Abstract
INTRODUCTION
Multiple myeloma is a monoclonal, immunoproliferative plasma-cell neoplasm of the B lymphoid cells. Extramedullary plasmacytoma is a type of plasma-cell neoplasm that can present as a primary tumour or secondary to another plasma-cell neoplasm, such as multiple myeloma. Secondary extramedullary plasmacytoma is usually noted in the advanced stages of the disease with ileum involvement being very rare.
PRESENTATION OF CASE
We report a rare case of a 58-year-old man, with known multiple myeloma, re-presenting with evidence of small bowel obstruction, secondary to an intussusception due to a malignant plasma cell deposit, which was successfully resected at laparotomy. Previous two similar admissions, prior to this index admission, failed to arrive at this difficult rare diagnosis.
DISCUSSION
Primary and secondary extramedullary plasmacytoma mainly affects the upper aero-digestive tract. Involvement of the ileum, as in this case, is a rare complication.
Prognosis of secondary extramedullary plasmacytoma affecting the gastrointestinal tracts is unknown, due to the small number of cases reported in the literature, but suggestive of a poor prognosis. The role of surgery is often palliative to deal with resolvable life-threatening emergencies and where possible to prolong life.
CONCLUSION
The case adds to the current literature of the rare event of visceral secondary extramedullary plasmacytoma involving the gastrointestinal tract, in the course of multiple myeloma and highlights the need for a high index of suspicion for such uncommon complications, to avoid delay in diagnosis and treatment.
Keywords: Multiple myeloma, Extramedullary plasmacytoma, Small bowel obstruction, Intussusception
1. Introduction
Extramedullary plasmacytoma (EMP) is a type of plasma cell neoplasm (PCN) that can present as a primary tumour or secondary to another PCN, such as multiple myeloma (MM). Most reports indicate that EMP commonly affects the upper respiratory tract and oral cavity.1 Gastrointestinal manifestations are rare, particularly involvement of the small intestine. Almost all cases reported in the English language literature are primary in nature.2 We report a rare and unusual case of a patient with a relapse of MM, presenting with small bowel obstruction due to intussusception resulting from secondary EMP, who underwent a small bowel resection.
2. Case presentation
BS, a 58-year-old man presented to the haematology day case unit with nausea, vomiting, abdominal distension and absolute constipation of two days duration. A week earlier he had been briefly admitted for three days with similar symptoms during his fifth cycle of lenolidamide and dexamethasone, with evidence of small bowel dilatation on abdominal radiograph. During that admission he was presumed to have gastroenteritis and treated conservatively with fluids and anti-emetics.
BS was diagnosed two years previously with MM, with monoclonal bands of IgA lambda light chains and multiple lytic lesions on radiological assessment. He was initially treated with cyclophosphomide, thalidomide and dexamethasone with adjuvant high dose melphalan and an autologous stem cell transplant after six months. BS relapsed with monoclonal bands of IgG Kappa six months after the transplant.
On two occasions, one year and also sixth months before this index admission, BS had similar symptoms, which resolved spontaneously at home and did not present to the medical services. On his index admission, the findings included anaemia (Haemoglobin of 11.1 g/dL) and abdominal distension. Small bowel dilatation was confirmed on abdominal X-rays. Due to failure to improve, an abdominal computed tomography (CT) scan was performed which confirmed a small bowel obstruction with an ileo-ileal intussusception in the distal ileum (Fig. 1).
Fig. 1.

Abdominal CT scan showing small bowel intussusception.
At emergency laparotomy an ileo-ileal intussusception was confirmed as well as a nodular mass in the mesentery at the apex of the intussusception (Fig. 2). A wedge resection of 25 cm of the small bowel and mesentery was carried out, with a hand sewn end-to-end anastomosis. All other visceral organs appeared normal.
Fig. 2.
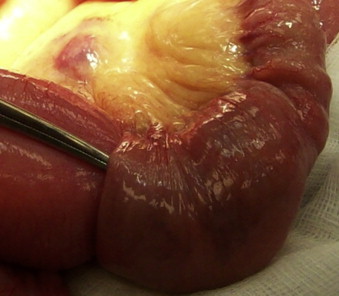
Instrument passed into the intussusceptum of an ileo-ileal intussusception close to nodal tumour deposit in the mesentery.
Histology confirmed a nodule of tumour composed of malignant plasma cells (plasmablastic type) centred within the subserosal and submucosa with focal extension into the lamina propria and ulceration onto the mucosal surface. The tumour cells showed diffuse positive staining for CD138, focal staining with CD79a and lambda light chain restriction. The MIB1 proliferation index was approximately 95%. There was no serosal breach at the leading point of the intussusception noted. Two out of three identified mesenteric nodes were positive for tumour. Given the history of MM, a diagnosis of secondary EMP was made.
BS developed hospital acquired pneumonia during the postoperative period and was discharged home on postoperative day eight, with ongoing treatment with lenalidomide and dexamethasone. He was readmitted two months after surgery with nausea, abdominal distension and electrolyte disturbances. A repeat abdominal CT scan revealed widespread metastases in the paracolic gutters, omentum, hepatic serosa and the retroperitoneum. He was managed by palliative care and died 13 weeks post surgery.
3. Discussion
This case is unusual on account of its rarity. Haematological malignancies are the fifth most common type of cancers in the UK and form a diverse group depending on the origin in the bone marrow derived cells. They can be broadly classified as those neoplasms of myeloid cell lines, neoplasm of lymphoid cell lines, lymphoproliferative disorders and Histiocytic/Dendritic cell neoplasm.
Plasma cell neoplasm (PCN) is a type of haematological malignancy arising as a result of monoclonal proliferation of plasma cells (lymphoid cell line) and associated with production of monoclonal proteins (M Proteins). They include monoclonal gammopathy of undetermined significance (MGUS), solitary plasmacytoma of the bone (SPB), extramedullary plasmacytoma (EMP), and multiple myeloma (MM).
EMP occurs when malignant plasmoblastic clones migrate into soft tissue and represents only 3–4% of all PCN.1 There are two major subtypes of EMP - primary and secondary. In the primary subtype, it occurs alone in the absence of another PCN, unlike in the secondary subtype, often with MM.1 Both primary and secondary EMP predominantly (>70%) affect the upper aero-digestive tract (nasopharynx, oropharynx, hypopharynx, larynx, trachea and oesophagus).2,3
Developing visceral secondary EMP involving the gastrointestinal tract in the course of MM (a monoclonal, immunoproliferative PCN of the B lymphoid cells) is extremely rare – estimated to occur in 0.9% of cases.4 Only 17 cases of EMP affecting the ileum have been reported in the English language literature - almost all primary in nature,1 with only three previous cases of EMP secondary to MM reported.3,5,6 This case falls into the latter category of an even rarer form of secondary EMP involving the ileum leading to small bowel intussusception and obstruction.
This case highlights the need for a high index of suspicion for uncommon complications of MM. It is reasonable to assume that this patient's previous symptoms were related to secondary EMP and should have been considered in his differential diagnosis. Even so, this can be a diagnostic challenge due to susceptibility of patients to gastrointestinal infections in the presence of immunosuppressive treatment. Furthermore, patients with MM have a higher risk of pseudo-obstruction of small bowel due to secondary amyloidosis.7
A primary EMP managed with local radiotheraphy and/or surgical resection has a good prognosis with a 15-year survival rate of 78%.8 In cases of secondary EMP, radiotheraphy or surgery alone is insufficient and systemic therapy is required. In younger patients, the use of immunomodulatory drugs with induction agents in combination with autologus haematopoietic stem cell transplantation results in higher remission rates and overall survival.2 The prognosis of secondary EMP with gastrointestinal involvement is unknown. However, the small number of cases reported in the literature indicates a poor prognosis.2,3,5,6,9,10 The role of surgery in secondary EMP is often palliative, to deal with resolvable life-threatening emergencies and where possible to prolong life.
Conflict of interest statement
None.
Funding
None.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
No alterations have been done that has led to distortion of scientific meaning.
Author contributions
A.A. & N.G. – Drafted the manuscript & made the corrections.
J.A.A. – reviewed & modified the manuscript.
References
- 1.Alexiou C., Kau R.J., Dietzfelbinger H., Kremer M., Spiess J.C., Schratzenstaller B. Extramedullary plasmacytoma. Cancer. 1999;85:2305–2314. [PubMed] [Google Scholar]
- 2.Lopes Da Silva R. Extramedullary plasmacytoma of the small intestine: clinical features, diagnosis and treatment. Journal of Digestive Disease. 2012;13:10–18. doi: 10.1111/j.1751-2980.2011.00544.x. [DOI] [PubMed] [Google Scholar]
- 3.Dzierzanowski M., Porter G.A. An unusual presentation of a secondary extramedullary plasmacytoma in a patient with multiple myeloma. Canadian Journal of Surgery. 2005;48:75–76. [PMC free article] [PubMed] [Google Scholar]
- 4.Talamo G., Cavallo F., Zangari M., Barlogie B., Lee C.K., Pineda-Roman M. Clinical and biological features of multiple myeloma involving the gastrointestinal system. Haematologica. 2006;91:964–967. [PubMed] [Google Scholar]
- 5.Hill S.A., Yudelman P.L. Multiple myelomatosis: an unusual cause of small bowel intussusception. Postgraduate Medical Journal. 1986;62:1043–1044. doi: 10.1136/pgmj.62.733.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tauscher A.E., Orme D.K., Forster J., Damjanov I. Hospital Physician. 2002;67:46–48. [Google Scholar]
- 7.Tada S., Iida M., Yao T., Kitamoto T., Yao T., Fujishima M. Intestinal pseudo-obstruction in patients with amyloidosis: clinicopathologic differences between chemical types of amyloid protein. Gut. 1993;34:1412–1417. doi: 10.1136/gut.34.10.1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galieni P., Cavo M., Pulsoni A., Avvisati G., Bigazzi C., Neri S. Clinical outcome of extramedullary plasmacytoma. Haematologica. 2000;85:47–51. [PubMed] [Google Scholar]
- 9.Vaiopoulos G., Viniou N., Plata E., Konstantopoulos K., Andreopoulos A., Rombos Y. Development of plasma cell tumours during treatment of multiple myeloma. Annals of Hematology. 1996;72:317–320. doi: 10.1007/s002770050178. [DOI] [PubMed] [Google Scholar]
- 10.Griffiths A.P., Shepherd N.A., Beddall A., Williams J.G. Gastrointestinal tumour masses due to multiple myeloma: a pathological mimic of malignant lymphoma. Histopathology. 1997;31:318–323. doi: 10.1046/j.1365-2559.1997.1610866.x. [DOI] [PubMed] [Google Scholar]


