Abstract
Background:
Tuberculosis (TB) is the most common serious opportunistic infection in HIV positive patients and is the manifestation of AIDS in more than 50% of cases in developing countries. TB can occur at any time during the course of HIV infection.
Aim:
To describe the socio-demographic profile and prevalence of pulmonary tuberculosis (HIV/TB co-infection) among HIV positive patients been attended at the antiretroviral therapy clinic (ART) clinic at tertiary care teaching hospital of western Maharashtra, India.
Materials and Methods:
A cross-sectional study was carried out at the ART clinic of Pravara Rural Hospital, Loni, from June 2011 to May 2012. A total of 1012 HIV positive patients, who attended ART clinic, receiving ART treatment during the study period, were included in the analysis. The statistical analysis was performed using SPSS software (Version 17.0).
Results:
This study showed 1012/172 (17%) prevalence of pulmonary tuberculosis among HIV positive patients, of which 87 (50.58%) were males and 85 (48.42%) were females. Low CD4 count (< 50/μl) had statistically significant association with HIV/TB co-infection as compared to HIV infection only (P < 0.0001).
Conclusion:
The study showed that 17% of HIV infected persons had tuberculosis co-infection. More strategic preventive measures that enhance body immunity among HIV patients are highly needed as early as possible before they develop active tuberculosis.
Keywords: Antiretroviral therapy clinic, HIV infection, Prevalence, Pulmonary tuberculosis
Introduction
India has the largest number of tuberculosis (TB) cases in the world. India shoulders about 14 million cases of TB and it is estimated that about 1.8 million incident cases of TB occur in India every year of which 0.82 million are highly infectious smear positive cases.[1]
TB was declared a global emergency in the year 1993; recently the Director General of WHO declared AIDS to be a global emergency as well. There exists a synergistic relationship between TB and HIV. The interface between TB and HIV is increased in countries like India where both TB and HIV infection are maximally prevalent in people of 15-49 years of age.[2] The association between HIV and tuberculosis present an immediate and grave public health and socioeconomic threat in developing countries.[3]
Persons infected by Tubercle bacilli have about a 10% chance of developing tuberculosis during the remainder of their lives: Thus, they have a less than 0.5% chance of developing overt disease annually,[4] while 10% of persons infected by both TB and HIV develop tuberculosis disease annually.[5] The implication of HIV infection is that it activates dormant tuberculosis to rapid disease progression of tuberculosis and death.[6] In fact, tuberculosis is now the most common opportunistic infection in patients from developing countries who die from AIDS.[7] Reports show that active tuberculosis increases the morbidity and fatality of HIV-infected person and about one-third die of tuberculosis.[5]
The largest increase in tuberculosis has occurred in locations and demographic groups with the highest HIV prevalence, which suggests that the epidemic of HIV is at least partially responsible for the increase of tuberculosis.[8] There is evidence that immune responses in tuberculosis and in other infection induce cytokines that enhance the replication of HIV and this drives the patient into full picture of AIDS.[9] Hence, this study was conducted in order to assess the socio-demographic profile and the prevalence of pulmonary tuberculosis among HIV positive patients who attended the ART clinic at tertiary care teaching hospital of western Maharashtra, India.
Material and Methods
The study was approved by the ethical committee of the institute.
A cross-sectional study was carried out in the ART clinic of Pravara Rural Hospital (PRH), Loni, Maharashtra, India, from June 2011 to May 2012. PRH is a tertiary level health care center attached as a teaching hospital of Rural Medical College, Loni, which caters to the needs of the Ahmednagar district and comes under the aegis of Pravara Medical Trust. A total of 1012 HIV positive patients, who were attended at ART clinic, having < 350/μl CD4 count and receiving ART treatment during study period, were included in the study.
A predesigned and pretested questionnaire was used to collect data on socio-demographic profile. Blood samples of these subjects were tested for HIV infection using highly specific enzyme-linked immunosorbent assay (ELISA) or Western Blot techniques. All the patients, irrespective of whether they had signs and symptoms of chest infection, were screened for pulmonary TB by chest X-ray, and subsequently by repeated microscopic examination of sputum for acid fast bacillus (AFB) using standard technique. Those individuals who were positive for AFB in their sputum received standard directly observed therapy short-course as per revised national tuberculosis control programme of the Government of India.[10] Blood samples were collected periodically after obtaining written informed consent. Blood samples were processed for the CD4 count. Socioeconomic status was assessed by the modified BG Prasad classification.[11]
Statistical analysis
The statistical analysis was performed using SPSS software (Version 17.0). All values are expressed in the form of percentages, mean, and standard deviation and the Chi-square test was applied wherever necessary. Statistical significance was set at P ≤ 0.05.
Results
Socio-demographic characteristics
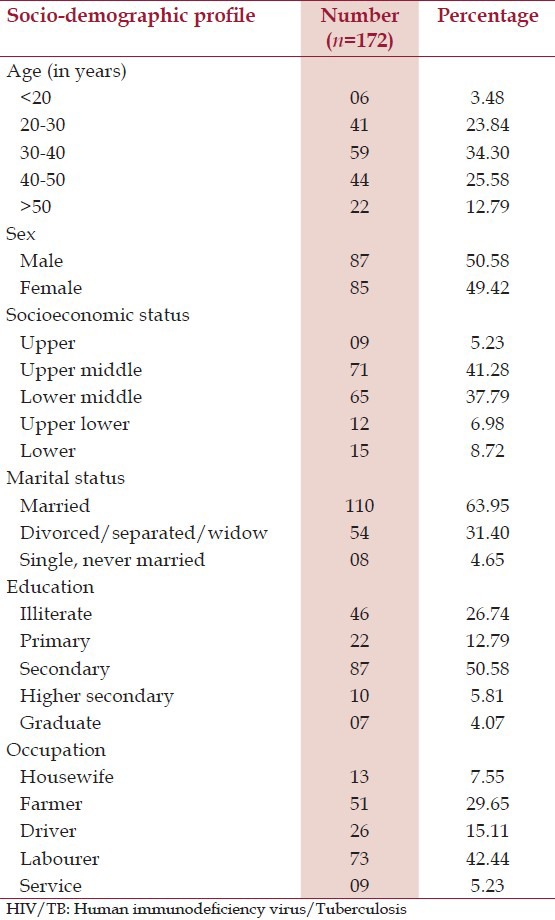
It was observed from Table 1 that, out of the 172 (17%) HIV/TB co-infection patients, 59 (34.30%) were in the age group of 30-40 years, followed by 44 (25.38%) in the age group of 40-50 years, and only 6 (3.40%) in the age group of less than 20 years. The mean age of the patients was 38.1 ± 3.2 years. There were 87 (50.58%) males and 85 (48.42%) females. As per the modified BG Prasad classification, most of the patients 71 (41.28%) belonged to upper middle class followed by 65 (37.79%) lower middle class; while only 9 (5.23%) from upper class. With more than half (63.95%) of the study population were married, while (31.40%) either divorced/widow or separated from their family. Education level of the study population indicated that 46 (26.74%) were illiterates and 87 (50.58%), 22 (12.79%), and 10 (5.81%) had education levels of secondary, primary, and higher secondary, respectively. Only 7 (4.07%) were graduates. Occupation of the study population of HIV/TB co-infection showed that (42.44%) were laborers, followed by (29.65%) was farmers and (15.11%) were driver.
Table 1.
Socio-demographic profile of HIV/TB co-infection patients
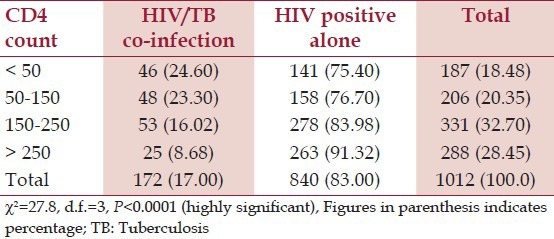
Distribution of CD4 count of HIV and TB cases
Low CD4 count (< 50/μl) had statistically significant association (P < 0.0001) with HIV/TB co-infection as compared to HIV infection only [Table 2].
Table 2.
Distribution of CD4 count of HIV and TB cases
Discussion
In this study, out of the total 1012 HIV positive patients, who attended the ART clinic and received treatment, 172 (17%) had HIV/TB co-infection and remaining 480 (83%) were HIV positive alone. Similarly a study done by Padyana et al.,[12] at a tertiary care hospital of South India, among 200 HIV positive patients, showed that 54 (27%) patients had HIV/TB co-infection and remaining 146 (73%) were HIV positive alone. Another study done by Kebede and Wabe[13] in South West Ethiopia, among 296 patients on concomitant tuberculosis and antiretroviral therapy at hospital treatment center, of them only 24 (8.1%) were co-infected by HIV and TB.
In developing countries, TB is one of the most common life-threatening infections among the persons living with HIV/AIDS. An estimate shows that around 5.1 million people are infected with HIV and about half of these cases are co-infected with tuberculosis.[14] In India, approximately 200 000 of these HIV-infected persons develop active TB each year.[15] Incidence of HIV/TB co-infection was reported to be very high (50%) in sub-Saharan Africa compared to that in Asia.[16] The rates of HIV/TB co-infection have been reported to vary in different regions of India. It was found to be between 0.4% and 20.1% in north India.[17] However, the incidence was 3.2% in 1991, which increased to 20.1% in 1996 in south India.[18]
This study shows that the prevalence of HIV/TB co-infection was 17% among HIV positive patients who attended the ART clinic in western Maharashtra. This prevalence of HIV/TB co-infection is different from the national figure (60.30%),[19] but almost similar (27.3%) to that of another study done by Dev et al.,[20] in Kolkata.
Low CD4 cells in HIV-infected persons indicates severely depressed immunity that makes them susceptible to fresh TB infection or reactivation of latent infection and rapid degradation of clinical condition. It has already been established that TB attributed to a six-fold to seven-fold increase of viral load in HIV positive population.[21] Unlike cryptococcal meningitis or toxoplasmosis, which occur at very low CD4 counts, TB is unique in that it can occur over a wide range of CD4 counts, although it is more frequent at CD4 counts < 300 cells/μl. According to an estimate of World Health Organization, TB has become one of the leading causes of death among HIV-infected persons.[22]
All HIV-infected individuals should be tested for tuberculosis prior to the initiation of ART in countries like India where tuberculosis is endemic. Several tests including chest x-ray and sputum cultures should be done to all individuals. This will result in early detection and treatment, and thus reduction of spread of disease.
Limitations
This study was a hospital-based analysis of the HIV/TB co-infected patients and the findings might not be generalizable. HIV/AIDS pandemic has caused a resurgence of TB, resulting in increased morbidity and mortality in urban as well as rural area. In India, most of the prevalence studies of HIV/TB co-infection were carried out only in the urban area, but very few like present study was carried out in the rural area, highlighted that HIV/TB co-infection is also becoming major health problem in the rural area.
Conclusion
Since the increase in HIV infection rate leads to increase in tuberculosis disease, there is need to re-examine the strategies for their effective control. The development of programs with an integrated approach to inducing behavioral change and promoting use of condoms may reduce the infectivity of HIV transmitters and the susceptibility of HIV-exposed persons. The most important aspect of this control program is public awareness and good health education on how tuberculosis and HIV are transmitted.
Acknowledgments
We express our deep sense of gratitude to the Management, Pravara Medical Trust and The Principal, Rural Medical College Loni, Maharashtra, India. We also acknowledge the help and support of Dr. P. P. Pargaonkar, Medical Officer, and Dr. Mrs. J. J. Deshpande, Co-ordinator ART Clinic and Medical Interns - Dnyaneshwar Kale, Parag Waghmode, and Piyush More.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Vidyanathan PS, Singh S. TB-HIV co-infection in India. NTI Bull. 2003;39:11–8. [Google Scholar]
- 2.Jain SK, Aggarwal JK, Rajpal S, Baveja U. Prevalence of HIV infection among tuberculosis patients in Delhi-A sentinel surveillance study. Indian J Tuberc. 2000;47:21–6. [Google Scholar]
- 3.Stylblo K. The global aspects of tuberculosis and HIV infection. Bull Int Union Tuberc Lung Dis. 1990;65:28–32. [PubMed] [Google Scholar]
- 4.Grange JM. Tuberculosis. In: Husler WJ Jr, Sussman M, editors. Topley and Wilson's Micropbiology and Microbial Infections. 9th ed. Vol. 3. London: Arnold; 1998. pp. 391–417. [Google Scholar]
- 5.Enarson DA, Rieder HL, Arnadottir T, Trebucq A. Management of tuberculosis, a guide for low income Countries. 5th ed. Paris: 2000. International union against tuberculosis and lung disease (IUATLD) Tuberculosis and HIV; pp. 10–53. [Google Scholar]
- 6.Escott S, Nsuteby E, Walley J, Khan A. Management of TB in countries with high HIV prevalence. Afr Health. 2001;23:12–5. [Google Scholar]
- 7.DeCock KM, Sero B, Coulibaly IM, Lucas SB. Tuberculosis and HIV infection is Sub-Sahara Africa. JAMA. 1992;278:1581–7. doi: 10.1001/jama.268.12.1581. [DOI] [PubMed] [Google Scholar]
- 8.Shafer RW. Tuberculosis. In: Broder S, Merigan TC Jr, Bolognesi D, editors. Textbook of AIDS medicine. 2nd ed. Baltimore: Williams and Wilkins (Publisher); 1994. pp. 259–82. [Google Scholar]
- 9.Festenstein F, Grange JM. Tuberculosis and the acquired immune deficiency syndrome. J Appl Bacteriol. 1991;71:19–30. [PubMed] [Google Scholar]
- 10.Global tuberculosis control: Surveillance, planning, financing. WHO Report 2008. WHO/ HTM/TB/2008.393. Geneva: WHO; 2008. World Health Organization; pp. 1–168. [Google Scholar]
- 11.Gupta MC, Mahajan BK. 3rd ed. New Delhi: Jaypee Brothers (Publishers); 2003. The text book of preventive and social medicine; pp. 117–8. [Google Scholar]
- 12.Padyana M, Bhat RV, Dinesha M, Nawaz A. HIV-tuberculosis: A study of chest X-Ray patterns in relation to CD4 count. N Am J Med Sci. 2012;4:221–5. doi: 10.4103/1947-2714.95904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kebede A, Wabe NT. Medication adherence and its determinants among patients on concomitant tuberculosis and antiretroviral therapy in South West Ethiopia. N Am J Med Sci. 2012;4:67–71. doi: 10.4103/1947-2714.93376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Narain JP, Pontali E, Tripathy S. Sentinel surveillance for HIV infection in tuberculosis patients in India. Indian J Tuberc. 2002;49:17–20. [Google Scholar]
- 15.Khatri GR, Frieden TR. Controlling tuberculosis in India. N Eng J Med. 2003;347:1420–5. doi: 10.1056/NEJMsa020098. [DOI] [PubMed] [Google Scholar]
- 16.Kaiser Weekly TB/Malaria Report. HIV/TB co-epidemic rapidly is spreading in sub-Saharan Africa. [Accessed November 2, 2011]. at http://www.globalhealth.kff.org/Daily-Reports/2007/02/dr00048620aspx .
- 17.Sharma SK, Agarwal G, Seth P, Saha PK. Increasing seropositivity among adult tuberculosis patients in Delhi. Indian J Med Res. 2003;117:239–42. [PubMed] [Google Scholar]
- 18.Paranjape RS, Tripathy SP, Menon PA, Mehendale SM, Khatavkar P, Joshi DR. Increasing trend of HIV seroprevalence among pulmonary tuberculosis patients in Pune, India. Indian J Med Res. 1997;106:207–11. [PubMed] [Google Scholar]
- 19.Govt. of India, Ministry of Health and Family. Welfare, National AIDS Control Organisation. National guidelines for clinical management of HIV/AIDS. 2003. [Accessed November 15, 2011]. at http://www.nacoindia.org .
- 20.Dey SK, Pal NK, Chakrabarty MS. Cases of immunodeficiency virus infection and Tuberculosis: Early experience of different aspects. J Indian Med Assoc. 2003;101:291–2. [PubMed] [Google Scholar]
- 21.Nissapatorn V, Christopher L, Init I, Mun Yik F, Abdullah KA. Tuberculosis in AIDS Patients. Malays Med Sci. 2003;10:60–4. [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization. Tuberculosis facts. 2007. [Accessed January 10, 2012]. at http://www.cdc.gov/hiv/resources/factsheets/hivtb.htm .


