Abstract
Introduction
Diabetes is a chronic condition associated with many long-term complications. People with diabetes need to actively manage their condition, which can be complex. In consultations with healthcare professionals, patients receive advice about their diabetes but do not always discuss things which concern them, perhaps because of the perceived limited time or embarrassment. We want to test a ‘preconsultation’ intervention in which the patient is supported by a healthcare assistant to complete a web-based intervention aimed at producing an agenda to help them identify important areas for discussion in the consultation. Use of this agenda may enable the patient to play a more active role in that consultation and consequently become more confident, and hence more successful, in managing their condition.
Methods and analysis
In this pilot randomised controlled trial, 120 people with diabetes will be randomised with equal allocation to receive the intervention or usual clinical care. The primary outcome is reduction in glycosylated haemoglobin(HbA1c). Secondary outcomes are patient-reported communication, enablement, self-care activity, diabetes-dependent quality of life, empowerment, satisfaction, health-related quality of life and resource use. The aim of the pilot study was to estimate parameters to inform the design of the definitive trial. Follow-up on quantitative outcomes will be at 3 and 6 months. A nested qualitative study will collect data on the patients’ experiences of producing an agenda. Resource use data and medication use will also be collected via a review of medical records for a sample of participants.
Ethics and dissemination
Approval was granted by the NHS Research Ethics Committee North West—Preston (13/NW/0123). Dissemination will include publication of quantitative and qualitative findings, and experience of public involvement in peer-reviewed journals. Results will also be disseminated to trial participants via workshops led by lay coapplicants.
Trial Registration
ISRCTN75070242.
Keywords: Quality in health care < HEALTH SERVICES ADMINISTRATION & MANAGEMENT, World Wide Web technology < BIOTECHNOLOGY & BIOINFORMATICS, Qualitative Research
Article summary.
Article focus
This paper describes a protocol for a pilot randomised controlled trial of a preconsultation web-based intervention to enable patients with diabetes to produce their own agenda for a consultation with their diabetologist.
Key messages
A preconsultation intervention in which the patient is supported by a healthcare sssistant to complete a web-based intervention will facilitate the production of ‘their agenda’ to help them identify important areas for discussion in the consultation.
Combining trial as well as qualitative research methods ensures that the ‘active ingredients’ of the intervention are identified and explored, which will enable estimate parameters to inform the design of a definitive trial.
Involving patients as collaborators ensures that this research deals explicitly with patients’ information needs, thus increasing the probability of the DIAT intervention being taken up in practice.
Strengths and limitations of this study
This study addresses areas identified as requiring more research in the 2013 Cochrane review of computer-based diabetes self-management interventions for adults with type 2 diabetes, which identified that interventions may have a small effect on blood glucose, but no benefits to cognitive, behavioural or emotional outcomes. The intervention is grounded in real-world patient experience, and pragmatically designed to be scaled up for a definitive trial and use in practice, but a potential limitation is that the follow-up period may not be long enough to demonstrate a reduction in glycosylated haemoglobin.
Introduction
Diabetes will affect an estimated 439 million people globally by 2030, with an estimated 2.5 million in the UK.1 Diabetes is a chronic disease, associated with a number of serious complications, and the costs of treating a person with diabetes rise by 60–90% as vascular problems progress.2 Up to 80% of the National Health Service's (NHS) £9.8 billion annual UK expenditure on diabetes is spent on treating complications.3
Diabetes is largely monitored and managed by patients themselves.4 Self-management is complex, involving, among other things, self-monitoring, behavioural change, medication management and a rigorous lifestyle regimen. Advice from professionals is vital to self-management, improving patients’ ability to cope with their illness. Effective consultations are associated with empowerment, positive behaviour change and improved diabetes outcomes.5–9 However, consultations with diabetologists are infrequent and patients often do not take full advantage of their time with their clinician.10 They may feel embarrassed, rushed or simply have forgotten some of the urgent problems they encountered since their previous consultation. Patients with types 1 and 2 diabetes attending two diabetes centres in England perceived that they were not commonly questioned about sensitive aspects of their condition, such as erectile dysfunction and gastroparesis.11 A UK service evaluation identified that health professionals, including diabetologists, felt competent in identifying patients’ psychological issues but less knowledgeable and skilled in handling them.12 Thus, methods to improve the quality of consultations in terms of the ability of the patient to discuss issues that concern them, understand information and remember and follow advice are consistently sought.
A systematic review found that the most common methods used to improve the quality of consultations are question checklists and patient coaching delivered immediately before consultations, and that information-seeking behaviour and patient satisfaction were most improved by combining coaching with written material.13 Greenfield et al's14 study, using a review of medical records, a treatment algorithm and a behavioural change strategy, improved patient participation in the consultation and glycaemic control. A recent systematic review of computer-based diabetes self-management interventions for adults with type 2 diabetes identified 16 randomised controlled trials, but was unable to distinguish between those that were set in primary care, outpatients or community settings.15 The reviewers concluded that diabetes self-management interventions may have a small effect on blood glucose, with mobile ‘phone-based interventions having a greater impact than computer-based interventions, and no evidence of benefits to cognitive, behavioural or emotional outcomes’. In conclusion, they were unable to discern the active ingredients or optimal ‘dose’ of the interventions.
A relatively inexpensive intervention has been developed by Cegala et al, evolving from an instruction booklet, to booklet plus coaching, to a web-based training module (http://patcom.jcomm.ohio-state.edu/). Cegala et al16 identified that effective communication involves patients: presenting detailed information about how they are feeling; asking questions if desired information is not provided; checking understanding of information that is given to them and expressing any concerns about the recommended treatment. This ‘PACE’ system has shown promise in oncology,17 has an outcome measure for communication18 and can easily be tailored for use by people with diabetes.
The intervention has been designed to facilitate the articulation of patients’ often unvoiced agendas16 18–25 which arise from their continual efforts to manage their conditions.26 27 Discussion of these agendas enables patients to manage their condition more effectively,7 28–30 which includes better adherence.31 32
The PACE intervention has been modified specifically for diabetes (as PACE-diabetes or PACE-D) by the DIAT Project Team. PACE-D is a web-based tool, designed to be completed by a patient before a clinic appointment. In this study, the appointment is with a consultant diabetologist.
A trained healthcare assistant (HCA) will facilitate the use of the PACE-D tool, with the aim of assisting patients to identify the things that they wish to discuss with the diabetologist (ie, their ‘agenda’) in the clinical consultation. The intervention takes approximately 20 min to complete, and consists of a series of open and closed questions, prompts and a list of possible concerns that people with diabetes have identified (eg, ‘increased thirst’ or ‘depression’). On completion, a concise agenda will automatically be produced, which the patient will take into their consultation with a diabetologist, and which may be used subsequently (ie, in discussions with the general practitioner (GP) or practice nurse, and to guide self-management).
PACE-D aims to enable patients to identify their agenda for discussion with the diabetologist, improving communication and empowering patients to be more proactive at managing their diabetes, potentially leading to improved clinical and quality-of-life outcomes. The intervention appears to be a simple and relatively inexpensive tool but requires a rigorous test of its efficacy and cost-effectiveness. Piloting the PACE-D intervention and agenda with people with diabetes could provide improvements in communication, blood glucose management, enablement, self-care, medication use and quality of life, with little impact on cost or clinic time. We will measure enablement and patient perceptions of the effectiveness of the consultation, which are perceived as crucial to effective diabetes control.28
The aim of this pilot study was to obtain the necessary information for the planning of a future definitive trial to assess the clinical and cost-effectiveness of a preclinic intervention specifically for diabetes.
The primary objective of this pilot study was to test the feasibility of running a randomised controlled trial of a preconsultation web-based intervention to improve the care quality and clinical outcomes of people with diabetes.
The secondary objectives were to determine:
The likely success of recruitment strategies.
The acceptability of the research plan to proposed participants and allowance for the estimation of likely participation and attrition rates.
The data that will be useful for estimating the required sample size for a full trial.
The training requirements of those clinic staff tasked with implementing the intervention.
Resource use, for example, the use of staff, required to provide the intervention and usual care.
A preliminary estimate of the cost of the intervention.
The validity and responsiveness of quality-of-life outcome measures in the patient group (including generic preference-based measures).
The practicality and accuracy of using alternative methods of data collection for service and resource use (ie, patient report/review of medical records).
Patient and public involvement
Patient and public involvement (PPI) is fundamental to all aspects of this research. The research question was generated from a research prioritisation exercise, undertaken by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care in the South West Peninsula (PenCLAHRC) with active involvement from the Peninsula Patient and Public Involvement Group (PenPIG).
People with diabetes identified the research topic and suggested that outpatient clinic appointments are pressured times, where health professionals can overlook issues that are worrying patients or where patients can feel inhibited from voicing their concerns. The same topic was identified by a diabetes specialist nurse (DSN) at a comparable professional workshop.
A project team was convened and a scoping exercise undertaken to assess what is known about the problem, and members of PenPIG discussed the existing research and perceptions of current and desired future clinic consultations. Two members of PenPIG who have diabetes joined the research team as coapplicants on this proposal. They also have representative roles within the local Diabetes Research Network and Devon Diabetes Service Strategy Implementation Group. Supported by a designated PPI Research Fellow, these two coapplicants have cowritten the study documentation and will assist in the analysis of the data and the dissemination of the research results to lay and professional audiences. They are members of the project management team and will assist in training HCAs.
If the findings of the pilot indicate feasibility, there will be patient and public coapplicants on the full trial proposal, which will be submitted to an appropriate source of funding. Members of the public involved in this pilot will be paid travel expenses and receive a payment in recognition of their contribution to the research.
Methods
Trial design
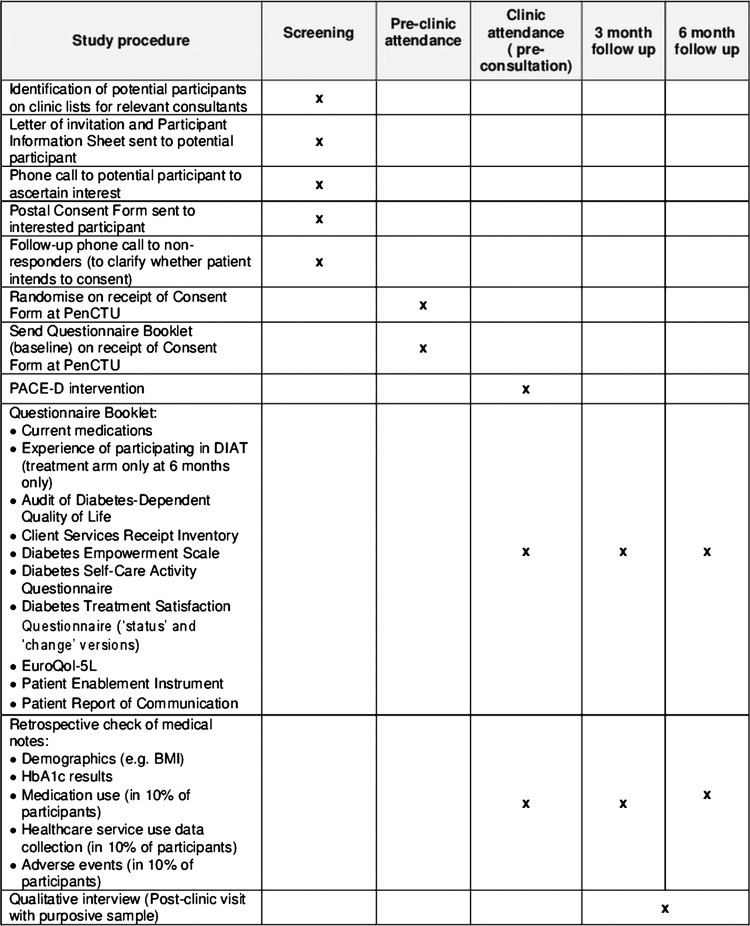
The pilot trial is a pragmatic pilot randomised controlled trial. The outcomes were chosen and the intervention designed during the development phase of the study (see Discussion section; figure 1).
Figure 1.
DIAT trial schedule.
Participants and study setting
The pilot trial will recruit 120 patients attending diabetes outpatient clinics at two hospitals in Devon, south-west England, which treat people from urban and rural settings. In 2010/2011, these two diabetes centres undertook approximately 9000 new appointments and 12 000 follow-up appointments. People with a range of diabetes complications and comorbidities will be included in the pilot, and the experiences gained will inform the inclusion and exclusion criteria of the larger trial. Although the intervention might potentially have benefit for all consultations (including those in primary care), the benefit is likely to be greater in secondary care where typically more issues and problems are discussed. Eligible patients are adults with type 1 or 2 diabetes mellitus who are due to attend outpatient appointments with a diabetologist. Participants are aged 18 or over and have basic spoken or written English (to complete outcome measures). Women with pre-existing or gestational diabetes and people receiving insulin pump therapy are excluded.
Recruitment of patients
The study sample comprises people with diabetes who are due to attend a general diabetes clinic appointment at the Macleod Diabetes and Endocrine Centre at the Royal Devon and Exeter Hospital, Exeter, or the Medical Outpatients Department at Derriford Hospital, Plymouth. Potential participants will be identified from the clinic lists of participating consultant diabetologists by a research nurse at each location. Patients who express an interest in participating in the trial will be sent an information sheet. A research nurse will telephone each potential participant after a minimum of 1 week, discuss any questions that the patient may have and establish if they are willing to participate. The nurse will then send a consent form and baseline questionnaires to those willing to take part. Following receipt of informed written consent and the completed baseline questionnaires, participants will be randomised to receive either the intervention or usual care (control), as detailed below.
Intervention
In a 20 min session immediately preceding the clinic appointment, a trained HCA will help the patient to complete the PACE-D tool (the aim being for the patient to identify and produce their own agenda for the consultation). After the intervention, the patient will proceed to the clinical consultation, in which the printed output from the PACE-D intervention will act as an agenda for the consultation. Owing to the nature of the intervention and the production of an agenda, it will not be possible to blind health professionals or patients to trial allocation. With consent, 10 participants across the two sites will be audio-recorded as they use the PACE-D tool, for qualitative analysis.
Control
This comprises clinical care normally given by the diabetologist in outpatient clinics.
Outcomes
Primary outcome measure
The primary outcome measure is glycosylated haemoglobin (HbA1c),33 a measure of glycaemic control. HbA1c levels will be measured within 4 weeks of each assessment (ie, at baseline, 3 and 6 months), and will be retrospectively obtained from participants’ medical records.
Secondary outcome measures
Secondary outcome measures (patient self-reported rating scales) will be measured at all three time points. The rating scales will be sent to all participants with instructions for completion and a prepaid return envelope. In addition, participants will be asked to document their current medication at each time point, as well as the number and type of contacts with primary and secondary care practitioners during the study. Those in the treatment arm will also be asked at 6 months about their experience of using the PACE-D tool and the utility of producing ‘their agenda’.
Patient self-reported outcome measures:
Audit of Diabetes-Dependent Quality of Life-19 (ADDQoL): Developed to measure an individual’s perception of the impact of diabetes on their quality of life,34 this tool has 2 overview items and 19 individual domains (eg, working life, holidays, physical appearance, etc). For each domain, the respondent reports the impact of diabetes on their quality of life (on a 5-point scale, scored from −3 to 1 with higher scores indicating a greater impact) and the importance of the domain (on a 4-point scale score from 0 to 3 with higher scores indicating greater importance). The quality-of-life score for each domain is calculated by taking the product of the impact and importance scores with scores ranging from –9 (maximum negative impact of diabetes) to +3 (maximum positive impact of diabetes). The average weighted impact score is calculated as the mean across the domain scores. The Patient Report of Outcomes Measure Group, Oxford35 recommends the use of ADDQoL as their preferred diabetes-specific measure.
Client services receipt inventory: Originally developed for collecting cost-related information for people with mental health problems over a given period (usually the past 6 or 12 months),36 this is a long-established and widely adapted questionnaire. It collects retrospective information about the interviewee's use of health and social care services, home and employment situation, as well as income and benefits. We will pilot a simplified version of this questionnaire, tailored for diabetes and capturing resource use over a 3-month period, for intended use in the main trial.
Diabetes empowerment scale-short form (DES): This scale was developed in the USA to measure diabetes-related psychosocial self-efficacy.37 38 This eight-item scale, derived from a behaviour change model, employs a five-point Likert scale (strongly disagree (1) to strongly agree (5)). An overall score for DES is calculated by taking the mean of the item scores.
Diabetes self-care activity measure: This 11-item instrument is a self-reported questionnaire of diabetes self-management which includes five aspects (activities) of the diabetes regimen.39 40 Questions for general diet (two items), specific diet (two items), exercise (two items), blood glucose testing (two items) and foot care (two items) use an eight-point Likert scale (from 0 to 7) to record the number of days in the past week that the activity was undertaken. The overall score for each activity is calculated as the mean of the two items. Smoking (during the past 7 days) is recorded as yes or no, with smokers additionally reporting the number of cigarettes smoked on an average day.
Diabetes treatment satisfaction questionnaire—status (status, DTSQ(S)) and change versions: DTSQ(S) was developed to measure patient satisfaction with diabetes treatment.41 42 DTSQ(S) consists of six items to assess treatment satisfaction and two items to capture patient perceived hypoglycaemia/hyperglycaemia. The DTSQ(S) items are scored on a Likert scale from 0 to 6 (0=very dissatisfied, 6=very satisfied). A total score is created as the sum of scores across the treatment satisfaction items (possible score from 0 to 36). In response to concerns about ceiling effects, where high baseline scores provide little opportunity to register change at follow-up, the authors produced the DTSQ ‘change’ version (DTSQ(C)), which contains the same items, but asks patients to consider their satisfaction with current treatment compared with their previous treatment.43 DTSQ(C) items are scored on a scale from −3 to 3 (−3=less satisfied now, 3=more satisfied now, with a midpoint of 0 reflecting no change). The total score is again calculated by summing the scores on the treatment satisfaction items, with the range of possible values from −18 to 18. Both versions will be used in order to capture initial perceptions and any change at follow-up.
EuroQoL (EQ-5D-5 L): The original EQ-5D is a generic measure for valuing and describing health. It defines health in terms of: mobility, self-care, usual activities, pain/discomfort and anxiety/depression and uses a three-point Likert scale (no problem, some problem, extreme problem44). EQ-5D health states, defined by the EQ-5D descriptive system, may be converted into a single summary index by applying a formula that essentially attaches values (also called weights) to each of the levels in each dimension. The Patient Report of Outcomes Measure Group, Oxford35 recommends the use of EQ5D as their preferred generic measure in combination with a disease-specific instrument. However, this instrument has also been found to suffer from ceiling effects, and a five-level version has been developed (EQ-5D-5 L), which uses a five-point Likert scale (no problem, slight problem, moderate problem, severe problem, extreme problem) and has demonstrated increased reliability and sensitivity.45
Patient enablement instrument (PEI): Developed to measure patient enablement after a consultation with a physician, PEI contains six items with a four-point Likert scale: not applicable/same or less (0); better/more (1); much better/much more (2).46 The total score is the sum of scores across the items (possible range of scores is 0 to a maximum score of 12). Haughney et al47 have subsequently modified the opening statement to capture perspectives on treatment specifically, and this version will be used.
Patient report of communication: Developed to measure communication in conjunction with the PACE tool, this instrument comprises 11 questions about perceived communication, with two items for each of the four PACE skills, two additional items for the patient's ability to state their preferences and a global item about the consultation.18 It uses a 5-point Likert scale that captures aspects of doctor–patient communication as never (1), not very often (2), sometimes (3), usually (4) and always (5). Mean scores will be calculated for each PACE skill and across all 11 items. This instrument has been shown to be reliable in patients with cancer and those undergoing surgery.18
Participant timeline
A brief explanation of the participant's timeline is shown in (figure 2).
Figure 2.
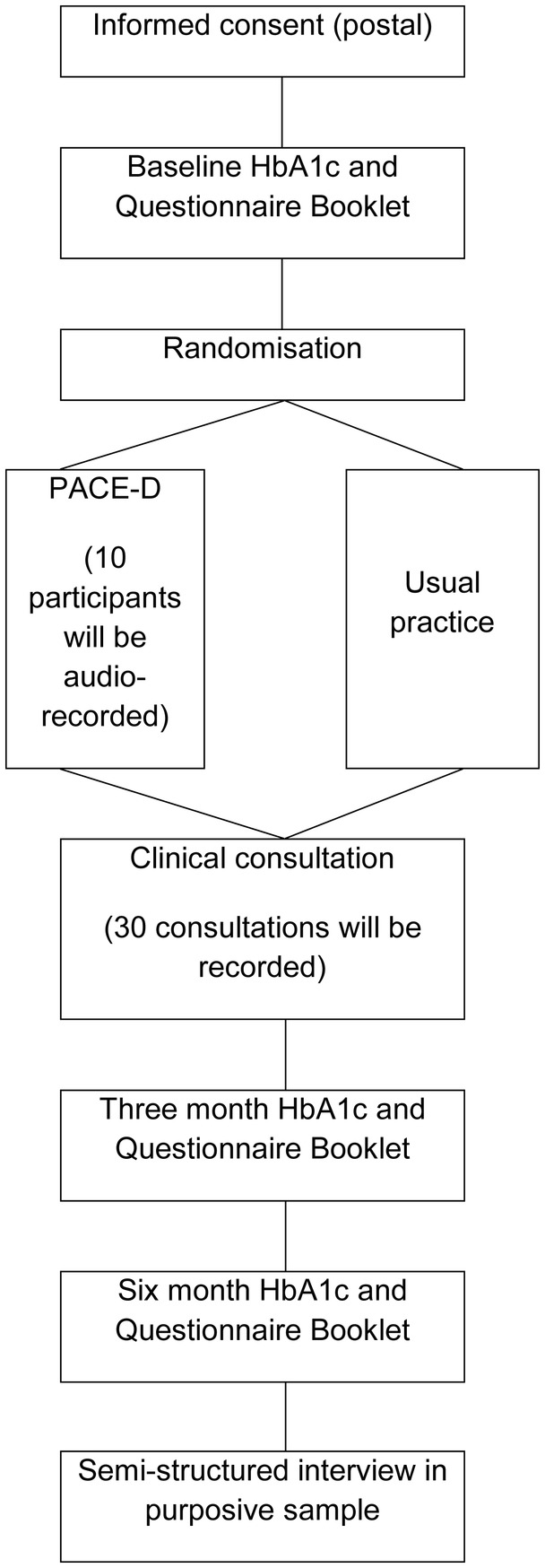
Flow of participants.
Sample size
As this is a pilot study, comparison of the outcomes between the trial arms is not a major objective and the study is not powered to do this. We aim to recruit 120 patients, 60 at each site. At least six clinic ‘sessions’ (ie, the period of time in which a clinic is held within the outpatient department, usually in the morning or afternoon, when 8–15 patients are seen by their consultant) at each site will be required.
An objective of the pilot study is to estimate the SD for continuous outcomes to be used in the definitive trial as this will facilitate the sample size calculation for that study. We anticipate that at least half of the participants (ie, 60) will provide the follow-up data at 6 months. Sixty patients are sufficient to estimate an SD to within 22% of its true value based on the upper bound of the 95% CI.
The study will also estimate the percentage of eligible participants that participate and the percentage of participants that are successfully followed up. If the true percentage of participants that provide follow-up data at 6 months is 50%, this study will be able to estimate this with a margin of error of ±13%, based on a 95% CI, assuming that participants from a given clinic session are no more likely to drop out than those from another session.
Randomisation
An independent statistician based at the Peninsula Clinical Trials Unit (PenCTU) will generate the randomisation list, using computer-generated random numbers. Randomisation will be stratified by clinic session.
Randomisation will be achieved by means of an automated web-based system created by a PenCTU data programmer in conjunction with the independent statistician and accessed by a separate member of the PenCTU staff on receipt of the completed consent form. Consenting participants will be allocated with equal probability to receive PACE-D or usual clinical care, using randomly permuted blocks of varying size to generate the allocation sequence and achieve balance in the numbers of participants allocated to each group.
Following randomisation, PenCTU will notify participants by standard letter about the arrival time for their clinic appointment. Those in the intervention arm will be notified that they are required to arrive 30 min early, while those in the control arm will be notified that they are not required to arrive early.
Statistical methods
The main aim of this pilot study was to estimate parameters that will ultimately inform the design of the main trial. The participation rate will be calculated as the percentage of eligible participants that are randomised, with 95% CIs. The loss to follow-up rate will be reported at 3 and 6 months with 95% CIs. SD will be reported with 95% CIs for the primary outcome. Other parameters to be reported include mean duration of the clinic conversation in each trial arm.
In ancillary analyses, baseline characteristics will be reported using percentages for categorical data, and means and SDs (or medians and IQRs) for quantitative data. The trial arms will be compared at 3 and 6 months using the t test for quantitative outcomes and the χ² test for binary outcomes. Linear and logistic regression, respectively, will be used to adjust comparisons for baseline scores on the outcome. There will be no interim analyses, and neither will stopping rules be applied. Missing data will not be imputed.
Qualitative methods
Ten intervention sessions will be audio-recorded with the participants’ consent, in order to explore how participants utilise the PACE-D intervention and the amount of assistance that they require from HCA in order to complete their agenda form.
In addition, approximately 30 clinical consultations across both trial arms and study sites will be audio-recorded, with the consent of both the participants and their diabetologist. Maximum variance sampling will be used so that any impact of variables of interest (ie, patient age, clinician grade or clinic site) can be explored.
Recording consultations is crucial to understanding the mechanism that underlies the impact of the production of an agenda on the clinical consultation, and its subsequent utilisation in practice, when compared with usual care. Hence, we will report on the fidelity of the intervention, content of the consultation, context for the use of the agenda and any impact on the consultation.
Semistructured interviews will also be conducted with a sample of 30 participants across trial arms and research sites, after participation in the trial has been completed and in order to examine aspects of intervention and participants’ experiences of diabetes consultations in more depth.48 With the participants’ consent, these interviews will be audio-recorded and will explore: participants’ experience of diabetes and clinical consultations; raising concerns with health professionals in primary and secondary care; participants’ experience of either usual care or intervention and trial participation.
For the semistructured interviews, participants in both trial arms will be purposefully sampled to include those with type 1 or 2 diabetes, new and existing patients, and people with different ages/genders/socioeconomic backgrounds and, where possible, different comorbidities, following a maximum variation sampling strategy.49 It is necessary to include interviews with participants in the usual care arm of the trial to explore how patients normally voice their agendas during diabetes consultations, and with what consequences. The interviews will take place after the final follow-up at 6 months, to avoid any influence of the interview on these measures. Interviews will be conducted at a location that is convenient to the participant.
A topic guide will be used, which has been developed with involvement from the PPI coapplicants, to ensure that the primary issues are covered, while allowing flexibility for new issues to emerge from each interview. Interviews will be digitally recorded, fully transcribed and anonymised to protect confidentiality.
In addition to the interviews with participants, approximately 10 interviews with health professionals (eg, HCAs, research nurses and diabetologists) involved in the study at each research site will be conducted near the end of the trial. They will explore the professionals’ views about the intervention and issues around implementation. A flexible topic guide will be employed and these interviews will explore: professionals’ experience of diabetes and clinical consultations; addressing patients’ concerns in secondary care; professionals’ experience of usual care and the intervention and trial participation.
The audio-recordings from the consultations and interviews will be transcribed and read in detail by team members who are experienced in qualitative research methods and a list of common themes and concepts drawn up.26 Data collection and analysis will be literative and ongoing, with the coding frame refined as new themes and categories are identified from subsequent interviews.50 The qualitative data will be managed using Nvivo software.
Cost-effectiveness methods
An economic evaluation will not be conducted as part of this pilot study. However, data will be collected to inform the design of the economic evaluation alongside the planned definitive trial, by: comprehensively estimating the range of care resource use and cost impacts related to the intervention (ie, potential costs of implementation using HCA or research nurses or DSNs or other modes of delivery) and its expected outcomes; refining and justifying the choices of outcome measures for health-related quality of life and testing the practicality and validity of methods for collecting patient-reported resource/service use; and providing some preliminary estimates of different parameters and their variances.
Dissemination
Dissemination of the results and projected outputs will be appropriate to that of a pilot study, and the key output will be an application to an appropriate funder for a definitive trial of the intervention. As the research question was generated through the PPI Group, and service users are integral to the research team, the results of the study will be of particular interest to those who use diabetic services. The PPI coapplicants with other members of the research team will disseminate the results of this pilot to the trial participants, via two workshops, which will be conducted at neutral locations towards the end of the study.
The results from the pilot will be more widely disseminated in order to share our experiences and to generate enthusiasm for the future definitive trial. We will inform people with diabetes through articles in lay health magazines, electronic forums and presentations. We will inform clinicians and health-service managers through submissions to appropriate journals and presentations at suitable conferences.
Results from the future definitive trial would be disseminated widely through a variety of media, including peer-reviewed journal articles and conference presentations, with an emphasis on reaching NHS policymakers and commissioners, health professionals and service users.
Discussion
During the development phase of the research, three key methodological aspects were discussed.
The research team has purposely chosen to trial the PACE-D (intervention) in secondary care—a decision which was much debated during the study development phase. Discussions included people with diabetes (both types 1 and 2, including those who have experience of consultations with diabetologists in the hospital outpatient setting), GPs, diabetologists, DSNs, practice nurses and lay and professional members of the Diabetes Research Network and Primary Care Network. Following these lengthy discussions, a decision was made to sample new and existing patients attending clinic appointments with six diabetologists at two different hospitals, as it is believed that these people may have a particular set of concerns. If the intervention is successful in this population, we may consider undertaking future research with the intervention in primary care settings, where patients may have a different set of concerns.
The potential for contamination between the trial arms resulting from the use of individual patient randomisation was debated by the research team, and a number of alternative randomisation strategies were considered, including cluster randomisation of clinics, consultants or sites. The research team reached a consensus that contamination is unlikely in this context, given that the active ingredient of the intervention is use of the PACE-D tool, and therefore decided to use individual randomisation.
People with diabetes identified the research topic and requested that the intervention (PACE-D) should be facilitated by a DSN. However, while the study was being designed and discussions with local NHS partners were undertaken, it was apparent that DSNs are increasingly time pressured. A pragmatic decision was therefore made by the research team, including lay representatives, that the trial intervention should be facilitated by a number of HCAs routinely present at general outpatient diabetes clinics, and who will be trained in study procedures by a DSN coapplicant. It is thought that this will provide a valid insight into how the intervention would work in a future trial and in the ‘real world’ clinical setting.
Conclusion
People with diabetes need to actively monitor and manage their condition; however, they are not always able to discuss things which concern them at clinical consultations with their diabetologist. Guidelines in the UK emphasise the importance of more actively involving people with diabetes in the consultation process and ongoing management of their condition. The DIAT study aims to inform best practice in this area by evaluating an intervention to assist patients to produce an agenda for their consultation. We think that this may enable patients to play a more active role in that consultation and subsequently make them more enabled, and hence successful at managing their condition.
Supplementary Material
Acknowledgments
The authors would like to thank the study sponsor: Royal Devon and Exeter NHS Foundation Trust. They are grateful to Donald Cegala (Emeritus Professor of Communication and Family Medicine, Ohio State University) for supporting their use and modification of the PACE intervention.
Footnotes
Collaborators: FH-G and JH, Peninsula Public Involvement Group (PenPIG), National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for the South West Peninsula.
Contributors: NB, CA, FH-G, JH, AG, OCU, BV, MD, JP and JF conceived the original study and developed the protocol with WI and JV. JF led the writing of the first draft of the manuscript, with contributions from RA, CA, MD, AG, WI, JP, OCU, BV, JV and NB. All authors contributed to the editing and redrafting.
Funding: This research is funded by the National Institute for Health Research (NIHR) under its Research for Patient Benefit (RfPB) Programme (Grant Reference Number PB-PG-0711-25087).
Competing interests: AG is funded by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for the South West Peninsula. OCU is partially supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for the South West Peninsula. NB is partially supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for the South West Peninsula.
Ethics approval: The study was approved by the NHS Research Ethics Committee North West—Preston (13/NW/0123).
Provenance and peer review: The research question was generated from a research prioritisation exercise, undertaken as part of the Peninsula Collaboration for Leadership in Applied Health Research and Care (CLAHRC) Patient and Public Involvement Group (PenPIG); internally peer reviewed.
References
- 1.Shaw J, Sicree R, Zimmet P. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010;87:4–14 [DOI] [PubMed] [Google Scholar]
- 2.Dancer S, Courtney M. Improving diabetes outcomes: framing research into the chronic care model. J Am Acad Nurse Pract 2010;22:580–5 [DOI] [PubMed] [Google Scholar]
- 3.Hex N, Bartlett C, Wright D, et al. Estimating the current and future costs of Type 1 and Type 2 diabetes in the UK, including direct health costs and indirect societal and productivity costs. Diabetic Med 2012;29:855–62 [DOI] [PubMed] [Google Scholar]
- 4.Anderson R, Funnell M. Patient empowerment: reflections on the challenge of fostering the adoption of a new paradigm. Patient Educ Couns 2005;57:153–7 [DOI] [PubMed] [Google Scholar]
- 5.Piette J, Schillinger D, Potter M, et al. Dimensions of patient-provider communication and diabetes self-care in an ethnically diverse population. J Gen Intern Med 2003;18:624–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Dam H, van der Horst F, van den Borne B, et al. Patient-provider interaction in diabetes care: effects on patient self-care and outcomes: a systematic review. Patient Educ Couns 2003;51:17–28 [DOI] [PubMed] [Google Scholar]
- 7.Williams G, McGregor H, Zeldman A, et al. Promoting glycaemic control through diabetes self-management: evaluating a patient activation intervention. Patient Educ Couns 2005;56:28–34 [DOI] [PubMed] [Google Scholar]
- 8.Sturt J, Taylor H, Doherty A, et al. A psychological approach to providing self-management education for people with type 2 diabetes: the Diabetes Manual. BMC Fam Pract 2006;7:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rose V, Harris M, Ho M, et al. A better model of diabetes self-management? Interactions between GP communication and patient self-efficacy in self-monitoring of blood glucose. Patient Educ Couns 2009;77:260–5 [DOI] [PubMed] [Google Scholar]
- 10.Keers J, Links T, Bouma J, et al. Do diabetologists recognise self-management problems in patients? Diabetes Res Clin Pract 2004;66:157–61 [DOI] [PubMed] [Google Scholar]
- 11.Grant P, Lipscomb D. How often do we ask about erectile dysfunction in the diabetes review clinic? Acta Diabetol 2009;46:285–90 [DOI] [PubMed] [Google Scholar]
- 12.Mosely K, Aslam A, Speight J. Overcoming barriers to diabetes care: perceived communication issues of healthcare professionals attending a pilot diabetes UK training programme. Diabetes Res Clin Pract 2010;87:e11–14 [DOI] [PubMed] [Google Scholar]
- 13.Kinnersley P, Edwards A, Hood K, et al. Interventions before consultations for helping patients address their information needs (review). Cochrane Database Syst Rev 2007;(3):CD004565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greenfield S, Kaplan S, Ware J, et al. Patients’ participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med 1988;3:448–57 [DOI] [PubMed] [Google Scholar]
- 15.Pal K, Eastwood SV, Michie S, et al. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev 2013;(3):CD008776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cegala D, Post D, McClure L. The effects of patient communication skills training on the discourse of elderly patients during a primary care interview. J Am Geriatr Soc 2001;49:1505–11 [DOI] [PubMed] [Google Scholar]
- 17.Fleisher L, Buzaglo J, Collins M, et al. Using health communication best practices to develop a web-based provider–patient communication aid: the CONNECT study. Patient Educ Couns 2008;71:378–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bylund C, D'Agostino T, Ho E, et al. Improving clinical communication through concordance based patient education. Commun Educ 2010;59:294–311 [Google Scholar]
- 19.Greenfield S, Cretin S, Worthman L, et al. Comparison of a criteria map to a criteria list in quality-of-care assessment for patients with chest pain: the relation of each to outcome. Med Care 1981;19:255–72 [DOI] [PubMed] [Google Scholar]
- 20.Greenfield S, Kaplan S, Ware J. Expanding patient involvement in care: effects on patient outcomes. Ann Intern Med 1985;102: 520–8 [DOI] [PubMed] [Google Scholar]
- 21.Kravitz R. Patients’ expectations for medical care: an expanded formulation based on review of the literature. Med Care Res Rev 1996;53:3–27 [DOI] [PubMed] [Google Scholar]
- 22.Cegala D, McClure L, Marinelli T, et al. The effects of communication training on patients: participation during medical interviews. Patient Educ Couns 2000a;41:209–22 [DOI] [PubMed] [Google Scholar]
- 23.Cegala D, Marinelli T, Post D. The effects of patient communication skills training on compliance. Arch Fam Med 2000b;9:57–64 [DOI] [PubMed] [Google Scholar]
- 24.Curtin R, Sitter D, Schatell D, et al. Self-management, knowledge, and functioning and well-being of patients on hemodialysis. Nephrol Nurs J 2004;31:378–86 [PubMed] [Google Scholar]
- 25.Sleath B, Chewning B, Svarstad B, et al. Patient expression of complaints and adherence problems with medications during chronic disease medical visits. J Soc Adm Pharm 2000;17:71–80 [Google Scholar]
- 26.Barry C, Bradley C, Britten N, et al. Patients’ unvoiced agendas in general practice consultations: qualitative study. BMJ 2000;320:1246–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hamilton W, Russell D, Stabb C, et al. The effect of patient self-completion agenda forms on prescribing and adherence in general practice: a randomised controlled trial. Fam Pract 2007;24:77–83 [DOI] [PubMed] [Google Scholar]
- 28.Funnell M, Anderson R. Empowerment and self-management of diabetes. Clin Diabetes 2004;22:123–7 [Google Scholar]
- 29.Williams G, Freedman Z, Deci E. Testing a self-determination theory process model for promoting glycaemic control through diabetes self-management. Health Psychol 2004;23:58–66 [DOI] [PubMed] [Google Scholar]
- 30.Williams G, Lynch M, Glasgow R. Computer-assisted intervention improves patient-centred diabetes care by increasing autonomy support. Health Psychol 2007;26:728–34 [DOI] [PubMed] [Google Scholar]
- 31.Roter DL. Patient participation in patient-provider interaction: the effects of patient question-asking on the quality of interaction, satisfaction, and compliance. Health Educ Monogr 1977;5:281–315 [DOI] [PubMed] [Google Scholar]
- 32.Rose V, Harris M, Ho M, et al. A better model of diabetes self-management? Interactions between GP communication and patient self-efficacy in self-monitoring of blood glucose. Patient Educ Couns 2009;77:260–5 [DOI] [PubMed] [Google Scholar]
- 33.Perry RC, Shankar RR, Fineberg N, et al. HbA1c measurement improves the detection of type 2 diabetes in high-risk individuals with non-diagnostic levels of fasting plasma glucose: the Early Diabetes Intervention Program (EDIP). Diabetes Care 2001;24:465–71 [DOI] [PubMed] [Google Scholar]
- 34.Bradley C, Todd C, Gorton T, et al. The development of an individualized questionnaire measure of perceived impact on diabetes and quality of life. Qual Life Res 1999;8:79–91 [DOI] [PubMed] [Google Scholar]
- 35.Gibbons E, Fitzpatrick R. Patient Reported Outcome Measures Group. A structured review of patient reported outcome measures for people with diabetes: an update 2009. http://phi.uhce.ox.ac.uk/pdf/Diabetes_2009FINAL.pdf (accessed 20 May 2013)
- 36.Beecham J, Knapp M. Costing psychiatric interventions. In: Thornicroft G.ed. Measuring mental health needs. 2nd edn London: Gaskell, 2001: 200–24 [Google Scholar]
- 37.Anderson R, Fitzgerald T, Funnell M, et al. The diabetes empowerment scale: a measure of psychosocial self-efficacy. Diabetes Care 2000;23:739–43 [DOI] [PubMed] [Google Scholar]
- 38.Anderson R, Fitzgerald J, Gruppen L, et al. The diabetes empowerment scale-short form (DES-SF). Diabetes Care 2003;26:1641–2 [DOI] [PubMed] [Google Scholar]
- 39.Toobert D, Glasgow R. Assessing diabetes self-management: the summary of diabetes self-care activities questionnaire. In: Bradley C.ed. Handbook of psychology and diabetes: a guide to psychological measurement in diabetes research and practice. Switzerland: Harwood Academic, 1994: 351–75 [Google Scholar]
- 40.Toobert D, Hampson S, Glasgow R. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care 2000;23:943–50 [DOI] [PubMed] [Google Scholar]
- 41.Bradley C, Lewis KS. Measures of psychological well-being and treatment satisfaction developed from the responses of people with tablet-treated diabetes. Diabetic Med 1990;7:445–51 [DOI] [PubMed] [Google Scholar]
- 42.Bradley C. Diabetes treatment satisfaction questionnaire. In: Bradley C.ed. Handbook of psychology and diabetes: a guide to psychological measurement in diabetes research and practice. Switzerland: Harwood Academic, 1994: 111–32 [Google Scholar]
- 43.Bradley C. The Diabetes treatment satisfaction questionnaire (DTSQ): change version for use alongside status version provides appropriate solution where ceiling effects occur. Diabetes Care 2007;22:530–2 [DOI] [PubMed] [Google Scholar]
- 44.Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53–72 [DOI] [PubMed] [Google Scholar]
- 45.Herdman M, Gudex C, Lloyd A, et al. Badia X development and preliminary testing of the new five level version of EQ-5D (EQ-5D-5 L). Qual Life Res 2011;20:1727–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Howie J, Heaney D, Maxwell M, et al. A comparison of a Patient Enablement Instrument (PEI) against two established satisfaction scales as an outcome measure of primary care consultations. Fam Pract 1998;15:165–71 [DOI] [PubMed] [Google Scholar]
- 47.Haughney J, Cotton P, Rosen J-P, et al. The use of a modification of the patient enablement instrument in asthma. Prim Care Respir J 2007;16:89–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Frost J, Shaw A, Montgomery M, et al. Women's views on the use of decision aids for decision making about the method of delivery following a previous caesarean section: qualitative interview study. Br J Obstet Gynaecol 2009;116:896–905 [DOI] [PubMed] [Google Scholar]
- 49.Patton MQ. Qualitative research and evaluation methods. 3rd edn London: Sage, 2002 [Google Scholar]
- 50.Mays N, Pope C. Qualitative research in health care. London: BMJ Books, 1996 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.