Abstract
Background:
Denture fracture is an unresolved problem in complete denture prosthodontics. However, the repaired denture often experiences a refracture at the repaired site due to poor transverse strength. Hence, this study was conducted to evaluate the effect of joint surface contours and glass fiber reinforcement on the transverse strength of repaired acrylic resins.
Materials and Methods:
A total of 135 specimens of heat polymerized polymethyl methacrylate resin of dimensions 64 × 10 × 2.5 mm were fabricated. Fifteen intact specimens served as the control and 120 test specimens were divided into four groups (30 specimens each), depending upon the joint surface contour (butt, bevel, rabbet and round), with two subgroups based on type of the repair. Half of the specimens were repaired with plain repair resin and the other half with glass fibers reinforced repair resin. Transverse strength of the specimens was determined using three-point bending test. The results were analyzed using one-way ANOVA and Tukey post-hoc test (α= 0.05).
Results:
Transverse strength values for all repaired groups were significantly lower than those for the control group (P < 0.001) (88.77 MPa), with exception of round surface design repaired with glass fiber reinforced repair resin (89.92 MPa) which was significantly superior to the other joint surface contours (P < 0.001). Glass fiber reinforced resin significantly improved the repaired denture base resins as compared to the plain repair resin (P < 0.001).
Conclusion:
Specimens repaired with glass fiber reinforced resin and round surface design exhibited highest transverse strength; hence, it can be advocated for repair of denture base resins.
Keywords: Denture fracture, denture repair, transverse strength
INTRODUCTION
The acrylic resin denture base material was introduced in 1937 and has been used extensively for the fabrication of denture base since then. Despite its popularity, the material although adequate in satisfying aesthetic demands and other ideal requirements for denture base material, lacks in the mechanical strength. This is reflected in the unresolved problem of denture fracture and accompanying cost of repair.[1]
The denture may fracture accidentally by an impact outside the mouth, as a result of expelling the denture from the mouth while coughing, or simply of dropping the denture. Inside the mouth, the causes of denture fracture include excessive bite force, improper occlusal plane, prominent mid-palatine raphe, high frenum attachment, or poor fit.[2] Denture fracture inside the mouth is generally a flexural fatigue failure caused by cyclic deformation of the base.[3] This type of fracture most often occurs on or close to the mid-line, and it occurs most often in maxillary than in mandibular dentures.[4] Various materials such as, heat activated and chemically activated repair resin have been proposed for repairing fractured denture bases. Chemically activated repair resin generally allows for a simple and quick repair. However, dentures repaired with chemically activated repair resin often experience a refracture at the repaired site. One of the reasons for this unfavorable phenomenon is the insufficient transverse strength of chemically activated repair resin.[5]
To overcome this problem, various methods for enhancing the strength of the repaired part have been advocated; these include the alteration of repair surface design,[6,7,8,9] the use of repair surface treatments,[5,10,11] and combined use of autopolymerizing acrylic resin with reinforcing materials.[5,12,13]
Over the years, many authors have tried to improve the transverse strength of repaired resin by different materials and change in repair design. However, the results have been varied and conflicting.[5,6,7,8,9,12,13] Harrison and Stansbury[6] studied the effect of three types of joint surface contours on the transverse strength of repaired acrylic resin and found round surface design to be superior among all. Nagai, et al.[5] evaluated the repair of denture base resin using woven metal and glass fiber and found that glass fiber reinforcement with pre-treatment exhibited higher transverse strength than intact plates. Hence, this study was undertaken to evaluate the effect of various joint surface designs and also the effect of loose short cut glass fibers reinforced repair resin on the transverse strength of repaired acrylic resin. The null hypothesis was that the joint surface contours and glass fiber reinforcement had no effect on the transverse strength of repaired acrylic resins.
MATERIALS AND METHODS
Fabrication of acrylic resin specimens
The dimensions of the specimens were standardized to 64 × 10 × 2.5 mm (American Dental Association Specification No. 12) using customized brass master dies to fabricate the heat polymerized polymethyl methacrylate specimens (Trevalon, Dentsply, DeTrey GmbH, Konstanz, Germany).[14] The heat polymerized acrylic resin was mixed according to the manufacturer's instructions. The material was packed in the dough stage into the mold cavity and two trial closures were performed. The flasks were closed and kept under bench press (for 30 min). Clamped flasks were kept in thermostatically controlled polymerization unit (Acrylizer C-73A, Confident Dental Equipments Ltd, Bangalore, India) at 74°C for 2 h. The temperature of the water bath was raised to 100°C and the flasks were kept in polymerization unit for another 1 h. The flasks were bench cooled overnight prior to deflasking. Deflasked resin specimens were finished with 600 grit silicon carbide paper under water irrigation. A total of 135 test specimens were prepared. Fifteen intact specimens served as the control “C” specimens. One hundred and twenty specimens were divided into four groups (30 specimens each) depending upon the joint surface contours, group I-butt joint, group II-bevel joint, group III-rabbet joint, and group IV-round joint [Figure 1].
Figure 1.
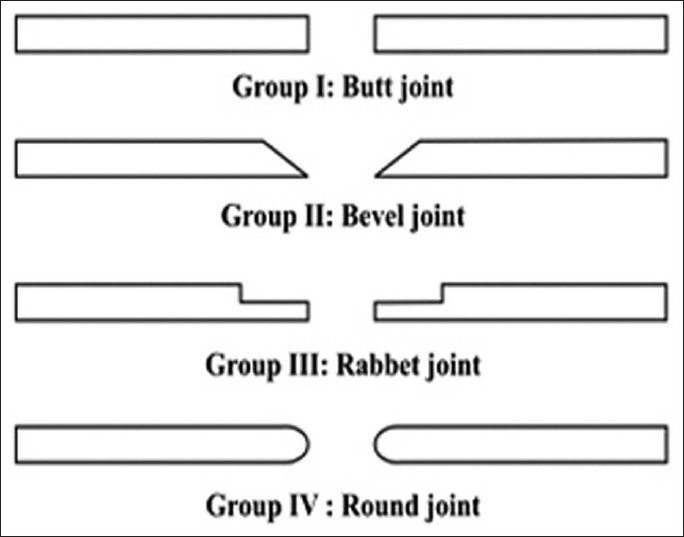
Schematic diagram showing four joint surface designs
Each interface design group was further divided into two subgroups A and B, depending upon the use of fiber for repair.
Surface designs preparation
For preparing surface designs, the specimens were inserted into a brass holding device, into which the specimens fitted exactly. At right angle, and in the center of the brass holding, a T-shaped guiding groove of 2 mm was milled. This served as a guide for the bur used to prepare the edge profile of the specimen prior to repair. Thus, the device ensured reproducibility of gap width and same zone of repair for all specimens. The straight micro-motor hand piece was attached to the surveyor (Ney, Dentsply, Toronto, Canada) arm and adjusted so that the end of the bur traveled across the bottom of the guiding groove. The holding device was fixed in the cast holder [Figure 2].
Figure 2.

Brass holding device and surveyor with clutch for holding hand piece
For the preparation of butt joint, a 2 mm space was created in the center of the specimen with straight fissure carbide bur (Fisher Tool Company Inc, New Taipei, Taiwan). For the preparation of 45° bevel joint, a 2 mm space was created in the center of the specimen. A line was drawn parallel to the prepared edge at 2 mm distance. 45° bevel was prepared by tilting the holding die at 45° angle to the carbide bur. For the preparation of rabbet surface designs, a 2 mm space was created in the center of the specimen. A line was drawn parallel to the prepared edge at 2 mm distance. After that, a recess measuring 1.5 mm deep and 2 mm wide was cut into the opposing interface surfaces by means of a straight fissure carbide bur. The round surface design was prepared by creating a 2 mm space in the center of the specimen. The outer edges of the interface were made rounded free hand. The prepared ends were smoothened with fine gauge abrasive strips (Oakey's abrasives, John Oakey and Mohan, Uttar Pradesh, India) to eliminate overhangs and unsupported acrylic extensions.
Repair method for test specimens
All the modified samples were repaired using two different repair resins. Modified samples were fixed in a metal mold with 2 mm gap between the fractured ends to provide bulk for the repair resin. Each surface design group was further divided into two subgroups “A” and “B” (15 sample each). Samples in subgroup “A” of each surface design group were repaired with chemically polymerized repair resin (Rapid repair, Dentsply, DeTrey GmbH, Konstanz, Germany) using the sprinkle-on monomer polymer technique. Samples in subgroup “B” of each surface design group were repaired with glass fibers (Saint Gobin Vertrotex, Hangzhou, Zhejing Province, France) reinforced chemically polymerized repair resin. The glass fibers (2%) were cut into 2 mm length and used randomly in loose form. Fibers were soaked in a silane coupling agent (Rely X Ceramic primer, 3M ESPE, St. Paul, Minnesota.) for 5 min to improve their bond to acrylic resin and were allowed to dry in the air for 20 min before they were incorporated in the repair resin. Fibers were mixed into the repair resin polymer with the help of glass stirrer. The mold was lubricated and the repair was carried out using the sprinkle-on monomer polymer technique. The joint space was slightly overfilled to allow for polymerization shrinkage. All the repaired specimens were finished and polished.
Assessment of the transverse strength of specimens
Transverse strength of the specimens was determined using three-point bending test. All specimens were stored in distilled water at 37°C ± 1°C for 48 h, prior to testing. Each specimen was subjected to the three-point bending test, at a crosshead speed of 5 mm/min, at a 50 mm distance with universal testing machine (Zwick, Materiaprufung 1445, Ulm, Germany). The load was applied to the center of the test specimen till fracture occurred. The fracture load was recorded in Kg and the transverse strength of each specimen was calculated using the formula: T.S. = 3Pl/2bd2, where T.S. = Transverse strength, P = Peak load applied, l = Distance between supports, b = Sample width, and d = Sample thickness.
RESULTS
Mean values and standard deviation of the transverse strength of studied groups were shown in Table 1. The highest and the lowest mean values were recorded for group IV B (89.92 MPa) and group I A (45.17 MPa), respectively.
Table 1.
Mean and standard deviation of transverse strength (MPa Megapascal) in the control and repaired specimens and Tukey groups
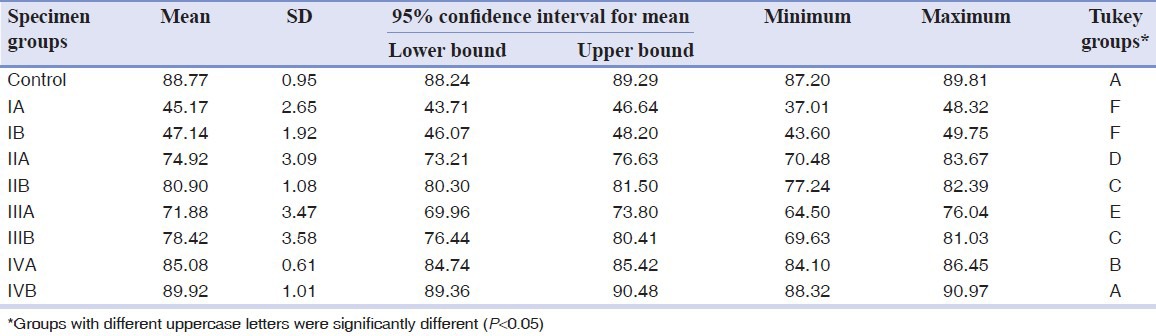
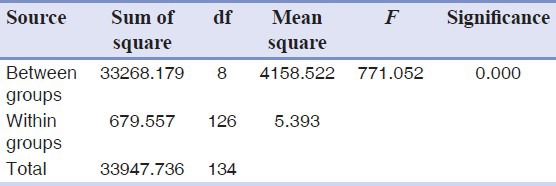
One-way ANOVA showed that there was significant difference between the studied groups (P < 0.001) [Table 2]. Tukey test was applied for pair wise comparison among the groups (P < 0.05). Control specimens showed significantly higher transverse strength value as compared to the all repaired specimens except for group IV B. Mean transverse strength of group IV B specimens was more than control specimens but the difference was not statistically significant (P = 0.91).
Table 2.
One-way analysis of variance
Subgroups A and B specimens of group IV showed significantly higher transverse strength value than subgroups A and B specimens of the other repaired groups (P < 0.05) [Table 1]. Specimens repaired with glass fiber reinforced chemically polymerized repair resin significantly improved the transverse strength value as compared to the plain chemically polymerized repair resin in all the four joint surface design groups; however, in group I, this difference was not significant (P = 0.342) [Table 1].
DISCUSSION
The results of this study showed that the combined effect of surface designs and glass fiber reinforcement affected the transverse strength of the repaired acrylic resin base; hence, the null hypothesis was rejected. Butt, bevel, rabbet, and round joint interface designs are most commonly advocated for repairing fractured denture bases; hence, these four surface designs were tested in this study.[6,7,8,14] In this study, chemically polymerized repair resin is used as a repair material for repairing test specimens because it is a quick procedure.[15]
Transverse strength is the most important value in function because dentures are most often under bending loads. Hence, the transverse strength test was considered to be an appropriate test method for this study. The results of this study showed that the transverse strength achieved by subgroups A and B specimens of group IV was significantly higher than the other repaired groups. Round joint was superior to the butt joint, bevel joint, and rabbet joint. These findings support the general principle that sharp-angled surfaces promote stress concentration.[6] The amount of stress concentration is directly related to the degree and abruptness of surface change. Therefore, since residual stress is produced and sharp-angled surface concentrates the stresses, when repairing fractured acrylic resin prosthesis, one should attempt to prevent recurrent structural failure by distributing these stresses as evenly as possible by repairing a joint with rounded interface surfaces. Similar results were obtained by Harrison and Stansbury[6] and Ward, et al.[7] The 45° bevel joint design showed higher transverse strength than butt and rabbet designs, as the geometry of 45° bevel shifts the interfacial stress pattern more toward a shear stress and away from the more damaging tensile stress during repair. Hanna, et al.[14] also investigated the effect of butt joint and 45° bevel joint on the transverse and impact strength and found higher values with 45° bevel joint. In this study, the control specimens showed significantly higher transverse strength value than all repaired groups except group IV B. This may be due to the residual monomer retained at the repair site. Residual monomer exerts a plasticizing action which weakens and softens the material.[16]
This study also focused on the effect of loose short cut glass fiber reinforcement (2%) on the transverse strength of repaired acrylic resin. In this study, glass fibers are used for reinforcement of repair resin because glass fibers are more aesthetic so they can be used in visible locations.[17] Loose glass fibers cut in 2 mm length were used for reinforcement of repair resin. The ease and simplicity of their inclusion would make this technique more acceptable for widespread use. 2% glass fibers were incorporated into repair resin polymer. Gutteridge[18] studied the effect of fiber content on the strength of the resin and reported that, any increase beyond 3% provides no beneficial effect. More than 4% fibers by weight are difficult to include in the resin during mixing, the resulting dough being dry and friable and difficult to pack. Transverse strength of the subgroup B specimens was higher than subgroup A specimens in all the four groups, except butt joint design in which the difference was not significant (P = 0.342). Mostafa and Lindsay[19] compared the fracture strength of a glass fiber-reinforced composite and a fiber-reinforced composite and showed more fracture strength with glass fiber-reinforced composite. Modulus of elasticity of glass fibers is very high; due to this, most of the stresses are received by them without deformation.[20] Incorporated fibers also shows dissipation of energy transmitted to any one point in the resin, before the critical value for the stress intensity exceeded.[21]
Although glass fiber may provide the best esthetic qualities among other fillers for dental applications, further research is needed to investigate the effect of glass fibers on oral mucosa. This in vitro study evaluated the transverse strength of repaired acrylic resin specimens by three-point bending test. This study design has limitations for simulating the clinical situation, as the specimens tested were different from actual denture configuration. Further investigations under more closely simulated clinical conditions are necessary.
CONCLUSION
Within the limitations of this study, the following conclusions can be drawn:
Transverse strength of round surface design samples repaired with glass fiber reinforced repair resin showed higher values than control but the difference is not significant.
Among all the surface design groups, butt surface and round surface designs showed the lowest and highest transverse strength, respectively.
Glass fiber reinforcement significantly improved the transverse strength of repaired acrylic resins with round, rabbet, and bevel joint surface designs.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Darbar UR, Huggett R, Harrison A. Denture fracture: A survey. Br Dent J. 1994;176:342–5. doi: 10.1038/sj.bdj.4808449. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal M, Nayak A, Hallikerimath R. A study to evaluate the transverse strength of repaired acrylic denture resins with conventional heat-cured, autopolymerizing and microwave-cured resins: An in vitro study. J Ind Pros Soc. 2008;8:36–41. [Google Scholar]
- 3.Shen C, Colaizzi FA, Birns B. Strength of denture repairs as influenced by surface treatment. J Prosthet Dent. 1984;52:844–8. doi: 10.1016/s0022-3913(84)80016-5. [DOI] [PubMed] [Google Scholar]
- 4.Kelly E. Fatigue failure in denture base polymers. J Prosthet Dent. 1969;21:257–66. doi: 10.1016/0022-3913(69)90289-3. [DOI] [PubMed] [Google Scholar]
- 5.Nagai E, Otani K, Satoh Y, Suzuki S. Repair of denture base resin using woven metal and glass fiber: Effect of methylene chloride pretreatment. J Prosthet Dent. 2001;85:496–500. doi: 10.1067/mpr.2001.115183. [DOI] [PubMed] [Google Scholar]
- 6.Harrison WM, Stansbury BE. The effect of joint surface contours on the transverse strength of repaired acrylic resin. J Prosthet Dent. 1970;23:464–72. doi: 10.1016/0022-3913(70)90014-4. [DOI] [PubMed] [Google Scholar]
- 7.Ward JE, Moon PC, Levine RA, Behrendt CL. Effect of repair surface design, repair material, and processing method on the transverse strength of repaired acrylic denture resin. J Prosthet Dent. 1992;67:815–20. doi: 10.1016/0022-3913(92)90591-w. [DOI] [PubMed] [Google Scholar]
- 8.Stipho HD, Stipho AS. Effectiveness and durability of repaired acrylic resin joints. J Prosthet Dent. 1987;58:249–53. doi: 10.1016/0022-3913(87)90186-7. [DOI] [PubMed] [Google Scholar]
- 9.Prabhudesia PS, Doiphode SS. A laboratory study to investigate the effect of joint design on the strength of repaired acrylic resin. J Indian Dent Assoc. 1984;56:229–33. [PubMed] [Google Scholar]
- 10.Gulve M, Gulve N. Effect of joint surface treatment on the flexural strength of repaired auto-polymerized acrylic resin. Internet J Dent Sci. 2011;9:1–8. [Google Scholar]
- 11.Pereira Rde P, Delfino CS, Butignon LE, Vaz MA, Arioli-Filho JN. Influence of surface treatments on the flexural strength of denture base repair. Gerodontology. 2012;29:e234–8. doi: 10.1111/j.1741-2358.2011.00454.x. [DOI] [PubMed] [Google Scholar]
- 12.Stipho HD. Repair of acrylic resin denture base reinforced with glass fiber. J Prosthet Dent. 1998;80:546–50. doi: 10.1016/s0022-3913(98)70030-7. [DOI] [PubMed] [Google Scholar]
- 13.Polyzois GL, Tarantili PA, Frangou MJ, Andreopoulos AG. Fracture force, deflection at fracture, and toughness of repaired denture resin subjected to microwave polymerization or reinforced with wire or glass fiber. J Prosthet Dent. 2001;86:613–9. doi: 10.1067/mpr.2001.120069. [DOI] [PubMed] [Google Scholar]
- 14.Hanna EA, Shah FK, Gebreel AA. Effect of joint surface contours on the transverse and impact strength of denture baseresin repaired by various methods. An in vitro study. J Am Sci. 2010;6:115–25. [Google Scholar]
- 15.Stanford JW, Burns CL, Paffenbarger GC. Self-curing resins for repairing dentures: Some physical properties. J Am Dent Assoc. 1955;51:307–15. doi: 10.14219/jada.archive.1955.0193. [DOI] [PubMed] [Google Scholar]
- 16.Anusavice KJ. 11th ed. St. Louis: Missouri; 2003. Phillips Science of Dental Materials; pp. 747–8. [Google Scholar]
- 17.Solnit GS. The effect of methyl methacrylate reinforcement with silane-treated and untreated glass fibers. J Prosthet Dent. 1991;66:310–4. doi: 10.1016/0022-3913(91)90255-u. [DOI] [PubMed] [Google Scholar]
- 18.Gutteridge DL. The effect of including ultra-high-modulus polyethylene fibre on the impact strength of acrylic resin. Br Dent J. 1988;164:177–80. doi: 10.1038/sj.bdj.4806395. [DOI] [PubMed] [Google Scholar]
- 19.Sadeghi M, Richards L. In vitro study of fracture strength of resin-bonded glass fiber-reinforced composite anterior fixed partial dentures. Dent Res J. 2005;2:14–8. [Google Scholar]
- 20.John J, Gangadhar SA, Shah I. Flexural strength of heat-polymerized polymethyl methacrylate denture resin reinforced with glass, aramid, or nylon fibers. J Prosthet Dent. 2001;86:424–7. doi: 10.1067/mpr.2001.118564. [DOI] [PubMed] [Google Scholar]
- 21.Schreiber CK. The clinical application of carbon fibre/polymer denture bases. Br Dent J. 1974;137:21–2. doi: 10.1038/sj.bdj.4803230. [DOI] [PubMed] [Google Scholar]


