Abstract
Background
In the last 6 months of life many older adults will experience a hospitalization followed by a transfer to a skilled nursing facility (SNF) for additional care. We sought to examine patterns of SNF use in the last 6 months of life.
Methods
We used the Health and Retirement Study, a longitudinal survey of older adults, linked to Medicare claims (1994-2007). We determined the number of individuals age 65 and older at death who used the SNF benefit in the last 6 months of life. We report demographic, social, and clinical correlates of SNF use. We examined the relationship between place of death and hospice use for those living in nursing homes and community prior to the last 6 months of life.
Results
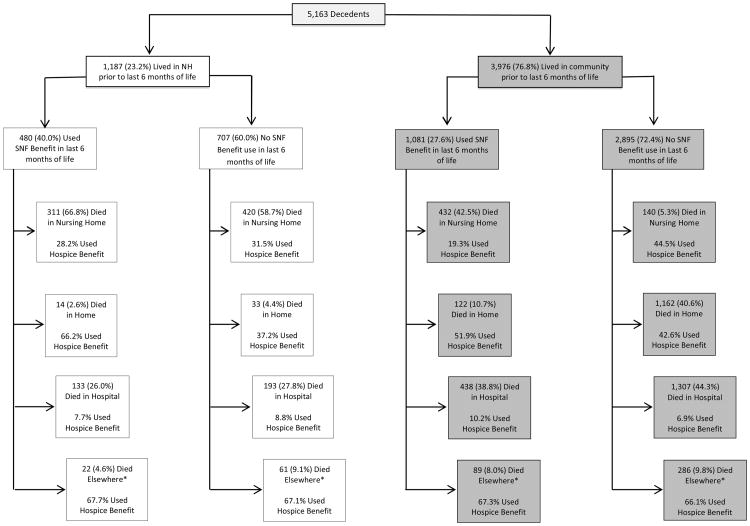
The mean age at death of the 5,163 subjects was 83 (54% female; 23% nursing home residents). We found 30.5% used the SNF benefit in the last 6 months of life, and 9.2% died enrolled on the SNF benefit. Use of the SNF benefit was greater among patients who were: 85 and older, had a high school education, did not have cancer, were nursing home residents, used home health services, and were expected to die (all p<0.01). Of community dwellers who used the SNF benefit 42.5% died in a nursing home, 10.7% died at home, 38.8% died in the hospital, and 8% died elsewhere. In contrast, of community dwellers that did not use the SNF benefit 5.3% died in a nursing home, 40.6% died at home, 44.3% died in the hospital, and 9.8% died elsewhere.
Conclusion
Nearly one-third of older adults receive care in a SNF in the last 6 months of life under the Medicare SNF benefit, and 1 out of 11 elders will die on the SNF benefit. Palliative care services should be incorporated into SNF-level care.
Introduction
The period leading up to death is a vulnerable time for patients and families with many symptoms that are difficult to witness and manage. This often leads to hospitalization and for some, discharge to a skilled nursing facility (SNF).
Skilled nursing facility use has exploded in recent decades. As hospital policy shifted to favor early discharge from the hospital in the 1980s and 1990s, a large proportion of nursing homes became certified to provide post-hospitalization skilled nursing care as a bridge between the hospital and home 1,2. Medicare beneficiaries are entitled to up to 100 days of SNF care if they have been hospitalized for 3 or more days and have a skilled need at discharge, such as rehabilitation, IV medications, and wound care. Medicare covers 100% of the cost for the first 20 days; after 20 days, if approved, the patient has a copay of $144.50 a day 3. Most enroll in SNF care for rehabilitation or life-prolonging care, but experience suggests that some dying patients are discharged to a SNF for end-of-life care.
Hospice services are often the only formal end-of-life care available in nursing homes 4. If a patient is in a nursing home under the Medicare SNF benefit, Medicare regulations prohibit concurrent enrollment in the hospice benefit for the same diagnosis 5. Rarely, a patient may receive SNF care while receiving hospice services if the SNF care is for a diagnosis unrelated to the hospice diagnosis 6. In addition, switching a patient from Medicare coverage under the SNF benefit to the hospice benefit has financial implications for both the patient and the nursing home. Medicare reimburses nursing homes at a higher rate for skilled services. Unlike the SNF benefit, the hospice benefit does not pay for room and board. Patients who transition to the hospice benefit must pay for room and board out of pocket or by Medicaid, for which many patients do not qualify.
Research has focused on the end of life experience in hospitals, but little is known about SNF use near the end-of-life. If SNF use is common near the end of life, this may have clinical implications for SNF patients, like greater engagement in advance care planning and goals of care as well as setting up reasonable expectations of what SNF care may be able to provide a person near the end of life. It may mean that SNF care needs to be reevaluated to incorporate a greater focus on end-of-life care.
Since there is very little known about SNF use at the end of life, we used the Health and Retirement Study, a nationally representative survey, linked to Medicare claims data to examine use of the Medicare SNF benefit at the end of life. The objective of this study was to use this data to look at the prevalence of use of the Medicare SNF benefit in the last 6 months of life, predictors of use, and care following use.
Methods
Subjects
The Health and Retirement Study (HRS) is a survey conducted by the Institute for Social Research at the University of Michigan and is sponsored by the National Institute on Aging. The goal is to study changes in health and wealth as people age. Since 1992 it has collected information on a representative sample of Americans 50 years and older; additional subjects are added every six years. Participants are interviewed every two years. After a subject dies, their next-of-kin provides information about the end-of-life time period in an exit interview. Data is collected on financial status, physical health and functioning, and place of death. More information about HRS sampling, data collection procedures, and measures can be found on the HRS web site (http://hrsonline.isr.umich.edu/).
We looked at HRS respondents age 65 years and older who died from 1994 to 2007 and had Medicare data (N = 6721) in the last 12 months of life. We excluded 1149 participants who had Medicare managed care because claims data is not complete for these individuals. There was incomplete Medicare data for an additional 409 people. The study sample consists of 5,163 HRS decedents with fee-for-service Medicare.
The Institutional Review Board at The University of California San Francisco approved this study.
Measures
Using Medicare claims data, we found the proportion of HRS decedents that used the SNF benefit in the last 6 months of life. Admitting diagnosis to SNF was determined using diagnosis related group (DRG) codes. We used Medicare claims to examine use of the hospice benefit while under the SNF benefit, length of use of the SNF benefit, time between hospital discharge and SNF benefit use, and the proportion of decedents who died on the SNF benefit.
We then looked for factors that might be associated with SNF benefit use at the end of life, based on prior research in end of life care and clinical experience 7-10. Demographic factors included age, gender, race and ethnicity. Social factors included marital status, education level, net worth, geographic region at death, any dependence in Activities of Daily Living (ADL) prior to the last 6 months of life (ADL include eating, toileting, dressing, bathing, transferring, walking across a room), nursing home residence prior to last 6 months of life, and if community dwelling, use of home health services prior to the last 6 months of life. For clinical factors, we examined seven health conditions (cancer, hypertension, diabetes, lung disease, heart disease, stroke, and cognitive impairment) and whether or not the death was expected as reported by the next-of-kin of the decedents during the exit interview.
Analyses
From the 5,163 HRS decedents we determined the percentage that used the SNF benefit in the last 6 months of life. We report age-adjusted prevalence of use of SNF benefit over time for those residing in a nursing home and those living in the community prior to SNF enrollment.
Participants had to be community dwelling at the time of enrollment in the HRS, which may have led to lower SNF use in the first several years of the study. Therefore, we report the mean use of SNF from 1994-1996, 1997-1999, 2000-2002, 2003-2005, and 2006-2007. We stratified use over time between those living in a nursing home and those living in the community prior to SNF use. We further divided the total number of SNF benefit users into three groups by age: 65-74, 75-84, and 85 and older to look for differences in use by age over time (an interaction effect).
To assess the association between demographic, social, and clinical factors and SNF benefit use at the end of life, we used a log-binomial regression and adjusted for age, gender, race/ethnicity, marital status, educational attainment, household net worth, region of death, history of ADL dependence, and presence or absence of chronic conditions to estimate relative risk. To look at clinical care differences between those who used the SNF benefit in the last 6 months of life and those who did not, we examined location of death and hospice use at the time of death. All reported analyses were weighted for the differential probability of selection and account for the complex design of HRS. The statistical analyses were performed using STATA 11 software and SAS 9.2 software.
Results
The final study sample consisted of 5,163 HRS decedents with fee-for-service Medicare in the last 12 months of life. The mean age at death was 82.8, with 41.3% age 85 and older, 45.5% male, 86.6% white, 41.7% married, 45.8% with less than a high school education, and 23.2% were nursing home residents prior to the last 6 months of life. Characteristics of decedents that did and did not use the SNF benefit are listed in Table 1.
Table 1. Characteristics of Subjects.
| Characteristics | HRS Decedents* (N=5,163) | Non-SNF Users* (N=3,602) | SNF Users* (N=1,561) | p-value |
|---|---|---|---|---|
|
| ||||
| Demographics | ||||
| Age at death, mean (SD) | 82.8 (7.9) | 82.2 (8.0) | 84.3 (7.6) | <0.001 |
| Age at death 65- <75yr, % | 17.8 | 19.8 | 13.2 | |
| Age at death 75 - <85yr, % | 40.9 | 42.7 | 36.9 | |
| Age at death 85 or older, % | 41.3 | 37.5 | 49.9 | |
| Male, % | 45.5 | 46.9 | 42.2 | 0.005 |
| Race/Ethnicity, % | 0.04 | |||
| Non-Hispanic White | 86.6 | 85.7 | 88.6 | |
| Non-Hispanic Black | 8.8 | 9.2 | 7.8 | |
| Hispanic | 3.5 | 3.8 | 2.8 | |
| Other | 1.1 | 1.3 | 0.8 | |
| Social Factors | ||||
| Married/partnered, % | 41.7 | 43.8 | 36.9 | <0.001 |
| Education < high school, % | 45.8 | 46.4 | 44.4 | 0.15 |
| Household net worth, median (IQR) | 80,000 (7,000-226,000) | 85,000 (10,000-232,500) | 66,000 (4,000-207,000) | 0.99 |
| Region Died, % | 0.24 | |||
| Midwest | 33.6 | 33.6 | 33.5 | |
| South | 29.9 | 30.9 | 27.6 | |
| Northeast | 24.0 | 23.2 | 25.9 | |
| West | 12.4 | 12.1 | 13.1 | |
| ADL Dependence prior to last 6 months of life, % | 33.8 | 32.0 | 37.9 | <0.001 |
| Nursing home residents prior to last 6 months of life, % | 23.2 | 20.0 | 30.5 | <0.001 |
| Used home health services prior to last 6 months of life, % | 33.1 | 30.6 | 38.8 | <0.001 |
| Clinical Factors | ||||
| Chronic Disease | ||||
| Cancer, % | 24.5 | 25.7 | 21.8 | 0.008 |
| Cognitive Impairment, % | 28.5 | 27.1 | 31.7 | 0.002 |
| Diabetes, % | 23.4 | 23.1 | 23.9 | 0.60 |
| Heart Disease, % | 49.9 | 49.4 | 51.0 | 0.30 |
| Hypertension, % | 61.0 | 60.6 | 61.8 | 0.50 |
| Lung Disease, % | 21.7 | 21.9 | 21.3 | 0.64 |
| Stroke, % | 24.2 | 23.6 | 25.6 | 0.26 |
| Death Expected | <0.001 | |||
| Yes, % | 60.5 | 56.5 | 69.7 | |
| No, % | 39.5 | 43.5 | 30.3 | |
| Year of Death | 0.008 | |||
| 1994, % | 3.8 | 4.6 | 2.0 | |
| 1995, % | 4.9 | 5.3 | 3.9 | |
| 1996, % | 6.4 | 6.5 | 6.0 | |
| 1997, % | 6.5 | 6.3 | 7.2 | |
| 1998, % | 6.3 | 6.5 | 6.0 | |
| 1999, % | 7.8 | 7.7 | 8.1 | |
| 2000, % | 6.8 | 6.7 | 6.9 | |
| 2001, % | 7.7 | 8.1 | 6.9 | |
| 2002, % | 8.0 | 8.0 | 8.0 | |
| 2003, % | 8.6 | 8.7 | 8.3 | |
| 2004, % | 8.6 | 8.3 | 9.1 | |
| 2005, % | 8.5 | 7.9 | 10.0 | |
| 2006, % | 8.6 | 8.4 | 9.0 | |
The values in this column represent the percent of the sample in the given subgroup, except for the age and household net worth variables. Reported values incorporate survey weights to account for the complex survey design.
Of the 5,163 HRS decedents, 30.5% used the SNF benefit in the last 6 months of life. A vast majority of SNF visits, 87.5%, were direct transfer from the hospital to SNF, and almost all SNF visits, 98.0%, were within 30 days of the hospital discharge. 58.2% were enrolled in SNF for 1-20 days and 41.8% stayed for over 20 days. Only 0.5% of all decedents used the SNF benefit and hospice benefit concurrently, and 1.5% enrolled in hospice on the day they were discharged from the SNF benefit.
Dying on the SNF benefit was not uncommon: 9.2% of HRS decedents died while on the SNF benefit: 3.2% died within one week and 7.2% died within 1 month (30 days) of admission.
We then explored place of death and use of the hospice benefit for decedents who were nursing home residents prior to the last 6 months of life. Place of death and use of hospice based on location were similar between nursing home residents who used the SNF benefit and those who did not (Figure 1).
Figure 1. Flow Diagram of Decedents.
*Inpatient Hospice, Assisted living facility, rest home, retirement home or senior care home
We then compared decedents who were residing in the community prior to the last 6 months of life. As shown in Figure 1, death in a nursing home was more common for community dwellers who used the SNF benefit in the last 6 months of life: 42.5% vs 5.3% of community dwelling non-SNF users. Of community dwellers who used the SNF benefit and died in a nursing home only 19.3% enrolled in hospice; whereas, 44.5% of community dwellers who did not use the SNF benefit and died in a nursing home used the hospice benefit. 53.5% of community dwellers who used the SNF benefit and died in the nursing home were on the SNF benefit at time of death.
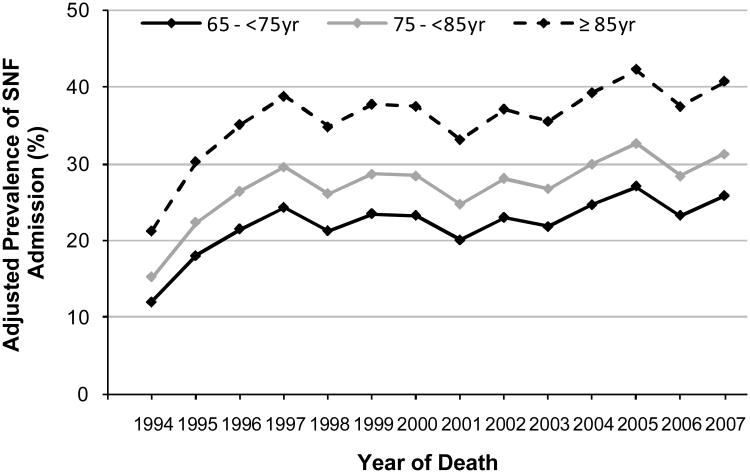
SNF benefit use was highest in those 85 years and older for each year of the study and no age by interaction effect was found (p>0.19) (Figure 2). The initial rise in rates of SNF benefit use were driven by community dwellers. From 1994-1996 to 1997-1999, the mean age-adjusted prevalence of use of the SNF benefit at the end of life among community dwellers increased from 20.3% to 30.6% (p<0.002). However, after this initial rise, the use of SNF has remained between 29.0-32.3 % from 2000-2007. There has been no significant change from 1994-2007 among nursing home residents who used the SNF benefit. Table 2 shows the top ten MEDPAR DRG admission diagnoses to SNF. After adjustment for demographic factors, social factors, chronic conditions, and ADL dependence, we found greater use of the SNF benefit among older adults (>85), those with at least a high school education, those who did not have cancer, those who lived in nursing home or if community dwelling used home health services prior to last 6 months of life, and had next-of-kin who expected death (Table 3).
Figure 2. Adjusted Prevalence of SNF Admission in the Last 6 Months of Life by Age Group.
Prevalence of SNF admission in the last 6 months of life was calculated with the adjustment for groups of age at death and year of death. Reported values incorporate survey weights to account for the complex survey design.
Table 2. Top 10 MEDPAR-DRG SNF Admission Diagnoses in the Last 6 Months of Life.
| DRG Code | Definition | Percent (%) |
|---|---|---|
| 127 | HEART FAILURE & SHOCK | 8.3 |
| 462 | REHABILITATION | 5.4 |
| 236 | FRACTURES OF HIP & PELVIS | 4.8 |
| 89 | SIMPLE PNEUMONIA & PLEURISY AGE >17 WITH COMPLICATIONS, COMORBIDITIES | 4.8 |
| 88 | CHRONIC OBSTRUCTIVE PULMONARY DISEASE | 4.4 |
| 12 | DEGENERATIVE NERVOUS SYSTEM DISORDERS | 3.6 |
| 14 | INTRACRANIAL HEMORRHAGE OR CEREBRAL INFARCTION (beginning 10-1-04) | 3.3 |
| 467 | OTHER FACTORS INFLUENCING HEALTH STATUS | 2.2 |
| 90 | SIMPLE PNEUMONIA & PLEURISY AGE >17 WITHOUT COMPLICATIONS, COMORBIDITIES | 2.1 |
| 82 | RESPIRATORY NEOPLASMS | 1.9 |
Table 3. Factors associated with use of the Medicare SNF benefit in the last 6 months of life.
| Unadjusted RR (95% CI) | P Value | Adjusted RR (95% CI)* | P Value | |
|---|---|---|---|---|
|
| ||||
| Demographic Factors | ||||
| Age at death | ||||
| < 85 | ref | ref | ||
| ≥ 85 | 1.42 (1.31-1.53) | <0.001 | 1.34 (1.20-1.49) | <0.001 |
|
| ||||
| Men | ref | ref | ||
| Women | 1.14 (1.04-1.25) | 0.005 | 1.01 (0.90-1.13) | 0.86 |
|
| ||||
| Race/Ethnicity | ||||
| Non-Hispanic White | ref | ref | ||
| Non-Hispanic Black | 0.87 (0.74-1.03) | 0.10 | 0.86 (0.71-1.03) | 0.10 |
| Hispanic | 0.78 (0.59-1.05) | 0.10 | 0.81 (0.59-1.09) | 0.16 |
| Other | 0.67 (0.41-1.09) | 0.10 | 0.67 (0.41-1.10) | 0.11 |
|
| ||||
| Social Factors | ||||
| Marital Status | ||||
| Married/Partnered | ref | ref | ||
| Not Married/Partnered | 1.22 (1.10-1.36) | <0.001 | 1.06 (0.94-1.20) | 0.33 |
|
| ||||
| Educational attainment | ||||
| < High school | 0.95 (0.88-1.02) | 0.15 | 0.89 (0.82-0.98) | 0.01 |
| ≥ High school | ref | ref | ||
|
| ||||
| Household Net Worth | ||||
| Quartile 1 (lowest) | 1.19 (1.05-1.35) | 0.008 | 1.15 (0.99-1.32) | 0.06 |
| Quartile 2 | 1.08 (0.94-1.22) | 0.27 | 1.10 (0.96-1.27) | 0.17 |
| Quartile 3 | 0.98 (0.85-1.13) | 0.78 | 0.99 (0.86-1.15) | 0.91 |
| Quartile 4 | ref | ref | ||
|
| ||||
| Region of Death | ||||
| Midwest | ref | ref | ||
| South | 0.92 (0.81-1.05) | 0.21 | 0.97 (0.85-1.09) | 0.58 |
| Northeast | 1.08 (0.93-1.26) | 0.33 | 1.09 (0.95-1.26) | 0.21 |
| West | 1.05 (0.87-1.28) | 0.60 | 1.03 (0.83-1.29) | 0.77 |
|
| ||||
| ADL dependence prior to last 6 months of life | ||||
| Yes | 1.19 (1.09-1.31) | <0.001 | 1.06 (0.95-1.18) | 0.30 |
| No | ref | ref | ||
|
| ||||
| Nursing home resident prior to last 6 months of life | ||||
| Yes | 1.45 (1.29-1.63) | <0.001 | 1.23 (1.06-1.42) | 0.006 |
| No | ref | ref | ||
|
| ||||
| Used home health services prior to last 6 months of life† | ||||
| Yes | 1.34 (1.20-1.50) | <0.001 | 1.24 (1.09-1.40) | 0.002 |
| No | ref | ref | ||
|
| ||||
| Clinical Factors | ||||
| Chronic Conditions | ||||
| Cancer | 0.86 (0.77-0.96) | 0.009 | 0.89 (0.80-0.99) | 0.04 |
| No Cancer | ref | ref | ||
| Hypertension | 1.04 (0.93-1.15) | 0.50 | 1.03 (0.93-1.13) | 0.61 |
| No Hypertension | ref | ref | ||
| Diabetes | 1.03 (0.91-1.17) | 0.60 | 1.11 (0.98-1.26) | 0.09 |
| No Diabetes | ref | ref | ||
| Lung Disease | 0.97 (0.87-1.09) | 0.64 | 1.02 (0.90-1.14) | 0.79 |
| No Lung Disease | ref | ref | ||
| Heart Disease | 1.05 (0.96-1.14) | 0.30 | 1.02 (0.93-1.12) | 0.61 |
| No Heart Disease | ref | ref | ||
| Stroke | 1.08 (0.94-1.24) | 0.25 | 0.99 (0.85-1.14) | 0.84 |
| No Stroke | ref | ref | ||
| Cognitive Impairment | 1.16 (1.06-1.28) | 0.002 | 1.04 (0.93-1.16) | 0.50 |
| No Cognitive Impairment | ref | ref | ||
|
| ||||
| Death Expected | ||||
| Yes | 1.50 (1.36-1.66) | <0.001 | 1.46 (1.30-1.63) | <0.001 |
| No | ref | ref | ||
Adjusted for age, gender, race/ethnicity, marital status, educational attainment, household net worth, region of death, history of ADL dependence, and presence or absence of chronic conditions.
Analysis only done on community dwelling residents
Comment
In this nationally representative study of older individuals, we found that nearly one-third of individuals 65 and older received SNF-level care in the last 6 months of life under the Medicare SNF benefit. Strikingly, 1 out of 11 elders died while enrolled on the SNF benefit. Nursing home residents prior to last 6 months of life died in similar locations and had similar rates of hospice use whether they used the SNF benefit or not. However, those who lived in the community and then went on to use the SNF benefit were different than those who did not use the SNF benefit. Nearly half of community dwellers who used the SNF benefit subsequently died in a nursing home and over half were on the SNF benefit at death. Less than a quarter were enrolled in hospice at death. In comparison, less than 10% of community dwellers who did not use the SNF benefit died in a nursing home, but twice as many (41.7%) enrolled in hospice. Rates of SNF benefit use increased among community dwelling individuals until 1999, then leveled out, likely due to minimal growth in SNF beds since that time 11.
Our finding that Medicare decedents commonly used SNF care at the end of life suggests a need to better understand who is using the SNF benefit and if they are receiving care that matches their goals. After hospitalization, elderly patients often experience a functional decline in one or more activities of daily living (ADLs) 12,13. When planning for discharge, the primary focus for these individuals is often providing skilled nursing or rehabilitative services that will allow a patient to return to the prior level of health and functioning, an important aspect of caring for older adults. Individuals that receive SNF care are likely seen as having more potential for recovery. What may not be recognized is that the decline during a hospitalization may reflect the patient's overall health condition will continue to deteriorate despite adequate rehabilitation. In fact, the very needs that necessitate SNF use are the same indicators of an end-of-life trajectory seen in frail elders 14. Honest and frank discussions around goals of care not only in the hospital but once they are admitted to SNF may allow for an earlier introduction to palliative care.
SNF benefit users had more disability and required more home health and nursing home care. Many studies have shown a noticeable, although variable, decline in function leading up to death 14,15. Patients transferring to SNF-level care often have high care needs and are medically complex 11. At discharge, patient's goals may not be consistent with hospice or providers may not recognize they are on an end-of-life path. By incorporating a palliative care focus into SNF care this may allow for earlier recognition of when someone is appropriate for hospice referral. While rehabilitation is an important aspect to elder care, there are other issues near the end of life that may not be focused on when on the SNF benefit, such as symptom management or discussions around goals of care.
Almost 1 in 11 elders died on the SNF benefit; most in the first 30 days of admission. For community dwellers, over half who died in the nursing home were on the SNF benefit at death, and next of kin expecting death was predictive of SNF benefit use. This suggests that patients are being discharged from hospitals to nursing homes under the Medicare SNF benefit for end-of-life care. While it is possible to be on the hospice and SNF benefits concurrently if the services are billed for separate conditions (e.g. SNF for rehabilitation following a fall, hospice for cancer), only 0.5% of decedents were enrolled in both programs simultaneously in our study. Besides functional decline, the end of life is associated with many other issues such as pain, shortness of breath, spiritual distress, caregiver burnout and grief 16. While our study provides no evidence about the quality of care received, the literature suggests that nursing home residents have little access to palliative care outside of hospice services 17-19. Hospice care in the nursing home can be variable, although patients and families report better symptom control and satisfaction with care when nursing home residents receive hospice care 20,21. Hospice services provide symptom management, bereavement services, social work and dedicated chaplaincy 17. The SNF benefit does not provide the depth of end-of-life services that hospice provides.
Unfortunately, financial issues may contribute to why patients near the end-of-life are using the SNF benefit and not the hospice benefit. Elderly patients living in the community who are becoming more symptomatic or functionally declining may go to the hospital because families cannot manage them at home. Our study suggests that older, more clinically complex patients are using the SNF benefit near the end of life. They may require care that cannot be provided in the home even with hospice. Unless someone already has Medicaid, hospice may not be an option because the cost of room and board in a nursing home is too burdensome. Families often face an uncomfortable choice – either they pay for room-and-board out of pocket to have access to hospice services, or continue on the Medicare SNF benefit, relying on the nursing home services for palliative and end-of-life services.
Likewise, nursing homes receive higher reimbursement for patients on the SNF benefit than long term care payments via Medicaid. Given Medicaid bed holding policies for nursing home residents, nursing homes have a financial incentive to hospitalize their patients 22,23. After hospitalization, nursing home residents may return on the Medicare SNF benefit, which will reimburse the SNF more than if they came back for custodial care paid for by Medicaid 24. SNF care may be appropriate for some of these patients, but for others who cannot receive SNF and hospice care concurrently for the same condition, this practice may lead to care that is not consistent with a patient's goals or poorer quality end-of-life of care.
Limitations are noted. While we report the admission diagnosis, we are unable to determine the true circumstances that led each individual to use the SNF benefit after hospitalization. A patient with heart failure that is near the end of life, for example, could have been transferred to a nursing home under the Medicare SNF benefit for management of intractable shortness of breath that cannot be managed at home. Hospice may have even been considered. We did find, however, that rehabilitation was a top DRG for admission to SNF, suggesting that at least a substantial minority of patients are not transferred to SNF for end-of-life care. Since we studied decedents, we are unable to compare with subjects that use the SNF benefit and go on to live longer lives. However, incorporation of a palliative focus alongside rehabilitation would likely be a benefit for patients whether or not they were clearly on an end-of-life trajectory. Finally, we were unable to describe SNF use for patients with Medicare Managed Care (17 %).
In conclusion, SNF Medicare benefit use is high at the end of life highlighting need to incorporate quality palliative care services in nursing homes. The hospice benefit is the primary way palliative care services are delivered in nursing homes. There is growing focus on developing palliative care in nursing homes alongside the current goals of functional improvement. Perhaps having Medicare pay concurrently for post-acute SNF care and hospice services for the same condition could allow for earlier incorporation of palliative care for these medically complex patients.
Acknowledgments
Dr. Smith was supported by the National Center for Research Resources UCSF-CTSI (UL1 RR024131). Dr. Covinsky was supported by a K-24 from the National Institute on Aging (K24AG029812).
Role of the Sponsor: The funding organizations had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
Grant Support: Dr. Smith was supported by the National Center for Research Resources UCSF-CTSI (UL1 RR024131). Dr. Covinsky was supported by a K-24 from the National Institute on Aging (K24AG029812).
Footnotes
Financial Disclosures: The authors have no conflicts of interest to report.
References
- 1.Kaplan SJ. Growth and Payment Adequacy of Medicare Postacute Care Rehabilitation. Archives of Physical Medicine and Rehabilitation. 2007;88(11):1494–1499. doi: 10.1016/j.apmr.2007.08.112. [DOI] [PubMed] [Google Scholar]
- 2.Levy CR, Fish R, Kramer AM. Site of Death in the Hospital Versus Nursing Home of Medicare Skilled Nursing Facility Residents Admitted Under Medicare's Part A Benefit. Journal of the American Geriatrics Society. 2004;52(8):1247–1254. doi: 10.1111/j.1532-5415.2004.52352.x. [DOI] [PubMed] [Google Scholar]
- 3.Medicare: Policy, Advocacy, and Education. [Accessed February 6, 2012];Medicare Part A- Hospital Insurance. http://www.cahealthadvocates.org/basics/partA.html#SNF.
- 4.Miller SC, Teno JM, Mor V. Hospice and palliative care in nursing homes. Clinics in geriatric medicine. 2004;20(4):717–734. vii. doi: 10.1016/j.cger.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 5.Huskamp HA, Stevenson DG, Chernew ME, Newhouse JP. A new medicare end-of-life benefit for nursing home residents. Health Aff (Millwood) 2010 Jan-Feb;29(1):130–135. doi: 10.1377/hlthaff.2009.0523. [DOI] [PubMed] [Google Scholar]
- 6. [Accessed October 27, 2011];Medicare Benefit Policy Manual: Chapter 9 - Coverage of Hospice Services Under Hospital Insurance. Revision 141: https://www.cms.gov/manuals/downloads/bp102c09.pdf.
- 7.Parker-Oliver D, Porock D, Zweig S, Rantz M, Petroski GF. Hospice and nonhospice nursing home residents. Journal of palliative medicine. 2003;6(1):69–75. doi: 10.1089/10966210360510136. [DOI] [PubMed] [Google Scholar]
- 8.Kwak J, Haley WE, Chiriboga DA. Racial Differences in Hospice Use and In-Hospital Death Among Medicare and Medicaid Dual-Eligible Nursing Home Residents. The Gerontologist. 2008;48(1):32–41. doi: 10.1093/geront/48.1.32. [DOI] [PubMed] [Google Scholar]
- 9.Gessert CE, Haller IV. Medicare Hospital Charges in the Last Year of Life: Distribution by Quarter for Rural and Urban Nursing Home Decedents With Cognitive Impairment. The Journal of Rural Health. 2008;24(2):154–160. doi: 10.1111/j.1748-0361.2008.00152.x. [DOI] [PubMed] [Google Scholar]
- 10.Stevenson DG, Bramson JS. Hospice care in the nursing home setting: a review of the literature. Journal of pain and symptom management. 2009;38(3):440–451. doi: 10.1016/j.jpainsymman.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Commissioin MPA. A Data Book: Health Care Spending and the Medicare Program. 2008. p. 210. [Google Scholar]
- 12.Volpato S, Cavalieri M, Sioulis F, et al. Predictive value of the Short Physical Performance Battery following hospitalization in older patients. J Gerontol A Biol Sci Med Sci. 2011 Jan;66(1):89–96. doi: 10.1093/gerona/glq167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sager MA, Franke T, Inouye SK, et al. Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med. 1996 Mar 25;156(6):645–652. [PubMed] [Google Scholar]
- 14.Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM. Patterns of functional decline at the end of life. JAMA. 2003 May 14;289(18):2387–2392. doi: 10.1001/jama.289.18.2387. [DOI] [PubMed] [Google Scholar]
- 15.Covinsky KE, Eng C, Lui LY, Sands LP, Yaffe K. The last 2 years of life: functional trajectories of frail older people. J Am Geriatr Soc. 2003 Apr;51(4):492–498. doi: 10.1046/j.1532-5415.2003.51157.x. [DOI] [PubMed] [Google Scholar]
- 16.Hanson LC, Eckert JK, Dobbs D, et al. Symptom experience of dying long-term care residents. Journal of the American Geriatrics Society. 2008;56(1):91–98. doi: 10.1111/j.1532-5415.2007.01388.x. [DOI] [PubMed] [Google Scholar]
- 17.Zerzan J, Stearns S, Hanson L. Access to palliative care and hospice in nursing homes. JAMA: the journal of the American Medical Association. 2000;284(19):2489–2494. doi: 10.1001/jama.284.19.2489. [DOI] [PubMed] [Google Scholar]
- 18.Happ MB, Capezuti E, Strumpf NE, et al. Advance Care Planning and End-of-Life Care for Hospitalized Nursing Home Residents. Journal of the American Geriatrics Society. 2002;50(5):829–835. doi: 10.1046/j.1532-5415.2002.50207.x. [DOI] [PubMed] [Google Scholar]
- 19.Casarett D, Karlawish J, Morales K, Crowley R, Mirsch T, Asch DA. Improving the use of hospice services in nursing homes: a randomized controlled trial. JAMA: the journal of the American Medical Association. 2005;294(2):211–217. doi: 10.1001/jama.294.2.211. [DOI] [PubMed] [Google Scholar]
- 20.Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. JAMA: the journal of the American Medical Association. 2004;291(1):88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 21.Reynolds K, Henderson M, Schulman A, Hanson LC. Needs of the dying in nursing homes. J Palliat Med. 2002 Dec;5(6):895–901. doi: 10.1089/10966210260499087. [DOI] [PubMed] [Google Scholar]
- 22.Intrator O, Grabowski DC, Zinn J, et al. Hospitalization of Nursing Home Residents: The Effects of States' Medicaid Payment and Bed-Hold Policies. Health services research. 2007;42(4):1651–1671. doi: 10.1111/j.1475-6773.2006.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grabowski DC, Zhanlian F, Intrator O, Mor V. Medicaid Bed-Hold Policy and Medicare Skilled Nursing Facility Rehospitalizations. Health services research. 2010 Dec;45(6p2):1963–1980. doi: 10.1111/j.1475-6773.2010.01104.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ersek M, Wilson SA. The challenges and opportunities in providing end-of-life care in nursing homes. J Palliat Med. 2003 Feb;6(1):45–57. doi: 10.1089/10966210360510118. [DOI] [PubMed] [Google Scholar]