CASE PRESENTATION
A 64-year-old man presented to hospital with a three-month history of progressively worsening mucousy bloody diarrhea, polyarthritis and a rash covering his lateral malleolus. His history was significant for previous quadriceps tendon rupture and supraventricular tachycardia. His only medication was a short course of prednisone initiated shortly before his hospitalization. He was a nonsmoker and nondrinker, with no significant family history.
Physical examination was significant for a fever of 38.2°C as well as a warm swollen left knee, ankle and foot. A bullous lesion 5 cm in size was present on the medial aspect of the left malleolus (Figure 1), with an erythematous base and draining serosanginous fluid. He exhibited multiple oral ulcers. The remainder of the examination was noncontributory.
Figure 1).

Bullous lesion characteristic of Sweet syndrome
Laboratory investigations revealed neutrophilia (14.5×109/L) and a normocytic anemia (1×105 g/L). Stool was negative for ova and parasites, and cell culture was negative for Clostridium difficile.
DIAGNOSIS
Colonoscopy demonstrated patchy inflammation and ulceration in the rectum, sigmoid and descending colon (Figure 2). The transverse and ascending colon, as well as the terminal ileum were within normal limits.
Figure 2).
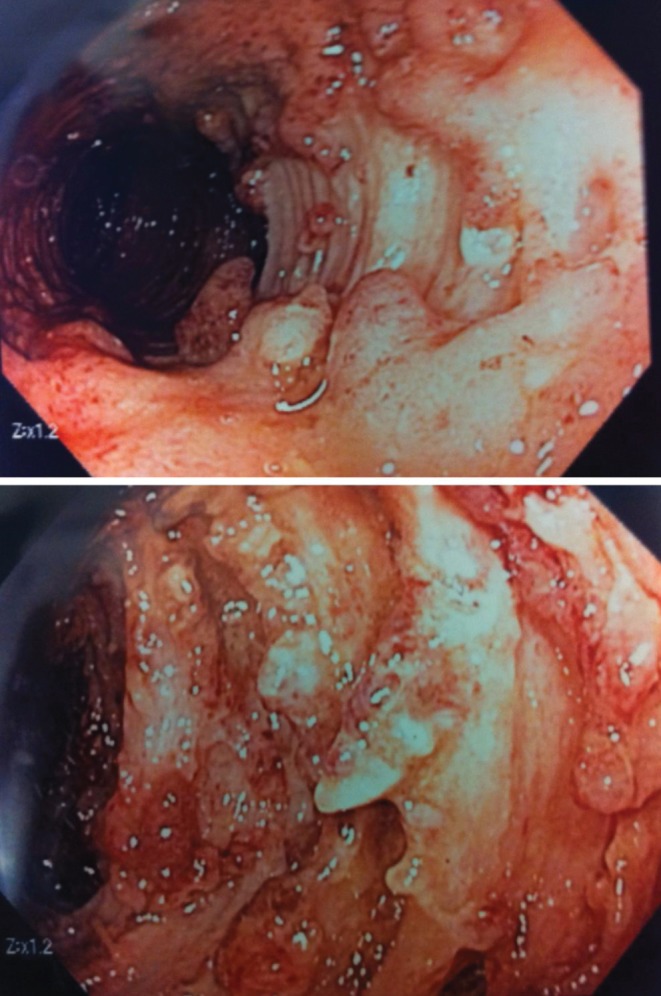
Endoscopic images of severe ulcerated inflammatory bowel disease in the sigmoid colon
Pathology of the colonic biopsies diagnosed inflammatory bowel disease (IBD). The patient ultimately required a hemicolectomy and the pathology of the resected colon confirmed IBD. Skin biopsies demonstrated diffuse inflammatory neutrophil-predominant infiltrate of the dermis, consistent with Sweet syndrome.
There are several features of the present case that are characteristic of Sweet syndrome. The patient presented with fever, leukocytosis and characteristic lesions. Arthralgias and oral ulcers can be extraintestinal manifestations of IBD, but are also apparent in 30% of patients with Sweet syndrome (1–4). Finally, the biopsy was characteristic of the diagnosis. Following bowel resection, the skin lesions, oral ulcers and arthralgias remained, all of which eventually responded to treatment with steroids.
DISCUSSION
Originally described by Robert Douglas Sweet in 1964 (5), Sweet syndrome is characterized by fever, leukocytosis and erythematous tender skin lesions with neutrophilic infiltration of the upper dermis (6,7). Several types of Sweet syndrome have been described including classical/idiopathic, malignancy-associated (8), drug-induced, pregnancy-related (9), parainfectious (10) and parainflammatory (1,2,6,7,11–13). Usually only the skin is involved but extracutaneous manifestations have been reported in bones, intestines, liver, aorta, lungs and muscles (1–4,14).
Differential diagnosis includes cellulitis, erythema multiforme, erythema nodosum, leukocytoclastic vasculitis, pyoderma gangrenosum, erysipelas and, rarely, disseminated Fusarium infection (7,15). While history, physical examination and other investigations can aid in the diagnosis, skin biopsy remains the gold standard.
First-line treatment options, based on uncontrolled case series and reviews, are systemic corticosteroids (6), potassium iodide (6), colchicine (16) or topical corticosteroids (6). Second-line medications include indomethacin (17), clofazimine (1), cyclosporine (18–20), dapsone (21–23) and doxycycline (24). Prognosis is generally good, with the rashes usually responding well to systemic steroids.
REFERENCES
- 1.von den Driesch P. Sweet’s syndrome (acute febrile neutrophilic dermatosis) J Am Acad Dermatol. 1994;31:535–56. doi: 10.1016/s0190-9622(94)70215-2. [DOI] [PubMed] [Google Scholar]
- 2.Kemmett D, Hunter JA. Sweet’s syndrome: A clinicopathologic review of twenty-nine cases. J Am Acad Dermatol. 1990;23:503–7. doi: 10.1016/0190-9622(90)70250-l. [DOI] [PubMed] [Google Scholar]
- 3.Hisanaga K, Iwasaki Y, Itoyama Y. Neuro-Sweet disease: Clinical manifestations and criteria for diagnosis. Neurology. 2005;64:1756–61. doi: 10.1212/01.WNL.0000161848.34159.B5. [DOI] [PubMed] [Google Scholar]
- 4.Moreland LW, Brick JE, Kovach RE. Acute febrile neutrophilic dermatosis (Sweet syndrome): A review of the literature with emphasis on musculoskeletal manifestations. Semin Arthrit Rheum. 1988;17:143–53. doi: 10.1016/0049-0172(88)90016-9. [DOI] [PubMed] [Google Scholar]
- 5.Sweet RD. An acute febrile neutrophilic dermatosis. Br J Dermatol. 1964;76:349–56. doi: 10.1111/j.1365-2133.1964.tb14541.x. [DOI] [PubMed] [Google Scholar]
- 6.Cohen PR. Sweet’s syndrome – a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis. 2007;2:34. doi: 10.1186/1750-1172-2-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burrall B. Sweet’s syndrome (acute febrile neutrophilic dermatosis) Dermatology online journal. 1999;5:8. [PubMed] [Google Scholar]
- 8.Cohen PR, Talpaz M, Kurzrock R. Malignancy-associated Sweet’s syndrome: Review of the world literature. J Clin Oncol. 1988;6:1887–97. doi: 10.1200/JCO.1988.6.12.1887. [DOI] [PubMed] [Google Scholar]
- 9.Cohen PR. Pregnancy-associated Sweet’s syndrome: World literature review. Obstetr Gynecol Surv. 1993;48:584–7. doi: 10.1097/00006254-199308000-00027. [DOI] [PubMed] [Google Scholar]
- 10.Chan HL, Lee YS, Kuo TT. Sweet’s syndrome: Clinicopathologic study of eleven cases. Int J Dermatol. 1994;33:425–32. doi: 10.1111/j.1365-4362.1994.tb04045.x. [DOI] [PubMed] [Google Scholar]
- 11.Sitjas D, Puig L, Cuatrecasas M, et al. Acute febrile neutrophilic dermatosis (Sweet’s syndrome) Int J Dermatol. 1993;32:261–8. doi: 10.1111/j.1365-4362.1993.tb04265.x. [DOI] [PubMed] [Google Scholar]
- 12.Fett DL, Gibson LE, Su WP. Sweet’s syndrome: Systemic signs and symptoms and associated disorders. Mayo Clin Proc. 1995;70:234–40. doi: 10.4065/70.3.234. [DOI] [PubMed] [Google Scholar]
- 13.Bourke JF, Keohane S, Long CC, et al. Sweet’s syndrome and malignancy in the U.K. Br J Dermatol. 1997;137:609–13. doi: 10.1111/j.1365-2133.1997.tb03796.x. [DOI] [PubMed] [Google Scholar]
- 14.Cohen PR, Kurzrock R. Sweet’s syndrome revisited: A review of disease concepts. Int J Dermatol. 2003;42:761–78. doi: 10.1046/j.1365-4362.2003.01891.x. [DOI] [PubMed] [Google Scholar]
- 15.Patterson TF, et al. Case records of the Massachusetts General Hospital. Case 22-2009. A 59-year-old man with skin and pulmonary lesions after chemotherapy for leukemia [corrected] N Engl J Med. 2009;361:287–96. doi: 10.1056/NEJMcpc0809065. [DOI] [PubMed] [Google Scholar]
- 16.Maillard H, Leclech C, Peria P, et al. Colchicine for Sweet’s syndrome. A study of 20 cases. Br J Deramatol. 1999;140:565–6. doi: 10.1046/j.1365-2133.1999.02747.x. [DOI] [PubMed] [Google Scholar]
- 17.Jeanfils S, et al. Indomethacin treatment of eighteen patients with Sweet’s syndrome. J Am Acad Dermatol. 1997;36:436–9. doi: 10.1016/s0190-9622(97)80222-8. [DOI] [PubMed] [Google Scholar]
- 18.Sharpe GR, Leggat HM. A case of Sweet’s syndrome and myelodysplasia: Response to cyclosporin. Br J Deramatol. 1992;127:538–9. doi: 10.1111/j.1365-2133.1992.tb14856.x. [DOI] [PubMed] [Google Scholar]
- 19.Bourke JF, Berth-Jones J, Graham-Brown RA. Sweet’s syndrome responding to cyclosporin. Br J Deramatol. 1992;127:36–8. doi: 10.1111/j.1365-2133.1992.tb14823.x. [DOI] [PubMed] [Google Scholar]
- 20.von den Driesch P, et al. Sweet’s syndrome – therapy with cyclosporin. Clin Exp Dermatol. 1994;19:274–7. doi: 10.1111/j.1365-2230.1994.tb01187.x. [DOI] [PubMed] [Google Scholar]
- 21.Aram H. Acute febrile neutrophilic dermatosis (Sweet’s syndrome). Response to dapsone. Arch Dermatol. 1984;120:245–7. [PubMed] [Google Scholar]
- 22.Fukae J, Noda K, Fujishima K. Successful treatment of relapsing neuro-Sweet’s disease with corticosteroid and dapsone combination therapy. Clin Neurol Neurosurg. 2007;109:910–3. doi: 10.1016/j.clineuro.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 23.Spencer B, Nanavati A, Greene J, et al. Dapsone-responsive histiocytoid Sweet’s syndrome associated with Crohn’s disease. J Am Acad Dermatol. 2008;59(2 Suppl 1):S58–60. doi: 10.1016/j.jaad.2008.03.044. [DOI] [PubMed] [Google Scholar]
- 24.Joshi RK, Atukorala DN, Abanmi A, et al. Successful treatment of Sweet’s syndrome with doxycycline. Br J Dermatol. 1993;128:584–6. doi: 10.1111/j.1365-2133.1993.tb00242.x. [DOI] [PubMed] [Google Scholar]


