Abstract
Introduction
Coping skills training interventions have been found to be efficacious in helping both patients and their partners manage the physical and emotional challenges they face following a cancer diagnosis. However, many of these interventions are costly and not sustainable. To overcome these issues, a self-directed format is increasingly used. The efficacy of self-directed interventions for patients has been supported; however, no study has reported on the outcomes for their partners. This study will test the efficacy of Coping-Together—a multimedia, self-directed, coping skills training intervention for patients with cancer and their partners.
Methods and analysis
The proposed three-group, parallel, randomised controlled trial will recruit patients diagnosed in the past 4 months with breast, prostate, colorectal cancer or melanoma through their treating clinician. Patients and their partners will be randomised to (1) a minimal ethical care (MEC) condition—selected Cancer Council New South Wales booklets and a brochure for the Cancer Council Helpline, (2) Coping-Together generic—MEC materials, the six Coping-Together booklets and DVD, the Cancer Council Queensland relaxation audio CD and login to the Coping-Together website or (3) Coping-Together tailored—MEC materials, the Coping-Together DVD, the login to the website and only those Coping-Together booklet sections that pertain to their direct concerns. Anxiety (primary outcome), distress, depression, dyadic adjustment, quality of life, illness or caregiving appraisal, self-efficacy and dyadic and individual coping will be assessed before receiving the study material (ie, baseline) and again at 3, 6 and 12 months postbaseline. Intention-to-treat and per protocol analysis will be conducted.
Ethics and dissemination
This study has been approved by the relevant local area health and University ethics committees. Study findings will be disseminated not only through peer-reviewed publications and conference presentations but also through educational outreach visits, publication of lay research summaries in consumer newsletters and publications targeting clinicians.
Trial registration
Australian New Zealand Clinical Trials Registry ACTRN12613000491763 (03/05/2013)
Keywords: Mental health, Public health, Statistics & Research Methods
Article summary.
Article focus
Coping skills training interventions to promote patients’ illness adjustment following a cancer diagnosis have been trialled, but equivalent research efforts to identify effective support for their partners are scarce, despite partners reporting as much if not more distress than patients.
This study will examine the efficacy and cost-efficacy of a novel, evidence-based, multimedia, self-directed coping skills training intervention to empower patients and partners to manage the physical and psychosocial challenges posed by a cancer diagnosis.
To the best of our knowledge, Coping-Together is the first intervention of its kind for couples adjusting to a recent cancer diagnosis.
Key messages
Coping-Together is an innovative coping skills training intervention that targets patients as well as their partners, and translates current, evidence-based strategies for effective illness self-management and coping into a readily accessible format that couples can use where and when they need to.
Over a 12-month period, this trial will directly examine the efficacy of Coping-Together in not only reducing negative psychological outcomes but also on a range of outcomes known to impact patients’ and partners’ cancer experience (eg, self-efficacy and dyadic coping).
The self-directed format of this intervention has the potential to address issues of access to psychosocial support, especially for couples in non-metropolitan areas. In addition, the self-directed nature of Coping-Together means that it has the potential to be cost-effective and be integrated into practice without increasing pressures on the oncology workforce.
Strengths and limitations of this study
Strengths include the projected sample size, recruitment from multiple sites across states and the use of a longitudinal design. Also, Coping-Together covers a broad range of cancer-related challenges identified to be common unmet needs of couples facing cancer. The cost-efficacy of the intervention will be directly assessed in this trial, an important consideration as economic evaluation is an often overlooked element of intervention research.
Challenges include recruitment and retention of the target population (which is vulnerable and facing the acute stress of a cancer diagnosis), and the longitudinal nature of the design potentially increases the likelihood of attrition.
Although substantial progress in the early detection and treatment of cancer means that the 5-year relative survival is now 66% for all cancers combined,1 a cancer diagnosis is still appraised as a life-threatening illness and elicits greater distress than any other medical diagnosis.2 From the time of diagnosis and throughout treatment, patients and their partners contend with a wide range of complex physical (eg, treatment side effects), psychosocial (eg, fear, uncertainty, anxiety) and healthcare challenges.3–9 The complexity of the situation is further heightened, as patients and partners contend with any number of these challenges at the same time that they are also trying to remain afloat with other life priorities.6
The difficulties experienced in managing cancer challenges are such that approximately one third of the patients experience high levels of physical or psychological distress,2 6 10 11 with some studies reporting comparable, if not higher, burden and distress among their partners.12–14 This might, in part, be attributed to partners’ tendency to subjugate their own needs for those of the patient and to protect patients from additional distress, often at the expense of their own emotional well-being. Although it is generally assumed that elevated anxiety and depression are confined to the acute postdiagnosis phase, a few studies have found that patients and partners experience chronic distress well into survivorship.15 16 This is concerning as high distress has been associated with lower treatment adherence,17 18 lower quality of life,11 19 20 higher incidence of cancer-related symptoms and side effects,21 higher health-risk behaviours17 and reduced-workplace productivity.22
Given the substantial burden of cancer, considerable research has focused on the impact of patients’ and partners’ coping with cancer challenges on their health and well-being.14 23 In their seminal book on stress and coping, Lazarus and Folkman24 defined coping as “cognitive and behavioural efforts to manage the demands of a situation or condition that is appraised as taxing or exceeding the resources of the person.” Coping is typically characterised either as problem-focused coping (alter the stressful situation using strategies such as information-seeking, planning and problem solving) or emotion-focused coping (regulate situation-related emotions using strategies such as positive reappraisal and behavioural disengagement) and further considered for their adaptive versus maladaptive nature. The assumption is that if individuals use adaptive coping and are able to regain a sense of control over cancer challenges and negative emotions, they are then less likely to experience distress.25 In this sense, coping is not only a valuable explanatory concept regarding variability in response to stress, it can also serve as a portal for intervention, that is, if adaptive coping skills are not known, they can then be learnt.23 26 Despite conflicting results, most studies support the notion that increasing patient engagement with the stressor, through both problem-focused and emotion-focused coping, is generally associated with more positive adjustment than when less functional coping responses are used (eg, avoidance and denial).13 25 26 A number of studies have also corroborated these findings among partners of individuals with cancer.14 27
Beyond individual approaches to coping, recent studies have further considered how patients and partners interact as they attempt to cope together with cancer-related stressors and challenges (termed dyadic coping).13 28 29 The evidence on the impact of different dyadic coping strategies mirrors to a certain extent that of individual coping, whereby adjustment is greater when patients and partners respond to each other's stress, view cancer challenges as a shared problem and engage in joint problem solving that involves the pooling of resources.28 29 Berg et al28 found that the relationship between collaborative coping and illness adjustment for men diagnosed with prostate cancer and their wives was partially moderated by heightened perceptions of coping effectiveness. Conversely, when patients and/or partners use avoidant coping,13 30 control30 or protective buffering31 illness adjustment was compromised.
On the basis of the aforementioned evidence on individual and dyadic coping, considerable research efforts have focused on the development of coping skills training interventions to maximise the use of adaptive coping by patients and partners and so decrease physical and psychological distress in response to cancer challenges.2 32 Coping skills fostered by these interventions typically include problem solving, symptom management, communication (with family/friends or healthcare professionals) and stress management. A number of reviews and meta-analyses have supported the efficacy of such multicomponent coping skills training interventions in decreasing patient and partner anxiety and increasing quality of life, particularly if these are based on principles of cognitive behaviour therapy.26 33 Traditionally, these interventions have mainly focused on how patients cope with cancer-related challenges; however, with the increased recognition of the substantial burden of cancer on partners and the reciprocal relationship between partner's reactions to the cancer diagnosis,12 coping skills training interventions are increasingly targeting both patients and partners as a unit.34 Recent reviews have suggested that, in some contexts, couple-based interventions might be more efficacious in achieving optimal patient and partner adjustment than individual-based interventions.34–36 This might in part be attributed to the shared learning that occurs in couple-based coping skills training interventions.34
Although couple-based coping skills interventions seem promising for patients and/or their partners, issues pertaining to their accessibility and delivery linger.32 Most coping interventions are labour intensive, requiring access to highly trained healthcare professionals, limiting their long-term sustainability due to high costs and problems with accessibility in rural and regional areas. Furthermore, there is evidence to suggest that conventional interventions may not be accessed by patients, due to personal preference, geographical barriers and mobility issues.32 37 38 One study found the uptake rate of referrals to psychosocial services by distressed patients to be as low as 14%.39 This suggests that service providers need to consider alternate approaches to ensure that the coping interventions for couples are not only efficacious and cost-effective but also accessible and sustainable. Using a group format instead of an individual format has been proposed to address cost issues.40 However, research has been equivocal regarding the suitability of these interventions in comparison to individual ones.40 41 In addition, failure to create and sustain a functioning group is a challenge with some patient populations, which in turn might compromise the efficacy of the intervention.40 To overcome some of the challenges, while maintaining cost-effectiveness, the use of a self-directed approach has been proposed.42
Self-directed (also termed self-help or self-administered) interventions address some of the issues surrounding access to face-to-face interventions and provide couples with greater flexibility regarding when and how they engage with the intervention content. There is a growing body of evidence to suggest that self-directed coping skills training interventions are cost-effective and acceptable to patients.42–45 Furthermore, research supports the efficacy of self-directed interventions for enhancing patient well-being,42–45 especially for patients reporting elevated levels of distress44 or high uncertainty.43 Regrettably, all self-directed interventions reviewed to date are mainly developed to directly address patients’ concern, neglecting those of the partners. To address this gap in the literature our team has recently developed Coping-Together,46–48 a self-directed coping skills training intervention for couples affected by cancer. This study will examine both the efficacy and cost-efficacy of this intervention.
Coping-Together intervention
Coping-Together is an evidence-based, multimedia, self-directed coping skills training intervention to provide couples with the resources they need to confront the challenges posed by the cancer diagnosis and enhance their ability to cope with these.46–48 Coping-Together takes a holistic approach to coping with cancer by addressing a range of common physical, social and psychological challenges. The Medical Research Council framework for developing and evaluating complex interventions49 was used to guide the development and evaluation of Coping-Together.
Theoretical underpinnings
Coping-Together builds on three main theoretical frameworks:
Lazarus and Folkman's Stress and Coping framework,50 which assumes that if individuals are able to cope and regain a sense of control over cancer challenges, they are then less likely to experience distress.
Bodenmann's51 framework of dyadic coping extends Lazarus and Folkman's framework by acknowledging the reciprocal nature of stress and coping within couples and has become increasingly popular in the cancer literature.52
Bandura's53 self-efficacy theory, which posits that people are likely to engage in activities to the extent that they perceive themselves to be competent at those activities. Individuals are postulated to achieve self-efficacy through various means, including performing a task successfully, witnessing other people successfully completing a task, being persuaded that one has the skills to succeed and managing psychological responses that can adversely impact on how a person feels about their abilities in a particular situation.54
A detailed description of how each of these frameworks has guided the development of Coping-Together has been published elsewhere.48
Content
Coping-Together encourages patients and their partners to try new skills and strategies demonstrated to be effective in helping couples: (1) manage symptoms and side effects, (2) forge a strong relationship with the healthcare team, (3) cope with treatment decision-making, (4) locate additional support, (5) communicate about cancer and (6) manage worries and emotions. These challenges were selected based on an initial perusal of the literature and content of existing couple-based interventions. Coping-Together collates the evidence on coping with these challenges and presents these as ‘suggestions’ to patients and partners across six booklets, a DVD, a relaxation CD, and a website.
For each key cancer challenge addressed by this intervention, the booklets focus on providing the following type of information: (1) social comparison information (testimonial and quotes from other patients and partners), (2) evidence-based, concrete ‘suggestions’ to manage the challenges, (3) comments about the effectiveness of these strategies from others diagnosed with cancer and (4) empirical evidence supporting the coping ‘suggestion’. In addition, the booklets include several cognitive-behavioural therapy-based exercises, adapted from other self-directed coping skills interventions with patients37 55 or developed by experienced clinicians and designed to encourage active learning. Table 1 summarises the content of each booklet. To ensure the accuracy of the information, the booklets were reviewed by experts in the field, including clinicians and researchers and the experts’ endorsement is included throughout each booklet.
Table 1.
Coping-Together booklet content
| Booklet title | Description | Example Challenges | Example coping strategies |
|---|---|---|---|
| Getting What You Need From Your Health Care Team | Working with your medical team, knowing how to ask the right questions, getting and understanding the information you need | We don't know what questions to ask We leave our appointments feeling we didn't get what we wanted |
Use question checklists Prepare for appointments, communicate assertively and use other methods of communication |
| Making Your Treatment Decision | Considering your options, treatment planning and adjusting to treatment-related delays | We feel overwhelmed by options We want more of a say in the decision |
Identify what is most important to you, talk to your healthcare team and use decision aids Use assertive communication and consider a second opinion |
| Getting on Top of Symptoms | Coping with common treatment side effects | Fatigue Pain |
Use a symptom diary, talk to your healthcare team and use self-care strategies |
| Dealing with Stress and Worry | Addressing the emotional reactions to diagnosis and treatment | I feel sad, down and/or isolated I'm having difficulties sleeping |
Do pleasant activities and connect with others Practice good sleep hygiene throughout the day |
| Supporting Each Other | Enhancing your communication and connection to your partner, and adjusting to changes that may arise in your relationship | I just don't know how to make my partner feel better I'm stressed by changes in my roles and responsibilities |
Use listening skills, body language and empathy, avoid roadblocks to listening well Negotiate changes in roles and responsibilities and accept offers of help from others |
| Getting the Support You Need | Finding appropriate support to address practical, emotional, financial, legal and informational needs | We need more information We need legal help |
Identify your information needs, identify the right source of information, check the information credibility and manage information overload Identify the legal issues you need addressed and find a service that is right for you |
The Coping-Together DVD features a clinician who delivers key content of the booklets and includes scenarios with couples (actors) to demonstrate specific coping skills. The Cancer Council Queensland relaxation CD is included to supplement the Dealing with Stress and Worry booklet. Lastly, the Coping-Together website contains the booklets and DVD content, complemented with interactive features such as a question checklist generator, and tips for addressing common negative thoughts. The website also contains an announcements page for communication postings by the research team, contacts page for participants to communicate with the research team and links to a variety of credible information and support websites.
Feasibility testing of the Coping-Together booklets
A recent acceptability study of the Coping-Together booklets supported its self-directed format and its practical approach. Patients and partners identified a number of benefits to using these booklets, including increased awareness of challenges to prepare for, facilitated independent coping, increased hope that something can help you ‘pull through’, provided a sense of normality, connected patients and partners to people and services and complemented support received from healthcare professionals.46 47 56 Many couples rated the booklets highly and the concrete coping strategies described was a feature that set Coping-Together apart from other resources. Participants also made particular comments on the appropriateness of the resource focusing on the couple, rather than on the individual.
Study aims and hypotheses
The primary aim of this study will be to assess the efficacy of Coping-Together, in comparison to a minimal ethical care (MEC) condition, in decreasing anxiety in patients diagnosed with breast, prostate or colorectal (bowel) cancer or melanoma and their partners at 3, 6 and 12 months postbaseline.
The secondary aims will be to assess (1) the efficacy of Coping-Together in comparison to the MEC condition in decreasing distress and depression, and increasing positive-illness appraisal or caregiving appraisal, self-efficacy, quality of life, relationship satisfaction and positive individual and dyadic coping at 3, 6 and 12 months postbaseline; (2) the efficacy of generic Coping-Together in comparison to a tailored version of Coping-Together in enhancing primary and secondary outcomes over time and (3) cost-efficacy of Coping-Together in comparison to the MEC condition.
The tertiary aim will be to explore moderators of outcomes, including distress, social support, self-efficacy, information needs and preferences and relevance and use of the material sent to address challenges experienced.
Hypotheses
Primary hypothesis: Significantly fewer Coping-Together participants will experience anxiety at 3, 6 and 12 months postbaseline than MEC participants.
Secondary hypotheses: (1) From the health and broader societal perspective, Coping-Together (generic or tailored) will be more cost-efficacious than the MEC condition and (2) Coping-Together participants will experience significantly less distress and depression and more positive illness or caregiving appraisal, self-efficacy, quality of life, relationship satisfaction and positive individual and dyadic coping at 3,6 and 12 months postbaseline than MEC participants.
Tertiary hypotheses: (1) Couples in the tailored Coping-Together condition will report greater use of the resource and higher illness adjustment across primary and secondary outcomes than couples in the generic Coping-Together condition and (2) the significant changes over time in anxiety among groups will be moderated by distress, social support, self-efficacy, information needs and preferences, resource use and perceived relevance of the material sent to address the challenges experienced.
Methods/design
Design
The proposed study is a multicentre, stratified, double-blind, three-group, parallel, randomised controlled trial to compare generic Coping-Together, tailored Coping-Together and the MEC condition (see figure 1). The CONSORT statement57 guided the design of this study.
Figure 1.
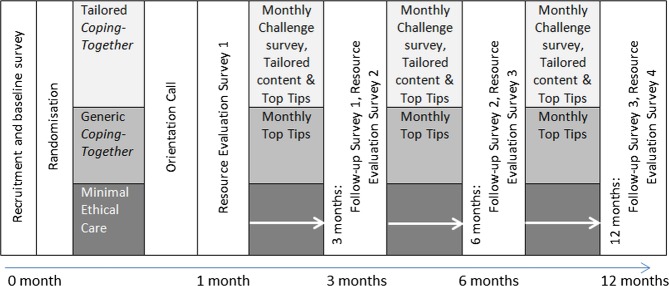
Study design and groups.
Sample and setting
Patients will be recruited from participating private and public outpatient, multidisciplinary oncology clinics in Australia (Australian Capital Territory, New South Wales, South Australia, Western Australia and Queensland). These clinics typically exist within large, general metropolitan or rural hospitals. Inclusion criteria are (1) a patient recently diagnosed (within 4 months) with a primary, early-stage breast, prostate or colorectal (bowel) cancer or melanoma and receiving or planning to receive cancer treatment with curative intent, (2) has a partner (spouse, boy/girlfriend or de facto) who is also willing to participate in the study, (3) the patient or their partner scores ≥4 on the Distress Thermometer (DT) and (4) the patient and partner are sufficiently fluent in English and cognitively able to read study materials and complete surveys. The patient's and the partner's consents are required for the couple to participate in this trial. These inclusion criteria were selected to reflect current recommendations for intervention studies in psycho-oncology, including targeting couples with elevated levels of distress to avoid the potential for floor effect.58
Sample size
Assuming that the SD of patients’ and partners’ scores on the Hospital Anxiety and Depression Scale-Anxiety subscale (HADS-A) is 414 39 and the correlation of baseline and follow-up measurement is approximately 0.5, 133 couples per group will be sufficient to have 90% power to detect the minimal clinically significant difference of 1.5 on the HADS-A,59 at the 2.5% significance level. This corresponds to over 80% power to detect a difference in the level of anxiety between treatment groups at follow-up of 17% (eg, 37% MEC vs 20% Coping-Together). The 2.5% significance value is chosen to adjust for the multiple comparisons, because the primary endpoint will be tested on the patient and partner separately. Assuming that the correlation between baseline and follow-up measurements of each of the secondary outcomes is similar to that of anxiety, the study will have 90% power to detect a difference between treatment groups of 0.375 SDs in each secondary outcome at the 2.5% significance level. In the unusual situation where there is no correlation between baseline and follow-up values, the study will have 90% power to detect a difference of 0.438 SDs between groups at the 2.5% significance level. To account for a 10% loss to follow-up at each time point,60 187 couples per group will be recruited at baseline. Based on our most recent pilot,48 it is estimated that recruitment will take 18 months.
Procedures
Most participants will be referred to the study by their main treating clinicians, who will identify patients meeting the medical and English fluency inclusion criteria, and briefly introduce the study to patients, provide them with the study brochure and obtain verbal or written consent to pass on their contact information to the research team. The research team will then follow-up with potential participants in approximately 1 week to confirm interest, further screen for their eligibility, and mail a study pack to eligible participants. The study pack will include an information statement, a consent form and baseline survey and a study pack to pass on to their partner. Couples will then be asked to return their consent forms and surveys, using the reply paid envelopes provided, with non-responders followed-up, initially by mail and then by phone. Potential participants can refuse to supply their contact details to their clinician and only take the brochure. Study participation will not be further discussed with their healthcare team.
Alternative recruitment strategies to cater to site-specific requirements include having an on-site research assistant (RA) to explain the study and provide the study pack or the referring clinician may choose to mail invitation letters and study brochures to patients who meet the eligibility criteria. The study will also be promoted by cancer care support organisations and through various media facilities, including print (eg, cancer care organisations consumer newsletters), radio, television and online (eg, Facebook). Interested individuals will also be able to contact the research team directly for more information. Study posters and brochures will also be available at all recruitment sites. This protocol has been approved by relevant local area health and University ethics committees.
Randomisation of group assignment
A computer-generated randomisation schedule with block lengths of variable size (6 or 9 couples) and stratified by cancer type will be programmed into a secure web-based randomisation service, only accessible to the main project manager. Allocation concealment will be ensured, as the website will not release the randomisation code until participants have returned their consent forms/baseline surveys and their consent and information is entered into the secure website.
Coping-Together and MEC conditions
At recruitment, participants will be informed that they will be mailed one of the three packs: the generic Coping-Together pack, the tailored Coping-Together pack or the MEC condition pack. All couples will receive their respective resource pack within 2 weeks of returning their baseline survey, and they will be informed that they can use any or all of these resources sent to them, at their own discretion and pace throughout the duration of the study.
Blinding
Participants are blinded to study hypotheses and group allocation, as they do not know which pack is the ‘study’ intervention, and the survey and contact with the research team are comparable across groups. Selected RA(s) will not be blinded to group allocation, and as part of their role will facilitate the randomisation of participants, assign participants identification numbers and follow-up with participants in accordance with the protocol. The chief investigators and statisticians will remain blinded to group allocation until the database is locked.
MEC condition
A ‘no treatment’ control group will not be employed to ensure that participants are blinded to group allocation and because participants have reported elevated distress. Couples randomised to this condition will receive two booklets (cancer-specific and the ‘Caring for Someone with Cancer’ booklets) from the ‘Understanding Cancer Series’ available at the Cancer Council New South Wales along with a Cancer Council Helpline brochure. One to 2 weeks thereafter, a member of the research team will phone the participants to orient them to the materials received (anticipated duration=20–35 min).
Generic Coping-Together
Generic Coping-Together couples will receive the six Coping-Together booklets previously described, the Coping-Together DVD, a relaxation audio CD and the login to the Coping-Together website. To ensure methodological equivalence of all groups, the generic Coping-Together group will also receive the relevant Cancer Council NSW booklets and Helpline brochure (as per the MEC condition). One to 2 weeks thereafter, a member of the research team will phone participants to orient them to Coping-Together. Then, monthly, the couples will be mailed a ‘Top Tips’ newsletter, featuring the timely aspects of the booklets.
Tailored Coping-Together
Patients and partners randomised to the tailored Coping-Together group will receive the log-in to the Coping-Together website and the DVD as well as an overview of the topics addressed by the Coping-Together booklets; however, throughout the study, they will only receive the Coping-Together booklet sections that pertain to their immediate concerns (main difference between this condition and generic Coping-Together). The first pack will be created on the basis of the challenges identified by the baseline survey, and will also contain the relevant Cancer Council NSW booklets and Helpline brochure (as per the MEC condition). Subsequent packs will be tailored based on the participant's responses to the Cancer-Related Challenge Scale, sent monthly throughout the study. Patients and partners might receive different tailored Coping-Together materials. Couples in this group will receive the orientation call previously described in the MEC condition.
Data collection
Initial distress screening with the DT
The DT will ask participants to rate their overall distress in the past week using a visual analogue scale ranging from 0=‘no distress’ to 10=‘extreme distress’.17 Since its publication, the DT has quickly become the measure of choice for screening for distress, as it is short, simple to use and quick to interpret. To be eligible, either the patient or their partner must score 4 or above, which is the recommended cut-off score on this measure.61 62
Survey
A survey will be completed at baseline (pen and paper) and at 3, 6 and 12 months postbaseline (pen and paper or online, according to participants' preferences) to measure the outcome variables, potential moderators, and sociodemographic and disease variables. Table 2 summarises all measures that will be used. The primary outcome (anxiety) will be measured using the seven-item anxiety subscale of the Hospital Anxiety and Depression Scale,63 the measure of choice to detect anxiety among patients with cancer64 65 and their partners.66
Table 2.
Coping-Together study outcomes and measures
| Measures and psychometrics |
||
|---|---|---|
| Outcomes | Patients | Partners |
| Primary outcome | ||
| Anxiety | Main survey: 7-item HADS-Anxiety Subscale63 (α=0.68–0.93)91 | |
| Secondary outcome | ||
| Depression | Main survey: 7-item HADS Depression subscale63 (α=0.68–0.93)91 | |
| Distress | Main survey: Single-item Distress Thermometer17 | |
| Quality of life (QOL) | Main survey: 35-item Assessment of Quality of Life—8 Dimensions Scale75 (overall α=0.91, subscale α=0.64–0.87)92 | Main survey. 35-item Assessment of Quality of Life—8 Dimensions Scale75 (overall α=0.91, subscale α=0.64–0.87)92 Main survey. 35-item Caregiver's QOL Index-Cancer (α=0.91)76 |
| Relationship satisfaction | Main survey: 32-item Dyadic Adjustment scale77(α=0.89–0.95)31 | |
| Appraisal | Main survey: 28-item Kessler Cognitive Appraisal of Health Scale (α>0.70)67 Main survey: 33-item Mishel's Uncertainty scale (α=.64–0.91)68 |
Main survey. 28-item Kessler Cognitive Appraisal of Health Scale (adapted) (α>0.70)67 Main survey. 33-item Mishel's Uncertainty scale (α=0.64–0.91)68 Main survey. 27-item Appraisal of Caregiving Scale (α>0.85)69 70 |
| Self-efficacy | Main survey: 12-item Communication and Attitudinal Self-Efficacy Scale for cancer (CASE-Cancer; α=0.76–0.77)71 Main survey: 29-item Strategies Used by People to Promote Health (SUPPH, α=0.76–0.92)72 Main survey: 40-item Health Education Impact Questionnaire (heiQ, α=0.70–0.89)73 |
Main survey. 12-item Communication and Attitudinal Self-Efficacy Scale for cancer (CASE-Cancer (adapted); α=0.76–0.77)71 Main survey. 29-item Strategies Used by People to Promote Health (SUPPH, α=0.76–0.92)72 Main survey. 48-item Caregiver Empowerment Scale (α=0.76–0.92)74 Main survey. 40-item Health Education Impact Questionnaire (adaptation, heiQ)73 |
| Dyadic and individual coping | Main survey: 37-item Dyadic Coping Inventory (α=0.73–0.96)79 Main survey: 28-item Brief COPE measures 14 individual-level coping strategies (α=0.60–0.90)78 |
|
| Moderators | ||
| Information-seeking preferences | Resource evaluation survey: 45-item Profile of Preferences for Cancer Information (PPCI) (adapted for partners)81 82 | |
| Information needs | Main survey: 37-item Cancer Information Needs Survey designed for use in the current study to assess the importance of receiving information on a variety of cancer-related topics, and the participant's degree of satisfaction with the information received to date. | |
| Social support | Main survey: 19-item MOS Social Support Survey (α=0.91–0.97)80 | |
| Cancer-related challenges | Main survey (all groups) and monthly for the tailored group: 28-item Cancer-Related Challenge Scale, developed for use in the current study, aligns with the challenges presented in the Coping-Together intervention materials and will assist in assessing resource relevance | |
| Use and relevance of Material sent | Resource evaluation survey: Developed for use in the current study, and ascertains the extent to which participants used the material sent to them, including proportion of the material used and amount of time spent reading the material. Also examines the coping strategies learnt and the usefulness of the resource | |
| Economic evaluation | Main survey: 26-items developed for the current study assessing health service usage, hospital admissions, out-of-pocket expenses, medication usage, community and pastoral care services, disruption to work and usual activities | |
Secondary outcomes (distress, depression, illness or caregiving appraisal, self-efficacy, quality of life, relationship satisfaction, individual and dyadic coping) will be measured by the DT,17 the Hospital Anxiety and Depression Scale depression subscale,63 Kessler's Cognitive Appraisal of Health Scale,67 Mishel's Uncertainty in Illness Scale,68 Caregiving Illness Appraisal Scale,69 70 the Communication and Attitudinal Self-Efficacy scale for cancer Scale,71 Strategies Used by People to Promote Health,72 Health Education Impact Questionnaire,73 Caregiver Empowerment Scale,74 Assessment of Quality of Life (AQoL-8D),75 Caregiver's QOL Index-Cancer,76 Spanier Dyadic Adjustment Scale,77 the Brief COPE78 and the Dyadic Coping Inventory.79
Moderators will be measured at baseline and at 3, 6 and 12 months postbaseline, including unmet information needs (The Cancer Information Needs Survey—designed for the current study) and social support (MOS-Social Support Survey80). Data pertaining the use/relevance of the resource, including coping skills learned will be collected shortly after receipt of the resource materials (first month) then again at 3, 6 and 12 months by the Resource Evaluation Survey. The Profile of Preferences for Cancer Information will also be completed within 1 month of receipt of the intervention materials. The main survey will also measure key sociodemographic, disease and medical variables.
Cost data
For the purpose of the economic analysis, couples will be asked to provide consent for the research team to access their Medicare data (Australia's universal health insurance scheme). Additional questions regarding disruption to usual activities, hospital admissions, use of private allied healthcare services, use of community support services and the use of complementary/alternative therapies will be assessed in the baseline and follow-up surveys.
Orientation phone calls
In addition, all couples (regardless of group allocation) will be contacted by a member of the study team for an initial orientation phone call, approximately 1–2 weeks after they receive their respective resource package. The intent of the orientation call is to ensure that participants received the material, to provide an overview of the content and to explore intended use of the resource. With the participant's consent, all phone calls will be audio recorded and coded to ascertain and monitor the topics that are discussed and as a quality check to ensure that counselling was not provided.
Strategies to enhance recruitment and minimise attrition
Based on other couple-based intervention studies83 and our pilot study,47 the following strategies will be used to maximise recruitment and minimise attrition: (1) the study will be presented to the staff at each participating clinic to elicit support; (2) bright posters will be displayed in the clinics; (3) couples will be approached at a time when the psychological aspects of their illness are more salient, thereby reinforcing psychosocial support as an important aspect of overall health84; (4) a self-directed intervention reduces participation burden, as participants can work through the materials at home and at their own pace and (5) communication with the Coping-Together participants will be maintained for the duration of the study period to encourage attachment and completion (ie, monthly ‘Top Tips’ newsletter).
Data management
All participant consent forms and surveys will be stored in a locked cabinet, as soon as logged by the project manager in the log and monitoring database. The data will be entered in a database specifically designed for this trial by trained personnel. A random 10% of all data entry will be double-checked.
Data analysis
Analysis of primary and secondary outcomes
Intention-to-treat and per protocol (ie, patients and carers who used the intervention for most of the duration of the study) analyses will be conducted. The primary outcome, anxiety, will be measured repeatedly across time, and therefore analysed using generalised-linear mixed models (GLMMs). In this context, GLMMs are similar to linear regression models, but take account of the correlation between repeated measurements on individuals. Sensitivity analysis will explore the robustness of the results against a range of missing data assumptions.85 Separate analyses for patients and partners will examine differences between conditions in anxiety at 3 and 6 months. The outcome in the model will be the participants’ scores at 3 and 6 months, the main predictor variable will be treatment group and the participants’ baseline score will be included as a covariate. Similar models will be used to determine if differences between groups are sustained to 12 months. GLMM will also be used to explore the secondary outcome measures. Multiple testings will be handled using the Benjamini and Hochberg method86 with a nominal α set at 0.05.
Economic analysis
This study will include a formal economic evaluation to assess the cost-efficacy of the intervention. The economic evaluation will comprise a cost-consequences analysis whereby the incremental costs of the intervention will be compared with the full spectrum of outcomes included in the study. This means that a series of cost-efficacy ratios will be determined rather than just one—such an approach has been shown to be useful to decision-makers. The inclusion of the AQoL-8D75 will also enable a cost-utility analysis to be undertaken whereby outcomes are expressed as generic quality adjusted life years (QALYs). Outcomes expressed as QALYs have the advantage of allowing practical judgements regarding the value for money credentials of the intervention to be made. The economic analysis will be largely from a societal perspective, although secondary analysis from narrower perspectives, such as health or government, will also be undertaken, as appropriate, to the different stakeholders of such a project. The actual costs of the interventions will be determined using information from the research team and provider records including interviews with key budgetary personnel to ensure all costs associated with the interventions have been captured. The Medicare data and information obtained during periodic follow-up surveys will be used to determine other resource use and costs incurred by patients and their partners.
The evaluation will first measure and value any change to the use of healthcare resources over the period of the study among the three arms of the trial and then compare any additional costs to the additional outcomes achieved. Standardised economic evaluation techniques including incremental analysis of mean differences, dominance analysis (where more than two interventions are compared) and bootstrapping to determine CIs will be used in the evaluation.
Analysis of orientation calls
All audiorecordings will be analysed by the interviewer using a summary data collection form to monitor the content of the orientation calls.
Ethics and dissemination
Minor adverse events (eg, a participant being tearful and distressed during a session) will be logged and fed back to the study team. Serious adverse events (eg, expressing suicidal thoughts) will be reported immediately to the chief investigator and to the ethics committees. Any protocol amendments will be submitted to the ethics committees before these are implemented, and changes will also be communicated to other relevant organisations (eg, trial registry). Study findings will be disseminated not only through peer-reviewed publications and conference presentations but also through educational outreach visits and interactive educational meetings, publication of lay research summaries and recommendations for further actions in consumer newsletters and websites and publications targeting clinicians.
Discussion
Coping-Together is an innovative coping skills training intervention that translates evidence-based strategies for effective illness self-management and coping into a readily accessible format that couples can use where and when they need to. To the best of our knowledge, Coping-Together is the first intervention of its kind for couples adjusting to a recent cancer diagnosis. Over a 12-month period, we will investigate how Coping-Together is used by both patients and their partners to address their main cancer-related challenges and examine how it impacts on the psychosocial outcomes of patients and partners, with a focus on anxiety, depression, distress, coping, self-efficacy, dyadic adjustment and quality of life. The findings of this trial will add to the literature arguing for greater psychosocial care in the acute postdiagnostic phase and early survivorship, while simultaneously identifying both individual-level and couple-level factors that contribute to patient and partner outcomes.
There are several strengths to this study and numerous potential benefits of the Coping-Together resource that make it potentially an invaluable addition to the psychosocial care of couples dealing with cancer. First, the projected sample size, recruitment from multiple sites across states and the use of a longitudinal design will address some of the methodological limitations of previous couple-based interventions in cancer care (eg, being under powered).87 Second, Coping-Together covers a broad range of cancer-related challenges recently identified across three reviews as common unmet needs of couples facing cancer. Specifically, the areas identified as requiring greater inclusion in interventions that are covered by Coping-Together are strategies for communicating with healthcare professionals,7 87 addressing communication difficulties between partners,7 88 dealing with emotional reactions such as fear, uncertainty, anxiety and depression in both partners7 87 88 and learning new skills to overcome a lack of effective coping skills.87 88 Third, this trial will directly examine the efficacy of Coping-Together in not only reducing negative psychological outcomes but also on a range of outcomes known to impact patients’ and partners’ cancer experience (eg, self-efficacy, dyadic coping). Fourth, the self-directed format addresses issues of access to psychosocial support, especially for couples in non-metropolitan areas. The use of multiple formats also potentially increases the appeal of the resource, and therefore may increase utility to a broader population of cancer patients and their partners. Finally, the self-directed nature of Coping-Together means that it has the potential to be cost-effective and be integrated into practice without increasing pressures on the oncology workforce. The cost-efficacy of the intervention will be directly assessed in this trial, an important consideration as economic evaluation is an often overlooked element of intervention research.89
Despite these strengths, there are also several challenges for the trial. The target population is vulnerable and experiencing an acute stressor, which in turn may impact on both recruitment and retention, a challenge identified by other trials with couples facing cancer.90 Furthermore, the longitudinal nature of the design increases the likelihood of attrition. An additional challenge is whether the measures employed to assess change over time will be sensitive enough to detect clinically significant improvements experienced by the couples.87 This challenge is partly mitigated by the integration of the Resource Evaluation Survey, which may help to clarify trends detected in the outcome data.
Supplementary Material
Acknowledgments
The study detailed in this protocol is endorsed by the Psycho-oncology Co-operative Research Group (PoCoG), The University of Sydney, Australia. The study protocol and relevant documents have been reviewed by the PoCoG Scientific Advisory Committee and the Joint Community Advisory Group.
Footnotes
Contributors: SDL conceived the study, participated in its design, led the development of the Coping-Together resource and drafted the manuscript. AG, JT, JL and KK participated in the design of this study, provided critical feedback on Coping-Together and provided feedback on the draft of this manuscript. CM and PME developed the economic and statistical analysis plan for the study and provided feedback on the draft of this manuscript. STFS and DB have critically reviewed all aspects of this study and the manuscript. All authors have read and approved the final manuscript.
Funding: This work is supported by a National Health and Medical Research Council Project Grant (APP1002715). SDL is supported by a National Health and Medical Research Council Research Fellowship (APP1012869) and AG by a Cancer Institute New South Wales grant.
Competing interests: None.
Ethics approval: Hunter New England Health Human Research Ethics Committee, University of New South Wales Human Research Ethics Committee, University of Newcastle Human Research Ethics Committee, and South West Sydney Local Hospital District Human Research Ethics Committee.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1.Australian Institute of Health and Welfare & Australasian Association of Cancer Registries Cancer in Australia: an overview 2012. Cancer series no. 74. Cat. no. CAN 70. Canberra: Australian Institute of Health and Welfare, 2012 [Google Scholar]
- 2.National Breast Cancer Centre NCCI Clinical Practice Guidelines for the psychosocial care of adults with cancer. Camperdown, NSW: National Breast Cancer Centre, 2003 [Google Scholar]
- 3.Girgis A, Lambert SD. Caregivers of cancer survivors: the state of the field. Cancer Forum 2009;33:167–71 [Google Scholar]
- 4.Girgis A, Lambert SD, Johnson C, et al. Physical, psychosocial, relationship and economic burden of caring for people with cancer: a review. J Oncol Pract 2012 (Epub ahead of print) doi: 10.1200/JOP.2012.000690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harden J. Developmental life stage and couples’ experiences with prostate cancer: a review of the literature. Cancer Nurs 2005;28:85–98 [DOI] [PubMed] [Google Scholar]
- 6.Holland JC, Breitbart WS, Jacobsen PB, et al. eds. Psycho-oncology. 2nd edn New York: Oxford, 2010 [Google Scholar]
- 7.Lambert SD, Harrison JD, Smith E, et al. The unmet needs of partners and caregivers of adults diagnosed with cancer: a systematic review. BMJ Support Palliat Care 2012;2:224–30 [DOI] [PubMed] [Google Scholar]
- 8.Lambert SD, Loiselle CG, Macdonald ME. An in-depth exploration of information-seeking behavior among individuals with cancer: part 1 understanding differential patterns of active information-seeking. Cancer Nurs 2009;32:11–23 [DOI] [PubMed] [Google Scholar]
- 9.Lambert SD, Loiselle CG, Macdonald ME. An in-depth exploration of information-seeking behavior among individuals with cancer: part 2 understanding patterns of information disinterest and avoidance. Cancer Nurs 2009;32:26–36 [DOI] [PubMed] [Google Scholar]
- 10.Dunn J, Ng SK, Holland J, et al. Trajectories of psychological distress after colorectal cancer. Psychooncology 2012. (Epub ahead of print) doi:10.1002/pon.3210 [DOI] [PubMed] [Google Scholar]
- 11.Zabora J, BrintzenhofeSzoc K, Curbow B, et al. The prevalence of psychological distress by cancer site. Psychooncology 2001;10:19–28 [DOI] [PubMed] [Google Scholar]
- 12.Hagedoom M, Sanderman R, Bolks H, et al. Distress in couples coping with cancer: a meta-analysis and critical review of role and gender effects. Psychol Bull 2008;134:1–30 [DOI] [PubMed] [Google Scholar]
- 13.Ben-Zur H, Gilbar O, Lev S. Coping with breast cancer: patient, spouse, and dyad models. Psychosom Med 2001;63:32–9 [DOI] [PubMed] [Google Scholar]
- 14.Lambert S, Girgis A, Lecathelinais C, et al. Walking a mile in their shoes: anxiety and depression among caregivers of cancer survivors at six and 12 months post-diagnosis. Support Care Cancer 2012;21:75–85 [DOI] [PubMed] [Google Scholar]
- 15.Henselmans I, Helgeson VS, Seltman H, et al. Identification and prediction of distress trajectories in the first year after a breast cancer diagnosis. Health Psychol 2010;29:160–8 [DOI] [PubMed] [Google Scholar]
- 16.Lambert SD, Jones B, Girgis A, et al. Distressed partners and caregivers do not recover easily: adjustment trajectories among partners and caregivers of cancer survivors. Ann BehavMed 2012;44:225–35 [DOI] [PubMed] [Google Scholar]
- 17.National Comprehensive Cancer Network Distress management clinical practice guidelines. National Comprehensive Cancer Network, 2012 [DOI] [PubMed] [Google Scholar]
- 18.Rabin EG, Heldt E, Hirakata VN, et al. Depression and perceptions of quality of life of breast cancer survivors and their male partners. Oncol Nurs Forum 2009;36:E153–8 [DOI] [PubMed] [Google Scholar]
- 19.Lynch BM, Steginga SK, Hawkes AL, et al. Describing and predicting psychological distress after colorectal cancer. Cancer 2008;112:1363–70 [DOI] [PubMed] [Google Scholar]
- 20.Given B, Wyatt G, Given C, et al. Burden and depression among caregivers of patients with cancer at the end-of-life. Oncol Nurs Forum 2005;31:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fann JR, Thomas-Rich AM, Katon WJ, et al. Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiat 2008;30:112–26 [DOI] [PubMed] [Google Scholar]
- 22.Trask PC, Paterson AG, Hayasaka S, et al. Psychosocial characteristics of individuals with non-stage IV melanoma. J Clin Oncol 2001;19:2844–50 [DOI] [PubMed] [Google Scholar]
- 23.Folkman S, Moskowitz J. Coping: pitfalls and promise. Annu Rev Psychol 2004;55:745–74 [DOI] [PubMed] [Google Scholar]
- 24.Lazarus R, Folkman S. Stress, appraisal, and coping. New York: Springer Publishing Company Inc, 1984 [Google Scholar]
- 25.Meyerowitz BE, Oh S. Psychosocial response to cancer diagnosis and treatment. In: Miller SM, Bowen DJ, Croyle RT, Rowland JH, eds. Handbook of cancer control and behavioral science: a resource for researchers, practitioners, and policymakers. Washington, DC: American Psychological Association, 2009:361–89 [Google Scholar]
- 26.Manne SL. Coping with cancer: findings of research and intervention studies. In: Martz E, Livneh H, eds. Coping with chronic illness and disability. New York: Springer Science and Business Media, 2007:191–293 [Google Scholar]
- 27.Ko CM, Malcarne VL, Varni JW, et al. Problem-solving and distress in prostate cancer patients and their spousal caregivers. Support Care Cancer 2005;13:367–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berg CA, Wiebe DJ, Butner J, et al. Collaborative coping and daily mood in couples dealing with prostate cancer. Psychol Aging 2008;23:505–16 [DOI] [PubMed] [Google Scholar]
- 29.Kayser K. Enhancing dyadic coping during a time of crisis: a theory-based intervention with breast cancer patients and their partners. Washington, DC: American Psychological Association, 2005 [Google Scholar]
- 30.Helgeson V, Cohen S, Schulz R, et al. Group support interventions for women with breast cancer: who benefits from what? Health Psychol 2000;19:107–14 [DOI] [PubMed] [Google Scholar]
- 31.Manne SL, Norton TR, Ostroff JS, et al. Protective buffering and psychological distress among couples coping with breast cancer: the moderating role of relationship satisfaction. J Fam Psychol 2007;21:380–8 [DOI] [PubMed] [Google Scholar]
- 32.Regan T, Lambert S, Kelly B. Uptake and attrition in couple-based interventions for cancer: perspectives from the literature. Psychooncology. 2013 (Epub ahead of print) doi:10.1002/pon.3342 [DOI] [PubMed] [Google Scholar]
- 33.Osborn RL, Demoncada AC, Feuerstein M. Psychosocial interventions for depression, anxiety, and quality of life in cancer survivors: meta-analyses. Int J Psychiat Med 2006;36:13–34 [DOI] [PubMed] [Google Scholar]
- 34.Regan T, Lambert SD, Girgis A, et al. Do couple-based interventions make a difference for couples affected by cancer? BMC Cancer 2012;12:279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scott JL, Halford KW, Ward BG. United we stand? The effects of a couple-coping intervention on adjustment to early stage breast or gynecological cancer. J Consult Clin Psychol 2004;72:1122–35 [DOI] [PubMed] [Google Scholar]
- 36.Nezu AM, Nezu CM, McClure KS, et al. Project Genesis: assessing the efficacy of problem-solving therapy for distressed adult cancer patients. J Consult Clin Psychol 2003;71:1036–48 [DOI] [PubMed] [Google Scholar]
- 37.Beatty L, Koczwara B, Rice J, et al. Evaluating the efficacy of self-help workbook for women recently diagnosed with breast cancer. Asia Pac J Clin Oncol 2009;5:A241 [Google Scholar]
- 38.Lambert S, Kelly B, Girgis A, et al. Self-reliance and perception of psycho-oncology service needs among distressed women with gynaecological cancer. Support Care Cancer 2012;20:S215 [Google Scholar]
- 39.Tuinman MA, Gazendam-Donofrio S, Hoekstra-Weebers J. Screening and referral for psychosocial distress in oncologic practice: use of the Distress Thermometer. Cancer 2008;113:870–8 [DOI] [PubMed] [Google Scholar]
- 40.Edgar L, Rosberger Z, Collet J-P. Lessons learned: outcome and methodology of a coping skills intervention trial comparing individual and group formats for patients with cancer. Int J Psychiat Med 2001;31:289–304 [DOI] [PubMed] [Google Scholar]
- 41.Tatrow K, Montgomery GH. Cognitive behavioral therapy techniques for distress and pain in breast cancer patients: a meta-analysis. J BehavMed 2006;29:17–27 [DOI] [PubMed] [Google Scholar]
- 42.Jacobsen PB, Meade CD, Stein KD, et al. Efficacy and costs of two forms of stress management training for cancer patients undergoing chemotherapy. J Clin Oncol 2002;20:2851–62 [DOI] [PubMed] [Google Scholar]
- 43.Stiegelis HE, Hagedoorn M, Sanderman R, et al. The impact of an informational self-management intervention on the association between control and illness uncertainty before and psychological distress after radiotherapy. Psychooncology 2004;13:248–59 [DOI] [PubMed] [Google Scholar]
- 44.Krischer MM, Xu P, Meade CD, et al. Self-administered stress management training in patients undergoing radiotherapy. J Clin Oncol 2007;25:4657–62 [DOI] [PubMed] [Google Scholar]
- 45.Beatty L, Lambert S. A systematic review of internet-based self-help therapeutic interventions to improve distress and disease-control among adults with chronic health conditions. Clin Psychol Rev 2013;33:609–22 [DOI] [PubMed] [Google Scholar]
- 46.Lambert S, Girgis A, Turner J, et al. Preliminary findings of a qualitative evaluation of a coping skills intervention for couples facing cancer: insights into preferences for self-directed learning. Psychooncology 2011;20:22 [Google Scholar]
- 47.Lambert S, Girgis A, Chambers SK, et al. Coping-Together: development and pilot testing of a self-directed coping skills intervention for patients-primary support person dyads. Psychooncology 2010;19:S259 [Google Scholar]
- 48.Lambert SD, Girgis A, Turner J, et al. A pilot randomized controlled trial of the feasibility of a self-directed coping skills intervention for couples facing prostate cancer: rationale and design. BMC Health Qual Life Outcomes 2012;10:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Medical Research Council. Developing and evaluating complex interventions: new guidance, 2009. [Google Scholar]
- 50.Folkman S. Positive psychological states and coping with severe stress. Soc Sci Med 1997;45:1207–21 [DOI] [PubMed] [Google Scholar]
- 51.Bodenmann G. A systematic-transactional conceptualization of stress and coping in couples. Swiss J Psychol 1995;54:34–49 [Google Scholar]
- 52.Kayser K, Feldman BN, Borstelmann NA, et al. Effects of a randomized couple-based intervention on quality of life of breast cancer patients and their partners. Soc Work Res 2010;34:20–32 [Google Scholar]
- 53.Bandura A. Social foundations of thought and action: a social cognitive theory. Prentice-Hall, Englewood Cliffs, 1986 [Google Scholar]
- 54.Bandura A. Self-efficacy. Encyclopedia of human behavior. New York: Academic Press, 1994 [Google Scholar]
- 55.Beatty L, Oxlad M, Koczwara B, et al. A randomised pilot of a self-help workbook intervention for breast cancer survivors. Support Care Cancer 2010;18:1597–603 [DOI] [PubMed] [Google Scholar]
- 56.Lambert SD, Girgis A, Turner J, et al. You need something like this to give you guidelines on what to do: couples’ evaluation of mailed, self-directed, coping skills training booklets. Support Care Cancer. In press. [DOI] [PubMed]
- 57.Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Linden W, Satin JR. Avoidable pitfalls in behavioral medicine outcome research. Ann Behav Med 2007;33:143–7 [DOI] [PubMed] [Google Scholar]
- 59.Puhan M, Frey M, Buchi S, et al. The minimal important difference of the Hospital Anxiety and Depression Scale in patients with chronic obstructive pulmonary disease. Health Qual Life Outcomes 2008;6:1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Harden J, Falahee M, Bickes J, et al. Factors associated with prostate cancer patients’ and their spouses’ satisfaction with a family-based intervention. Cancer Nurs 2009;32:482–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Baken DM, Woolley C. Validation of the Distress Thermometer, Impact Thermometer and combinations of these in screening for distress. Psychooncology 2011;20:609–14 [DOI] [PubMed] [Google Scholar]
- 62.Boyes A, D'Este C, Carey M, et al. How does the Distress Thermometer compare to the Hospital Anxiety and Depression Scale for detecting possible cases of psychological morbidity among cancer survivors? Support Care Cancer 2012:1–9 [DOI] [PubMed] [Google Scholar]
- 63.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiat Scand 1983;67:361–70 [DOI] [PubMed] [Google Scholar]
- 64.Luckett T, Butow PN, King MT, et al. A review and recommendations for optimal outcome measures of anxiety, depression and general distress in studies evaluating psychosocial interventions for English-speaking adults with heterogeneous cancer diagnoses. Support Care Cancer 2010;18:1241–62 [DOI] [PubMed] [Google Scholar]
- 65.Lambert S, Pallant JF, Boyes A, et al. A Rasch analysis of the Hospital Anxiety and Depression Scale (HADS) among cancer survivors. Psychol Assess 2013;25:379–90 [DOI] [PubMed] [Google Scholar]
- 66.Lambert SD, Pallant JF, Girgis A. Rasch analysis of the Hospital Anxiety and Depression Scale among caregivers of cancer survivors: implications for its use in psycho-oncology. Psychooncology 2011;20:919–25 [DOI] [PubMed] [Google Scholar]
- 67.Kessler TA. The Cognitive Appraisal of Health Scale: development of psychometric evaluation. Res Nurs Health 1998;21:73–82 [DOI] [PubMed] [Google Scholar]
- 68.Mishel MH. The measurement of uncertainty in illness. Nurs Res 1981;30:258–63 [PubMed] [Google Scholar]
- 69.Northouse LL, Mood DW, Schafenacker A, et al. Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer 2007;110:2809–18 [DOI] [PubMed] [Google Scholar]
- 70.Northouse L, Kershaw T, Mood D, et al. Effects of a family intervention on the quality of life of women with recurrent breast cancer and their family caregivers. Psychooncology 2005; 14:478–91 [DOI] [PubMed] [Google Scholar]
- 71.Wolf MS, Chang CH, Davis T, et al. Development and validation of the Communication and Attitudinal Self-Efficacy scale for cancer (CASE-cancer). Patient Educ Couns 2005;57:333–41 [DOI] [PubMed] [Google Scholar]
- 72.Lev EL, Owen SV. A measure of self-care self-efficacy. Res Nurs Health 1996;19:421–9 [DOI] [PubMed] [Google Scholar]
- 73.Osborne R, Elsworth G, Whitfield K. The Health Education Impact Questionnaire (heiQ): an outcomes and evaluation measure for patient education and self-management interventions for people with chronic conditions. Patient Educ Couns 2007;66:192–201 [DOI] [PubMed] [Google Scholar]
- 74.Krouse HJ. Video modelling to educate patients. J Adv Nurs 2001;33:748–57 [DOI] [PubMed] [Google Scholar]
- 75.Richardson J, Khan M, Iezzi A, et al. The AQoL-8D (PsyQoL) MAU Instrument: overview September 2009. Research paper 39, Centre for Health Economics, 2009
- 76.Weitzner MA, Jacobsen PB, Wagner H, et al. The Caregiver Quality of Life Index–Cancer (CQOLC) scale: development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Qual Life Res 1999;8:55–63 [DOI] [PubMed] [Google Scholar]
- 77.Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J Marriage Fam 1976;38:15–28 [Google Scholar]
- 78.Carver CS. You want to measure coping but your protocol's too long: consider the Brief COPE. Int J Behav Med 1997;4:92–100 [DOI] [PubMed] [Google Scholar]
- 79.Feldman BN, Broussard CA. The influence of relational factors on men's adjustment to their partners’ newly-diagnosed breast cancer. J Psychosoc Oncol 2005;23:23–43 [DOI] [PubMed] [Google Scholar]
- 80.Sherbourne C, Stewart A. The MOS social support survey. Soc Sci Med 1991;32:705–14 [DOI] [PubMed] [Google Scholar]
- 81.Lambert S, Loiselle C. Multi-phase development of the profile of preferences for cancer information scale: challenges and promises. Asia Pac J Clin Oncol 2009;5:A249 [Google Scholar]
- 82.Loiselle CG, Lambert SD. Theoretical and evidence-based development of the profile of preferences for cancer information scale. Psychooncology 2009;18:S74 [Google Scholar]
- 83.Cooley ME, Sarna L, Brown JK, et al. Challenges of recruitment and retention in multisite research. Cancer Nurs 2003;26:376–86 [DOI] [PubMed] [Google Scholar]
- 84.Kayser K, Scott JL. Helping couples cope with women's cancers: an evidence-based approach for practitioners. New York: Springer Science + Business Media, 2008 [Google Scholar]
- 85.White IR, Carpenter J, Horton NJ. Including all individuals is not enough: lessons for intention-to-treat analysis. Clin Trials (Epub ahead of print) doi:10.1177/1740774512450098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Peate M, Saunders C, Gregson J, et al. Development and evaluation of an information booklet about breast cancer and early menopause. Breast J 2012;18:95–6 [DOI] [PubMed] [Google Scholar]
- 87.Baik OM, Adams KB. Improving the well-being of couples facing cancer: a review of couples-based psychosocial interventions. J Marital Fam Ther 2011;37:250–66 [DOI] [PubMed] [Google Scholar]
- 88.Waldron EA, Janke EA, Bechtel CF, et al. A systematic review of psychosocial interventions to improve cancer caregiver quality of life. Psychooncology 2012. (Epub ahead of print) doi:10.1002/pon.3118 [DOI] [PubMed] [Google Scholar]
- 89.Badr H, Krebs P. A systematic review and meta-analysis of psychosocial interventions for couples coping with cancer. Psychooncology 2012. (Epub ahead of print) doi:10.1002/pon.3118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hopkinson JB, Brown JC, Okamoto I, et al. The effectiveness of patient-family carer (couple) intervention for the management of symptoms and other health-related problems in people affected by cancer: a systematic literature search and narrative review. J Pain Symptom Manag 2012;43:111–42 [DOI] [PubMed] [Google Scholar]
- 91.Bjelland I, Dahl A, Haug T, et al. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res 2002;52:69–77 [DOI] [PubMed] [Google Scholar]
- 92.Feldman-Stewart D, Brundage MD, Van Manen L, et al. Evaluation of a question-and-answer booklet on early-stage prostate-cancer. Patient Educ Couns 2003;49:115–24 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


