Abstract
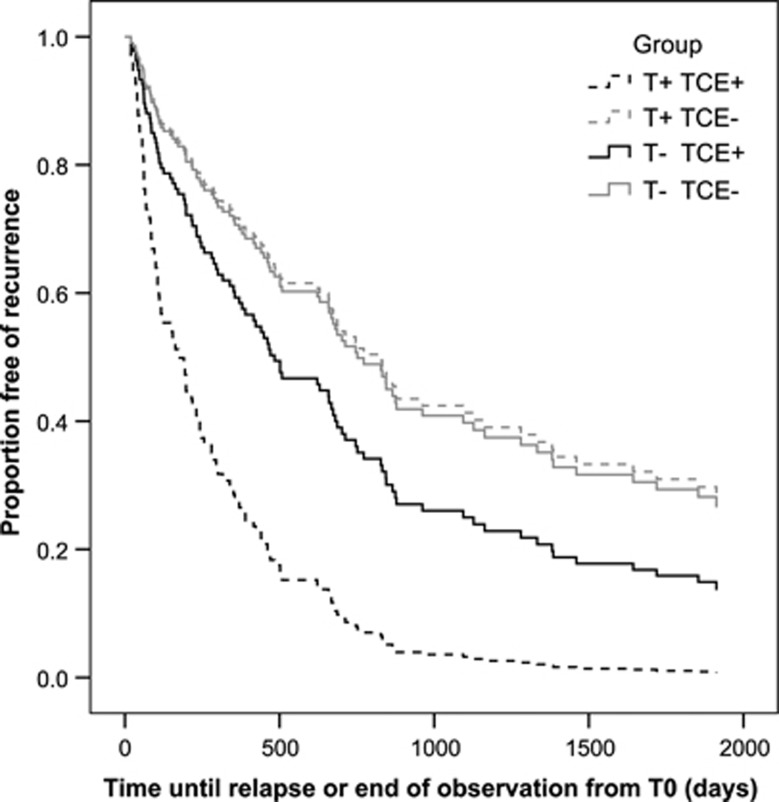
Childhood trauma is associated with the onset and recurrence of major depressive disorder (MDD). The thermolabile T variant of the methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism (rs1801133) is associated with a limited (oxidative) stress defense. Therefore, C677T MTHFR could be a potential predictor for depressive symptomatology and MDD recurrence in the context of traumatic stress during early life. We investigated the interaction between the C677T MTHFR variant and exposure to traumatic childhood events (TCEs) on MDD recurrence during a 5.5-year follow-up in a discovery sample of 124 patients with recurrent MDD and, in an independent replication sample, on depressive symptomatology in 665 healthy individuals from the general population. In the discovery sample, Cox regression analysis revealed a significant interaction between MTHFR genotype and TCEs on MDD recurrence (P=0.017). Over the 5.5-year follow-up period, median time to recurrence was 191 days for T-allele carrying patients who experienced TCEs (T+ and TCE+); 461 days for T− and TCE+ patients; 773 days for T+ and TCE− patients and 866 days for T− and TCE− patients. In the replication sample, a significant interaction was present between the MTHFR genotype and TCEs on depressive symptomatology (P=0.002). Our results show that the effects of TCEs on the prospectively assessed recurrence of MDD and self-reported depressive symptoms in the general population depend on the MTHFR genotype. In conclusion, T-allele carriers may be at an increased risk for depressive symptoms or MDD recurrence after exposure to childhood trauma.
Keywords: childhood trauma, gene–environment interaction, major depressive disorder, methylenetetrahydrofolate reductase gene, recurrence
Introduction
Childhood maltreatment is associated with substantial and long-lasting cognitive and biological effects on the brain including heightened stress sensitivity. Therefore, individuals who have been exposed to childhood maltreatment are predisposed to an unfavorable course of major depressive disorder (MDD) and treatment outcome, as indicated by a recent meta-analysis.1 However, not all individuals exposed to traumatic stress develop a depression. Therefore, it is important to characterize the gene–environment interplay underlying the effects of traumatic childhood events (TCEs) on depression outcomes.
After a first episode of MDD, ∼50% of patients will experience recurrences, which are responsible for considerable disability and impairment.2, 3, 4, 5 Burcusa and Iacono6 stated as an explanation for recurrence in MDD that ‘individuals at high risk for multiple episodes possess the necessary characteristics to make them prone to recurrent depression, and such characteristics exist even before their first episode'. The recurrent type of MDD has a higher heritability than a single episode of MDD.7 Furthermore, biological studies in individuals at risk for MDD, or remitted from MDD, as well as their nondepressed family members, showed that pathophysiological disturbances also precede the development of MDD and remain present after remission, suggestive of stable heritable vulnerability traits, that is, endophenotypes.8, 9, 10, 11, 12 However, a direct identification of candidate genes with recurrence of MDD has proven to be difficult, presumably as a result of complex interactions between genes and environmental stressors.13, 14
A recently emerged pathway potentially underlying susceptibility to onset, symptomatology and recurrence of MDD is folate-mediated one-carbon (1-C) metabolism.15, 16 The 1-C-cycle plays a central role in (1) the regulation of oxidative stress and (2) the generation of methyl groups for methylation of DNA, proteins, phospholipids and neurotransmitters.17, 18 A crucial enzyme in this pathway is 5,10-methylenetetrahydrofolate reductase (MTHFR). A single-nucleotide polymorphism (SNP) in the MTHFR gene (C677T or rs1801133) results in the production of a thermolabile variant of MTHFR, which is associated with decreased methylation capacity19 and increased oxidative stress. This genetically determined variation in 1-C cycle activity associated with increased stress sensitivity may contribute to alterations in neurocognitive functioning and mood regulation.20, 21
Nevertheless, results of meta-analyses on data linking polymorphisms in the MTHFR gene with MDD have been inconsistent.22, 23, 24, 25, 26 From these studies it has become apparent that the main genetic effects overall are weak in MDD, whereas gene–environment interactions may provide stronger predictors.27 Investigating genetic susceptibility to stress is of particular relevance in the context of MDD as stress is considered one of the main pathogenic factors involved in depressive symptomatology and MDD recurrence: TCEs, recent life events, daily hassles and stress related to previous depressive episodes all pose increased risks for MDD and its recurrences.1, 28, 29, 30, 31, 32 Especially during early life, traumatic stress may result in lifelong programming, potentially through methylation-mediated alterations in expression of genes implicated in MDD.27, 33, 34, 35, 36, 37, 38, 39 As mentioned above, the thermolabile T variant of the MTHFR C677T polymorphism is associated with increased vulnerability to oxidative stress and a decreased DNA methylation capacity. Therefore, carriers of the MTHFR C677T variant may be particularly vulnerable to long-lasting effects of childhood traumatic stress on depressive symptomatology and MDD.
To study this proposed relation, we investigated the possible gene × environment interaction between TCEs and the MTHFR genotype as a potential predictor for depressive symptoms and recurrence in patients with a high risk of recurrence of depression over a 5.5-year follow-up period. We hypothesized that recurrently depressed patients carrying the T-allele would have a shorter time to MDD recurrence after exposure to TCEs, whereas this association would not be present in T-allele carriers without exposure to TCEs. Because the effects of the MTHFR genotype may not only be limited to MDD but also be present in the general population, we examined this gene–environment interaction in an independent population-based sample for replication.
Materials and methods
Study participants
The current study was part of the DELTA study, a randomized clinical trial, investigating the effect of cognitive therapy on recurrence in 172 euthymic patients.40, 41 In the DELTA study, we sampled a group of patients with recurrent MDD. We considered these patients to suffer from a more biologically pronounced and endogenously determined subtype of MDD with a relatively high recurrence rate.12 Inclusion criteria of the original trial were: ≥2 previous MDD episodes in the past 5 years, as defined by the Structured Clinical Interview for DSM-IV disorders (SCID);42 in remission >10 weeks and <2 years ago, as defined as a score of <10 on the 17-item Hamilton Depression Rating Scale (HDRS17)43; and 18–65 years old. Exclusion criteria were: (a history of) bipolar spectrum disorder or any psychotic disorder, organic brain damage, alcohol and/or drug abuse and/or dependency or predominant anxiety disorder, all assessed by the SCID. The background, methodology and procedure of the DELTA study have been described in more detail previously.40 At 2 years after baseline, we asked the patients to provide DNA for the current study. After complete description of the study to the subjects, written informed consent was obtained before enrolment. The study was approved by the ethics committee of the Academic Medical Center of the University of Amsterdam (MEC 02/048).
CannabisQuest cohort
Participants in the discovery sample were recruited using a project website launched in 2006 targeted at Dutch young adults and adolescents from age 18 to 25 years (www.cannabisquest.nl).44 Strategies to generate traffic on the project website included collaboration with over a hundred colleges, universities and youth centers, as well as the use of online commercial advertisement products (that is, banners and text links).44 The chance to win an Apple iPod or a Nintendo Wii was used as an incentive. Double entries were prevented by exclusion of subjects with an identical e-mail address, surname and date of birth. Anonymous submission of data was not possible. The online assessment included verification questions to protect against random answers, and participants failing to correctly complete the verification questions were subsequently excluded. From the online data (N=17 698), 1259 participants were included for subsequent genetic assessment in two waves. First, in order to increase power for gene × environment interactions,45 in the context of cannabis and psychosis, we prioritized a sample of 719 participants who belonged to the top or bottom quintile of total scores of psychotic experiences as measured by the Community Assessment of Psychic Experiences (CAPE) score who were either cannabis naive (that is, a lifetime cannabis exposure frequency of <6 times) or were heavy cannabis users (that is, current expenditure for personal cannabis use exceeded 3€ weekly). Second, an unselected sample of 540 individuals was included. As ascertained with the validated Dutch version of either the SCID42 or the MINI International Neuropsychiatric Interview,46 healthy controls had no history of any psychotic disorder. For 84 participants, no interview data were available, and for these cases the presence of a psychotic disorder was excluded by the absence of antipsychotic drug use or a history of psychiatric treatment. The possible concomitant use of recreational drugs was assessed with the substance abuse module of the Composite International Diagnostic Interview.47 Of the 1259 participants who completed comprehensive assessments and provided blood samples for genetic testing, complete data were available for 665 subjects because of a later implementation of the Childhood Trauma Questionnaire (CTQ)48 assessment in the study. All participants provided a urine sample to screen for the presence of recreational drugs in order to verify recent self-reported cannabis use. The study was approved by the ethical review board of the University Medical Center Utrecht and all participants gave written informed consent.
Measurements
Depression
Discovery sample. Using SCID-I, current and past depressive episodes were assessed at baseline, and at 5 follow-up measurements at 3, 12, 24, 36 and 66 months after baseline. With these follow-up assessments, we diagnosed relapses (<6 months after a previous major depressive episode) or recurrences during follow-up, both further addressed as ‘recurrence' for clarity reasons. The trained SCID evaluators were blind to treatment condition and subjects were instructed not to reveal their treatment condition to the interviewers (psychologist/research assistants). All interviews were audio taped. Two independent experienced psychiatrists, also blinded to treatment condition, evaluated all occasions of participants meeting the DSM-IV criteria for MDD. In cases of disagreement, we used the ratings of the psychiatrists. The κ-value for inter-rater agreement between the interviewers and psychiatrist on categorization of a relapse/recurrence or no relapse/recurrence was 0.96, indicating high agreement.40
Replication sample. In the replication sample, the Beck Depression Inventory (BDI) was used to assess depressive symptoms. This validated 21-item self-report questionnaire measures current depressive symptoms during the last week. Each question has four possible answer choices ranging in intensity (0–3), resulting in a total BDI score ranging from 0 to 63.
Traumatic childhood events
Discovery sample. We defined TCEs as having experienced one of the following traumatic events before age 16: parental loss, sustained alcohol and/or drug abuse by caregiver, victim of a serious crime, victim of a serious accident and victim of sexual and/or physical abuse. We selected traumatic stress variables and stressors occurring to the self within this age period using the 7 items from the Negative Life Events Questionnaire that indicate traumatic events: items 5 and 8–13.49, 50 This questionnaire proved to have a good predictive validity, as the number of negative life events predicted MDD symptom severity. We dichotomized the absence or presence of experienced TCEs.
Replication sample. In the replication sample, childhood maltreatment was assessed using the 25-item version of the CTQ.48 The CTQ assesses five types of self-report childhood trauma: emotional abuse, physical abuse, sexual abuse, emotional neglect and physical neglect. The validity of the CTQ, including a Dutch translation, has been demonstrated in clinical and community samples.48,51 One translated item (I believe I was molested) was excluded as this translation was found to be an invalid indicator of childhood sexual abuse in a previous validation study.51 Childhood maltreatment was used as the continuous sum score divided by the number of completed items. One item of the CTQ was only available for a subset of the replication sample (My family was a source of strength and support). Additional analyses in which this item was excluded altogether did not affect the results.
Genotyping procedures and analysis
Discovery sample. We collected 20 ml blood samples at patients' homes by venipuncture. DNA was isolated from blood using a filter-based method (QIAamp DNA Mini Kit, Qiagen, Manchester, UK). The PCR primers were designed using Primer 3 (http://frodo.wi.mit.edu/primer3/input.htm). The PCR primer sequence was 5′-GGCAGGTTACCCCAAAGGC-3′ and 5′-TGGGGTGGAGGGAGCTTATG-3′, and the PEX primer sequence was 5′-GAGAAGGTGTCTLCGGGAG-3′. Genotyping was done using a matrix-assisted laser desorption/ionization time-of-flight mass spectrometer from Bruker Daltonics (Wormer, The Netherlands). All samples were genotyped in duplicate to increase reliability.52 Genotyping error rate based on these duplicates was 3.7%.
Replication sample. All participants were of Dutch ancestry. Genotype data were generated on three different array platforms: the Illumina (San Diego, CA, USA) Human Omni Express (N=576), the Illumina Human610-Quad Beadchip (N=768) and the Illumina HumanHap550 array (N=34). For each SNP platform, quality control procedures were initially performed separately using PLINK V1.07.53 Subjects were excluded based on >5% missing genotypes and gender errors. We used linkage disequilibrium-based SNP pruning to select the most informative SNPs (R2 <0.2) only for the subsequent quality control step. This resulted in ∼67k SNPs for the sets to assess heterozygosity (F <3 s.d.), homozygosity (F>3 s.d.) and relatedness by pairwise identity-by-descent values (PIHAT >0.15). Data sets were merged with Hapmap Phase 3 individuals to check ethnicity. After these quality control procedures on subjects (excluding in total 101 individuals), quality control on SNPs was performed as follows. All SNPs were filtered on missingness (>2%) and Hardy–Weinberg (P>1e−6) before merging the three data sets. Four duplicates and three related sample pairs were detected in the merged data sets (according to criteria described above) and one outlier after clustering the merged data set. From these data, the MTHFR genotype (rs1801133) was extracted.
Cannabis use (replication sample)
In the replication sample, cannabis use was defined as current use of more than an equivalent of 3€ per week (roughly equivalent to weekly cannabis use) during the past month or longer. The monetary amount spent on cannabis has been reported as a valid proxy of exposure to Δ9-tetrahydrocannabinol.54
Statistical analysis
Genotypes
Although significantly different enzymatic activity and thermolability were reported, overlapping profiles for the TT and CT genotypes have been described, with CC remaining as a distinct genotype.55 Therefore, and for power reasons, the MTHFR C677T polymorphism variable was dichotomized into T-allele carriers (TT and CT combined) and non-T carriers (the wild-type genotype CC) groups in the discovery sample. In the replication sample, genotypes were coded 0, 1, or 2 and modeled as a linear effect (additive genetic model) to account for different genotype distributions because it avoids small subgroup stratification.57 Deviation from Hardy–Weinberg equilibrium was tested by allele counting and χ2 analysis.
Discovery sample. The interaction between the MTHFR genotype and TCEs on MDD recurrence was investigated using Cox regression, which takes into account differences in time at risk and censoring (no recurrence during the study period of 5.5 years). Half the study sample was randomly allocated to preventive cognitive therapy (CT: 8 sessions during the first 3 months after inclusion in the DELTA study). Preventive CT has a protective effect on recurrence that increases with the number of previous depressive episodes.40 To test whether this intervention modified the relation between MTHFR genotype, TCEs and recurrence, we assessed the significance of the four-way interaction of treatment condition by MTHFR genotype by TCEs by the number of previous episodes. Because neither the four-way MTHFR genotype by TCEs by treatment by previous episodes nor the three-way MTHFR genotype by TCEs by treatment interaction terms were significant, patients who were or were not randomized to receive CT were pooled for the Cox regression analyses. MTHFR, TCEs and MTHFR × TCEs were included as predictors in the model; the interaction term tests our hypothesis whether the effect of the MTHFR C677T variant (T-allele carrier, non-T carrier) is modified by TCEs (present, absent). To ensure that our results were not influenced by initial differences in group characteristics, we also reanalyzed the data adjusted for age, gender and antidepressant use by incorporating these variables as covariates in the Cox regression model. We used PASW statistics 18.0 (IBM SPSS, 2010, Chicago, IL, USA). We considered P<0.05 statistically significant.
Replication sample. To examine the interaction between the MTHFR genotype and TCEs on depressive symptoms, the total BDI score was regressed on TCEs, MTHFR genotype, their interaction and covariates using the following model: BDI= β0+(β1*covariate)+(β2* rs1801133)+(β3*TCEs)+(β4* rs1801133*TCEs). As covariates we included cannabis use (modeled as a dichotomous indicator), age and gender. Analyses were performed in R (www.r-project.org).56 Continuous sum scores of the BDI and the CTQ were used.
Results
Sample characteristics
Descriptives of both samples are depicted in Table 1.
Table 1. Characteristics of the discovery and replication samples.
|
Discovery sample |
Replication sample |
|
|---|---|---|
| Characteristics | (n=124) | (n=665) |
| Female % | 74 | 56 |
| Age (range) | 44.5 (21–63) | 20.5 (18–40) |
| Depression scorea | 3.6 (0–9) | 5.4 (0–34) |
| Caucasian % | 100 | 100 |
| MTHFR C677T genotype (rs1801133) | ||
| T/T, % | 12 | 10 |
| T/C, % | 40 | 43 |
| C/C, % | 48 | 47 |
| HWE (P-value) | 0.32 | 0.94 |
| Childhood traumab | 44 | 1.4 (1.0–4.3) |
Abbreviations: HWE, Hardy–Weinberg equilibrium; MTHFR, methylenetetrahydrofolate reductase.
Discovery sample: Hamilton depression rating scale (HDRS) total score; replication sample: Beck Depression Inventory (BDI) total score.
Discovery sample: percent experienced traumatic childhood event(s) (TCE); replication sample: total score Childhood Trauma Questionnaire (CTQ).
Discovery sample
Of the 172 patients of the original trial, 137 provided DNA. Of these 35 patients, 15 (8.7%) were lost to follow-up and the remaining patients (11.6%) did not participate because of a diversity of reasons (for example, being afraid of needles, ethical issues concerning genetic study). Five patients could not be analyzed because of MTHFR C677T genotyping failure (genotyping success rate=96.3%). Of the remaining 132 patients, 1 was non-Caucasian, 2 were lost to follow-up and we could not obtain TCEs data for 4 patients. All analyses pertain to the resulting 124 patients. These 124 patients were comparable to the other 48 patients on gender, age, educational level, number of previous episodes and age of onset of first depression, but differed on marital status and antidepressant use. Compared with the 48 excluded patients, the 124 remaining patients comprised fewer singles (37% vs 54% χ2=4.14, d.f.=1, P=0.042), and more users of antidepressants (57% vs 35% χ2=6.61, d.f.=1, P=0.010).
The MTHFR C677T genotype counts and frequencies in the patients were 60 (48.4%) for the CC variant, 49 (39.5%) for the CT variant and 15 (12.1%) for the TT variant. No deviation from Hardy–Weinberg Equilibrium was observed (χ2=1.00, d.f.=1, P=0.317). T-allele carriers and non-T-allele carriers were largely comparable on demographic and psychopathological characteristics (Table 2), with the exception of educational level, and body mass index. T-allele carriers comprised more persons with medium-level education and had a higher mean body mass index, whereas non-T-allele carriers comprised more individuals with higher-level education.
Table 2. Demographic and clinical characteristics of the discovery sample (Δ) a.
|
T-carriers (n=64) |
Non-T-carriers (n=60) |
||||
|---|---|---|---|---|---|
| Characteristics | Mean | s.d. | Mean | s.d. | P-value |
| Sex (M/F) | 16/48 | 16/44 | 0.832 | ||
| Age, year | 44.0 | 9.8 | 45.1 | 9.7 | 0.534 |
| Educational levelb | 0.020 | ||||
| Low, % | 34 | 32 | |||
| Middle, % | 39 | 20 | |||
| High, % | 27 | 48 | |||
| Marital status (single), % | 42 | 32 | 0.226 | ||
| Received cognitive therapy, % | 48 | 58 | 0.270 | ||
| AD use, yes % | 56 | 58 | 0.815 | ||
| BMI | 28.0 | 6.0 | 26.0 | 4.3 | 0.045 |
| HDRS17 score | 3.8 | 3.0 | 3.5 | 3.0 | 0.638 |
| Number of previous episodes | 4.5 | 4.7 | 7.0 | 12.0 | 0.138 |
| Age of first onset, years | 29.4 | 12.7 | 27.9 | 12.7 | 0.510 |
| Psychiatric diseases first relatives (%) | 63 | 75 | 0.150 | ||
| TCEs (%) | 40.6 | 46.7 | 0.498 | ||
Abbreviations: AD, antidepressant, BMI, body mass index, F, female; HDRS17, 17-item Hamilton Depression Rating Scale; M, male; TCE, traumatic childhood event.
Group comparisons were calculated using Student's t-tests, χ2 tests or Fisher's exact tests.
All data represent baseline values.
Educational level is defined as follows: low, primary education or preparatory middle-level applied education; middle, higher general continued education or middle-level applied education; high, preparatory scientific education, higher applied education or scientific education.
Replication sample
Table 1 reports the distribution of demographic characteristics, childhood maltreatment, BDI and the MTHFR C677T genotype from individuals in the replication sample. Characteristics in the replication sample generalized to the full sample that includes all nongenotyped individuals.44 Genotyping was successful in all subjects and no departure from Hardy–Weinberg Equilibrium was detected.
Recurrence in the discovery sample
Overall, 98 patients (79.0%) experienced relapse/recurrence at least once over the 5.5 years. Mean time to recurrence was 750 days (s.e.=61.7 with a median of 493 days (range 20–2056 days)). The MTHFR C677T by TCE interaction predicted time to recurrence (P=0.017). This indicates that the predictive effect of TCEs on MDD recurrence was modified by MTHFR genotype (T-allele carriers; Table 3). This result did not change after adjusting for age, gender and antidepressant use (P=0.016).
Table 3. Effect of MTHFR modified by TCE in the discovery sample.
| β | s.e.β | Wald | d.f. | P-value | RR | |
|---|---|---|---|---|---|---|
| MTHFR | −0.081 | 0.284 | 0.080 | 1 | 0.777 | 0.923 |
| TCE | 0.368 | 0.296 | 1.544 | 1 | 0.214 | 1.445 |
| MTHFR × TCE a | 0.979 | 0.410 | 5.713 | 1 | 0.017 | 2.663 |
Abbreviations: MTHFR, methylenetetrahydrofolate reductase; TCE, traumatic childhood event; RR, relative risk.
Cox regression analysis.
MTHFR: T-allele carrying patients versus non-T-allele carrying patients, with non-T-allele carriers as the reference category.
TCE: experienced TCE yes/no, with no TCE as the reference category.
P=0.016 after adjustment for age, gender and antidepressant (AD) use.
The extent of the effect modification can be seen by comparing the risk for recurrence between the four MTHFR C677T by TCE combination groups (T+ and TCE+ N=26; T+ and TCE− N=38; T− and TCE+ N=28; T− and TCE− N=32). We found a significantly higher hazard for the T+ and TCE+ groups as compared with the T− and TCE− groups (hazard ratio 3.55; Wald 17.7, d.f.=1, P<0.001). For patients who experienced TCEs, the hazard for recurrence in T-allele carriers was 2.4 times higher than in non-T-allele carriers (P=0.002; Figure 1). This corresponds to the observed differences in median time till recurrence that were respectively 191 days for T+ and TCEs+ patients; 461 days for T− and TCE+ patients; 773 days for T+ and TCE− patients and 866 days for T− and TCE− patients.
Figure 1.
The effect of the gene–environment interaction between methylenetetrahydrofolate reductase (MTHFR) and traumatic childhood events (TCEs) on time to recurrence in 124 euthymic patients with recurrent major depressive disorder (MDD) over 5.5 years. T+ TCE+ vs T− TCE−=3.55 (P<0.001); T+ TCE− vs T− TCE−=0.92 (P=0.78); and T− TCE− vs T− TCE−=1.45 (P=0.21). Relative risk for recurrence of MDD calculated with Cox regression analysis. T−, non-T-allele carriers; T+, T-allele carriers; TCE−, no experience of TCEs; TCE+, experienced TCEs.
Depressive symptoms in the replication sample
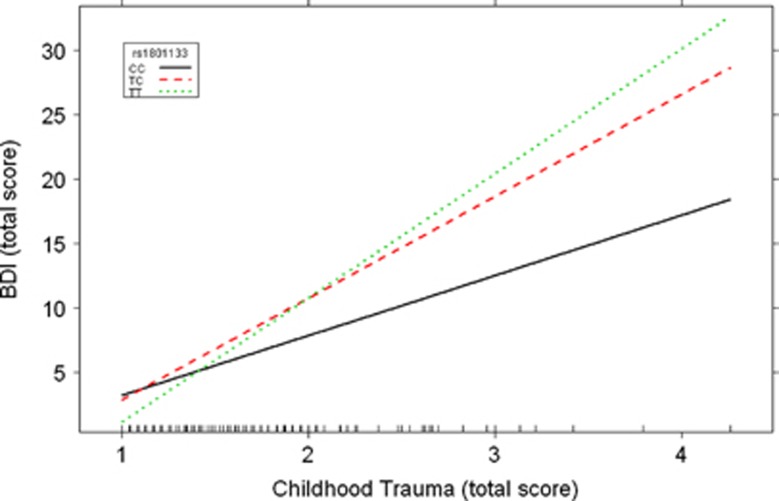
Table 4 shows the results of the linear regression model in the replication sample. Significant effects on depressive symptoms were present for childhood maltreatment (β=11.08, P=5.7 × 10−11), gender (β=−1.06, P=0.036), cannabis use (β=1.25, P=0.027) and the MTHFR genotype (β=4.13, P=0.0054). Moreover, there was a significant interaction between childhood maltreatment and the MTHFR genotype (β=−3.19, P=0.0027). For individuals carrying the TT genotype, childhood maltreatment resulted in increased levels of depressive symptoms (Figure 2).
Table 4. The effects of childhood maltreatment and the MTHFR genotype and their interaction on depressive symptoms in the replication sample.
| Sample | β | s.e. | t-Value | P-value |
|---|---|---|---|---|
| Intercept | −9.00 | 2.98 | −3.02 | 0.0026** |
| Gender | −1.06 | 0.50 | −2.10 | 0.036* |
| Age | −0.023 | 0.091 | −0.26 | 0.80 |
| Cannabis | 1.25 | 0.56 | 2.22 | 0.027* |
| Childhood maltreatment | 11.08 | 1.66 | 6.66 | 5.7 × 10−11*** |
| MTHFR genotype | 4.13 | 1.48 | 2.79 | 0.0054** |
| Maltreatment × MTHFR genotype | −3.19 | 1.06 | −3.03 | 0.0026** |
Abbreviation: MTHFR, methylenetetrahydrofolate reductase.
*P<0.05, **P<0.01, ***P<0.001.
Figure 2.
The gene–environment interaction between methylenetetrahydrofolate reductase (MTHFR) genotype and traumatic childhood events (TCEs) on depressive symptoms in 665 individuals from the general population (P=0.0027). 0, T/T genotype; 1, C/T genotype; and 2, C/C genotype.
To ensure that cannabis use in the replication sample did not influence the interaction between the MTHFR genotype and childhood maltreatment, additional stratified analyses were carried out in noncannabis users (N=478) and cannabis users (N=187).
In both subsamples of the replication sample, the MTHFR × maltreatment interaction was present with a similar directionality (P=0.050 and P=0.056). Moreover, cannabis use did not interact with the MTHFR genotype in the replication sample (P=0.85). Therefore, it is unlikely that cannabis use affected the interaction between childhood maltreatment and the MTHFR genotype.
In both the discovery and replication samples, no significant association was found between the genotype and childhood maltreatment, making the presence of gene–environment correlations unlikely.
Discussion
This study shows that remitted recurrently depressed patients with the thermolabile variant of the MTHFR genotype who have experienced TCEs have a poor prognosis over a follow-up period of 5.5 years, in terms of recurrence of depression. This finding supports existing evidence on the specific role of gene–environment interactions in recurrent depression, especially when TCEs are examined27 and the overall reported unfavorable course in patients with childhood trauma.1 It may explain part of the vulnerability for recurrences in MDD. In support, we also found a significant interaction between childhood trauma and the MTHFR genotype on depressive symptoms in an independent sample from the general population, underscoring the overall importance of MTHFR as a genetic risk factor for depression in the context of early-life stress.
This impact of the combination of early childhood trauma and C677T MTHFR polymorphism on onset of depressive symptomatology and recurrences in MDD gives rise to hypotheses about the underlying pathophysiological pathways. The thermolabile variant of the MTHFR gene may represent a genetic vulnerability factor for limited defense against (oxidative) stress, because it results in a reduction of methyl donors for essential methylation processes, for example, glutathione production and synthesis of neurotransmitters.18 This vulnerability becomes exposed when triggered by enhanced environmental stress such as childhood trauma.37 This could be the result of long-lasting trauma-induced epigenetic changes. These changes include DNA methylation and chromatin modifications, patterns that are inherited but responsive to environmental shifts such as stress, and especially vulnerable during development.58 McGowan et al.59 showed altered methylation of the promoter region of the glucocorticoid receptor gene in hippocampus tissue from suicide victims with a history of childhood abuse. Interestingly, Shalev et al.60 recently reported stress-related accelerated telomere erosion already in childhood; compared with their counterparts, children who experienced two or more kinds of violence exposure showed significantly more telomere erosion. The authors suggest that these effects are mediated by oxidative stress. Heim et al.61 proposed that many of the biological changes thought to be characteristic of MDD might, in fact, be secondary to early-life trauma and represent the risk of developing MDD. Moreover, Nanni et al.1 revealed that childhood maltreatment was associated with lack of response (or remission) during treatment for MDD. Hypothetically, TCEs disrupt the physiological response to stress, the overactivation of which may lead to detrimental consequences in stress-sensitive systems, namely the nervous, immune, metabolic and endocrine systems.61, 62 The resulting cumulative biological ‘weight' might determine poor prognosis in terms of recurrences in MDD. However, thus far, prospective studies in recurrent MDD were lacking.
The observed gene–environment interaction is of clinical importance, as the burden of MDD is mainly because of its lifelong recurrent nature.63 The T− and TCE− patient groups remained on average recurrence free for 1.85 years longer than the T+ and TCE+ patient groups. This suggests that MDD patients with a childhood trauma history and carriers of the thermolabile variant of the MTHFR gene constitute a subgroup of patients who may particularly require tailored interventions. Those interventions have to combat both MDD recurrence and the consequences of childhood trauma.1, 64, 65 The gene–environment interaction in two independent samples suggests benefit from the integration of two types of therapeutic approaches: on one hand, psychotherapeutic interventions specifically aimed at the consequences of TCEs (including psychotherapeutic treatment of trauma-related problems) that, on the other hand, could be combined with interventions aimed at the 1-C cycle; (oxidative) stress may be corrected by improving antioxidant defenses through dietary modification and (add-on) exercise.66 These interventions should be investigated further with randomized controlled trials in specific high-risk groups.
The limitations of our study include the assessment of TCEs with a self-report questionnaire rather than an interview. Those questionnaires may be subject to recall bias through the effects of depressive symptomatology, and therefore the validity of such an approach may be reduced.38 However, this effect may be limited in the discovery sample because at baseline all participants were euthymic. Moreover, in the replication sample, all individuals were healthy. Furthermore, other constructs of TCEs (such as parental neglect, bullying) than those represented in the used questionnaire could play a role. In addition, the questionnaire provides no information regarding the specific timeframe in which the TCEs took place and how prolonged they were. It could be that the effect of TCEs is modified by these time-dependent factors. Another limitation in the discovery sample is the possibility of selection bias because the final sample contained 124 patients of the 172 patients from the original trial. We lost 8.7% to follow-up and 19.2% to a diversity of reasons (for example, genotyping failure, being afraid of needles, ethical issues concerning genetic study). However, the patients of the final sample did not differ on the main clinical variables from those excluded from the analyses. This makes it unlikely that this selection of 124 patients out of the original sample induced any additional selection bias. Similarly, in the replication sample, we cannot exclude that recruitment strategies have resulted in a sample that is not completely representative of the general population with regard to age and educational level, and therefore we cannot be sure that the findings in the replication sample can be generalized to the general population.
In spite of these limitations, our study is unique in providing the opportunity to investigate the role of the interaction between genes and environment on prospectively assessed recurrence over 5.5 years. In addition, this was investigated in a specific sample of highly recurrent depressed patients, which can be considered characteristic for those patients particularly causing the large MDD-associated burden of disease.63 By including specific recurrently depressed patients, we were able to investigate a clinically highly relevant sample. Our replication of the interaction in a population sample supports the robustness of our findings and suggests that this genetic vulnerability is relevant in the broader context of depression.
In summary, the results of the present study indicate that an interaction between MTHFR C677T and TCEs increased risk of recurrence in recurrent MDD patients over 5.5 years of follow-up and is associated with depressive symptoms in the general population. More attention to specific at-risk individuals, that is, patients who experienced TCEs and genetic alterations, including MTHFR C677T, could help to improve treatment strategies to prevent depression and recurrences. However, the exact nature of the connection between MTHFR C677T, TCEs and the course of recurrence in MDD remains to be clarified. Future, preferably prospective, studies are warranted to replicate these findings.
Acknowledgments
This study has been made possible because of financial aid of The Netherlands Foundation for Mental Health, Utrecht, and the Health Research Development Council, Department Prevention Program (ZONMw). The replication study was supported by a grant of NWO, the Dutch council for scientific research (ZonMW TOP Grant no. 91207039). Funders had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review or approval of the manuscript. We are most grateful to the participants of our study. In addition, we express our appreciation to the participating psychiatric sites for their recruitment efforts. We also thank our interviewers and independent raters and specifically Irene Visch for assistance with data management and support. The following colleagues contributed to the DELTA (Depression Evaluation Longitudinal Therapy Assessment) Study: Mascha ten Doesschate, Jochanan Huyser, Guido Nabarro, Philip Spinhoven, Ellie Wekking and Luuk Wouters. We also thank Chris Schubart and Willemijn van Gastel for their input in the replication sample. The Clinical Trial registration for this work isISRCTN 68246470 http://www.controlled-trials.com/ISRCTN68246470/bockting.
The authors declare no conflict of interest. AL had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. Am J Psychiatry. 2012;169:141–151. doi: 10.1176/appi.ajp.2011.11020335. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997;349:1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- Ormel J, Oldehinkel AJ, Brilman EI. The interplay and etiological continuity of neuroticism, difficulties, and life events in the etiology of major and subsyndromal, first and recurrent depressive episodes in later life. Am J Psychiatry. 2001;158:885–891. doi: 10.1176/appi.ajp.158.6.885. [DOI] [PubMed] [Google Scholar]
- Crown WH, Finkelstein S, Berndt ER, Ling D, Poret AW, Rush AJ, Russell JM. The impact of treatment-resistant depression on health care utilization and costs. J Clin Psychiatry. 2002;63:963–971. doi: 10.4088/jcp.v63n1102. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Harkness KL. Recurrence in major depression: a conceptual analysis. Psychol Rev. 2011;118:655–674. doi: 10.1037/a0025190. [DOI] [PubMed] [Google Scholar]
- Burcusa SL, Iacono WG. Risk for recurrence in depression. Clin Psychol Rev. 2007;27:959–985. doi: 10.1016/j.cpr.2007.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Prescott CA. Clinical characteristics of major depression that predict risk of depression in relatives. Arch Gen Psychiatry. 1999;56:322–327. doi: 10.1001/archpsyc.56.4.322. [DOI] [PubMed] [Google Scholar]
- Modell S, Lauer CJ, Schreiber W, Huber J, Krieg JC, Holsboer F. Hormonal response pattern in the combined DEX-CRH test is stable over time in subjects at high familial risk for affective disorders. Neuropsychopharmacology. 1998;18:253–262. doi: 10.1016/S0893-133X(97)00144-9. [DOI] [PubMed] [Google Scholar]
- Holsboer F. The corticosteroid receptor hypothesis of depression. Neuropsychopharmacology. 2000;23:477–501. doi: 10.1016/S0893-133X(00)00159-7. [DOI] [PubMed] [Google Scholar]
- Nemeroff CB, Vale WW. The neurobiology of depression: inroads to treatment and new drug discovery. J Clin Psychiatry. 2005;66:5–13. [PubMed] [Google Scholar]
- Assies J, Pouwer F, Lok A, Mocking RJT, Bockting CLH, Visser I, Abeling NG, Duran M, Schene AH. Plasma and erythrocyte fatty acid patterns in patients with recurrent depression: a matched case-control study. PLoS One. 2010;5:e10635. doi: 10.1371/journal.pone.0010635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lok A, Mocking RJ, Ruhe HG, Visser I, Koeter MW, Assies J, Bockting CL, Olff M, Schene AH. Longitudinal hypothalamic-pituitary-adrenal axis trait and state effects in recurrent depression. Psychoneuroendocrinology. 2012;37:892–902. doi: 10.1016/j.psyneuen.2011.10.005. [DOI] [PubMed] [Google Scholar]
- Uher R, Caspi A, Houts R, Sugden K, Williams B, Poulton R, Moffitt TE. Serotonin transporter gene moderates childhood maltreatment's effects on persistent but not single-episode depression: replications and implications for resolving inconsistent results. J Affect Disord. 2011;135:56–65. doi: 10.1016/j.jad.2011.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kupfer DJ, Frank E, Phillips ML. Major depressive disorder: new clinical, neurobiological, and treatment perspectives. Lancet. 2012;379:1045–1055. doi: 10.1016/S0140-6736(11)60602-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjelland I, Tell GS, Vollset SE, Refsum H, Ueland PM. Folate vitamin B12, homocysteine, and the MTHFR 677C->T polymorphism in anxiety and depression: the Hordaland Homocysteine Study. Arch Gen Psychiatry. 2003;60:618–626. doi: 10.1001/archpsyc.60.6.618. [DOI] [PubMed] [Google Scholar]
- Elkins JS, Johnston SC, Ziv E, Kado D, Cauley JA, Yaffe K. Methylenetetrahydrofolate reductase C677T polymorphism and cognitive function in older women. Am J Epidemiol. 2007;166:672–678. doi: 10.1093/aje/kwm140. [DOI] [PubMed] [Google Scholar]
- Sugden C. One-carbon metabolism in psychiatric illness. Nutr Res Rev. 2006;19:117–136. doi: 10.1079/NRR2006119. [DOI] [PubMed] [Google Scholar]
- Hoffman M. Hypothesis: hyperhomocysteinemia is an indicator of oxidant stress. Med Hypotheses. 2011;77:1088–1093. doi: 10.1016/j.mehy.2011.09.009. [DOI] [PubMed] [Google Scholar]
- Castro R, Rivera I, Ravasco P, Camilo ME, Jakobs C, Blom HJ, de Almeida IT. 5,10-methylenetetrahydrofolate reductase (MTHFR) 677C-->T and 1298A-->C mutations are associated with DNA hypomethylation. J Med Genet. 2004;41:454–458. doi: 10.1136/jmg.2003.017244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frankenburg FR. The role of one-carbon metabolism in schizophrenia and depression. Harv Rev Psychiatry. 2007;15:146–160. doi: 10.1080/10673220701551136. [DOI] [PubMed] [Google Scholar]
- Tchantchou F. Homocysteine metabolism and various consequences of folate deficiency. J Alzheimers Dis. 2006;9:421–427. doi: 10.3233/jad-2006-9408. [DOI] [PubMed] [Google Scholar]
- Zintzaras E. C677T and A1298C methylenetetrahydrofolate reductase gene polymorphisms in schizophrenia, bipolar disorder and depression: a meta-analysis of genetic association studies. Psychiatr Genet. 2006;16:105–115. doi: 10.1097/01.ypg.0000199444.77291.e2. [DOI] [PubMed] [Google Scholar]
- Gilbody S, Lewis S, Lightfoot T. Methylenetetrahydrofolate reductase (MTHFR) genetic polymorphisms and psychiatric disorders: a HuGE review. Am J Epidemiol. 2007;165:1–13. doi: 10.1093/aje/kwj347. [DOI] [PubMed] [Google Scholar]
- López-León S, Janssens AC, González-Zuloeta Ladd AM, Del-Favero J, Claes SJ, Oostra BA, van Duijn CM. Meta-analyses of genetic studies on major depressive disorder. Mol Psychiatry. 2008;13:772–785. doi: 10.1038/sj.mp.4002088. [DOI] [PubMed] [Google Scholar]
- Gaysina D, Cohen S, Craddock N, Farmer A, Hoda F, Korszun A, Owen MJ, Craig IW, McGuffin P. No association with the 5,10-methylenetetrahydrofolate reductase gene and major depressive disorder: results of the depression case control (DeCC) study and a meta-analysis. Am J Med Genet B Neuropsychiatr Genet. 2008;147:699–706. doi: 10.1002/ajmg.b.30665. [DOI] [PubMed] [Google Scholar]
- Peerbooms OL, van Os J, Drukker M, Kenis G, Hoogveld L, MTHFR in Psychiatry Group. de Hert M, Delespaul P, van Winkel R, Rutten BP. Meta-analysis of MTHFR gene variants in schizophrenia, bipolar disorder and unipolar depressive disorder: evidence for a common genetic vulnerability. Brain Behav Immun. 2011;25:1530–1543. doi: 10.1016/j.bbi.2010.12.006. [DOI] [PubMed] [Google Scholar]
- Heim C, Binder EB. Current research trends in early life stress and depression: review of human studies on sensitive periods, gene-environment interactions, and epigenetics. Exp Neurol. 2012;233:102–111. doi: 10.1016/j.expneurol.2011.10.032. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The effects of stressful life events on depression. Ann Rev Psychol. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Thornton LM, Gardner CO. Genetic risk, number of previous depressive episodes, and stressful life events in predicting onset of major depression. Am J Psychiatry. 2001;158:582–586. doi: 10.1176/appi.ajp.158.4.582. [DOI] [PubMed] [Google Scholar]
- Bockting CLH, Spinhoven P, Koeter MWJ, Wouters LF, Schene AH, Depression Evaluation Longitudinal Therapy Assessment Study Group Prediction of recurrence in recurrent depression and the influence of consecutive episodes on vulnerability for depression: a 2-year prospective study. J Clin Psychiatry. 2006;67:747–755. [PubMed] [Google Scholar]
- Ten Doesschate MC, Bockting CLH, Koeter MWJ, Schene AH. Prediction of recurrence in recurrent depression: a 5.5-year prospective study. J Clin Psychiatry. 2010;71:984–991. doi: 10.4088/JCP.08m04858blu. [DOI] [PubMed] [Google Scholar]
- Hardeveld F, Spijker J, De Graaf R, Nolen WA, Beekman AFT. Recurrence of major depressive disorder and its predictors in the general population: results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS) Psychol Med. 2012;31:1–10. doi: 10.1017/S0033291712002395. [DOI] [PubMed] [Google Scholar]
- Farmer AE, McGuffin P. Humiliation, loss and other types of life events and difficulties: a comparison of depressed subjects, healthy controls and their siblings. Psychol Med. 2003;33:1169–1175. doi: 10.1017/s0033291703008419. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Kuhn JW, Prescott CA. Childhood sexual abuse, stressful life events and risk for major depression in women. Psychol Med. 2004;34:1475–1482. doi: 10.1017/s003329170400265x. [DOI] [PubMed] [Google Scholar]
- Murgatroyd C, Wu Y, Bockmühl Y, Spengler D. Genes learn from stress: how infantile trauma programs us for depression. Epigenetics. 2010;5:194–199. doi: 10.4161/epi.5.3.11375. [DOI] [PubMed] [Google Scholar]
- Nugent NR, Tyrka AR, Carpenter LL, Price LH. Gene-environment interactions: early life stress and risk for depressive and anxiety disorders. Psychopharmacology (Berl) 2011;214:175–196. doi: 10.1007/s00213-010-2151-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karg K, Burmeister M, Shedden K, Sen S. The serotonin transporter promoter variant (5-HTTLPR), stress, and depression meta-analysis revisited: evidence of genetic moderation. Arch Gen Psychiatry. 2011;68:444–454. doi: 10.1001/archgenpsychiatry.2010.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labonté B, Suderman M, Maussion G, Navaro L, Yerko V, Mahar I, Bureau A, Mechawar N, Szyf M, Meaney MJ, Turecki G. Genome-wide epigenetic regulation by early-life trauma. Arch Gen Psychiatry. 2012;69:722–731. doi: 10.1001/archgenpsychiatry.2011.2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bockting CL, Schene AH, Spinhoven P, Koeter MW, Wouters LF, Huyser J, Kamphuis JH. Preventing relapse/recurrence in recurrent depression with cognitive therapy: a randomized controlled trial. J Consult Clin Psychol. 2005;73:647–657. doi: 10.1037/0022-006X.73.4.647. [DOI] [PubMed] [Google Scholar]
- Bockting CL, Spinhoven P, Wouters LF, Koeter MW, Schene AH, DELTA Study Group Long-term effects of preventive cognitive therapy in recurrent depression: a 5.5-year follow-up study. J Clin Psychiatry. 2009;70:1621–1628. doi: 10.4088/JCP.08m04784blu. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JB. User Guide for the Structured Clinical Interview for DSM-IV Axis 1 Disorders. American Psychiatric Association: Washington, DC; 1996. [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:6–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubart CD, van Gastel WA, Breetvelt EJ, Beetz SL, Ophoff RA, Sommer IE, Kahn RS, Boks MP. Cannabis use at a young age is associated with psychotic experiences. Psychol Med. 2010. pp. 1–10. [DOI] [PubMed]
- Boks MP, Schipper M, Schubart CD, Sommer IE, Kahn RS, Ophoff RA. Investigating gene environment interaction in complex diseases: increasing power by selective sampling for environmental exposure. Int J Epidemiol. 2007;36:1363–1369. doi: 10.1093/ije/dym215. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59 (Suppl 20:22–33. [PubMed] [Google Scholar]
- Compton WM.Advantages of the CIDI family of instruments in epidemiological research of substance use disorders Int J Methods Psychiatr Res 1993. Special Issue: The WHO Composite International Diagnostic Interview3109–119. [Google Scholar]
- Bernstein DP, Fink L. Childhood Trauma Questionnaire: A Retrospective Self-Report Manual. The Psychological Corporation: San Antonio, TX; 1998. [Google Scholar]
- Kraaij V, de Wilde EJ. Negative life events and depressive symptoms in the elderly: a life span perspective. Aging Ment Health. 2001;5:84–91. doi: 10.1080/13607860020020681. [DOI] [PubMed] [Google Scholar]
- Kraaij V, Garnefski N, de Wilde EJ, Dijkstra A, Gebhardt W, Maes S. Negative life events and depressive symptoms in late adolescence: bonding and cognitive coping as vulnerability factors. J Youth Adolesc. 2003;32:185–193. [Google Scholar]
- Thombs BD, Bernstein DP, Lobbestael J, Arntz A. A validation study of the Dutch Childhood Trauma Questionnaire-Short Form: factor structure, reliability, and known-groups validity. Child Abuse Negl. 2009;33 (8:518–523. doi: 10.1016/j.chiabu.2009.03.001. [DOI] [PubMed] [Google Scholar]
- Pusch W, Wurmbach JH, Thiele H, Kostrzewa M. MALDI-TOF mass spectrometry-based SNP genotyping. Pharmacogenomics. 2002;3:537–548. doi: 10.1517/14622416.3.4.537. [DOI] [PubMed] [Google Scholar]
- Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, Maller J, Sklar P, de Bakker PI, Daly MJ, Sham PC. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81 (3:559–575. doi: 10.1086/519795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niesink R, Rigter S, Hoek J, den Boer N. THC-concentraties in wiet, nederwiet en hasj in Nederlandse coffeeshops (2008–2009) The Trimbos Institute (Dutch Institute of Mental Health and Addiction): Utrecht, The Netherlands; 2009. [Google Scholar]
- Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG, Boers GJ, den Heijer M, Kluijtmans LA, van den Heuvel LP. A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet. 1995;10:111–113. doi: 10.1038/ng0595-111. [DOI] [PubMed] [Google Scholar]
- Pinheiro J, Bates D, DebRoy S, Sarkar D, Team TRDC nlme: Linear and Nonlinear Mixed Effects Models. R package version. 2012;3:1–105. [Google Scholar]
- Cordell HJ, Clayton DG. Genetic association studies. Lancet. 2005;366:1121–1131. doi: 10.1016/S0140-6736(05)67424-7. [DOI] [PubMed] [Google Scholar]
- Devlin AM, Brain U, Austin J, Oberlander TF. Prenatal exposure to maternal depressed mood and the MTHFR C677T variant affect SLC6A4 methylation in infants at birth. PLoS One. 2010;5:e12201. doi: 10.1371/journal.pone.0012201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan PO, Sasaki A, D'Alessio AC, Dymov S, Labonté B, Szyf M, Turecki G, Meaney MJ. Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nat Neurosci. 2009;12:342–348. doi: 10.1038/nn.2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shalev I, Moffitt TE, Sugden K, Williams B, Houts RM, Danese A, Mill J, Arseneault L, Caspi A. Exposure to violence during childhood is associated with telomere erosion from 5 to 10 years of age: a longitudinal study. Mol Psychiatry. 2013;18:576–581. doi: 10.1038/mp.2012.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heim C, Newport DJ, Mletzko T, Miller AH, Nemeroff CB. The link between childhood trauma and depression: Insights from HPA axis studies in humans. Psychoneuroendocrinology. 2008;33:693–710. doi: 10.1016/j.psyneuen.2008.03.008. [DOI] [PubMed] [Google Scholar]
- Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012;106:29–39. doi: 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- Greden JF. The burden of recurrent depression: causes, consequences, and future prospects. J Clin Psychiatry. 2001;62:5–9. [PubMed] [Google Scholar]
- Nemeroff CB, Heim CM, Thase ME, Klein DN, Rush AJ, Schatzberg AF, et al. Differential responses to psychotherapy versus pharmacotherapy in patients with chronic forms of major depression and childhood trauma. Proc Natl Acad Sci USA. 2003;100:14293–14296. doi: 10.1073/pnas.2336126100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heim C, Shugart M, Craighead WE, Nemeroff CB. Neurobiological and psychiatric consequences of child abuse and neglect. Dev Psychobiol. 2010;52:671–690. doi: 10.1002/dev.20494. [DOI] [PubMed] [Google Scholar]
- Kruisdijk FR, Hendriksen IJ, Tak EC, Beekman AT, Hopman-Rock M. Effect of running therapy on depression (EFFORT-D). Design of a randomised controlled trial in adult patients [ISRCTN 1894] BMC Public Health. 2012;12:50. doi: 10.1186/1471-2458-12-50. [DOI] [PMC free article] [PubMed] [Google Scholar]