Abstract
Objective
To evaluate the effect of simultaneous zinc and vitamin A supplementation on diarrhoea and acute lower respiratory infections in children.
Study design
Randomised double blind placebo controlled trial.
Setting
Urban slums of Dhaka, Bangladesh.
Participants and methods
800 children aged 12-35 months were randomly assigned to one of four intervention groups: 20 mg zinc once daily for 14 days; 200 000 IU vitamin A, single dose on day 14; both zinc and vitamin A; placebo. The children were followed up once a week for six months, and morbidity information was collected.
Results
The incidence and prevalence of diarrhoea were lower in the zinc and vitamin A groups than in the placebo group. Zinc and vitamin A interaction had a rate ratio (95% confidence interval) of 0.79 (0.66 to 0.94) for the prevalence of persistent diarrhoea and 0.80 (0.67 to 0.95) for dysentery. Incidence (1.62; 1.16 to 2.25) and prevalence (2.07; 1.76 to 2.44) of acute lower respiratory infection were significantly higher in the zinc group than in the placebo group. The interaction term had rate ratios of 0.75 (0.46 to 1.20) for incidence and 0.58 (0.46 to 0.73) for prevalence of acute lower respiratory infection.
Conclusions
Combined zinc and vitamin A synergistically reduced the prevalence of persistent diarrhoea and dysentery. Zinc was associated with a significant increase in acute lower respiratory infection, but this adverse effect was reduced by the interaction between zinc and vitamin A.
What is already known on this topic
Trials of vitamin A supplementation have failed to show a beneficial effect on morbidity in children
Experimental studies have shown that, in the presence of zinc deficiency, vitamin A supplementation fails to reverse vitamin A deficiency
Coexistence of deficiencies of zinc and vitamin A could be a reason for the failure of vitamin A supplementation, but data in humans are limited
What this paper adds
Combined zinc and vitamin A supplementation is more effective in reducing persistent diarrhoea and dysentery than either vitamin A or zinc alone
Zinc alone increased respiratory illnesses, but interaction between zinc and vitamin A reduced this adverse effect
Introduction
Trials of vitamin A supplementation have consistently shown a beneficial effect on childhood mortality,1–4 but the effect of vitamin A on morbidity is unclear. In some studies, the incidences of diarrhoea and respiratory infections were reduced with vitamin A supplementation.5,6 Other studies have reported an effect on diarrhoea but no effect on respiratory infection.7,8 Several studies have failed to show that vitamin A supplementation reduces morbidity.9–12 One possible explanation for the inconsistent findings is that multiple nutrient deficiencies affect the bioavailability of vitamin A and thereby prevent its beneficial effect. Among these micronutrient deficiencies, zinc is a likely suspect because of its interaction with vitamin A.13 Experimental studies have shown that serum retinol concentration is reduced in zinc deficient animals, and vitamin A supplementation failed to increase the low serum retinol to a normal concentration.14 However, when the animals were supplemented with zinc, either alone or in combination with vitamin A, the serum retinol concentration increased. In children with severe protein energy malnutrition, zinc supplementation improved serum retinol binding protein and retinol concentration.15 Deficiencies of zinc and vitamin A often coexist in malnourished children, so supplementation with zinc might overcome the failures with vitamin A supplementation observed in several studies.
We hypothesised that combining zinc with vitamin A supplementation would result in improved vitamin A status, reduced morbidity, and increased growth. We report the effect of supplementation with simultaneous zinc and vitamin A on the prevalence of diarrhoea and acute lower respiratory infection in children.
Methods
We carried out a randomised double blind placebo controlled trial in children aged 12-35 months. Children who had received a vitamin A capsule in the previous four months or who were severely malnourished (weight for age <60% of the National Center for Health Statistics median) were excluded. Children were randomised to receive one of four treatments: zinc, vitamin A, both zinc and vitamin A, or placebo. The zinc group received 5 ml (1 teaspoonful) zinc syrup (20 mg elemental zinc) daily for 14 days and a placebo capsule on day 14. The vitamin A group received 5 ml placebo syrup daily for 14 days and a 200 000 IU (60 mg) vitamin A capsule on day 14. The zinc plus vitamin A group received 5 ml zinc syrup daily for 14 days and a 200 000 IU vitamin A capsule on day 14. The placebo group received 5 ml placebo syrup daily for 14 days and a placebo capsule on day 14. The composition of the syrup has been described elsewhere.16 The study was conducted in urban slums of Dhaka, Bangladesh, during October 1997 to May 1998. The study was approved by the ethical review committee of the International Centre for Diarrhoeal Disease Research, Bangladesh, and the committee of human research of the University of Alabama at Birmingham, Alabama, USA.
Sample size—To detect a 25% reduction in morbidity with combined zinc and vitamin A at 5% level of significance with a power of 90% and an expected loss to follow up of 20%, our calculated sample size was 800.
Supplementation procedure—Each child was fed a teaspoon of syrup daily for 14 days and one capsule on day 14. The health assistant visited the child at home on day 7 and day 14 and measured the amount of syrup taken by subtracting the remaining volume from 50 ml. Mothers were also asked about any problems encountered during feeding the syrup.
Outcome variables—The outcome variables were diarrhoea and acute lower respiratory infection.
Morbidity follow up—For a period of six months, the health assistant visited the child at home every seven days. During the visits the mother was asked about her child's illness, and each sign or symptom was recorded. The health assistant recorded the child's body temperature and counted the respiratory rate if the child had fever.
Outcome definitions—Diarrhoea was defined as the passage of three or more watery or liquid stools in 24 hours or the presence of blood in the stools. Three consecutive days free from disease were regarded as resolution of previous diarrhoeal illness. Persistent diarrhoea was defined as any diarrhoea that lasted for at least 14 consecutive days. Dysentery was defined as the presence of blood and mucus in the stools. Acute lower respiratory infection was defined as the presence of cough, difficult or rapid breathing, and fever. Chest retraction was added to these symptoms to define severe lower respiratory infection. Seven consecutive days free from disease were regarded as resolution of previous respiratory illness.
Analytical methods—Data analysis was performed by using SPSS version 8.0 (SPSS Inc, Chicago, IL) and SAS version 6.1 (SAS Inc, Cary, NC). Poisson regression was performed to calculate the rate ratios and 95% confidence intervals. To calculate the incidence rate, the number of episodes was modelled as the dependent variable by using the event-trials options (total episodes as event and days at risk as trials) with group assignment as the independent variable. Number of days at risk was defined as the number of observed days minus the number of days with illness minus the days (gaps) between episodes of illness.To calculate the prevalence rates, the number of days with illness was modelled as the dependent variable (days as events and days of observation as trials) with group as the independent variable. To examine the interaction between zinc and vitamin A, the interaction term (for example, zinc*vitamin A) was added into the model. The analysis was done in a factorial design, and comparisons were made between groups containing zinc versus placebo, groups containing vitamin A versus placebo, and interaction term versus placebo.
Assignment—Sets of two bottles of syrup and a capsule were serially numbered according to the randomisation list and corresponding to the study serial numbers. The enrolled children were assigned the numbered bottles in the order in which they were enrolled.
Masking—The zinc and placebo syrups were supplied in bottles that looked identical, and the appearance and consistency of the syrups were similar. Vitamin A and placebo capsules were identical in appearance. The randomisation code was kept sealed until the completion of the study. The treatment allocations were disclosed after the final analysis.
Results
Flow and follow up of participants
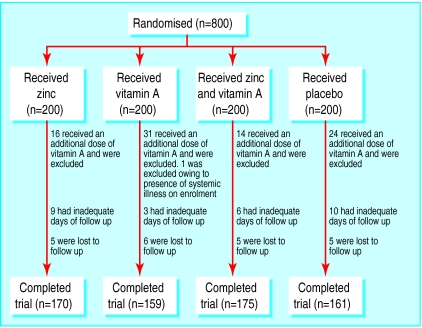
Eight hundred children were enrolled (200 in each group) (figure). However, 135 (17%) were excluded from the study or dropped out. Of these 135 children, 85 (11% of total) were excluded because they had received vitamin A after enrolment during the “National vitamin A week” campaign in Bangladesh. Forty nine (6%) children were lost to follow up or had fewer than 90 days of observation period, and one child was excluded owing to complicated illness. The baseline characteristics of the children who were excluded or lost to follow up were comparable to those of the children who continued in the study. The final analysis included 665 children: 170 in the zinc group, 159 in the vitamin A group, 175 in the zinc and vitamin A group, and 161 in the placebo group.
Analysis
Baseline characteristics were comparable among the four groups (table 1). Ninety two per cent of the mothers reported having no problems feeding the syrup, 5% of mothers had to forcibly feed it to their children as they usually did not want to take any medicine, and 3% of the children vomited once or twice during the 14 day supplementation period. The mean intake of syrup was 72.4 (SD 16.5) ml and >90% children had an intake of at least 50 ml. Compliance did not differ between groups receiving zinc and groups not receiving zinc.
Table 1.
Characteristics of children at entry. Values are numbers (percentages) unless stated otherwise
| Zinc (n=170) | Vitamin A (n=159) | Zinc plus vitamin A (n=175) | Placebo (n=161) | |
|---|---|---|---|---|
| Age (months): | ||||
| 12-23 | 84 (49) | 66 (42) | 89 (51) | 82 (51) |
| 24-35 | 86 (51) | 94 (59) | 86 (49) | 79 (49) |
| Mean (SD) | 23.6 (7.0) | 24.2 (7.3) | 23.5 (7.5) | 23.6 (7.5) |
| Sex: | ||||
| Male | 91 (54) | 89 (56) | 98 (56) | 76 (47) |
| Female | 79 (47) | 71 (45) | 77 (44) | 85 (53) |
| Weight for age Z score: | ||||
| <−2.0 | 111 (65) | 103 (65) | 119 (68) | 105 (65) |
| ⩾−2.0 | 59 (35) | 57 (36) | 56 (32) | 56 (35) |
| Mean (SD) | −2.3 (0.9) | −2.3 (0.33) | −2.4 (0.8) | −2.3 (0.9) |
| Continued breast feeding | 121 (71) | 104 (65) | 131 (75) | 112 (70) |
| Median (range) family income ($/month) | 62 (16-289) | 62 (25-247) | 62 (21-227) | 62 (10-268) |
Table 2 shows a small but significant reduction in the incidence and prevalence of diarrhoea (acute and persistent) in the zinc and vitamin A groups compared with the placebo group. However, there was no interaction effect between zinc and vitamin A in reducing diarrhoea. Persistent diarrhoea was significantly less prevalent in the zinc group than in the placebo group. Vitamin A alone did not have a significant effect on persistent diarrhoea, but the reduction of persistent diarrhoea by zinc was augmented by vitamin A. Zinc and vitamin A in combination reduced dysentery, although neither nutrient did so by itself.
Table 2.
Effect of supplementation with zinc, vitamin A, or both on diarrhoea and dysentery
| Intervention groups | Incidence*
|
Prevalence†
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Episodes | Person years at risk | Incidence* | Rate ratio (95% CI) | Days with illness | Person years | Prevalence† | Rate ratio (95% CI) | ||
| Diarrhoea (all types) | |||||||||
| Zinc (n=345) | 1142 | 48 867 | 8.5 | 0.89 (0.79 to 0.99) | 4980 | 56 322 | 32.3 | 0.82 (0.78 to 0.87) | |
| Vitamin A (n=334) | 1087 | 47 247 | 8.4 | 0.84 (0.74 to 0.94) | 5013 | 54 727 | 33.4 | 0.89 (0.84 to 0.94) | |
| Placebo (n=161) | 616 | 21 989 | 10.2 | 1.0 | 2828 | 26 215 | 39.4 | 1.0 | |
| Interaction of zinc and vitamin A | 1.07 (0.91 to 1.27) | 1.08 (0.99 to 1.17) | |||||||
| Persistent diarrhoea | |||||||||
| Zinc (n=345) | 46 | 55 442 | 0.30 | 0.81 (0.47 to 1.40) | 871 | 56 322 | 5.6 | 0.81 (0.72 to 0.92) | |
| Vitamin A (n=334) | 52 | 53 724 | 0.35 | 1.08 (0.65 to 1.81) | 985 | 54 727 | 6.6 | 1.08 (0.96 to 1.22) | |
| Placebo (n=161) | 28 | 25 656 | 0.40 | 1.0 | 535 | 26 215 | 7.4 | 1.0 | |
| Interaction of zinc and vitamin A | 0.82 (0.38 to 1.77) | 0.79 (0.66 to 0.94) | |||||||
| Dysentery | |||||||||
| Zinc (n=345) | 155 | 55 045 | 1.03 | 1.19 (0.87 to 1.62) | 1151 | 56 322 | 7.46 | 1.17 (1.04 to 1.32) | |
| Vitamin A (n=334) | 139 | 53 608 | 0.95 | 1.03 (0.75 to 1.43) | 1002 | 54 727 | 6.68 | 0.95 (0.84 to 1.08) | |
| Placebo (n=161) | 72 | 25 608 | 1.03 | 1.0 | 535 | 26 215 | 7.28 | 1.0 | |
| Interaction of zinc and vitamin A | 0.67 (0.42 to 1.05) | 0.80 (0.67 to 0.95) | |||||||
Episodes per child year.
Days per child year.
Table 3 shows the incidence and prevalence acute lower respiratory infection in the four intervention groups. Compared with the placebo group, the zinc group had a 62% increase in incidence and a twofold increase in prevalence of acute lower respiratory infection. The incidence of acute lower respiratory infection in the vitamin A group did not differ significantly from that in the placebo group, but the prevalence of acute lower respiratory infection tended to be higher (by 20%). The interaction effect between zinc and vitamin A reduced the adverse effect of zinc on both incidence and prevalence of acute lower respiratory infection, but the effect was significant only for prevalence. There was a twofold increase in the incidence and prevalence of severe acute lower respiratory infection in the zinc group compared with the placebo group.
Table 3.
Effect of supplementation with zinc, vitamin A, or both on acute lower respiratory infection and severe acute lower respiratory infection
| Intervention groups | Incidence*
|
Prevalence†
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Episodes | Person years at risk | Incidence* | Rate ratio (95% CI) | Days with illness | Person years | Prevalence† | Rate ratio (95% CI) | ||
| Acute lower respiratory infection | |||||||||
| Zinc (n=345) | 172 | 55 003 | 1.14 | 1.62 (1.16 to 2.25) | 787 | 56 322 | 5.10 | 2.07 (1.76 to 2.44) | |
| Vitamin A (n=334) | 137 | 53 762 | 0.93 | 1.06 (0.74 to 1.53) | 580 | 54 727 | 3.87 | 1.20 (0.99 to 1.45) | |
| Placebo (n=161) | 56 | 25 836 | 0.79 | 1.0 | 211 | 26 215 | 2.94 | 1.0 | |
| Interaction of zinc and vitamin A | 0.75 (0.46 to 1.20) | 0.58 (0.46 to 0.73) | |||||||
| Severe acute lower respiratory infection | |||||||||
| Zinc (n=345) | 90 | 55 993 | 0.59 | 2.03 (1.24 to 3.33) | 329 | 56 322 | 2.13 | 2.06 (1.60 to 2.64) | |
| Vitamin A (n=334) | 69 | 54 495 | 0.46 | 1.23 (0.71 to 2.13) | 232 | 54 727 | 1.55 | 1.22 (0.84 to 1.48) | |
| Placebo (n=161) | 23 | 26 123 | 0.32 | 1.0 | 92 | 26 215 | 1.28 | 1.0 | |
| Interaction of zinc and vitamin A | 0.66 (0.33 to 1.31) | 0.56 (0.39 to 0.80) | |||||||
Episodes per child year.
Days per child year.
Discussion
This study shows that zinc and vitamin A in combination are more effective than either vitamin A or zinc alone in reducing persistent diarrhoea and dysentery. Our earlier report from the same cohort showed that vitamin A alone failed to reverse vitamin A deficiency, as determined by measurement of vitamin A concentrations, but that combined zinc and vitamin A supplementation successfully reversed this deficiency.16 This improved vitamin A status in the children supplemented with both zinc and vitamin A indicates the existence of a biological interaction between zinc and vitamin A and may explain the reduction of diarrhoea.13
Faruque et al recently reported that zinc reduced the proportion of children with acute diarrhoea who went on to have prolonged episodes, but no additional benefit was observed in children given combined zinc and vitamin A.17 The study, however, did not follow the children to examine whether supplementation reduced the subsequent incidence and prevalence of diarrhoea. Sazawal et alreported a significant reduction in the incidence and prevalence of acute and persistent diarrhoea with zinc supplementation in Indian children.18,19 However, children in the study also received multivitamins, including vitamin A and zinc. The beneficial effect in the Indian studies could be the result of a synergistic effect between zinc and the vitamin A contained in the multivitamin supplement. The findings may therefore be consistent with ours.
The beneficial effect of vitamin A supplementation on diarrhoea, but not on acute lower respiratory infection, in the present study is consistent with previous reports from India and Brazil.7,8 Both studies found a significant reduction in the severity of diarrhoea with vitamin A supplementation but no effect on acute lower respiratory infection. Rather, in the Indian study, children younger than 23 months given a vitamin A supplement had a 42% increase in the prevalence of acute lower respiratory infection,7 which is consistent with our findings. Studies from Haiti, Peru, and Ecuador reported an adverse effect of vitamin A on pneumonia.20–22 This adverse effect has been explained by the ability of high doses of vitamin A to enhance immunity that increases the inflammatory response in the lungs.21
In the present study, although zinc reduced diarrhoea, it increased respiratory illness. These findings are consistent with the study by Ruel et al, who showed an adverse effect of zinc supplementation on respiratory infection and a beneficial effect on diarrhoea.23 In their study, Ruel et al found that both the incidence and the prevalence of respiratory infection were higher in children who received zinc supplementation, although the differences were not statistically significant, presumably because of a small sample size. The increase in acute lower respiratory infection with zinc supplementation could be explained by experimental studies showing that zinc enhances microbial function, growth, and virulence.24 Another explanation is that, although zinc has been shown to improve immune status, not all the components of immunity are positively influenced by zinc. Zinc has been shown to inhibit some functions of polymorphonuclear leucocytes,25 to inhibit alveolar macrophage activity, and to facilitate pulmonary tissue injury.26 Schlesinger et al have shown that zinc supplementation inhibits phagocytic and fungicidal activity in malnourished infants.27 A recent study in Bangladesh showed that severely malnourished children who received daily supplements of 6 mg/kg zinc for 30 days had significantly higher mortality than children who received 1.5 mg/kg zinc.28 Most of these deaths were related to sepsis, which supports the possibility of an effect of zinc on bacterial proliferation.
The contrasting effect of zinc on diarrhoea and acute lower respiratory infection is a public health concern, because zinc supplementation is carried out in many nutrition rehabilitation units. We do not, however, know whether a lower dose of zinc would have had a beneficial effect on acute lower respiratory infection. Further studies are therefore warranted. The adverse effect of zinc supplementation on acute lower respiratory infection should also be weighed against the beneficial effect of zinc in reducing diarrhoea. In the present cohort of children, 104 episodes of diarrhoea per 100 children were prevented per year with zinc supplementation, whereas only 30 episodes of acute lower respiratory infection per 100 children were attributed to zinc supplementation (data not shown). Finally, the finding also suggests that the interaction between vitamin A and zinc reduces the adverse effect of zinc on acute lower respiratory infection and supports combined supplementation.
Figure.
Flow of participants, withdrawals, and completion of follow up
Footnotes
Funding: Thrasher Research Fund.
Competing interests: None declared.
References
- 1.Sommer A, Tarwotjo I, Djunaedi E, West KP, Jr, Loeden AA, Tilden R, et al. Impact of vitamin A supplementation on childhood mortality. A randomized controlled community trial. Lancet. 1986;1:1169–1173. doi: 10.1016/s0140-6736(86)91157-8. [DOI] [PubMed] [Google Scholar]
- 2.Rahmathullah L, Underwood BA, Thulasiraj RD, Milton RC, Ramaswamy K, Rahmathullah R, et al. Reduced mortality among children in southern India receiving a small weekly dose of vitamin A. N Engl J Med. 1990;323:929–935. doi: 10.1056/NEJM199010043231401. [DOI] [PubMed] [Google Scholar]
- 3.Fawzi WW, Chalmers TC, Herrera MG, Mosteller F. Vitamin A supplementation and child mortality. A meta-analysis. JAMA. 1993;269:898–903. [PubMed] [Google Scholar]
- 4.West KP, Jr, Pokhrel RP, Katz J, LeClerq SC, Khatry SK, Shrestha SR, et al. Efficacy of vitamin A in reducing preschool child mortality in Nepal. Lancet. 1991;338:67–71. doi: 10.1016/0140-6736(91)90070-6. [DOI] [PubMed] [Google Scholar]
- 5.Lie C, Ying C, Wang EL, Brun T, Geissler C. Impact of large-dose vitamin A supplementation on childhood diarrhoea, respiratory disease and growth. Eur J Clin Nutr. 1993;47:88–96. [PubMed] [Google Scholar]
- 6.Ghana VAST Study Team. Vitamin A supplementation in northern Ghana: effects on clinic attendances, hospital admissions, and child mortality. Lancet. 1993;342:7–12. [PubMed] [Google Scholar]
- 7.Bhandari N, Bhan MK, Sazawal S. Impact of massive dose of vitamin A given to preschool children with acute diarrhoea on subsequent respiratory and diarrhoeal morbidity. BMJ. 1994;309:1404–1407. doi: 10.1136/bmj.309.6966.1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barreto ML, Santos LM, Assis AM, Araujo MP, Farenzena GG, Santos PA, et al. Effect of vitamin A supplementation on diarrhoea and acute lower-respiratory-tract infections in young children in Brazil. Lancet. 1994;344:228–231. doi: 10.1016/s0140-6736(94)92998-x. [DOI] [PubMed] [Google Scholar]
- 9.Rahmathullah L, Underwood BA, Thulasiraj RD, Milton RC. Diarrhoea, respiratory infections, and growth are not affected by a weekly low-dose vitamin A supplement: a masked, controlled field trial in children in southern India. Am J Clin Nutr. 1991;54:568–577. doi: 10.1093/ajcn/54.3.568. [DOI] [PubMed] [Google Scholar]
- 10.Abdeljaber MH, Monto AS, Tilden RL, Schork MA, Tarwotjo I. The impact of vitamin A supplementation on morbidity: a randomized community intervention trial. Am J Public Health. 1991;81:1654–1656. doi: 10.2105/ajph.81.12.1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramakrishnan U, Latham MC, Abel R, Frongillo EA., Jr Vitamin A supplementation and morbidity among preschool children in south India. Am J Clin Nutr. 1995;61:1295–1303. doi: 10.1093/ajcn/61.6.1295. [DOI] [PubMed] [Google Scholar]
- 12.Dibley MJ, Sadjimin T, Kjolhede CL, Moulton LH. Vitamin A supplementation fails to reduce incidence of acute respiratory illness and diarrhea in preschool-age Indonesian children. J Nutr. 1996;126:434–442. doi: 10.1093/jn/126.2.434. [DOI] [PubMed] [Google Scholar]
- 13.Christian P, West KP., Jr Interactions between zinc and vitamin A: an update. Am J Clin Nutr. 1998;68:435–41S. doi: 10.1093/ajcn/68.2.435S. [DOI] [PubMed] [Google Scholar]
- 14.Smith JC, Jr, McDaniel EG, Fan FF, Halsted JA. Zinc: a trace element essential in vitamin A metabolism. Science. 1973;181:954–955. doi: 10.1126/science.181.4103.954. [DOI] [PubMed] [Google Scholar]
- 15.Shingwekar AG, Mohanram M, Reddy V. Effect of zinc supplementation on plasma levels of vitamin A and retinol-binding protein in malnourished children. Clin Chim Acta. 1979;93:97–100. doi: 10.1016/0009-8981(79)90249-3. [DOI] [PubMed] [Google Scholar]
- 16.Rahman MM, Wahed MA, Fuchs GJ, Baqui AH, Alvarez JO. Synergistic effect of zinc and vitamin A on the biochemical indexes of vitamin A nutrition in children. Am J Clin Nutr 2001 (in press). [DOI] [PubMed]
- 17.Faruque AS, Mahalanabis D, Haque SS, Fuchs GJ, Habte D. Double-blind, randomized, controlled trial of zinc or vitamin A supplementation in young children with acute diarrhoea. Acta Paediatr. 1999;88:154–160. doi: 10.1080/08035259950170312. [DOI] [PubMed] [Google Scholar]
- 18.Sazawal S, Black RE, Bhan MK, Jalla S, Bhandari N, Sinha A, et al. Zinc supplementation reduces the incidence of persistent diarrhea and dysentery among low socioeconomic children in India. J Nutr. 1996;126:443–450. doi: 10.1093/jn/126.2.443. [DOI] [PubMed] [Google Scholar]
- 19.Sazawal S, Black RE, Bhan MK, Jalla S, Sinha A, Bhandari N. Efficacy of zinc supplementation in reducing the incidence and prevalence of acute diarrhea—a community-based, double-blind, controlled trial. Am J Clin Nutr. 1997;66:413–418. doi: 10.1093/ajcn/66.2.413. [DOI] [PubMed] [Google Scholar]
- 20.Stansfield SK, Pierre-Louis M, Lerebours G, Augustin A. Vitamin A supplementation and increased prevalence of childhood diarrhoea and acute respiratory infections. Lancet. 1993;342:578–582. doi: 10.1016/0140-6736(93)91410-n. [DOI] [PubMed] [Google Scholar]
- 21.Stephensen CB, Franchi LM, Hernandez H, Campos M, Gilman RH, Alvarez JO. Adverse effects of high-dose vitamin A supplements in children hospitalized with pneumonia. Pediatrics. 1998;101:E3. doi: 10.1542/peds.101.5.e3. [DOI] [PubMed] [Google Scholar]
- 22.Sempertegui F, Estrella B, Camaniero V, Betancourt V, Izurieta R, Ortiz W, et al. The beneficial effects of weekly low-dose vitamin A supplementation on acute lower respiratory infections and diarrhea in Ecuadorian children. Pediatrics. 1999;104:e1. doi: 10.1542/peds.104.1.e1. [DOI] [PubMed] [Google Scholar]
- 23.Ruel MT, Rivera JA, Santizo MC, Lonnerdal B, Brown KH. Impact of zinc supplementation on morbidity from diarrhea and respiratory infections among rural Guatemalan children. Pediatrics. 1997;99:808–813. doi: 10.1542/peds.99.6.808. [DOI] [PubMed] [Google Scholar]
- 24.Sugarman B. Zinc and infection. Rev Infect Dis. 1983;5:137–147. doi: 10.1093/clinids/5.1.137. [DOI] [PubMed] [Google Scholar]
- 25.Stankova L, Drach GW, Hicks T, Zukoski CF, Chvapil M. Regulation of some functions of granulocytes by zinc of the prostatic fluid and prostate tissue. J Lab Clin Med. 1976;88:640–648. [PubMed] [Google Scholar]
- 26.Mustafa MG, Cross CE, Munn RJ, Hardie JA. Effects of divalent metal ions on alveolar macrophage membrane adenosine triphosphatase activity. J Lab Clin Med. 1971;77:563–571. [PubMed] [Google Scholar]
- 27.Schlesinger L, Arevalo M, Arredondo S, Lonnerdal B, Stekel A. Zinc supplementation impairs monocyte function. Acta Paediatr. 1993;82:734–738. doi: 10.1111/j.1651-2227.1993.tb12548.x. [DOI] [PubMed] [Google Scholar]
- 28.Doherty CP, Sarkar MA, Shakur MS, Ling SC, Elton RA, Cutting WA. Zinc and rehabilitation from severe protein-energy malnutrition: higher-dose regimens are associated with increased mortality. Am J Clin Nutr. 1998;68:742–748. doi: 10.1093/ajcn/68.3.742. [DOI] [PubMed] [Google Scholar]