema, which should suggest first a post-intubation tracheal wound and can lead to delayed diagnosis of anastomotic leakage. After colorectal surgery, body scan with rectal opacification is the best exam to make the diagnosis. The absence of gas in the pelvis is in favor of a tracheal injury and should lead to bronchial fibroscopy.10 If an anastomotic leak is shown on imaging, a revision surgery is necessary in most cases. An anastomotic leakage without localized peritonitis in a patient with few symptoms is a rare situation in which the surgical management is poorly codified. Conservative treatment with suture, drainage and ileostomy diversion resulted in favorable outcomes in this case. Moreover, the large subcutaneous emphysema was amended after 10 days without complication as mediastinitis or necrotizing fasciitis. The risk of infection associated with the dissemination of pneumoperitoneum is poorly documented but seems low and justifies a monitoring of the evolution of subcutaneous emphysema without routine specific treatment.11,12
4. Conclusion
There are many differential diagnoses of subcutaneous emphysema and its etiology is potentially lethal. Isolated subcutaneous emphysema after left colectomy should suggest first a post-intubation tracheal wound. This case shows that an anastomotic leakage must be evocated and eliminated.
Conflict of interest statement
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author's contributions
Souche R – First author. Registrar in charge of patient care. Second surgeon jointly performed the operation. Obtained consent. Written the entire case. Reviewed and proofread case. Performed literature review.
Bouyabrine H. – Second author. Primary surgeon who performed the operation. Assisted in writing case. Proofread and review draft several times. Performed literature search. Also assisted in processing digital image.
Navarro F – Third author. Consultant of the unit, overall responsible for the care of patient. Provided overall supervision, direction and suggestion for the case report. Reviewed and proofread draft and offered critiques.
References
- 1.Branagan G., Finnis D., Wessex Colorectal Cancer Audit Working Group Prognosis after anastomotic leakage in colorectal surgery. Diseases of the Colon and Rectum. 2005;48(May (5)):1021–1026. doi: 10.1007/s10350-004-0869-4. [DOI] [PubMed] [Google Scholar]
- 2.Khan A.A., Wheeler J.M., Cunningham C., George B., Kettlewell M., Mortensen N.J. The management and outcome of anastomotic leaks in colorectal surgery. Colorectal Disease. 2008;10(July (6)):587–592. doi: 10.1111/j.1463-1318.2007.01417.x. [DOI] [PubMed] [Google Scholar]
- 3.Mirzayan R., Cepkinian V., Asensio J.A. Subcutaneous emphysema, pneumomediastinum, pneumothorax, pneumopericardium, and pneumoperitoneum from rectal barotrauma. Journal of Trauma. 1996;41(December (6)):1073–1075. doi: 10.1097/00005373-199612000-00027. [DOI] [PubMed] [Google Scholar]
- 4.Brunet C., Thomas P., Sielezneff I., Ugarte S., Giudicelli R., Sastre B. Subcutaneous cervical emphysema: complication of constipation. Review of the literature. Journal de Chirurgie. 1995;132(April (4)):198–200. [PubMed] [Google Scholar]
- 5.Arana-Arri E., Cortés H., Cabriada V., Lekerika N., García-Verdugo A., Shengelia-Shapiro L. Giant fecaloma causing perforation of the rectum presented as a subcutaneous emphysema, pneumoperitoneum and pneumomediastinum: a case report. European Journal of Emergency Medicine. 2007;14(December (6)):351–353. doi: 10.1097/MEJ.0b013e3282004952. [DOI] [PubMed] [Google Scholar]
- 6.Hajdú N., Zsoldos P., Neuberger G. Rectum tumor diagnosed by subcutaneous emphysema of the chest. Magyar Sebeszet. 2009;62(October (5)):308–311. doi: 10.1556/MaSeb.62.2009.5.4. [DOI] [PubMed] [Google Scholar]
- 7.Cappello M., Randazzo C., Peralta S., Cocorullo G. Subcutaneous emphysema, pneumomediastinum and pneumoperitoneum after diagnostic colonoscopy for ulcerative colitis: a rare but possible complication in patient with multiple risk factors. International Journal of Colorectal Disease. 2011;26(March (3)):393–394. doi: 10.1007/s00384-010-1005-7. [DOI] [PubMed] [Google Scholar]
- 8.Marwan K., Farmer K.C., Varley C., Chapple K.S. Pneumothorax, pneumomediastinum, pneumoperitoneum, pneumoretroperitoneum, and subcutaneous emphysema following diagnostic colonoscopy. Annals of the Royal College of Surgeons of England. 2007;89(July (5)):W20–W21. doi: 10.1308/147870807X188506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saldua N.S., Fellars T.A., Covey D.C. Bowel perforation presenting as subcutaneous emphysema of the thigh. Clinical Orthopedics and Related Research. 2010;468(February (2)):619–623. doi: 10.1007/s11999-009-1015-3. Case report. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martí de Gracia M., Gutiérrez F.G., Martínez M., Dueñas V.P. Subcutaneous emphysema: diagnostic clue in the emergency room. Emergency Radiology. 2009;16(September (5)):343–348. doi: 10.1007/s10140-009-0794-x. [DOI] [PubMed] [Google Scholar]
- 11.Lee K.B., Moon E.S., Jung S.T., Seo H.Y. Subcutaneous emphysema mimicking gas gangrene following perforation of the rectum: a case report. Journal of Korean Medical Science. 2004;19(October (5)):756–758. doi: 10.3346/jkms.2004.19.5.756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Puneet, Mahalik S.K., Gupta S.K. Infective subcutaneous emphysema after laparoscopic rectopexy: a rare complication. Surgical Laparoscopy, Endoscopy and Percutaneous Techniques. 2008;18(June (3)):308–309. doi: 10.1097/SLE.0b013e31816aa119. [DOI] [PubMed] [Google Scholar]


