Abstract
OBJECTIVES
To test the effect of changes in Medicaid reimbursement on clinical outcomes of long-stay nursing home (NH) residents.
DESIGN
Longitudinal, retrospective study of NHs, merging aggregated resident-level quality measures with facility characteristics and state policy survey data.
SETTING
All free-standing NHs in urban counties with at least 20 long-stay residents per quarter (length of stay >90 days) in the continental United States between 1999 and 2005.
PARTICIPANTS
Long-stay NH residents
INTERVENTIONS
Annual state Medicaid average per diem reimbursement and the presence of case-mix reimbursement in each year.
MEASUREMENTS
Quarterly facility-aggregated, risk-adjusted quality-of-care measures surpassing a threshold for functional (activity of daily living) decline, physical restraint use, pressure ulcer incidence or worsening, and persistent pain.
RESULTS
All outcomes showed an improvement trend over the study period, particularly physical restraint use. Facility fixed-effect regressions revealed that a $10 increase in Medicaid payment increased the likelihood of a NH meeting quality thresholds by 9% for functional decline, 5% for pain control, and 2% for pressure ulcers but not reduced use of physical restraints. Facilities in states that increased Medicaid payment most showed the greatest improvement in outcomes. The introduction of case-mix reimbursement was unrelated to quality improvement.
CONCLUSION
Improvements in the clinical quality of NH care have been achieved, particularly where Medicaid payment has increased, generally from a lower baseline. Although this is a positive finding, challenges to implementing efficient reimbursement policies remain.
Keywords: nursing homes, Medicaid, outcomes, policy, evaluation
There is a long history of poor quality performance in U.S. nursing homes (NHs). Over the past several decades, numerous initiatives have been implemented in an attempt to address this problem. Since the Omnibus Budget Reconciliation Act of 1987, regulatory oversight has substantially increased and now includes certification and on-site inspection of all facilities, mandatory resident assessment, and public reporting of facility quality measures.1,2 In addition, the Centers for Medicare and Medicaid Services (CMS) has made major investments in quality improvement activities through its Quality Improvement Organizations (QIOs). Despite these efforts, recent scandals and government reports reveal that quality problems persist in many facilities.3–5
The Medicaid payment rate is the most important factor influencing the level of resources available to NHs. Medicaid, the dominant purchaser of NH services in the United States, gives financially indigent people access to NHs by directly reimbursing NHs for their care. State Medicaid programs provide approximately 50% of all NH reimbursements, and Medicaid recipients constitute 70% of all bed days. States have considerable discretion in setting Medicaid payment methods and rates.6
Several cross-sectional studies have revealed that Medicaid payment rates are associated with resident outcomes, but none have shown how changes in those rates might influence care.7,8 Several studies have shown that Medicaid NH payment increases are associated with higher staffing levels and more skilled staffing, although case-mix reimbursement appears to increase resident acuity and staffing.9 However, research has yet to demonstrate that increases in Medicaid payment rates to NHs are associated with improvements in resident outcomes. This is a particularly important question as growth in home and community-based long-term care services puts greater demands on state Medicaid budgets while acuity levels and the need for intensive nursing services of NH residents continues to rise.6,10,11
This study empirically tests the relationship between increases in Medicaid payment and selected measures of clinical quality in long-stay NH residents. State policy data for a 6-year period were combined with facility-level, aggregated, resident-level, risk-adjusted quality measures created from resident assessment data. The now well-documented improvements in various NH quality measures over the study period and facility factors were controlled for using fixed effects.12
METHODS
Study Design and Data
Changes in facility-level outcomes between 1999 and 2005 were examined. Data were obtained from three sources. State policy data came from a survey of state Medicaid offices conducted through the Center for Gerontology and Health Care Research at Brown University, described in greater detail elsewhere.6,10 Briefly, state Medicaid officials were asked to provide information on several NH reimbursement policies for 1998 through 2004. For each year, information was obtained on per diem Medicaid payments and whether the state had instituted case-mix reimbursement. Facility data were obtained from the On-line Survey Certification and Reporting (OSCAR) database maintained by CMS. OSCAR data consist of all items collected during the annual NH survey process, including those on ownership, structure, and staffing. A longitudinal OSCAR file has been constructed that tracks changes in ownership, staffing, and resident mix.13 Resident data are from the Minimum Data Set (MDS), a federally mandated resident assessment that includes measures of resident functioning, diagnoses, and demographics. Facility nurses complete the MDS upon admission and at least quarterly thereafter. Computerization of the MDS data is mandated, and all data are compiled in a national repository. The repository was made available through a Data Use Agreement with CMS (DUA 15293).
Sample
The sample consisted of all free-standing NHs in urban counties, as defined in the Area Resource File, in the continental U.S. states. Rural facilities were excluded because they operate under different market conditions and experience different hospitalization rates and because many states have special reimbursement arrangements for rural facilities.14 At each quarterly interval, the sample was restricted to facilities that had at least 20 long-stay residents in that interval. This restriction was applied to stabilize facility-level outcome measures and focus on long-stay residents because changes in Medicaid payment rates affect them most directly. Residents were considered long-stay if they had been in the NH for at least 90 days.8
Conceptual Framework for Assessing Effect of Medicaid Reimbursement
NHs in the United States operate in a complex regulatory and financial market and, regardless of ownership, must respond to policies changes and market forces to survive.15 The conceptual framework used in this study posits that NH operators respond to state and federal policy changes, taking into consideration the local market characteristics in which they operate. The strategic choices operators make to continue to function and meet minimal financial margins (necessary for for-profit and nonprofit facilities) affect the outcomes residents experience. The strategic choices operators make include reaching out to different patient populations (e.g., greater acuity), increasing or decreasing staffing levels or the skill mix of staff, and even the wages that staff are paid to attract more and better staff.9,13,16 Numerous specific policies contribute to the net Medicaid payment rates that individual NHs receive. Research has shown that several of these affect inputs such as staffing, case mix, and outcomes such as hospitalization.17–19 Thus, changes in policies apparently influence case mix and staffing inputs, which act as intermediaries that, in turn, should influence resident outcomes. All Medicaid NH reimbursement policies (e.g., case-mix reimbursement, wage mandates, and provider bed taxes) are ultimately components of the overall Medicaid reimbursement rate. In light of this, it was decided to test how changes in this most salient policy to NHs is related to changes in resident outcomes.
Measuring States’ Policies
States reported the average per diem Medicaid reimbursement rate for each year between 1998 and 2004. All payment rates were adjusted to 2004 dollars using the annual Consumer Price Index (CPI), and rates were set to $10 increments. States reported the presence of case-mix reimbursement policies in place for each year between 1999 and 2004 based on whether NH reimbursement rates were adjusted for resident acuity.10,17,20
Outcome Measures
There are numerous possible resident outcome measures; a parsimonious set was chosen that included processes and outcomes, cross-sectional and longitudinal, all of which have been repeatedly identified as historically salient and clinically important.12 MDS data were used to create four resident-level quality measures, three of which were longitudinal insofar as they depended on the resident’s prior assessment. Functional decline was defined as a change of at least 4 points on the MDS-embedded activity of daily living (ADL) 28-point scale over a 90-day period.21,22 This was restricted to residents who were at risk of declining at least this much by excluding the small number of residents each quarter already at the highest three levels of impairment (bed bound with limited bed mobility). A minimum of a 4-point decline was required to be included in the numerator because fewer than 10% of long-stay residents who decline that much revert to their baseline state in the following assessment, suggesting that the decline was likely permanent and not merely a measurement artefact. Pressure ulcer (PU) incidence was defined as reporting a PU for a resident who did not have one reported at baseline or reporting a more-advanced-stage PU than reported previously. Persistent pain was defined as the presence of daily pain, at any level, reported at two consecutive MDS assessments (90 days ±30).23 All longitudinal measures, whether measuring change or persistence, required at least 20 observations in the at risk group (denominator), or they were set to missing for that facility for that quarter. Consistent with recent research, the measures for ADL decline, PU incidence, and pain persistence were risk adjusted at the patient level before aggregation for diagnoses and cognitive impairment. The nursing case-mix index on which the Resource Utilization Groups (RUGs) was applied at the facility level was an adjustment of the aggregated measure.10,24,25 Finally, restraint use was defined as the use of any limb or trunk restraints or the use of chairs that prevent rising in the 7 days before assessment. It was decided not to apply any risk adjustment to physical restraint use because most experts agree that physical restraints can be avoided in many circumstances. The rationale for this decision is that many facilities are restraint free regardless of the characteristics of their patients.26 With the exception of restraint use, these aggregated measures are not those in use by CMS in the Nursing Home Compare web site (www.nursinghomecompare.gov).
To create facility-level outcome measures, an individual level regression model was run that adjusted for cognitive performance, RUG score, and selected diagnoses that generated a predicted probability of the outcome relative to the average U.S. NH resident. The proportion of residents in the NH who met the outcome condition (e.g., acquired a PU, had unresolved pain) was then calculated as if the home served the average resident of a U.S. facility. This was aggregated to the NH-level, resulting in a continuous distribution for each facility-quarter cell. To improve interpretability and to adjust for skewed distributions, each of the outcome measures was dichotomized, classifying NHs according to whether they met a given threshold indicative of high-quality care in each quarter. The published literature was consulted and empirical trends in the data examined to define these thresholds.22,23,27,28 The high-quality thresholds were defined as fewer than 5% of long-stay residents experienced ADL decline of 4 points or more, fewer than 2% presented with new or worsened PUs, fewer than 1% experienced persistent pain, and fewer than 1% were physically restrained. The continuous version of each outcome was retained, and both forms of the outcome variables were analyzed as a sensitivity analysis.
Control Variables
Because of the potential for endogeneity in testing the effect of a state policy, control variables were included selectively. As noted, the introduction of case-mix reimbursement and Medicaid payment rate have been associated with changes in staffing; as such, staffing and state policies are endogenous with respect to their effects on quality, so staffing measures were not controlled for.17 Several facility-level, annualized time-varying covariates were included: average admission nursing case-mix index (an indicator of acuity), percentage of long-stay residents who were African American, and number of admissions per bed as a surrogate for facility postacute population (calculated as the number of unique admissions from the MDS per bed as measured in the OSCAR). At the county-level, the average number of empty beds per NH, a measure of NH market competition that has been found to be more effective than the Herfindahl index in prior research, and the annual area wage index, to control for regional variation in the buying power of the Medicaid payment rate, were controlled for.15
Analytical Strategy
For each outcome measure, generalized estimating equation (GEE) methods were used to develop a model to estimate a NH’s probability of reaching each of the four high-quality thresholds in each quarter. In addition to the potential confounders described above, time trends and state effects were also controlled for by including a set of dummy variables representing quarterly time periods beyond the baseline of the first quarter in 1999 and facility dummy variables. Huber-White robust variance estimators were applied to adjust for within-facility clustering over time. State policies were lagged by 1 year to ensure that they were implemented before outcomes reporting. The same model was used for each outcome measure.
The analyses were replicated using a logged form of the continuous outcome variables using a facility fixed-effects model. Furthermore, various sensitivity analyses were performed to test the robustness of the findings. First, the models were tested on the 12 states with the lowest average annual CPI-adjusted Medicaid payment rate growth and the 12 states with the highest annual growth in the CPI-adjusted Medicaid rate. States with the lowest rate of CPI-adjusted Medicaid payment rate increases tended to have higher baseline Medicaid payment rates. Second, the models were stratified according to NH characteristics to determine whether the results differed across important facility descriptors, including profit status, chain membership, bed size, and presence of a dementia special care unit at baseline.
RESULTS
Nine thousand three hundred ninety-eight facilities were included in the analyses. Table 1 summarizes the structural, ownership, staffing, and resident acuity characteristics of study facilities in 1999 and 2005. The average bed size was 120, almost three-quarters of facilities were proprietary, and average occupancy rates were approximately 86%. The average number of total direct care staff hours per resident day was 3.2 in 1999 and rose slightly over the 6-year period. As shown in previous research, the average nursing case-mix index increased in acuity over the 6-year study period (0.98 to 1.03), as did the number of admissions per bed.
Table 1.
Characteristics of Free-Standing U.S. Urban Nursing Homes
| Characteristic | 1999 (n = 9,398) | 2005 (n = 9,320) |
|---|---|---|
| Number of beds, mean (IQR) | 120 ± 70.7 (73) | 121 ± 67.2 (68) |
| Occupancy rate, mean (IQR) | 86.1 ± 14.7 (14.2) | 87.0 ± 12.4 (12.9) |
| Total direct-care staffing hours per resident day, mean (IQR) | 3.2 ± 2.0 (0.9) | 3.3 ± 1.3 (0.9) |
| For-profit, % | 73.3 | 72.4 |
| Part of chain, % | 58.4 | 53.8 |
| Percentage Medicaid, mean (IQR) | 64.5 ± 24.7 (27.7) | 62.3 ± 22.5 (24.6) |
| Percentage Medicare, mean (IQR) | 9.3 ± 13.5 (8.4) | 14.2 ± 13.2 (11.1) |
| Percentage private pay, mean (IQR) | 26.2 ± 22.0 (24.0) | 23.5 ± 18.7 (19.5) |
| Nursing case-mix index (admission), mean (IQR) | 0.98 ± 0.12 (0.13) | 1.03 ± 0.11 (0.11) |
| Number of admissions per bed, mean (IQR) | 1.4 ± 2.2 (1.0) | 1.7 ± 1.9 (1.3) |
IQR = interquartile range.
From 1998 to 2004, the number of states reporting case-mix reimbursement policies increased from 26 to 35. During the same time, the average CPI-adjusted Medicaid rate increased from $109 ± 22 to $131 ± 25 in constant 2004 dollars. State-level minimum payments increased from $71 to $91 and maximum payments from $184 to $189.6
Figure 1 displays average percentage changes in states’ Medicaid NH payment rate relative to the 1999 baseline. It displays the same type of information for each of the four outcomes, all standardized to 100 at the baseline year of 1999 and presented as three-quarter moving averages to reduce seasonal fluctuations. At baseline in 1999, between 5% and 10% of NHs met the high-quality threshold for all outcomes except restraints; 17% of facilities were virtually restraint free at baseline. Real Medicaid payment rates increased approximately 25% over 6 years, and for all outcomes, except PU worsening, the percentage of NHs reaching the benchmark steadily increased over the 28 quarters. The greatest change occurred for physical restraint use and persistent pain (~75% improvement). The percentage of facilities achieving the 5% threshold for declining 4 ADL points or more increased almost 50% (in absolute terms from 5% to >8%). This means that the average facility 4-point ADL decline rate dropped from roughly 15% in early 1999 to 10% in late 2005. Improvement in the physical restraint rate was most dramatic, with the percentage of facilities that were virtually restraint free nearly doubling, from 15% to almost 30%.
Figure 1.
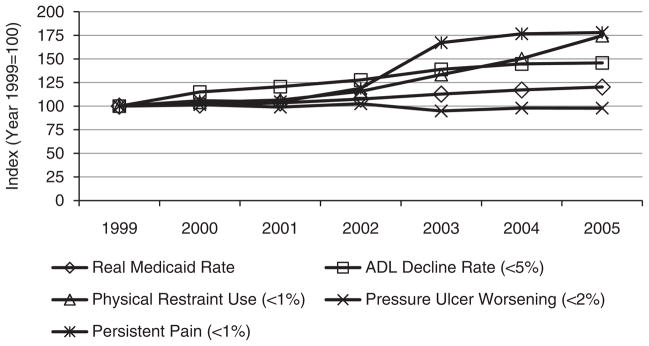
Average percentage change (Y-axis) in state Medicaid payment rate standardized to 1999 baseline levels contrasted with average percentage change in the proportion of U.S. nursing homes achieving indicated benchmark performance levels on four nursing home long-stay resident quality measures, 1999–2005 (X-axis).
Table 2 presents the results of the GEE analyses controlling for facility case mix (admissions per bed, case-mix index), changing racial composition, time, and the introduction of case-mix reimbursement. Results reveal that increases in Medicaid payment are positively associated with three of the four quality measures. For every $10 increase in Medicaid per diem reimbursement, the odds of a NH reaching the high-quality threshold increased 9.2% for ADL decline, 2.1% for PU incidence, and 5.5% for persistent pain. The odds of a NH reaching the quality threshold on restraint use decreased significantly (adjusted odds ratio = 0.96) with increases in Medicaid payment, this in the face of a substantial downward trend in restraint use. The introduction of case-mix reimbursement policies per se was not significantly associated with any of the four quality measures examined. Similar results were observed when a facility fixed-effects model was used on the logged form of the continuous outcomes (not shown).
Table 2.
Cross-Sectional Time Series Generalized Estimating Equation Logistic Regression Results: Effect of Changes in States’ Medicaid Payment Rate and Case Mix Reimbursement on the Likelihood of Nursing Homes Achieving a High-Quality Threshold on Four Long-Stay Resident Quality Thresholds: 1999–2005
| Medicaid Payment Rate and Case Mix Reimbursement | Activity of Daily Living Decline <5% | Restraint Use <1% | Pressure Ulcer Worsening <2% | Persistent Pain <1% |
|---|---|---|---|---|
| Consumer Price Index–adjusted Medicaid rate (by $10) | 1.092** | 0.961** | 1.021* | 1.055** |
| Case-mix reimbursement (1/0) | 0.943 | 0.898+ | 1.067 | 0.942 |
| Average number of empty beds in county | 0.999 | 1.002 | 0.997* | 0.998 |
| Area Wage Index (by 1 SD) | 1.082** | 1.124** | 0.971* | 1.004 |
| Number of admissions per bed | 0.767** | 1.073** | 0.771** | 0.919** |
| Average Nursing Case Mix Index on admission (by 1 SD) | 0.815** | 0.911** | 0.791** | 0.938** |
| % Blacks | 1.006** | 1.001 | 0.996** | 0.997** |
Robust standard errors adjusted for clustering with facility. Quarterly trend terms and facility dummy variables not shown.
The first quarter of 1999 was the reference.
Bold indicates P<.05.
P<**.01,*.05,+.10.
SD = standard deviation.
The sensitivity analyses revealed comparable effects for different subgroups of facilities. That is, the same patterns were observed for larger and smaller facilities, for for-profit and nonprofit facilities, and for facilities that were and were not part of chains. The effect of a $10 increase in Medicaid payment rate on the rate of ADL decline was stronger in states with the largest increase in payment (Figure 2). States with the lowest payment rates at baseline tended to include facilities that had the greatest rate of improvement. Nevertheless, restraint use reductions were greatest in states with the lowest rate of payment rate changes, suggesting that facilities in states with higher baseline levels of Medicaid payment continued to improve with regard to restraint use (Figure 3).
Figure 2.
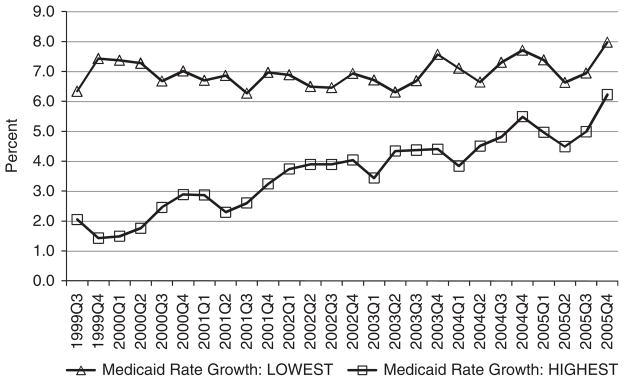
Percentage of nursing homes reaching the high-quality threshold on activity of daily living decline for long-stay residents: 1999–2005.
Figure 3.
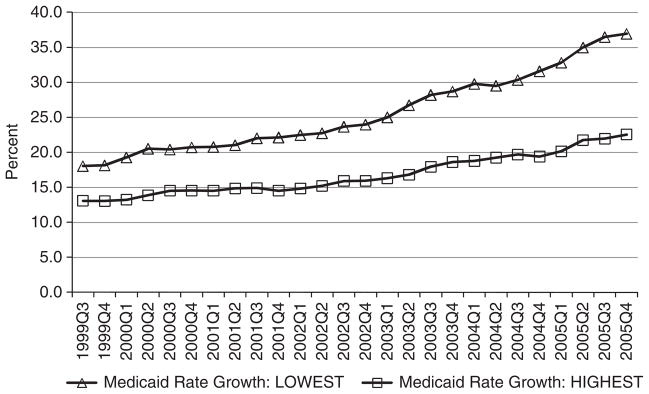
Percentage of nursing homes reaching the high-quality threshold on physical restraints for long-stay residents: 1999–2005.
DISCUSSION
This study found that a $10 a day increase in Medicaid reimbursement rates was associated with significant reductions in rates of ADL decline and persistent pain in long-stay NH residents but had a weaker effect on reducing the incidence of PUs. In the face of a strong secular trend in falling physical restraint use, facilities in states that increased Medicaid payment rates most did not reduce restraint rates as much as did facilities in states with lower rates of Medicaid payment increase, perhaps because these states had much higher payment rates at baseline, particularly because the absolute restraint use rates declined substantially across all types of facilities and states. On the whole, this is good news. Medicaid payment rates have been rising, and this study suggests that these increases have resulted in benefits for the long-stay NH population.6
The identification of a clear association between increases in Medicaid payment and important quality measures has timely policy implications. State Medicaid programs are facing pressures to reconsider the dollars allocated to NH care. Recent state budget shortfalls have provided state policymakers with the impetus to revisit overall Medicaid spending.29 States look to NH care as a potential area to cut spending.30 Indeed, recent evidence reveals a relatively stable Medicaid NH population between 1999 and 2007 but one that consumed 15% more in spending.31 This pattern is consistent with increasing case-mix acuity of NH residents that has been associated with the introduction of Medicaid case-mix reimbursement.10 Given rising acuity, the findings of the current study suggest that Medicaid payment rates may need to continue to increase if quality of care is not to suffer.
State Medicaid programs are also trying to invest in home- and community-based settings, but decisions concerning long-term care expenditures often take place within a zero-sum framework, with increases in spending in home-and community-based settings presumably corresponding to decreases in NH spending.32 Although experience suggests that institutional and community-based spending tends to increase, the primary finding—that an increase in Medicaid payments to NHs is related to the quality of NH care—must be considered in light of the demands to transfer funds to NH alternatives.31 As legislative efforts to direct scarce state resources into home and community-based programs are pursued, the frailest and neediest recipients of long-term care (individuals for whom NH residence may not be reversible) face greater risk of receiving poor-quality care in settings where Medicaid payments are inadequate.
Although it is encouraging that by greater resource investment appears to translate into positive resident outcomes, more-efficient strategies for further improvement are needed, but with approximately 1 million Medicaid residents on any given day, that nominal amount quickly adds up to a high cost—roughly an extra $3.65 billion per year. The real, but modest, improvements associated with higher Medicaid spending observed here suggest that it is necessary to better understand how best to target the added resources. Because most nursing facilities care for a combination of long-stay Medicaid patients and postacute patients for whom Medicare more highly reimburses, it is increasingly important to understand the mechanisms by which these differing revenue sources are used to subsidize care for Medicaid patients or not. Because Medicare’s share of NH patients and spending has been increasing dramatically, it is increasingly important to understand whether there are spillover effects with respect to quality.31
Policies that can focus additional resources on specific areas, such as staffing, technology, and management, may achieve comparable benefits more efficiently. One policy being tested in many states is to mandate that payment increases be devoted to increases in staffing—for higher wages or more staff. Based on prior research, there is reasonably good evidence that increases in Medicaid payment tend, on average, to translate into higher staffing levels; recent evidence suggests that payment increases targeted to staffing yield increases in the number of direct care staff in a facility but still unknown is the extent to which these policies reduce turnover.17 Further improvements in NH quality, in conjunction with concurrent diversification of long-term care spending into community services, will be contingent on the implementation of efficiently targeted policies. This is worth further investigation with well-designed demonstration projects.
The challenge of improving NH quality while expanding state-funded home- and community-based services will be considerable. Policies introduced in the Deficit Reduction Act that aim to discharge or deflect admission of Medicaid-supported residents whose care needs are minimal would reduce total Medicaid payments to NHs. There are indications that between 5% and 13% of all long-stay residents do not require NH level of care.33 Because most of these individuals are Medicaid recipients, even with increases in payment rates, total Medicaid NH payments could decline, or at least remain stable. Nonetheless, consistent with the results of the current study, as such “low care” cases are discharged or deflected, resident acuity rises, and with it the plea for increasing average daily payment levels, particularly in states with case-mix reimbursement.
This study has limitations that should be considered. First, quality indicators that focus on clinical care were chosen, and other important domains such as quality of life and resident satisfaction were not examined.34 In addition, the analysis was limited to broadly applicable quality measures, and those that may be pertinent to particular subgroups such as those who are dying or have severe cognitive impairments were not considered. Nonetheless, the process and outcome measures that were chosen are nursing sensitive and highly relevant to the long-stay population. Second, MDS data, which have documented measurement limitations, were relied on, especially for items such as pain intensity,23,35 although the facility fixed-effects design minimizes systematic measurement biases that may exist because of interfacility variation in assessment practices. Third, state average Medicaid payment was used rather than facility-specific measures for payment. Numerous policies affecting reimbursement were instituted over the study period, but only the annual Medicaid NH payment rate and the introduction of case-mix reimbursement were assessed. Some state policies, such as the provider tax, resulted in making more money available for MA payments for NHs because taxes on private pay and Medicare bed days effectively subsidize MA payments because these added funds are “re-cycled” through general revenue and made available for increases in MA payments.36 The way MA payments were defined at the state level effectively includes all manner of specific policies designed to increase reimbursement because the “gross,” inflation adjusted amount was used regardless of which types of policies made more funds available. Furthermore, because a panel study was used, the effects of increases in MA payments on the average quality change were estimated. Although less precise in terms of understanding how individual facilities responded to increased payment, this approach improves the ability to test the effect of policies because they are exogenous to the outcomes of interest. The actual variations in state Medicaid NH reimbursement levels even within a state are substantial, meaning that even states using case-mix reimbursement formulae do not pay the same rates to facilities with the same case mix.37 Although some may argue that the complex interplay of various changing state policy interventions needs to be better understood, the finding that the greatest improvements in outcomes were experienced in states that increased payment rates most lends credence to the interpretation, particularly because quality improvements, albeit less substantial, were also found in states with higher absolute payment rates at baseline.
It was decided to evaluate changes in quality by examining whether facilities were able to meet what was considered to be a relatively high-quality threshold in any given quarter and not whether facilities were able to maintain that level of quality over time. NH-level quality indicators exhibit substantial volatility over time, so further investigation into the influence of increased funding on sustained improvement is warranted. This study provides useful baseline information that can inform policy regarding community placement and pay-for-performance strategies.
Summary and Policy Implications
Overall, greater state spending on NH services was associated with measurable increases in quality. There are still many poorly performing facilities and substantial volatility in outcomes over time, which suggests that management and work-force problems need to be specifically addressed. Nonetheless, higher Medicaid payment rates appear to be associated with improvement in the quality of NH care. All things considered, this is good news, but it presents an array of policy challenges for further sustainable improvement.
Acknowledgments
This study was funded in part by National Institute on Aging (NIA) Grant RO-1 AG20557 to Brown University, Vincent Mor, Principal Investigator and by NIA Grant KO-1 AG24403 to Harvard University, David Grabowski, Principal Investigator.
Sponsor’s Role: None.
Footnotes
Author Contributions: All the authors took significant part in the concept, design, methods, data analysis, and the writing of this paper.
Conflict of Interest: Vincent Mor is a founder and on the board of directors of PointRight, Inc., an information services company serving NHs on quality measurement and improvement. Dr. Mor receives no research funding, data, or consultation on his research from PointRight.
References
- 1.Hawes C, Mor V, Phillips CD, et al. The OBRA-87 nursing home regulations and implementation of the Resident Assessment Instrument: Effects on process quality. J Am Geriatr Soc. 1997;45:977–985. doi: 10.1111/j.1532-5415.1997.tb02970.x. [DOI] [PubMed] [Google Scholar]
- 2.Mor V. Improving the quality of long-term care with better information. Milbank Q. 2005;83:333–364. doi: 10.1111/j.1468-0009.2005.00405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kitchener M, O’Meara J, Brody A, et al. Shareholder value and the performance of a large nursing home chain. Health Serv Res. 2008;43:1062–1084. doi: 10.1111/j.1475-6773.2007.00818.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stevenson DG, Studdert DM. The rise of nursing home litigation: Findings from a national survey of attorneys. Health Aff (Millwood) 2003;22:219–229. doi: 10.1377/hlthaff.22.2.219. [DOI] [PubMed] [Google Scholar]
- 5.Winzelberg GS. The quest for nursing home quality: Learning history’s lessons. Arch Intern Med. 2003;163:2552–2556. doi: 10.1001/archinte.163.21.2552. [DOI] [PubMed] [Google Scholar]
- 6.Grabowski DC, Feng Z, Intrator O, et al. Medicaid nursing home payment and the role of provider taxes. Med Care Res Rev. 2008;65:514–527. doi: 10.1177/1077558708315968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grabowski DC, Angelelli JJ, Mor V. Medicaid payment and risk-adjusted nursing home quality measures. Health Aff (Millwood) 2004;23:243–252. doi: 10.1377/hlthaff.23.5.243. [DOI] [PubMed] [Google Scholar]
- 8.Intrator O, Grabowski DC, Zinn J, et al. Hospitalization of nursing home residents: The effects of states’ Medicaid payment and bed-hold policies. Health Serv Res. 2007;42:1651–1671. doi: 10.1111/j.1475-6773.2006.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zinn J, Feng Z, Mor V, et al. Restructuring in response to case mix reimbursement in nursing homes: A contingency approach. Health Care Manage Rev. 2008;33:113–123. doi: 10.1097/01.HMR.0000304506.12556.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feng Z, Grabowski DC, Intrator O, et al. The effect of state Medicaid case-mix payment on nursing home resident acuity. Health Serv Res. 2006;41:1317–1336. doi: 10.1111/j.1475-6773.2006.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grabowski DC. The cost-effectiveness of noninstitutional long-term care services: Review and synthesis of the most recent evidence. Med Care Res Rev. 2006;63:3–28. doi: 10.1177/1077558705283120. [DOI] [PubMed] [Google Scholar]
- 12.Werner RM, Konetzka RT, Kruse GB. Impact of public reporting on unreported quality of care. Health Serv Res. 2009;44:379–398. doi: 10.1111/j.1475-6773.2008.00915.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zinn JS, Mor V, Feng Z, et al. Doing better to do good: The impact of strategic adaptation on nursing home performance. Health Serv Res. 2007;42:1200–1218. doi: 10.1111/j.1475-6773.2006.00649.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gruneir A, Miller SC, Intrator O, et al. Hospitalization of nursing home residents with cognitive impairments: The influence of organizational features and state policies. Gerontologist. 2007;47:447–456. doi: 10.1093/geront/47.4.447. [DOI] [PubMed] [Google Scholar]
- 15.Zinn J, Mor V, Feng Z, et al. Determinants of performance failure in the nursing home industry. Soc Sci Med. 2009;68:933–940. doi: 10.1016/j.socscimed.2008.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gruneir A, Lapane KL, Miller SC, et al. Long-term care market competition and nursing home dementia special care units. Med Care. 2007;45:739–745. doi: 10.1097/MLR.0b013e3180616c7e. [DOI] [PubMed] [Google Scholar]
- 17.Feng Z, Grabowski DC, Intrator O, et al. Medicaid payment rates, case-mix reimbursement, and nursing home staffing-1996–2004. Med Care. 2008;46:33–40. doi: 10.1097/MLR.0b013e3181484197. [DOI] [PubMed] [Google Scholar]
- 18.Feng Z, Lee YS, Kuo S, et al. Do Medicaid wage pass-through payments increase nursing home staffing? Health Serv Res. 2010;45:728–747. doi: 10.1111/j.1475-6773.2010.01109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grabowski DC, Feng Z, Intrator O, et al. Medicaid bed-hold policy and Medicare skilled nursing facility rehospitalizations. Health Serv Res. 2010 Apr 6; doi: 10.1111/j.1475-6773.2010.01104.x. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grabowski DC, Feng Z, Intrator O, et al. Recent trends in state nursing home payment policies. Health Aff (Millwood) 2004;(Suppl Web Exclusives):W4, 363–373. doi: 10.1377/hlthaff.w4.363. [DOI] [PubMed] [Google Scholar]
- 21.Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci. 1999;54:M546–M553. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- 22.Carpenter GI, Hastie CL, Morris JN, et al. Measuring change in activities of daily living in nursing home residents with moderate to severe cognitive impairment. BMC Geriatr. 2006;6:7. doi: 10.1186/1471-2318-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu N, Miller SC, Lapane K, et al. The quality of the quality indicator of pain derived from the minimum data set. Health Serv Res. 2005;40:1197–1216. doi: 10.1111/j.1475-6773.2005.00400.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fries BE, Schneider DP, Foley WJ, et al. Refining a case-mix measure for nursing homes: Resource Utilization Groups (RUG-III) Med Care. 1994;32:668–685. doi: 10.1097/00005650-199407000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Mukamel DB, Glance LG, Li Y, et al. Does risk adjustment of the CMS quality measures for nursing homes matter? Med Care. 2008;46:532–541. doi: 10.1097/MLR.0b013e31816099c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mor V. Persistent restraints: A performance marker and a call for action. Med Care. 2002;40:851–852. doi: 10.1097/00005650-200210000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Ooi WL, Morris JN, Brandeis GH, et al. Nursing home characteristics and the development of pressure sores and disruptive behaviour. Age Ageing. 1999;28:45–52. doi: 10.1093/ageing/28.1.45. [DOI] [PubMed] [Google Scholar]
- 28.Wu N, Miller SC, Lapane K, et al. Impact of cognitive function on assessments of nursing home residents’ pain. Med Care. 2005;43:934–939. doi: 10.1097/01.mlr.0000173595.66356.12. [DOI] [PubMed] [Google Scholar]
- 29.NASBO NAoSBO. The Fiscal Survey of States. Washington, DC: National Association of State Budget Officers; 2008. [Google Scholar]
- 30.State Budgets under Stress: How Are States Planning to Reduce the Growth in Medicaid Costs? Washington, DC: Kaiser Family Fund; 2003. [Google Scholar]
- 31.Ng T, Harrington C, Kitchener M. Medicare and Medicaid in long-term care. Health Aff (Millwood) 2010;29:22–28. doi: 10.1377/hlthaff.2009.0494. [DOI] [PubMed] [Google Scholar]
- 32.Kane RA. Expanding the home care concept: Blurring distinctions among home care, institutional care, and other long-term-care services. Milbank Q. 1995;73:161–186. [PubMed] [Google Scholar]
- 33.Mor V, Zinn J, Gozalo P, et al. Prospects for transferring nursing home residents to the community. Health Aff (Millwood) 2007;26:1762–1771. doi: 10.1377/hlthaff.26.6.1762. [DOI] [PubMed] [Google Scholar]
- 34.Kane RL, Bershadsky B, Kane RA, et al. Using resident reports of quality of life to distinguish among nursing homes. Gerontologist. 2004;44:624–632. doi: 10.1093/geront/44.5.624. [DOI] [PubMed] [Google Scholar]
- 35.Cadogan MP, Schnelle JF, Yamamoto-Mitani N, et al. A minimum data set prevalence of pain quality indicator: Is it accurate and does it reflect differences in care processes? J Gerontol A Biol Sci Med Sci. 2004;59A:281–285. doi: 10.1093/gerona/59.3.m281. [DOI] [PubMed] [Google Scholar]
- 36.Grabowski DC, Zhanlian F, Mor V. Medicaid nursing home payment and the role of provider taxes. Med Care Res Rev. 2008;65:514–527. doi: 10.1177/1077558708315968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miller EA, Mor V, Grabowski DC, et al. The devil’s in the details: Trading policy goals for complexity in Medicaid nursing home reimbursement. J Health Polit Policy Law. 2009;34:93–135. doi: 10.1215/03616878-2008-993. [DOI] [PubMed] [Google Scholar]


