Abstract
Zambia has over 1 million HIV infections nationwide and an urban prevalence rate of 23%. This study compared the impact of male involvement in multiple and single session risk reduction interventions among inconsistent condom users in Zambia and the role of serostatus among HIV-seropositive and serodiscordant couples. Couples (N=392) were randomised into intervention arms. Among inconsistent condom users at baseline (N=83), condom use increased in both conditions and this increase was maintained over a 12-month period. At 12 months, seronegative men in the multiple session condition increased sexual barrier (male and female condoms) use in comparison with those in the single session condition (F=16.13, p=0.001) while seropositive individuals increased sexual barrier use regardless of condition. Results illustrate the importance of both single and multiple session risk reduction counselling among seronegative men in serodiscordant couples in Zambia, and highlight the differing perception of risk between seropositive and serodiscordant persons.
Keywords: HIV, men, women, Africa, high-risk behaviour, behavioural intervention
Introduction
Persons living with HIV numbered 33.2 million in November 2007, of whom over 22.5 million resided in sub-Saharan Africa (UNAIDS, 2007). Zambia, a sub-Saharan country of 10.2 million persons, has urban prevalence rates of 23% (over 1 million estimated infections nationwide; Central Statistical Office, 2002). Prevention programmes such as voluntary counselling and testing (VCT) that target marital and cohabiting couples have been successful in reducing transmission following counselling (Allen et al., 1999; Roth et al., 2001), but protocols are needed to maintain long-term risk reduction (Bunnell et al., 2005). Like other health behaviours, an HIV diagnosis may increase condom use only temporarily (Allen et al., 1999); partners may not disclose their serostatus (Simbayi et al., 2007), protect an uninfected partner or restrict transmission of a potentially resistant virus between HIV seropositive partners (Kalichman, 2007).
In Zambia, men are the sexual decision-makers regarding condom use and women may not be able or willing to consistently use strategies for protection (Jones et al., 2005). In Africa and among other non-African populations, condom use is often the most consistent outside the marital relationship (Chimbiri, 2007). Long-term changes are difficult as sexual risk reduction within the primary relationship requires both sexual partners to make significant changes in their sexual practices and to agree to adhere to their use (Kalichman et al., 2003). The majority of sexual risk reduction interventions have targeted only one member of the couple or relied on single session ‘couples counselling’, assessing short-term (6 months or less) outcomes. In addition, interventions often target only couples in seroconcordant relationships. Previous research in the USA and Zambia found that gender-specific group sexual behaviour interventions enhance the acceptability and use of sexual barrier products (male and female condoms) among HIV-seropositive men (Jones et al., 2005) and women (Jones et al., 2004; Jones et al., 2006). Existing studies have found that seronegative men and women in serodiscordant relationships represent a unique population within those couples living with HIV.
The current study compared sexual risk behaviour among both HIV-seroconcordant positive and serodiscordant Zambian couples and multiple and single session group interventions for men in couple relationships to assess the influence of degree of male involvement and serostatus in couples’ sexual behaviour change. In addition, this study examined long-term sexual (12-month) risk behaviour following short- and long-term interventions among inconsistent condom users and evaluated the role of serostatus and degree of male involvement on risk behaviour over time.
Methods
Research approach
The Partner Project was a randomised study that recruited 420 HIV-seroconcordant and serodiscordant Zambian couples 18 years of age or older between January 2003 and June 2006. Of these, both partners participated and completed a baseline assessment of sexual and demographic data. A total of 392 couples were assessed from which additional analyses were conducted utilising data from a sample of participants with less than consistent condom use (N=83 couples). Couples were excluded if they reported no sexual activity within the last month.
Study candidates currently in heterosexual couple relationships were recruited from VCT clinics in the University Teaching Hospital, community health centres and non-governmental organisations. Randomisation was used to distribute the influence of VCT across both conditions. Couples were enrolled following HIV counselling and testing and provided verification of seropositive status of one or both members of the couple. Couples were screened for eligibility, i.e. currently sexually active, 18 years or older, couple relationship (minimum of 6 months as a couple to reduce potential attrition due to separation), and at least one member HIV seropositive.
Recruiters, assessors and interventionists were multilingual (e.g. Bemba, Nyanja, English) and assessments were conducted in the preferred language of the participant; the majority of assessments were conducted in English. Intervention sessions were conducted using a combination of Bemba, Nyanja and English, due to the mixture of audience language (73 local and 3 primary regional languages in Zambia); all study staff were fluent in the three intervention languages. All participants received monetary compensation for their travel expenses.
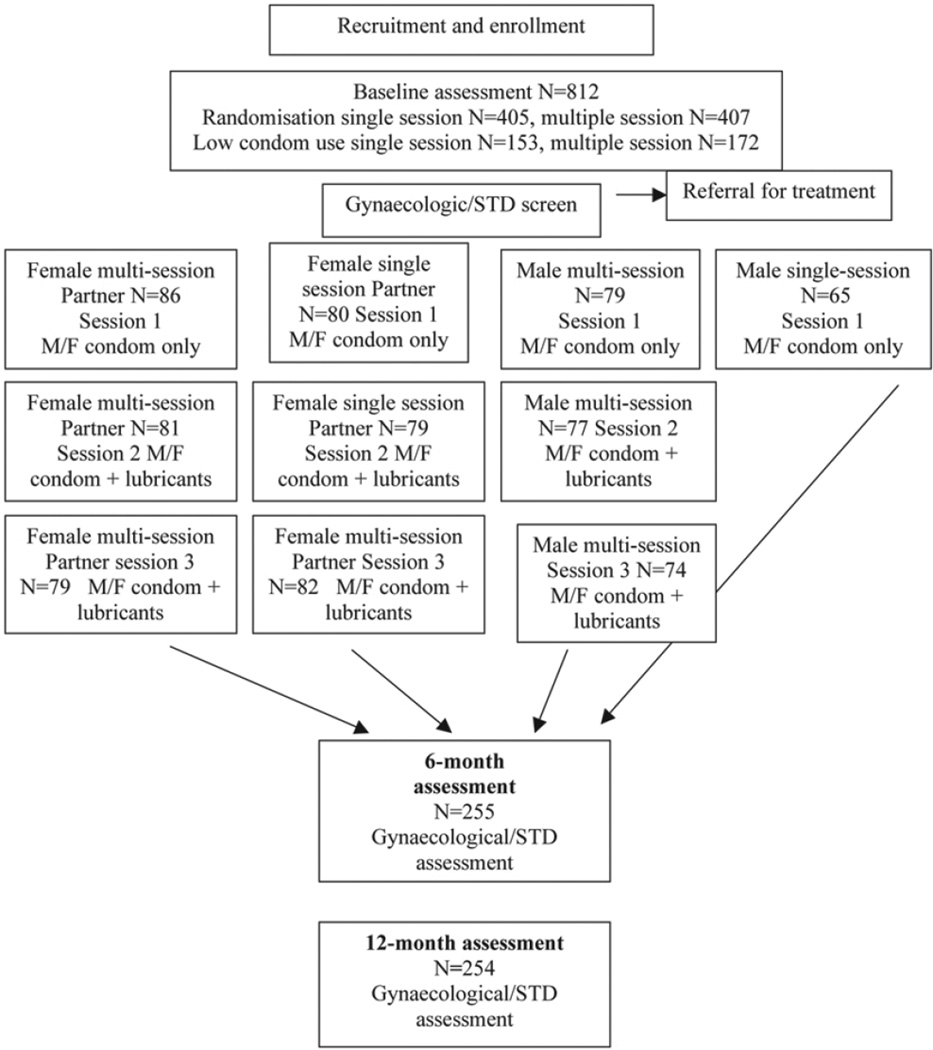
Participants (i) completed an informed consent; (ii) were tested for other sexually transmitted infections (STDs; HIV, antibody test, syphilis, serum; chlamydia and gonorrhoea, Gram stain) and vaginal infections (bacterial vaginosis, candidiasis, trichomonas), and penile infections; (iii) completed a baseline assessment of demographic information and sexual behaviour; and (iv) were randomised to condition (see Fig. 1).
Fig. 1.
Enrollment, randomisation, intervention and assessment.
All sessions were gender-concordant groups. All female participants completed the multiple (3) session intervention; their male partners were randomised into multiple (3) session and single (1) session group intervention arms to assess the relative influence of increased participation by male partners on sexual risk reduction within the couple. Both arms were introduced to and provided with the same number of male (18) and female (6) condoms per couple; multiple session group intervention participants were also provided with a lubricant pack of three vaginal lubricants to serve as placebos to assess product acceptability for future potential introduction of microbicides (Astroglide® & KY® gels, Lubrin® suppositories). Participants were notified of their STD or screening results and were provided with appropriate treatment prior to receiving study products. For those participants who were lost to followup, recruiters conducted home visits in the community to encourage study involvement and if the participant withdrew, establish the reason for attrition. In the event of permanent loss of one member of a couple (e.g. illness, death, estrangement), individual participants were encouraged to continue to participate. The primary causes for attrition over 12 months (15%) were moving to another location, (75%) employment, (10%) illness, (5%) divorce, and death (5%).
Ethical considerations
Though this represents a limitation in the study design, due to ethical concerns related to the transmission of HIV by participants, no control group or ‘usual care’ arm was included in this study. Data from previous studies indicate that even enhanced ‘usual care or control’ VCT clients significantly decreased their use of sexual barrier products over time (Jones et al., 2004).
Prior to participant recruitment, Institutional Review Board and Research Ethics Committee approvals were obtained in accordance with the provisions of the US Department of Health and Human Services and the University of Zambia regarding the conduct of research.
Intervention
The intervention (N=10 participants per gender-specific group) was developed from feedback from pilot studies with men in the USA and Zambia, and has been described in earlier journal literature (Jones et al., 2006; 2008). The 2- hour sessions emphasised participation and experimentation with sexual barrier products and provided an opportunity for practice, feedback, and reinforcement of sexual risk reduction strategies. Participants engaged in skill-building in a supportive environment, utilising communication techniques, negotiation skills, and experiential/interactive skill training to expand and reframe perceptions of barrier use and to increase self-efficacy and skill mastery. Material was presented utilising the conceptual model of the theory of reasoned action and planned behaviour (Albarracin et al., 2001) which suggests that (i) perceived behavioural control over situations will influence the intention to engage in behaviour and behaviour itself as a predictor of sexual barrier use, and (ii) personal intentions for specific behaviour influences attitudes about specific issues and subjective norms regarding issues, which (iii) influences beliefs about those behaviours. Thus, the perception of control over sexual behaviour will influence the intention to use condoms, and the intention to use condoms will influence attitudes about condom use and perceptions of norms regarding condom use, which will influence beliefs regarding using condoms. Additionally, participants were provided with vaginal lubricant products to try during the intervention, to inform the development of microbicidal products by assessing acceptability. Information on acceptability of the lubricant products has been extensively addressed in previous literature (Jones et al., 2004; 2006; 2008).
Facilitators were trained gender-matched male and female registered nurses, licensed practical nurses and health care staff trained in the administration of each condition. The intervention and accompanying videos were developed in English and translated into Zambian local languages (Nyanja and Bemba).
Session 1
The first session provided all participants with information on HIV/STD transmission, hierarchical counselling and skill training to facilitate male and female condom use. Sessions included videos and written materials on instructions for use. The correct method of male and female condom use and commonly asked questions were presented and discussed. After each session, participants were provided with a one-month supply of male and female condoms at no cost (9 male condoms and 3 female condoms each for man and woman, totalling 24 potential sex acts in 30 days), based on average sex act reporting of 3 times per week in previous samples in this context. Male condoms are available at no cost in community clinics; female condoms cost approximately $0.75 each. A lubricant pack was included with each female condom and in-session instructions for lubricant use were provided with the female condom.
Session 2
The second session provided exposure and experiential training with vaginal lubricants (high [Astroglide®] and low viscosity [KY®] gels and suppositories [Lubrin®]) and 1 month’s supplies of male and female condoms and vaginal lubricants. Participants were asked to try the lubricants in order to discuss their acceptability in the ensuing sessions, to inform the development of microbicidal products. Participants were strongly encouraged to use the condoms provided along with the vaginal lubricants during each act of sexual intercourse.
Session 3
The third session provided an opportunity for feedback and discussion regarding experiences with lubricants and condoms. An in-session discussion was conducted in which participants were asked to compare their experiences with each of the three lubricants and participants were then provided with additional condoms and lubricants of their choice.
Data collection tools and design
Demographics
This questionnaire included data collection on age, religion, nationality, ethnicity, educational level, employment status, residential status, HIV serostatus, approximate date of HIV diagnosis, mode of infection, marital status/current partner and children’s serostatus, living situation and number of children.
Sexual diary
This scale assessed the number of sex acts and the use of each sexual product during the reported sex act(s) over the last 7 days in a ‘yes’ or ‘no’ format. The sexual diary was administered at baseline, 6 and 12 months individually with an assessor, and monthly for months 1 to 6 during group sessions with an assessor.
This study used a repeated measures design with experimental arm (multiple, single) as the between-subjects factor and time (baseline and post-intervention) as the within-subjects factor. Correlations are reported as Pearson’s r statistics; analysis of variance repeated measures between arms are reported as F statistics; all comparisons used an alpha (2-tailed) of 0.05. Data were analysed using the Statistical Package for Social Sciences (SPSS).
Results
Sample size for the study was obtained from previous studies addressing sexual behaviour (Jones et al., 2004). As noted, no control group was included in the study design, all comparisons are between single and multiple session, males and females, and serostatus (positive and negative). Couples in which both partners completed a baseline assessment (N=392) were HIV seropositive (N=262) or serodiscordant (N=130), sexually active and living in urban Lusaka. The mean age among women was younger (mean age = 32) than men (mean age = 37); 25% of men and 8% of women were employed full-time, 49% of men and 67% of women were unemployed and 44% lived in poverty (less than $100 a month combined income). Most participants were Bemba (27%); Lozi (11%); Tonga (10%); Nsenga, Ngoni, Tumbuka (32%); Mambwe, Namwanga (7%); or another ethnic group (13%). The majority of men had a higher level of educational attainment (secondary school, 62%); 59% of women had completed no more than primary school (6 years). Most couples had children (93%; mean number of children, 3). One-third of couples planned to have more children. In order to distribute the effect of demographic variables and previous product exposure across conditions, participants were randomised at baseline. There were no significant demographic differences between single and multiple session participants at baseline.
Baseline
Consistent sexual barrier use among men (53%) and women (52%) was moderate at baseline. Among those who had been sexually active in the last 7 days, seronegative men (87) and women (43) with seropositive partners were less likely to use sexual barriers (men, F=14.65, p<0.001, women, F=25.93, p<0.001; see Table 1 for baseline and follow-up means). One per cent of men and 17% of women thought their partners had additional sexual partners outside their primary relationship. There were no differences in sexual behaviour between arms at baseline (F=1.69, p=0.194). Among demographic variables, only education was slightly associated with condom use (r=0.10, p=0.005. Couples reporting inconsistent condom use (‘inconsistent condom users’) at baseline were selected for analyses (N=83 couples). A validity check of reports of percentage of sexual barrier use over the last 7 days did not differ between couple members (F=2.41, p=0.123).
Table 1.
Sexual behaviour - mean per cent protected sex
| Single session | Multiple session | |
|---|---|---|
| Baseline | ||
| Men | 76% | 71% |
| Women | 77% | 73% |
| 6-month follow-up | ||
| Men | 89% | 84% |
| Women | 89% | 84% |
| 12-month follow-up | ||
| Men | 94% | 88% |
| Women | 94% | 88% |
Follow-up
To examine the effect of the number of sessions in the intervention on sexual behaviour, outcomes by both serostatus and gender over time were compared. At 6 months, while both men and women increased their condom use over time, there was no difference between conditions (single v. multiple sessions) among seronegative (men, F=0.216, p=0.65; women, F=0.439, p=0.52) or seropositive (men, F=4.1, p=0.05; women, F=0.06, p=0.807) participants. At 6 months post baseline, sexually active participants in both conditions reported a significant increase in consistent sexual barrier use over the last 7 days (men, t=-14.11, p<0.001, women, t=-13.4, p<0.001); 25% of participants reported female condom use, an increase from 3%. No demographic variables were associated with follow-up condom use at either time period.
In contrast, at 12 months, seronegative men in the multiple group condition had continued to increase their condom use in contrast with the single session condition (F=16.13, p=0.001) while seropositive men and women did not differ between conditions on level of condom use (men, F=0.069, p=0.794; women, F=1.97, p=0.169). Consistent male condom use over the last 7 days continued to increase in both conditions (men, t=16.78, p<0.001, women, t=-14.89, p<0.001), while 10% of participants continued to report female condom use.
Hierarchical multiple regression was used to assess the relative contribution of condition, when controlling for serostatus, on condom use at 12 months. Serostatus, entered at step one, did not explain any of the variance in condom use, while among the men, condition assignment predicted 18% of the variance in condom use (F=9.66, p=0.003); among women, neither serostatus nor condition predicted condom use (F=5.44, p=0.001, beta=-0.34).
Discussion
This study assessed sexual barrier use following a single-session or multiple-session risk reduction intervention in Zambia. Both men and women increased and maintained their condom use in both conditions over 12 months. The study also assessed risk reduction among inconsistent condom users and examined the role of serostatus among HIV-seropositive and serodiscordant Zambian couples. Among inconsistent users, sexual barrier use increased at 6 months and was maintained over a 12-month period in women with male partners in both the single and multiple session conditions. However, seronegative men in the multiple session condition reported higher levels of sexual barrier use than those in the single session condition at 12 months post baseline, while seropositive men increased their sexual barrier use regardless of condition.
The goal of this intervention was to increase sexual barrier use in seropositive and serodiscordant couples through improved communication, knowledge and perceived control. Results indicate that both the single- and multiple-session interventions were successful in increasing sexual barrier use in seropositive couples; changes in communication were not assessed and results related to perceived control have been presented in previous literature (Jones et al., 2005). Among those seronegative men, multiple sessions were more efficacious in increasing use. Both interventions were associated with increased use of female condoms, though rates overall were low. Results suggest that the intervention was beneficial, and that implementation in conjunction with VCT may be useful. However, due to ethical considerations no control group was used, thus limiting the strength of study findings. Results would be more statistically compelling with a true control condition; future studies should consider strategies to compare similar interventions to the standard of care in Zambia.
Although our previous study (Jones et al., 2004) found participants receiving VCT to decrease sexual barrier use over time, VCT may also result in an initial increase in sexual barrier use prior to participation in the intervention. This could also suggest that additional decreases in sexual barrier use may have been offset by participation in the intervention. However, VCT represents a useful component in HIV education, which provides a risk-reduction intervention that could be followed by the single- or multiple- session intervention to enhance longer term sexual barrier use.
As noted, the single-session intervention increased sexual barrier use in seropositive men, while seronegative men benefited more from multiple sessions. Previous literature supports the finding that VCT counselling services may increase barrier use; however, studies on how those changes are sustained over time is needed. The cost of providing a single-session group intervention to eight participants is eight times less than that of providing eight individual sessions, and the benefit of the added group session to VCT may also include reduced risk of HIV and STD transmission. The benefit of a single session versus the cost of a multiple-session intervention is important to consider when creating HIV prevention programmes. While multiplesession interventions may be higher in cost due to training and infrastructure needs associated with sustainability, they provide a strategy for influencing sexual risk behaviour in seronegative Zambian men. However, as HIV-seronegative men benefited more from a multiple (3) session intervention, the investment in the additional sessions may be merited.
Previous research with HIV-seropositive men and women in Zambia found that group risk-reduction interventions increased barrier use (Jones et al., 2005; 2004; 2006) and this finding appears to have been sustained. However, in keeping with other literature, serodiscordant couples represent a unique group (Bunnell et al., 2005) who may require longer term or more specific intervention (Allen et al., 2003) than seroconcordant couples. Zambian seronegative men differed in their response to these short- and long-term group interventions. As in other populations in sub-Saharan Africa (Schatz, 2005; Kalichman, Simbayi, Cain & Jooste, 2007), sexual risk-taking and personal risk-perception may influence behaviour among Zambian seronegative men and these men may require more time to change their behaviour. Longer-term interventions that address health beliefs and perceived risk may be integral to behavioural change in Zambian seronegative men.
In contrast, seropositive men increased their use of sexual barrier products regardless of condition. Seropositive Zambian men may have a perception of increased risk as a function of HIV-seropositive diagnosis, while Zambian seronegative men may perceive themselves as less likely to become infected due to their continued seronegative status. Differences between level of sexual barrier use among Zambian seronegative and positive women were not identified. This difference between genders may reflect the relative inability of Zambian women to force their male partners to use condoms if they choose not to do so. Study results were limited by the relatively small number of serodiscordant couples within the total sample and the lack of control condition, as noted earlier. It is important to note that the 12-month behaviour change may not have been sustained once the intervention and its measurement ended. In addition, results were drawn from a hospital clinical study rather than from a possibly more representative sample from community health centre clinics. Future studies should examine the efficacy of the study in the community health centre setting, and the practicality of translating the study from the hospital environment to the community. Additionally, the intervention could be strengthened by increased focus on enhancing communication within couples.
Lubricants were provided to participants to assess acceptability of vaginal lubricant products to guide the development of microbicidal products. The assessment of acceptability has been extensively discussed in previous literature (Jones et al., 2004; 2006; 2008). As previously noted, participants were asked to try these non-spermicidal and non-microbicidal lubricants and asked about the acceptability of the products. There was no association between lubricant use and male condom use, and female condoms can only be used with lubrication, which was provided to both single and multiple session conditions. Thus, it does not appear that lubricants influenced male condom use.
Conclusion
Results of this study support the recommendations for the use of cognitive behavioural intervention programmes to reduce the potential of HIV transmission (Healthy Living Project Team, 2007) within serodiscordant Zambian couples. This study illustrates the importance of group, single- and multiplesession counselling for risk reduction among seronegative men in serodiscordant couples in Zambia, and the need to tailor interventions to the meet the needs and perceived risk of both men and women.
Acknowledgements
This research was supported by a grant from the National Institute of Child Health and Human Development, R24HD43613. The support of the members of the research teams at the University of Zambia School of Medicine and the University Teaching Hospital in Lusaka for providing referrals in Zambia is acknowledged. Most importantly, the support of the study participants is appreciated.
Contributor Information
Deborah L Jones, Research Associate Professor, University of Miami Miller School of Medicine, Department of Psychiatry and Behavioral Sciences and a licensed clinical psychologist..
Ndashi Chitalu, Senior Lecturer in the Department of Medicine at the University of Zambia School of Medicine, and head of Emergency Care at the Pediatrics Unit of the University Teaching Hospital..
Phillimon Ndubani, Director of the Institute for Social and Economic Research, University of Zambia..
Miriam Mumbi, Registered Nurse and Project Coordinator at the University of Zambia School of Medicine..
Stephen M Weiss, Professor of Psychiatry and Behavioral Sciences; Medicine; and Psychology; and Vice Chair for Research, Department of Psychiatry and Behavioral Sciences, University of Miami Miller School of Medicine..
Olga Villar-Loubet, Lecturer in the Department of Psychiatry and Behavioral Sciences, University of Miami Miller School of Medicine..
Szonja Vamos, Research assistant at the University of Miami Miller School of Medicine..
Drenna Waldrop-Valverde, Research Associate Professor in the Department of Psychiatry & Behavioral Sciences at the University of Miami, Miller School of Medicine..
References
- Albarracin D, Johnson BT, Fishbein M, Muellerleile PA. Theories of reasoned action and planned behaviour as models of condom use: a meta-analysis. Psychological Bulletin. 2001;127:142–161. doi: 10.1037/0033-2909.127.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen SA, Karita E, N’Gandu N, Tichacek E. The evolution of voluntary testing and counselling as an HIV prevention strategy. In: Gibney, et al., editors. Preventing HIV in Developing Countries: Biomedical and Behavioural Approaches. New York: Plenum Press; 1999. [Google Scholar]
- Allen S, Meinzen-Derr J, Kautzman M, Zulu I, Trask S, Fideli U, Musonda R, Kasolo F, Gao F, Haworth A. Sexual behaviour of HIV discordant couples after HIV counselling and testing. AIDS. 2003;17:733–740. doi: 10.1097/00002030-200303280-00012. [DOI] [PubMed] [Google Scholar]
- Bunnell RE, Nassozi J, Marum E, Mubangizi J, Malamba D, Dillon B, Kalule J, Bahizi UJ, Musoke N, Mermin JH. Living with discordance: knowledge, challenges and prevention strategies of HIV-discordant couples in Uganda. AIDS Care. 2005;17:999–1012. doi: 10.1080/09540120500100718. [DOI] [PubMed] [Google Scholar]
- Central Statistical Office. ANC Sentinel Surveillance of HIV/Syphilis Trends in Zambia 1994–2002. Lusaka: Central Statistical Office, Zambia; 2002. [Google Scholar]
- Chimbiri AM. The condom is an “intruder” in marriage: evidence from rural Malawi. Social Science Medicine. 2007;64:1102–1115. doi: 10.1016/j.socscimed.2006.10.012. [DOI] [PubMed] [Google Scholar]
- Jones DL, Bhat GJ, Weiss SM, Bwalya V. Influencing sexual practices among HIV positive Zambian women. AIDS Care. 2006;18:629–634. doi: 10.1080/09540120500415371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones D, Ross D, Weiss SM, Bhat G, Chitalu N. Influence of partner participation on sexual risk behaviour reduction among HIV-positive Zambian women. Journal of Urban Health. 2005;82:92–100. doi: 10.1093/jurban/jti111. [DOI] [PubMed] [Google Scholar]
- Jones DL, Weiss SM, Bhat GJ, Feldman DA, Bwalya V, Budash DA. A sexual barrier intervention for HIV+/− Zambian women: acceptability and use of vaginal chemical barriers. Journal of Multicultural Nursing and Health. 2004;10:27–31. [PMC free article] [PubMed] [Google Scholar]
- Jones DL, Weiss SM, Chitalu NW, Mumbi MM, Shine A, Vamos S, Villar O. Acceptability and use of sexual barrier products and lubricants among HIV sero-positive Zambian men. AIDS Patient Care and STDs. 2008;12:1015–1020. doi: 10.1089/apc.2007.0212. 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman S. The synergies of HIV treatment, adherence and prevention. Future HIV Therapy. 2007;1:145–148. [Google Scholar]
- Kalichman SC, Cain D, Zweben A, Swain G. Sensation seeking, alcohol use and sexual risk behaviours among men receiving services at a clinic for sexually transmitted infections. Journal of the Study of Alcohol. 2003;64:564–569. doi: 10.15288/jsa.2003.64.564. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Cain D, Jooste S. Alcohol expectancies and risky drinking among men and women at high-risk for HIV infection in Cape Town South Africa; Addictive Behaviour; Jan 23; 2007. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth DL, Stewart KE, Clay OJ, van der Straten A, Karita E, Allen S. Sexual practices of HIV discordant couples in Rwanda: Effects of a testing and counselling program for men. International Journal of STD & AIDS. 2001;12:181–188. doi: 10.1258/0956462011916992. [DOI] [PubMed] [Google Scholar]
- Schatz E. ‘Take your mat and go!’: Rural Malawian women’s strategies in the HIV/AIDS era. Culture, Health & Sex. 2005;7:479–492. doi: 10.1080/13691050500151255. [DOI] [PubMed] [Google Scholar]
- Simbayi LC, Kalichman SC, Strebel A, Cloete A, Henda N, Mqeketo A. Disclosure of HIV status to sex partners and sexual risk behaviours among HIV-positive men and women, Cape Town, South Africa. Sexually Transmitted Infections. 2007;83:29–34. doi: 10.1136/sti.2006.019893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Healthy Living Project Team. Effects of a behavioural intervention to reduce risk of transmission among people living with HIV: The Healthy Living Project Randomized Controlled Study. Journal of Acquired Immune Deficiency Syndrome. 2007;44:213–221. doi: 10.1097/QAI.0b013e31802c0cae. [DOI] [PubMed] [Google Scholar]
- UNAIDS. UNAIDS/WHO AIDS Epidemic Update. 2007 Retrieved January 28, 2008, from http://data.unaids.org/pub/EPISlides/2007/2007_epiupdate_en.pdf.