Abstract
INTRODUCTION
Liver rupture is a serious event that is most commonly due to blunt abdominal trauma. We present a case of peliosis hepatis in a patient admitted for acute pyelonephritis who developed hemoperitoneum due to spontaneous hepatic rupture from this rare liver condition.
PRESENTATION OF CASE
We report a 44 year-old woman who presented to our hospital with acute pyelonephrititis and hemoperitoneum due to spontaneous hepatic rupture from peliosis hepatis. Physicians should be aware of this rare condition in patients who present with non-traumatic hepatic rupture with hemoperitoneum.
DISCUSSION
PH should be considered in all patients with known risk factors who present with typical morphological changes or a hepatic mass, especially when the cause of sudden intraperitoneal hemorrhage is obscure.
CONCLUSION
Peliosis hepatis is most often asymptomatic and an incidental finding at autopsy. In symptomatic patients, surgery should be reserved for those patients whose hemorrhage is-life-threatening. Familiarity with the imaging characteristics can help in earlier diagnosis of peliosis hepatis.
Abbreviations: PH, peliosis hepatis; CT, computed tomography; HS, Dhepatic sinusoidal dilatation; RCB, red blood cell
Keywords: Hepatic rupture, Peliosis hepatis, Spontaneous liver rupture
1. Introduction
Liver rupture is a serious event that is most commonly due to blunt abdominal trauma. We present a case of peliosis hepatis in a patient admitted for acute pyelonephritis who developed hemoperitoneum due to spontaneous hepatic rupture from this rare liver condition.
2. Presentation of case
A 44-year-old woman was admitted into our unit through Emergency Room for acute pyelonephritis (fever and abdominal pain). Initially the patient was stable and abdominal examination revealed no abdominal signs. The vital signs were: blood pressure 95/60 mmHg, heart rate 130 beats/min, respiratory rate 28 breaths/min and body temperature 36, 5 °C. The laboratory findings were white blood cell count 6.1 × 10 °C/L (normal 4 × 109–10 × 109/L), hemoglobin 8.9 g/L (normal 13.1–17.5 g/L), normal liver tests, and platelet count 81 × 10 °C/L (normal 140 × 109–400 × 109/L). CT scan (Fig. 1) showed acute left pyelonephritis and a normal liver. Antibiotics were started and the patient was discharged home. Two days later, the patient presented with persistence of fever, abdominal pain and hypovolemic shock; Investigations revealed hemoglobin of 6 g/dL (normal 13.1–17.5 g/L), and platelet count 74 × 10/L (normal 140 × 109–400 × 109/L). Liver function tests showed total bilirubin 7 μmol/L (normal < 1.3 mg/dL), alkaline phosphatase 146 U/L (normal < 220 IU/L), alanine aminotransferase 323 U/L (normal < 43 IU/L), aspartate aminotransferase 412 IU/L (normal < 38 IU/L), prothrombin time 50 s (normal 11–15 s). The serum creatinine was normal. Repeat abdominal CT scan showed many hypodense areas with contrast leakage in the right liver and liver capsule rupture (Fig. 2). The patient received massive red blood cell (8 RBC) transfusion and fluid resuscitation. The clinical condition continued to deteriorate with a platelet count of 40 × 109/L. An emergency exploratory laparotomy was performed and confirmed the liver rupture with many hemorrhagic areas from both sides of the liver. Packing was done after. Several liver biopsies were made (Fig. 3). The postoperative period showed persistence of hemodynamic instability which needed massive transfusions (9 RCB). Two days later a relaparotomy was done and a new packing was changed. The initial postoperative period remained stable. Investigations revealed alanine aminotransferase 3500 U/L, aspartate aminotransferase 1400 U/L, alkaline phosphatase 408 U/L, total bilirubin 28 μmol/L, creatinine 440 μmol/L, lactate 3.6 UI/L (normal 190–390 UI/L), bicarbonate 45 (normal 22–31 mmol/L), prothrombin time 67 s. Another CT scan showed hemoperitoneum due to persistent bleeding from the liver. An arterial embolization was decided. At hepatic angiography performed via the common hepatic artery multiple contrast filling small lesions mainly in the right liver, were shown (Fig. 5). Gel foam embolization was performed successfully and until cessation of extravasation of contrast. On the first day after embolization, another abdominal exploration was carried out, the packings were removed and a new liver biopsy was made. She died soon afterwards because of multiple organ failure. The diagnosis of peliosis hepatis was made histologically (Fig. 4a and b).
Fig. 1.

CT of the abdomen showing the normal liver.
Fig. 2.

CT of the abdomen showing many areas hypodenses in right liver suggesting acute blood collection in these areas.
Fig. 3.
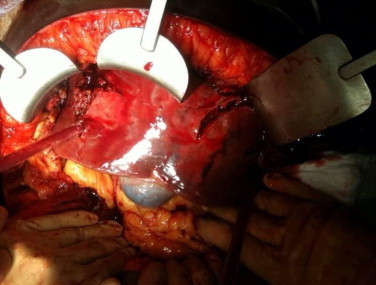
Surface of the liver parenchyma showing many hemorrhagic areas.
Fig. 5.

Late arterial phase from a hepatic angiogram shows hepatic artery branches displaced by a multiple lesions in the right liver (solid arrows). Puddling of contrast from capillaries is seen.
Fig. 4.
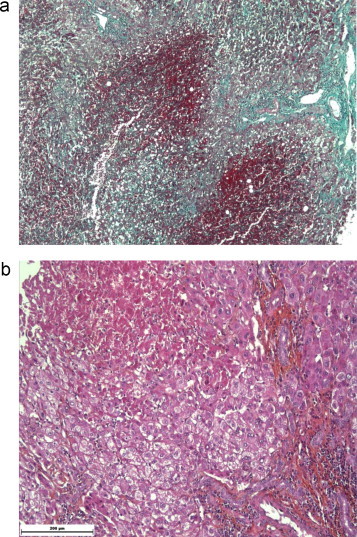
(a) Liver Biopsie: hémorrhagic necrosis on healthy liver. (b) Liver Biopsie: hémorrhagic necrosis on healthy liver.
3. Discussion
Peliosis hepatis is an abnormality of the reticuloendothelial system in the liver. The etiology is still unknown. The association with pregnancy was first described by Abercrombie.1,4,7,8,11 Anabolic steroid use is another potential cause.2 The theory that toxic substances may induce peliosis is supported by the finding of increased endothelial cell permeability with numerous red blood cells in the space of Disse. The idiopathic pure hepatic sinusoidal dilatation (HSD) is associated with immunological features of antiphospholipid syndrome.6,12,16,17 Hepatic rupture affects the right side of liver in 75%, left side in 11% and both sides in 14% of cases.3,5,13 Various forms of surgical procedures have been described to treat this complication including peri-hepatic packing, segmentectomy and hemi-hepatectomy. Treatment should be tailored to the individual case to obtain the best outcome.15 In rare cases, total hepatectomy followed by liver transplantation is the only option available for severe uncontrollable hemorrhage.7 Hepatic rupture is difficult to diagnose9; it is often missed or delayed because its appearance on radiological imaging only suggests a neoplasm or an abscess.18,22 The diagnosis of peliosis hepatis (PH) on angiography is made by visualizing small multiple accumulations of contrast material in the late arterial phase which persists into the venous phase.21 A definitive diagnosis of PH is made from histological findings. Laparotomy appears to be the most appropriate procedure when tissue confirmation is needed. Histological examination permits assessment of macroscopic appearance of peliosis and liver biopsy can be carried out with adequate hemostasis. There is no specific treatment for PH. Conservative management may be appropriate if the patient's condition is stable and the liver capsule is intact. Laparoscopic drainage of hematoma may also play a role in certain patients. Emergency liver transplantation is the ultimate treatment in patients with imminent liver failure.7 The natural course of PH is not well known. Reports have described outcomes ranging from spontaneous resolution to fatal hepatic failure due to intraperitoneal massive hemorrhage.10,14 PH should be considered in all patients with known risk factors who present with typical morphological changes or a hepatic mass, especially when the cause of sudden intraperitoneal hemorrhage is obscure.19,20
4. Conclusions
Peliosis hepatis is most often asymptomatic and an incidental finding at autopsy. In symptomatic patients, surgery should be reserved for those patients whose hemorrhage is life-threatening. Familiarity with the imaging characteristics can help in earlier diagnosis of peliosis hepatis.
Conflict of interest statement
None.
Funding
University of Reims, France.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
A copy of the written consent is available for review by this Editor-in-Chief of the Journal on request.
Author contributions
Elisa Palladino: data collection and writing the case report. Daniele Sommacale: review of literature. Marie Danielle Diebold: pathology imaging. Esther L Tamby: study design. A Reza Kianmanesh: analysis data.
References
- 1.Nelson E.W., Archibald L., Albo D. Spontaneous hepatic rupture in pregnancy. American Journal of Surgery. 1977;134:817–820. doi: 10.1016/0002-9610(77)90333-6. [DOI] [PubMed] [Google Scholar]
- 2.Larrey D., Freneux E., Berson A., Babany G., Degott C., Valla D. Peliosis hepatis induced by 6-thioguanine administration. Gut. 1988;29:1265–1269. doi: 10.1136/gut.29.9.1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adam G., Lesser T., Neumann R. Liver rupture in peliosis hepatis. Zentralblatt fur Chirurgie. 1991;116:399–403. [PubMed] [Google Scholar]
- 4.Smith L.G., Moise K.J., Dildy G.A., Carpentier R.J. Spontaneous rupture of liver during pregnancy: current teraphy. Obstetrics and Gynecology. 1991;77:171–175. doi: 10.1097/00006250-199102000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Hayward S.R., Lucas C.E., Ledgerwood A.M. Recurrent spontaneous intrahepatic hemorrhage from peliosis hepatis. Archives of Surgery. 1991;126:782–783. doi: 10.1001/archsurg.1991.01410300128021. [DOI] [PubMed] [Google Scholar]
- 6.Ludwing J., Hashimoto E., Obata H. Idiopatic portal hypertension. Hepatology. 1993;17:1157–1162. [PubMed] [Google Scholar]
- 7.Hunter S.K., Martin M., Benda J.A., Zlantik F.J. Liver transplant after massive spontaneous hepatic rupture in pregnancy complicated by preeclampsia. Obstetrics and Gynecology. 1995;85:819–822. doi: 10.1016/0029-7844(94)00348-h. [DOI] [PubMed] [Google Scholar]
- 8.Stevenson J.T., Graha D.J. Hepatis haemorrhage ans HELLP syndrome: a surgeon's perspective. American Surgeon. 1995;61:756–760. [PubMed] [Google Scholar]
- 9.Cozzi P.J., Morris D.L. Two cases of spontaneous liver rupture and literature review. HPB Surgery. 1996;9:257–260. doi: 10.1155/1996/24016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jacqemin E., Pariente D., Fabre M., Huault G., Valayer J., Bernard O. Peliosis hepatis with initial presentation as acute hepatic failure and intraperitoneal hemorrhage in children. Journal of Hepatology. 1999;30:1146–1150. doi: 10.1016/s0168-8278(99)80271-2. [DOI] [PubMed] [Google Scholar]
- 11.Sheik R.A., Yasmeen S., Pauly M.P., Riegler J.L. Spontaneous intrahepatic haemorrhage and hepatic rupture in HELLP Syndrome. Journal of Clinical Gastroenterology. 1999;28:323–328. doi: 10.1097/00004836-199906000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Denninger M.H., Chait Y., Casadevall N. Cause of portal or hepatic venous thrombosis in adults: the role of multiple concurrent factors. Hepatology. 2000;31:587–591. doi: 10.1002/hep.510310307. [DOI] [PubMed] [Google Scholar]
- 13.Wang S.Y., Ruggles S., Vade A., Newmann B.M., Borge M.A. Hepatic rupture caused by peliosis hepatis. Journal of Pediatric Surgery. 2001;36:1456–1459. doi: 10.1053/jpsu.2001.26397. [DOI] [PubMed] [Google Scholar]
- 14.Fidelman N., LaBerge J.M., Kerlan R.K. Panel case 4: massive intraperitoneal hemorrhage caused by peliosis hepatis. Journal of Vascular and Interventional Radiology. 2002;13:542–545. doi: 10.1016/s1051-0443(07)61539-5. [DOI] [PubMed] [Google Scholar]
- 15.Toth P., Takacs I., Kerekes L., Sapy P. Surgical Treatment of intraabdominalhemorrhage in peliosis hepatis. Chirurg. 2002;73:83–85. doi: 10.1007/s104-002-8034-5. [DOI] [PubMed] [Google Scholar]
- 16.Saadoun D., Cazals-Hatem D., Denninger M.-H., Boudaoud L., Pham B.-N., Mallet V. Association of idiopathic hepatic sinusoidal dilatation with the immunological features of the antiphospholipid. Gut. 2004;53:1516–1519. doi: 10.1136/gut.2003.037135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tirigotis P., Sella T., Shapira M.Y., Bitan M., Bloom A., Kiselgoff D. Peliosis hepatis following treatment with androgen-steroids in patients with bone marrow failure syndromes. Haematologica. 2007;92:106–110. doi: 10.3324/haematol.11343. [DOI] [PubMed] [Google Scholar]
- 18.Kim E.A., Yoon K.H., Jeon S.J., Cai Q.Y., Lee Y.W., Yoon S.E. Peliosis hepatis with hemorrhagic necrosis and rupture: a case report with Emphasis on the multi-detector CT. Korean Journal of Radiology. 2007;8:64–69. doi: 10.3348/kjr.2007.8.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sun-Keun, Jin J.-S., Cho S.-G., Choi S.-J., Kim C.-S., Choe Y.-M. Spontaneous liver rupture in a patient with peliosis hepatis: a case report. World Gastroenterology. 2009;15(November (43)):5493–5497. doi: 10.3748/wjg.15.5493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Buelow B., Otjen J., Sabath A.P., Harruff R.C. Peliosis hepatis presenting as liver rupture in a vulnerable adult: a case report. American Journal of Forensic Medicine and Pathology. 2011;(November) doi: 10.1097/PAF.0b013e31823a8b38. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21.Suzuki S., Suzuki, Mochida Y. Liver hemorrhage due to idiopathic peliosis hepatis successfully treated with hepatic artery embolization. International Surgery. 2011;96(October–December (4)):310–315. doi: 10.9738/cc43.1. [DOI] [PubMed] [Google Scholar]
- 22.Xiong W.J., Hu L.J., Jian Y.C., He Y., Zhou W., Guo X.L. Focal peliosis hepatis in a colon cancer patient resembling metastatic liver tumor. World Journal of Gastroenterology. 2012;18(November (41)):5999–6002. doi: 10.3748/wjg.v18.i41.5999. [DOI] [PMC free article] [PubMed] [Google Scholar]


