Abstract
Objective
Longer duration of untreated psychosis (DUP) is associated with poorer early-course and long-term outcomes, and is a target of early detection and intervention efforts. Given the paucity of research on childhood and adolescent stressors (e.g., maltreatment and neighborhood disorder) as potential predictors of DUP, limited research on premorbid substance use as a determinant of DUP, and inconclusive findings on the association between DUP and neurocognition, we conducted three sets of analyses to address these issues. Mode of onset of psychosis was also considered, given its established role as an illness-level correlate of DUP.
Methods
We rigorously assessed DUP and other pertinent variables in 180 predominantly African American, low-income, and socially disadvantaged first-episode psychosis patients hospitalized in five psychiatric units.
Results
Mode of onset of psychosis, prior incarceration, and the level of childhood/adolescent maltreatment were all significant independent predictors of DUP. Regarding premorbid substance use, having ever used cannabis and the amount of premorbid alcohol use were significantly associated with DUP. None of the seven neurocognitive domains were even modestly, or clinically meaningfully, associated with DUP.
Conclusions
These and other findings on DUP may be informative for early detection and intervention services. For example, such services might benefit from special outreach to criminal justice settings and disadvantaged neighborhoods, and to young people likely to have a history of childhood/adolescent maltreatment and gradually developing psychotic symptoms.
Keywords: childhood maltreatment, duration of untreated psychosis, first-episode psychosis, psychosis, schizophrenia, treatment delay
1. Introduction
Duration of untreated psychosis (DUP), or the period of treatment delay between onset of psychotic symptoms and treatment initiation, is associated with poorer outcomes of psychotic disorders (Marshall et al., 2005; Perkins et al., 2005). Related to this, early detection and intervention services are being implemented in many countries (Birchwood et al., 2002; Edwards and McGorry, 2002; Compton et al., 2008b). Longer DUP is a predictor of poorer outcomes in terms of greater positive symptom severity, lower remission rates, and greater functional impairment; however, whether DUP is causally related to, or only a marker of, poorer outcomes remains unclear (McGlashan, 2008). Aside from knowledge of DUP as a predictor of outcomes, less is known about predictors of DUP itself, especially regarding socio-environmental factors and premorbid substance use. Additionally, there is a prominent dearth of research on treatment delay among young African Americans with emerging psychotic disorders. In fact, aside from our own studies, we are unaware of other research that focuses on this population. In our prior independent sample, we found that DUP is predicted by mode of onset of psychosis, living below the federal poverty level, poor family functioning, not having health insurance, the family’s report of financial problems, and the family’s report of barriers to seeking care (Compton et al., 2009a; Compton et al., 2009b; Compton et al., 2011). In the present study, we extend this line of research by studying additional hypothesized predictors of treatment delay in another sample comprised predominantly of African Americans. A somewhat unresolved question is whether DUP is associated with neurocognition, which is increasingly recognized as a crucial domain of early-course psychotic disorders.
Predictors of DUP are known to exist at the patient/illness-, family-, and health-services levels (Compton et al., 2008a; Compton et al., 2009a; Compton et al., 2009b; Compton & Broussard, 2011; Compton et al., 2011). For example, patient/illness-level predictors include single marital status (Pek et al., 2006), living in poverty (Compton et al., 2011), greater negative symptoms (Boonstra et al., 2012), and perhaps most importantly, a more gradual mode of onset of psychosis (Compton et al., 2008a). However, little evidence exists on other patient-level factors, such as childhood maltreatment, as well as macro-level factors like neighborhood disarray. Furthermore, relatively little is known about the impact of substance use on DUP. Though studies have been limited, in a meta-analysis, Burns (2012) found no significant differences in DUP between cannabis users and non-users, or between those using and not using substances in general.
A potential association between longer DUP and poorer neurocognitive functioning has been of interest during the past decade. If proven, it might support the notion that untreated psychosis is somehow neurotoxic, and serve to explain the well-established association between DUP and functional outcomes (Perkins et al., 2005). Cognitive dysfunction is also a plausible risk factor for lengthening DUP, by attenuating illness recognition or hindering capacity to complete tasks necessary to initiate treatment. Over a dozen studies to date have examined the association between DUP and neurocognition. For example, in their meta-analysis, Perkins and colleagues (2005) noted eight studies investigating correlations between DUP and cognitive functioning in various domains. While findings were mixed, several larger studies did not find an association, and most subsequent inquiries also have not (Barnes et al., 2008; Goldberg et al., 2009; Malla et al., 2011; Rund et al., 2007), though exceptions exist. Longer DUP might be associated with impaired performance in verbal IQ, verbal learning, and verbal working memory (Lappin et al., 2007), and memory and pre-attentional visual tasks (Cuesta et al., 2012). The Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) Consensus Cognitive Battery (MCCB; Neuchterlein et al., 2008), which we administered in this study, offers a comprehensive approach to measuring neurocognition in schizophrenia, and thus testing associations between neurocognition and DUP.
In light of limited research on predictors of DUP, including socio-environmental adversity (e.g., maltreatment and neighborhood disorder in childhood/adolescence), insufficient study of pre-illness substance use as a potential determinant of DUP, and inconclusive findings on the association between DUP and neurocognition, we rigorously measured DUP and other key variables and conducted three sets of analyses. First, we examined demographic and clinical variables, as well as premorbid functioning, childhood maltreatment, and neighborhood disorder, in predicting DUP. Second, we assessed the potential influence of premorbid alcohol and cannabis use on DUP. Both analyses considered the effect of mode of onset of psychosis given its known role as a determinant of DUP (Compton et al., 2008a). Third, we examined correlations between DUP and diverse neurocognitive domains assessed with the MCCB. Given the extent of negative findings to date, the third aim of our study is admittedly the least interesting. Nonetheless, due to some positive findings, we wanted to assess any possible associations in light of our rigorous measurement of DUP and thorough ratings of neurocognition. Additionally, none of the previous studies have focused on African Americans.
2. Methods
2.1. Setting and Sample
Consecutively admitted first-episode psychosis patients were enrolled from five inpatient psychiatric units, three in Atlanta, Georgia, and two in Washington, D.C., all primarily serving low-income, and socially disadvantaged patients with no insurance or with public-sector insurance. The majority of participants were male (135, 75%), and the mean age was 24.2 ± 4.9 years (range: 18–39). Furthermore, most participants were African American (154, 85.6%), with less than ten percent being Caucasian (15, 8.3%), only two percent being Asian (4, 2.2%), and four percent being “other” such as Native American (7, 3.9%).
Patients were excluded if they: (1) were not English-speaking, (2) did not have a diagnosis of a primary non-affective psychotic disorder, (3) were outside the range of 18–40 years, (4) had known or suspected mental retardation, (5) had a Mini-Mental State Examination (Folstein et al., 1975; Cockrell and Folstein, 1988) score of <24, (6) had received >3 months of prior antipsychotic treatment, (7) had been hospitalized >3 months prior to index admission, (8) had a significant medical condition compromising ability to participate, or (9) were unable to provide informed consent.
2.2. General Procedures
Trained masters- or doctoral-level assessors conducted research assessments once psychotic symptoms were stabilized sufficiently for informed consent and participation. When possible, assessments were conducted with family members/informants to provide collateral information on select variables. This information was used, in addition to participant data, when arriving at consensus-based best estimates for some of the below measures. Study procedures were approved by all relevant Institutional Review Boards.
2.3. Measures and Rating Scales
Diagnoses were made using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; First et al., 1998). An adapted version of the Family Interview for Genetic Studies (FIGS)—an interview guide for obtaining diagnostic information on family members (Maxwell, 1992)—was completed with patients and one or two informants when available (if they were a family member or spouse) to establish presence or absence of a psychotic disorder in first-degree relatives. Mode of onset of psychosis was categorized into five types defined by the World Health Organization’s International Pilot Study of Schizophrenia (Jablensky et al., 1992) and then trichotomized as acute, subacute, and chronic. A consensus-based estimate of mode of onset of psychosis was rated only when it could be accurately judged (Compton et al., 2008a).
Age at onset of psychosis and DUP (the latter operationalized as duration in weeks from onset of hallucinations/delusions to first hospital admission) were determined using the Symptom Onset in Schizophrenia (SOS) inventory (Perkins et al., 2000). We used the SOS criteria to determine when hallucinations and/or delusions met the threshold for psychosis. The consensus-based date identifies the onset of symptoms, specifically when the severity of the symptom met clinical criteria, and the symptom occurred often enough to meet or exceed the required frequency. Hallucinations are defined as “a sensory perception that has the compelling sense of reality of a true perception but that occurs without external stimulation of the relevant sensory organ… must last more than several minutes, occur multiple times a day, or affect more than one sensory modality.” Delusions are defined as “a false belief based on incorrect inference about external reality that is firmly sustained despite what almost everyone else believes and despite what constitutes incontrovertible and obvious proof or evidence to the contrary…” In order to date the onset of hallucinations or delusions, the symptom must have occurred repeatedly, and at a minimum of at least “2-sporadically.” A rating of “2-sporadically” is defined as “the symptom has occurred more than four times within one year. A rating of “3-recurrent” is defined as “has had the symptom at least half of the time and the symptom has persisted at least three consecutive months. A rating of “4-continuous” is given when the person “has had the symptom everyday or almost everyday continuously up to the initial treatment contact.” Prior reports describe our standardized approach to using the SOS and deriving age at onset and DUP using consensus-based best-estimate methods (Compton et al., 2008a; Compton et al., 2009a; Compton et al., 2009b; Compton et al., 2011).
The Premorbid Adjustment Scale (PAS) is the most widely used, reliable, and valid (Cannon-Spoor et al., 1982; Brill et al., 2008) measure of premorbid functioning among individuals with schizophrenia. To conservatively ensure that premorbid, and not prodromal, functioning was assessed, we did not rate functioning in any of the three age periods if prodromal or psychotic symptoms began during or within one year of that period (Monte et al., 2008).
The 28-item Childhood Trauma Questionnaire–Short Form (CTQ-SF) measures childhood maltreatment (emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect) with acceptable internal consistency and test-retest reliability, as well as convergent and discriminant validity (Bernstein et al., 1994; Bernstein et al., 2003). The Neighborhood Disorder Scale (NDS; Ross and Mirowsky, 1999), known to have good reliability and validity, was adapted to assesses adolescent experiences with neighborhood-level adversity; i.e., regarding the neighborhood where participants resided for the longest period during ages 12–18 years. The Lifetime Substance Use Recall (LSUR) assesses premorbid alcohol and cannabis use (Ramsay et al., 2011). This interviewer-administered questionnaire—guided by a timeline filled out collaboratively with the participant to enhance recall—collects data on all substances used during each year from first use until hospitalization. Total estimated premorbid “dosages” of alcohol and cannabis were calculated.
Seven cognitive domains were assessed with the MCCB (Kern et al., 2008; Neuchterlein et al., 2008). Cognitive domains included: (1) visual and verbal processing speed (Category Fluency Test, Trail Making Test (TMT), and Brief Assessment of Cognition in Schizophrenia (BACS) symbol coding subtest), (2) verbal learning (Hopkins Verbal Learning Test–Revised (HVLT-R)), (3) visual learning (Brief Visuospatial Memory Test–Revised (BVMT-R)), (4) verbal working memory (Letter Number Sequencing (LNS)), (5) visuospatial working memory (Wechsler Memory Scale, third edition (WMS-III) block design subtest), (6) reasoning and problem solving (Neuropsychological Assessment Battery (NAB) mazes subtest), and (7) sustained attention and vigilance (Continuous Performance Test–Identical Pairs (CPT-IP)).
2.4. Data Analyses
Analyses were conducted using log-transformed DUP, though for ease of reading below, results are given using “DUP” rather than “log(DUP)” terminology. Bivariate analyses relied on Pearson correlations and Student’s t-tests. Significant predictors in bivariate analyses were entered into multiple linear regressions; final models were arrived at using stepwise backward elimination. All analyses were conducted using IBM SPSS Statistics 18.0.
3. Results
3.1. Sample Characteristics
Participants’ diagnoses include: schizophrenia, paranoid type (79, 43.9%); psychotic disorder not otherwise specified (25, 13.9%); schizophreniform disorder (22, 12.2%); schizophrenia, undifferentiated type (20, 11.1%); schizoaffective disorder, depressive type (18, 10%); schizophrenia, disorganized type (6, 3.3%); schizoaffective disorder, bipolar type (5, 2.8%); delusional disorder (3, 1.7%); and brief psychotic disorder (2, 1.1%). Basic demographic and clinical characteristics are given in Table 1.
Table 1.
Select Demographic and Clinical Sample Characteristics (n=180)
| Continuous Variables | mean | SD |
| Age | 24.2 | 4.9 |
| Age at onset of psychosis | 21.2 | 5.3 |
| Years of school completed | 11.8 | 2.1 |
| Categorical Variables | n | % |
| Ethnicity | ||
| African American | 154 | 85.6% |
| Caucasian | 15 | 8.3% |
| Other | 7 | 3.9% |
| Asian | 4 | 2.2% |
| Gender, male | 135 | 75.0% |
| Marital status, single and never married | 161 | 89.4% |
| Unemployed in the month prior to hospitalization | 123 | 68.3% |
| Living with family members in the month prior to hospitalization | 115 | 63.9% |
| History of incarceration (n=179) | 102 | 57.0% |
| Living below the federal poverty level (n=149) | 65 | 43.6% |
| First-degree family history of schizophrenia or psychosis (n=173) | 34 | 19.7% |
| Mode of onset of psychosis (n=142) | ||
| Acute | 58 | 40.8% |
| Subacute | 20 | 14.1% |
| Chronic | 64 | 45.1% |
3.2. Demographic, Clinical, and Socio-Environmental Predictors of DUP
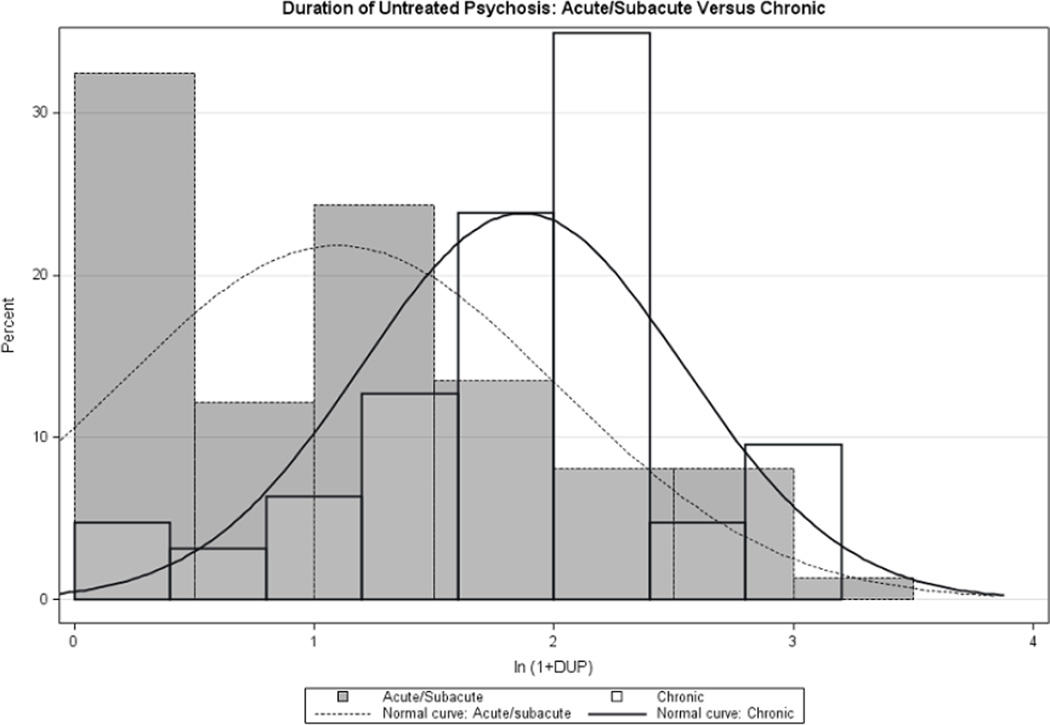
One of the strongest predictors of DUP is mode of onset of psychosis (acute, subacute, chronic): F(2, 139)=16.26, p<.0005, with medians of 11.2, 16.9, and 71.9 weeks, respectively. However, post-hoc tests revealed that the acute and subacute categories were not distinguishable statistically (SNK test of harmonic means, p=0.339). Figure 1 shows distributions of log(DUP) values for acute/subacute and chronic modes of onset. Age at onset of psychosis was significantly negatively associated with DUP (r=−.26, p<.001). Years of school completed, gender, marital status, employment status, and living below the federal poverty level were not significantly related to DUP. Living with family members in the month before hospitalization was significantly associated with DUP, as was history of incarceration. Specifically, participants living with family members had a shorter DUP compared to those living alone or with others (t=2.95, df=178, p=.004; to facilitate interpretation, median DUP values in these two groups were 24.1 and 60.0 weeks, respectively). Those previously incarcerated had a longer DUP (t=3.12, df=177, p=.002; median DUP values of 49.9 and 19.5 weeks, respectively). Having a first-degree family history of psychosis was not significantly related to DUP.
Figure 1.
Distributions of log(DUP) Values for Acute/Subacute and Chronic Modes of Onset
Correlations between premorbid functioning domains and DUP are shown in Table 2. The only correlation to reach statistical significance pertained to the childhood summary score (r=.17, p=.03), which takes into account both academic and social adjustment during ages 6–11. This childhood premorbid functioning summary score was used in subsequent analyses.
Table 2.
Correlations between Premorbid Functioning Domains and DUP
| Age Period | Academic Adjustment |
Social Adjustment |
Summary Score |
|---|---|---|---|
| Childhood, ages 6–11 (n=162) | .12 | .15 | .17* |
| Early adolescence, ages 12–15 (n=132) | .15 | .12 | .16 |
| Late adolescence, ages 16–18 (n=87) | .03 | .04 | .04 |
p=.03
Correlations between childhood maltreatment domains and DUP are given in Table 3. All domains except physical neglect were significantly associated with DUP, r=.18–.25. The correlation between the total CTQ-SF score and DUP was r=.26 (p=.001), and this summary score was used in subsequent analyses. Lastly, neighborhood disorder was significantly correlated with DUP (r=.25, p=.001).
Table 3.
Correlations between Childhood Maltreatment Domains and DUP
p<.05
p≤.001
Given the above bivariate associations, six predictors were entered into a linear regression model—age at onset of psychosis, not living with family members, history of incarceration, childhood premorbid functioning score, CTQ-SF score, and NDS score—to eliminate redundant sources of variance. Of note, correlations among these predictors were checked to avoid problems with multi-collinearity; all correlations were <.40, with the strongest correlations being between CTQ-SF and NDS scores (r=.37, p<.001) and between CTQ-SF and childhood premorbid functioning scores (r=.34, p<.001). All other inter-correlations ranged r=.01–.26. After stepwise backward elimination, the remaining independent predictors were: not living with family members, history of incarceration, and CTQ-SF score. This model accounted for 9.2% of variance in DUP. We then tested to see if any of these independent predictors altered the association with mode of onset of psychosis (the sample size thus being reduced to n=122 because mode could not be accurately determined in all cases). Mode of onset, incarceration, and CTQ-SF score remained significant, but living situation was no longer an independent predictor of DUP. This model accounted for 31.6% of variance in DUP.
3.3. Substance Use Variables as Predictors of DUP
Our second set of analyses assessed the potential influence of premorbid alcohol and cannabis use on DUP. Because some participants had not used these substances premorbidly (thus resulting in a substantial frequency of zeros in our “premorbid dosages” of alcohol and cannabis use variables), these concepts were represented in each case by a pair of variables: (1) use/nonuse and (2) amount of use among users. Specifically, while the use/nonuse variables are stand-alone predictors, total estimated amounts of premorbid use can only be assessed with use/nonuse in the model. After a stepwise backward elimination process, both alcohol and cannabis intake were shown to be predictors of DUP, with any cannabis use and the amount of alcohol use significantly associated with DUP. This accounted for 9.4% of the variance in DUP. We then tested to see if controlling for these predictors affected the association with mode of onset of psychosis. Mode of onset and both substance use predictors remained significant (with the combined predictors accounting for 29.6% of variance in DUP).
3.4. Associations between DUP and MCCB Domains
Correlations between DUP and seven neurocognitive domains revealed no significant or even modestly clinically meaningful associations: (1) visual and verbal processing speed (category fluency, r=.13; TMT, r=−.02; BACS symbol coding, r=.02); (2) verbal learning (HVLT-R, r=.03); (3) visual learning (BVMT-R, r=.06); (4) verbal working memory (LNS, r=− .00); (5) visuospatial working memory (WMS-III block design, r=−.00); (6) reasoning and problem solving (NAB mazes, r=.05); and (7) sustained attention/vigilance (CPT-IP, r=.03).
4. Discussion
Using a rigorous approach to measuring DUP and other constructs of interest in a relatively large sample of well-characterized first-episode psychosis patients, we addressed three unresolved issues pertaining to DUP. First, we found that factors such as history of incarceration and childhood/adolescent maltreatment are indeed predictors, even when considering the strong main effect of mode of onset of psychosis. Furthermore, in bivariate tests, neighborhood disorder during adolescence was a meaningful predictor. Second, we verified an association between premorbid substance use and DUP, again independent of the main effect of mode of onset. Third, we confirmed that DUP is unassociated with diverse neurocognitive domains.
As expected, mode of onset of psychosis is a potent predictor of DUP. As we measure it, mode of onset refers to the pace at which psychotic symptoms evolve before they reach a threshold of frank psychosis; once onset of frank psychosis has occurred (and mode of onset has thus established itself), DUP begins. The strong association between mode of onset and duration of treatment delay is probably present in diverse medical conditions. To give one example, if we consider frank pain in the right lower abdomen to be 5/10 on a pain scale, pain reaching that threshold acutely is likely to prompt fairly immediate help-seeking, whereas pain reaching a 5/10 gradually is likely to be related to a longer treatment delay. Although mode of onset accounts for a substantial portion of variance in DUP, we established several new patient-level predictors of DUP. Having been previously incarcerated is associated with a longer DUP. For the first time, we document that childhood maltreatment is associated with longer treatment delay, in some cases years after such maltreatment occurs. This adds to the extensive literature on the detrimental effects of adverse early life experiences across diverse mental and physical health domains (Felitti et al., 1998; Anda et al., 2006). Together, these findings have implications for early detection and intervention services; for example, special outreach attention might be warranted for young people in criminal justice settings and for families in disadvantaged neighborhoods.
Although most of the limited studies examining DUP among cannabis users and nonusers report a shorter DUP in users (Burns, 2012), we found associations between substance use and a longer DUP. In addition to well-documented associations between cannabis use and poorer outcomes of psychotic disorders (Ramsay and Compton, 2011), these results indicate that premorbid substance use may also contribute to longer treatment delays. Longitudinal studies should clarify the nature of relations among premorbid cannabis use, age at onset, DUP, and other early-course features.
Our third analysis adds to a body of literature rejecting the notion that cognitive impairment is either the result of, or a risk factor for, treatment delays (Barnes et al., 2008; Goldberg et al., 2009; Malla et al., 2010; Perkins et al., 2005; Rund et al., 2007). We found no meaningful associations whatsoever between DUP and seven MCCB-based neurocognitive domains. Longitudinal studies of patients after their first-episode (Rund et al., 2007) and of individuals at ultra-high risk who later developed psychosis (Becker et al., 2010) found that cognitive functioning is already impaired when first symptoms emerge and may not deteriorate further during the early course. These impairments do not appear to hinder treatment-seeking, suggesting that other variables, such as patient/illness-related, familial, and socio-environmental factors, are more influential.
At least two methodological limitations should be considered in interpreting our findings. First, given the narrow sociodemographic and clinical characteristics of our sample, generalizability of these findings to dissimilar first-episode samples in different settings is limited. However, there is a prominent dearth of research on treatment delay among young African Americans with emerging psychotic disorders. In fact, aside from our own studies, we are unaware of other research that focuses on this understudied and underserved population. There is limited research on DUP in any population, especially the African American population, and the relative homogeneity of our sample enhances internal validity of results. Second, because mode of onset of psychosis could not be confidently rated for all participants, the sample sizes for models including mode of onset were smaller (n=122 rather than n=180). Yet, our rigorous method of rating mode of onset, and our convention of not rating it when we cannot confidently do so, enhances validity of this crucial variable.
Treatment delay is a complex behavioral phenomenon driven by diverse factors, including illness-related predictors (e.g., mode of onset of psychosis, age at onset, premorbid functioning), patient-related issues (e.g., with whom one lives, history of incarceration, premorbid substance use), family-related factors such as family coping (Compton et al., 2009a), health system-level variables like health insurance status (Compton et al., 2009b), and, now, socio-environmental factors such as abuse and neglect during childhood/adolescence, and even neighborhood disorder. Uncovering such determinants is of importance to early intervention services seeking to reduce DUP.
Acknowledgements
The authors express gratitude to the participants involved in this study and the clinicians at the referral sites who identified eligible and interested patients. Research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health under Award Number R01MH081011. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Role of the Funding Source
The funding source had no role in data analyses, the writing of the manuscript, or the decision to submit it for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
The authors know of no conflicts of interest pertaining to this research.
Contributors
All authors contributed to the conceptualization and writing of this article, and all approved the final article for publication.
References
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, Dube SR, Giles WH. The enduring effects of abuse and related adverse experiences in childhood: a convergence of evidence from neurobiology and epidemiology. Eur. Arch. Psychiatry Clin. Neurosci. 2006;256:174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes TR, Leeson VC, Mutsatsa SH, Watt HC, Hutton SB, Joyce EM. Duration of untreated psychosis and social function: 1 year follow-up study of first-episode schizophrenia. Br. J. Psychiatry. 2008;193:203–209. doi: 10.1192/bjp.bp.108.049718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker HE, Nieman DH, Wiltink S, Dingemans PM, van der Fliert JR, Velthorst E, de Haan L, van Amelsvoort TA, Linszen DH. Neurocognitive functioning before and after the first psychotic episode: does psychosis result in cognitive deterioration? Psychol. Med. 2010;40:1599–1606. doi: 10.1017/S0033291710000048. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, Sapareto E, Ruggiero J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am. J. Psychiatry. 1994;151:1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D, Zule W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27:169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Birchwood M, Fowler D, Jackson C. Early Intervention in Psychosis: A Guide to Concepts, Evidence and Interventions. Chichester, West Sussex, England: John Wiley & Sons; 2002. [Google Scholar]
- Boonstra N, Klaassen R, Sytema S, Marshall M, De Haan L, Wunderink L, Wiersma D. Duration of untreated psychosis and negative symptoms – a systematic review and meta-analysis of individual patient data. Schizophr. Res. 2012;142:12–19. doi: 10.1016/j.schres.2012.08.017. [DOI] [PubMed] [Google Scholar]
- Brill N, Reichenberg A, Weiser M, Rabinowitz J. Validity of the Premorbid Adjustment Scale. Schizophr Bull. 2008;34:981–983. doi: 10.1093/schbul/sbm128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns JK. Cannabis use and duration of untreated psychosis: a systematic review and meta-analysis. Curr. Pharm. Des. 2012;18:5093–5104. doi: 10.2174/138161212802884672. [DOI] [PubMed] [Google Scholar]
- Cannon-Spoor HE, Potkin SG, Wyatt RJ. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr. Bull. 1982;8:470–484. doi: 10.1093/schbul/8.3.470. [DOI] [PubMed] [Google Scholar]
- Cockrell JR, Folstein MF. Mini-Mental State Examination (MMSE) Psychopharmacol. Bull. 1988;24:689–692. [PubMed] [Google Scholar]
- Compton MT, Broussard B. Conceptualizing the multi-faceted determinants of the duration of untreated psychosis. Curr. Psychiatry Rev. 2011;7:1–11. [Google Scholar]
- Compton MT, Chien VH, Leiner AS, Goulding SM, Weiss PS. Mode of onset of psychosis and family involvement in help-seeking as determinants of duration of untreated psychosis. Soc. Psychiatry Psychiatr. Epidemiol. 2008a;43:975–982. doi: 10.1007/s00127-008-0397-y. [DOI] [PubMed] [Google Scholar]
- Compton MT, Gordon TL, Goulding SM, Esterberg ML, Carter T, Leiner AS, Weiss PS, Druss BG, Walker EF, Kaslow NJ. Patient-level predictors and clinical correlates of duration of untreated psychosis among hospitalized first-episode patients. J. Clin. Psychiatry. 2011;72:225–232. doi: 10.4088/JCP.09m05704yel. [DOI] [PubMed] [Google Scholar]
- Compton MT, Goulding SM, Gordon TL, Weiss PS, Kaslow NJ. Family-level predictors and correlates of the duration of untreated psychosis in African American first-episode patients. Schizophr. Res. 2009a;115:338–345. doi: 10.1016/j.schres.2009.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton MT, Goulding SM, Ramsay CE, Addington J, Corcoran C, Walker EF. Early detection and intervention for psychosis: perspectives from North America. Clinical Neuropsychiatry. 2008b;5:263–272. [PMC free article] [PubMed] [Google Scholar]
- Compton MT, Ramsay CE, Shim RS, Goulding SM, Gordon TL, Weiss PS, Druss B. Health services determinants of the duration of untreated psychosis among African-American first-episode patients. Psychiatr. Serv. 2009b;60:1489–1494. doi: 10.1176/ps.2009.60.11.1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuesta MJ, García de Jalón E, Campos MS, Ibáñez B, Sánchez-Torres AM, Peralta V. Duration of untreated negative and positive symptoms of psychosis and cognitive impairment in first episode psychosis. Schizophr. Res. 2012;141:222–227. doi: 10.1016/j.schres.2012.08.019. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationships of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (Clinical Version) SCID-I. Arlington, VA: American Psychiatric Publishing; 1997. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-Mental State: A Practical Method for Grading the Cognitive State of Patients for the Clinician. Oxford: Pergamon Press; 1975. [DOI] [PubMed] [Google Scholar]
- Goldberg TE, Burdick KE, McCormack J, Napolitano B, Patel RC, Sevy SM, Goldman R, Lencz T, Malhotra AK, Kane JM, Robinson DG. Lack of an inverse relationship between duration of untreated psychosis and cognitive function in first episode schizophrenia. Schizophr. Res. 2009;107:262–266. doi: 10.1016/j.schres.2008.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards J, McGorry PD. Implementing Early Intervention in Psychosis: A Guide to Establishing Early Psychosis Services. London: Martin Dunitz; 2002. [Google Scholar]
- Jablensky A, Sartorius N, Ernberg G, Anker M, Korten A, Cooper JE, Day R, Bertelsen A. Schizophrenia: manifestations, incidence and course in different cultures. A World Health Organization ten-country study. Psychol. Med. Monogr. 1992;(Suppl. 20):1–97. doi: 10.1017/s0264180100000904. [DOI] [PubMed] [Google Scholar]
- Kern RS, Nuechterlein KH, Green MF, Baade LE, Fenton WS, Gold JM, Keefe RS, Mesholam-Gately R, Mintz J, Seidman LJ, Stover E, Marder SR. The MATRICS Consensus Cognitive Battery, Part 2: Co-norming and standardization. Am. J. Psychiatry. 2008;165:214–220. doi: 10.1176/appi.ajp.2007.07010043. [DOI] [PubMed] [Google Scholar]
- Lappin JM, Morgan KD, Morgan C, Dazzan P, Reichenberg A, Zanellia JW, Fearon P, Jones PB, Lloyd T, Tarrant J, Farrant A, Leff J, Murray RM. Duration of untreated psychosis and neuropsychological function in first episode psychosis. Schizophr. Res. 2007;95:103–110. doi: 10.1016/j.schres.2007.05.037. [DOI] [PubMed] [Google Scholar]
- Malla AK, Bodnar M, Joober R, Lepage M. Duration of untreated psychosis is associated with orbital-frontal grey matter volume reductions in first episode psychosis. Schizophr. Res. 2011;125:132–120. doi: 10.1016/j.schres.2010.09.021. [DOI] [PubMed] [Google Scholar]
- Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch. Gen. Psychiatry. 2005;62:975–983. doi: 10.1001/archpsyc.62.9.975. [DOI] [PubMed] [Google Scholar]
- Maxwell ME. Clinical Neurogenetics Branch, Intramural Rsearch Program. National Institute of Mental Health; 1992. Manual for the FIGS. [Google Scholar]
- McGlashan TH. Premorbid adjustment, onset types, and prognostic scaling: still informative? Schizophr. Bull. 2008;34:801–805. doi: 10.1093/schbul/sbn073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monte RC, Goulding SM, Compton MT. Premorbid functioning of patients with first-episode nonaffective psychosis: a comparison of deterioration in academic and social performance, and clinical correlates of Premorbid Adjustment Scale scores. Schizophr. Res. 2008;104:206–213. doi: 10.1016/j.schres.2008.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, Essock S, Fenton WS, Frese FJ, Gold JM, Goldberg T, Heaton RK, Keefe RS, Kraemer H, Mesholam-Gately R, Seidman LJ, Stover E, Weinberger DR, Young AS, Zalcman S, Marder SR. The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am. J. Psychiatry. 2008;165:203–213. doi: 10.1176/appi.ajp.2007.07010042. [DOI] [PubMed] [Google Scholar]
- Pek E, Mythily S, Chong SA. Clinical and social determinants of duration of untreated psychosis in first-episode psychosis patients. Ann. Acad. Med. Singapore. 2006;35:24–26. [PubMed] [Google Scholar]
- Perkins DO, Gu H, Boteva K, Lieberman JA. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am. J. Psychiatry. 2005;162:1785–1804. doi: 10.1176/appi.ajp.162.10.1785. [DOI] [PubMed] [Google Scholar]
- Perkins DO, Leserman J, Jarskog LF, Graham K, Kazmer J, Lieberman JA. Characterizing and dating the onset of symptoms in psychotic illness: the Symptom Onset in Schizophrenia (SOS) inventory. Schizophr. Res. 2000;44:1–10. doi: 10.1016/s0920-9964(99)00161-9. [DOI] [PubMed] [Google Scholar]
- Ramsay CE, Abedi GR, Marson JD, Compton MT. Overview and initial validation of two detailed, multidimensional, retrospective measures of substance use: The Lifetime Substance Use Recall (LSUR) and Longitudinal Substance Use Recall for 12 Weeks (LSUR-12) Instruments. J. Psychiatr. Res. 2011;45:83–91. doi: 10.1016/j.jpsychires.2010.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsay CE, Compton MT. The interface of cannabis misuse and schizophrenia-spectrum disorders. In: Ritner MS, editor. Handbook of Schizophrenia Spectrum Disorders, Volume III: Therapeutic Approaches, Comorbidity, and Outcomes. New York: Springer; 2011. pp. 289–320. [Google Scholar]
- Ross CE, Mirowsky J. Disorder and decay: The concept and measurement of perceived neighborhood disorder. Urban Aff. Rev. 1999;34:412–432. [Google Scholar]
- Rund BR, Melle I, Friis S, Johannessen JO, Larsen TK, Midbøe LJ, Opjordsmoen S, Simosen E, Vaglum P, McGlashan T. The course of neurocognitive functioning in first-episode psychosis and its relation to premorbid adjustment, duration of untreated psychosis, and relapse. Schizophr. Res. 2007;91:132–140. doi: 10.1016/j.schres.2006.11.030. [DOI] [PubMed] [Google Scholar]