Abstract
Young men who have sex with men (YMSM) are at alarming risk for HIV acquisition, demonstrating the highest rates of incident infection of any age-risk group. GRINDR is a global positioning service-based social networking application popular with YMSM for sexual partnering. To assess the characteristics of YMSM who use GRINDR, we conducted a computer-assisted self-interview-based survey of 375 YMSM using GRINDR in metropolitan Los Angeles, recruited using the GRINDR platform. The median age was 25 (interquartile range, 22–27) years old, 42.4 % caucasian, 6.4 % African American, 33.6 % Latino, and 14.1 % Asian/Pacific Islander. Participants reported high rates of sexual partnering and unprotected anal intercourse (UAI). The majority (70 %) of those reporting unprotected anal intercourse reported low perception of HIV-acquisition risk. Of the participants, 83.1 % reported HIV testing within the past 12 months; 4.3 % had never been HIV tested. Of the participants, 4.5 % reported HIV-positive serostatus; 51.7 % indicated that they would be interested in participating in a future HIV prevention trial. Latinos were more likely than either caucasians or African Americans to endorse trial participation interest (odds ratio, 1.9; 95 % confidence interval [1.1–3.3]). HIV-positive test results were associated with increased number of anal sex partners in the past 3 months (adjusted odds ratio (AOR), 1.53 [0.97–2.40]), inconsistent inquiry about partners’ serostatus (AOR, 3.63 [1.37–9.64]), reporting the purpose for GRINDR use including “friendship” (AOR, 0.17 [0.03–1.06), and meeting a sexual partner in a bookstore in the past 3 months (AOR, 33.84 [0.99–1152]). Men recruited via GRINDR were high risk for HIV acquisition or transmission and interested in clinical trial participation, suggesting potential for this method to be used for recruitment of YMSM to HIV prevention trials.
Keywords: Sexual risk behavior, HIV prevention, Education, Study recruitment
Background
Men who have sex with men (MSM) account for 61 % of incident HIV infections in the USA, totaling over 30,000 new HIV infections annually. MSM are over 40 times more likely to be HIV-infected than the general population.1 Young MSM (YMSM) age 13–29 have the highest HIV incidence rate of any age-risk population segment and represent the only risk group with an increase in incidence from 2006 to 2009 and disproportionately so for young African American and Latino MSM.2 In Los Angeles County, MSM represent 84 % of newly diagnosed HIV infections.3
In the USA, 93 % of young adults own a cell phone; 65 % of young adults access the Internet via their cell phones. Seventy-two percent of online young adults report using social networking sites, and 48 % access these sites via their cell phones. African Americans outpace Caucasian and English-speaking Latino counterparts in mobile internet usage.4,5
Young MSM are technologically savvy6 and have adopted Internet-based services to facilitate sexual partnering. Sexually transmitted infections (STIs) have been traced through electronic social networks,7 and some studies suggest an increase in numbers of sexual partners and STIs/HIV among those who seek partnerships via the Internet.8,9 A variety of electronic methods have also been used to characterize, survey, and recruit young MSM into research protocols, and the ways such populations are similar to, and distinct from conventional recruitment and survey methods have been characterized.10–13
GRINDR is a smartphone application (“app”) used by MSM to facilitate sexual partnering. GRINDR uses global positioning service (GPS) capability to identify other app users, sorting users by current (or last identified) proximity. GRINDR launched in March 2009 and currently maintains over 1.5 million user profiles; GRINDR reports estimated daily traffic of 250,000 users and approximately 3,000 new users per day. There are approximately 45,000 GRINDR users in the City of Los Angeles. GRINDR members’ profiles contain a photograph and demographic data, along with a user-created tag line, and are displayed in order of proximity to the user. Recently, “advertising blasts” on the GRINDR platform were successfully used to recruit participants for a rectal microbicide acceptability study.10 No data are currently available to understand the behaviors associated with GRINDR use, nor the GRINDR (and more generally the “mobile app”) universe as a risk environment.
We employed the GRINDR application to recruit young MSM to a computer-assisted self-interview (CASI) to characterize the epidemiology, sexual risk behaviors, HIV serostatus and testing behavior, and uptake of biomedical HIV prevention strategies among young MSM who use GRINDR in metropolitan Los Angeles, CA, USA. We additionally sought to determine the feasibility of using GPS-based social networking apps to engage YMSM in HIV prevention studies.
Methods
Study Design
A CASI-based survey was administered to participants in field-based settings using a web-enabled tablet computer. Participants were eligible to participate if they were self-reported to be over 18 years old and used the GRINDR platform via their smartphone. Repeat survey participation was not allowed and screened for via logs maintained of GRINDR profiles using unique identifier codes. The UCLA Institutional Review Board provided regulatory oversight for and reviewed all procedures and documents associated with study conduct.
Assessments
The questionnaire included 37 items, modified from the National HIV Behavioral Survey (NHBS), and including face-valid assessments for GRINDR-focused questions that were piloted with a population of four research assistants and key informants. The research assistants were bachelors- and masters-level volunteers from a pool of individuals who had volunteered in research or outreach capacities at the UCLA CARE Center previously. Key informants were a convenience sample of community contacts of the staff and volunteers of the CARE Center. Assessment items parsed into nine domains: Demographics, HIV Testing Behavior, Sexually Transmitted Disease History, Sexual Risk Behavior, Drug/Alcohol Use, HIV-Related Attitudes/Beliefs, Prevention Strategies, Clinical Trial Participation, and GRINDR use. The questionnaire was programmed onto a secure server for Internet-based administration using a mobile data connection-enabled tablet computer.
Territory Mapping
The City of Los Angeles and its surrounding areas were mapped using an iterative process. An Internet search was performed for MSM-focused/themed venues within the City of Los Angeles. Key informants from the target population of young MSM were then convened to review the results of the Internet search and amend the list based on locations they or their friends would be likely to frequent. Additionally, key informants provided days of the week and times for maximizing attendance at individual locations, creating venue–date–time (VDT) units. Over a 2-month period, key informants refined the map list, which included bars, dance clubs, commercial sex venues, public locations (parks, alleys, beaches, and malls), restaurants, and special events. Research staff then attended each VDT unit (provided that it was not a special event) to confirm its appropriateness (defined as proximate men on the GRINDR platform). Mapping was revised monthly based on research team field experience and monthly reassessment with the key informants. Nonproductive VDT units were removed, and new VDT units added at each revision. The mapped list of VDT units was revised a total of five times during study conduct. On a monthly basis, the number of VDT units from which random selection took place ranged from 68 to 143. Productive locations were determined based on hit rates alone (ratio of enrolled vs. non-enrolled individuals contacted via GRINDR’s chat feature).
Participant Recruitment
At each VDT unit, teams of two research assistants identified a safe location for study conduct. Study staff logged onto the GRINDR application using their own personal profiles. GRINDR users who self-identified as between 18 and 29 years old were then “messaged” in order of proximity to the study staff based on GRINDR’s GPS functionality. If a proximate GRINDR user was identified as having previously participated in the study, or previously refused participation, they were not recontacted. A standardized script was used in interactions with potential participants. Participants who, in the opinion of study staff, were sufficiently intoxicated or altered that they were unable to understand the research information sheet and/or provide appropriate assent to participation were not enrolled in the study.
Participants were administered the questionnaire on the tablet computer without assistance from research staff, unless so requested by the participant; research staff could not review participant responses. Upon completion of the questionnaire, participants were provided a $25 gift card.
While performing GRINDR-application-based recruitment, other VDT attendees, requesting to participate in the study, often approached study teams. If such participants were self-reported to be between the ages of 18 and 29 and were able to demonstrate the GRINDR application on their smartphone, such “walk-on” participants were allowed study participation.
Statistical Analysis
Summary statistics were used to report basic demographic information to characterize the study population and to summarize major study results. For bivariate analysis, simple logistic regression or two-way contingency tables were used to evaluate the association between variables. Multiple logistic regression analysis was used to evaluate the association between outcomes of interest and basic demographic variables. All p values are two-sided, and all analyses were performed using SAS version 9.2 (SAS, Cary, NC, USA).
Results
Participants
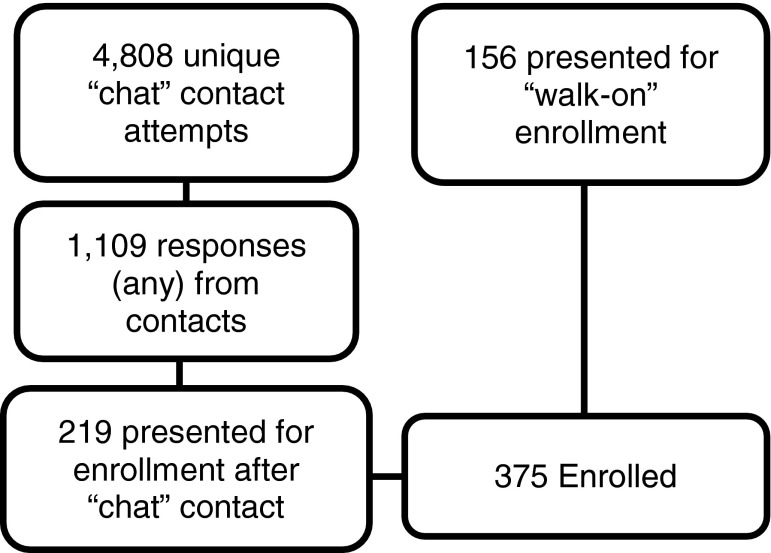
From October 2010 through March 2011, 4,808 unique GRINDR contacts were made, and 375 participants enrolled in the study, yielding an overall contact success rate of 8.7 %. When adjusted for the 156 participants who enrolled via the “walk-on” procedure, the contact success rate using the GRINDR messaging platform was 4.5 % (Fig. 1).
FIGURE 1.
Study recruitment.
Demographics of the study population are described in Table 1. Three hundred sixty-nine (98.4 %) study participants reported sexual intercourse or oral sex with a man in the past year. Thirty-seven (9.9 %) reported sex with a woman in the past year (YMSM/W); 36 of these YMSM/W also reported sex with a man in the past year. The demographics of this YMSM/W population was 10 (27.8 %) Caucasian, 5 (13.9 %) African American, 13 (36.1 %) Latino, 1 (2.8 %) Asian/Pacific Islander and 7 (19.4 %) mixed race. Details of study participants’ GRINDR usage are presented in Table 2.
Table 1.
Characteristics of MSM participants recruited in GRINDR-based survey
| Variable | Number (%) |
|---|---|
| Age | |
| 18–20 | 27 (7) |
| 21–24 | 191 (51) |
| 25–29 | 131 (35) |
| >29 | 26 (7) |
| Residence | |
| Los Angeles Metro (includes incorporated municipalities) | 239 (63.7) |
| Los Angeles County | 66 (17.6) |
| Surrounding counties | 49 (13.1) |
| Northern California | 10 (2.7) |
| Out-of-state | 9 (2.4) |
| Race/ethnicitya | |
| Caucasian | 159 (42.4) |
| Black/African American | 24 (6.4) |
| Latino (regardless of race) | 126 (33.6) |
| Asian/Pacific Islander | 53 (14.1) |
| Native American | 4 (1.1) |
| Mixed Race | 28 (7.5) |
| Other | 1 (0.3) |
aMultiple responses possible
Table 2.
GRINDR usage characteristics
| Variable | Number (%) |
|---|---|
| Duration of GRINDR membership/use | |
| <1 month | 39 (10.4) |
| 1–3 months | 35 (9.3) |
| 3 months–1 year | 125 (33.3) |
| > 1 year | 170 (45.3) |
| Frequency of logging in to GRINDR | |
| At least once a day | 228 (60.8) |
| More than once a week, but not every day | 77 (20.5) |
| Once a week | 26 (6.9) |
| Less often than once a week | 37 (9.9) |
| Purpose of GRINDR use (multiple responses possible) | |
| Friendship | 289 (77.1) |
| Dating | 252 (67.2) |
| One-on-one sex | 233 (62.1) |
| Group sex | 64 (17.1) |
| Phone sex | 22 (5.9) |
| Frequency of sexual partnering via GRINDR | |
| At least once a day | 6 (1.6) |
| More than once a week, but not every day | 20 (5.3) |
| Once a week | 29 (7.7) |
| Less often than once a week | 170 (45.3) |
| Do not use GRINDR for sexual partnering | 134 (35.9) |
| Quantity of friends who use GRINDR | |
| All | 25 (6.7) |
| Most but not all | 84 (22.4) |
| Many | 115 (30.7) |
| Some | 81 (21.6) |
| A few | 50 (13.3) |
| None | 11 (2.9) |
| Since beginning to use GRINDR, sex partners are | |
| More in number | 82 (21.9) |
| Closer to my age | 79 (21.1) |
| Live closer to me | 167 (44.5) |
| Easier to meet | 163 (43.5) |
| Are “more like me” | 61 (16.3) |
HIV/STI Testing and Serostatus
A total of 312 participants (83.2 %) reported an HIV test within the previous 12 months (“in-compliance” with CDC testing guidelines).14 Sixteen (4.3 %) had never been HIV tested even though 15 of these 16 participants reported anal intercourse in the previous 12 months. Sixteen (4.5 %) participants providing a history of HIV testing reported a positive HIV test, 337 (93.4 %) reported a negative HIV test, and 3 (0.1 %) never received their results. A prior diagnosis of gonorrhea, chlamydia, or syphilis was reported by 17.9, 13.6, and 9.1 % of participants, respectively.
Sexual Risk Behaviors
Participants reported a mean of 1.9 (SD 3.4) anal sex partners in the previous month, 3.8 (SD 7.2) in the previous 3 months, and 10.0 (SD 21.7) in the previous year; 46.1 and 38.9 % reported any unprotected anal intercourse (UAI) and any unprotected receptive anal intercourse (URAI), respectively, in the past 3 months. Caucasian participants, compared to African-American or Latino participants were significantly more likely to report both UAI (odds ratio (OR), 2.77; 95 % confidence interval (CI) [1.62–4.73], p < 0.001) and URAI (OR, 2.24 [95 %CI, 1.31–3.81], p = 0.003). Of those reporting UAI, 70 % reported believing that it was “unlikely” or “very unlikely” that they were ever going to acquire HIV infection. Of the participants, 52.8 % did not always ask sex partners about their HIV status. Participants met sexual partners in the previous 3 months via GRINDR (56 %), Internet sex-focused websites (40.5 %), through friends (44.3 %), at bars or dance clubs (37.1 and 33.3 %, respectively), Internet dating websites (25.1 %), at bathhouses or sex clubs (7.7 %), and at bookstores (1.6 %). Thirteen (3.7 %) participants reported having used postexposure prophylaxis (PEP) in the past, six participants reported having used pre-exposure prophylaxis (PrEP) for HIV prevention. Three of the participants reporting PrEP use were also reporters of prior PEP use.
Drug and Alcohol Use
One hundred eighty-one (48 %) of the participants reported drug or alcohol use during sex in the past month, and among those, 91.7 % reported alcohol use at the time of sex, 59.7 % marijuana use, 34.8 % amyl nitrate or other inhalants, 30.4 % ecstasy (MDMA), 27.1 % cocaine, and 14.4 % methamphetamine.
Clinical Trial/Research Participation
Forty-two participants (11.2 %) reported previous participation in a clinical trial or research study; 194 (51.7 %) indicated that they would be definitely interested in participating in a future HIV prevention study. In univariate analysis, YMSM of Latino ethnicity were significantly more likely to report interest in prevention study participation than non-Latinos (OR, 1.9; 95 % CI [1.1–3.3], p = 0.02). Fifty-four (14.4 %) indicated that they were categorically not interested in such a study.
Predictors of HIV Serostatus and Prior HIV Chemoprophylaxis Use
Multivariable analysis controlling for age, race, ethnicity, and location of residence was used to assess predictors of self-reporting an HIV-positive result and prior PEP or PrEP use. Compared to HIV-negative men, reporting an HIV-positive result on last test was associated with increased number of anal sex partners in the past 3 months (adjusted (AOR), 1.53 [0.97–2.40], p = 0.05), inconsistent inquiry about partners’ serostatus (AOR, 3.63 [1.37–9.64], p = 0.008), reporting the purpose for GRINDR use including “friendship” (AOR, 0.17 [0.03–1.06], p = 0.05), and meeting a sexual partner in a bookstore in the past 3 months (AOR 33.84 [0.99–1152]), p = 0.04. Compared to men who reported no use of HIV chemoprophylaxis, prior PEP or PrEP use was associated with reporting increased numbers of sex partners since beginning to use GRINDR (AOR, 4.7 [1.6–14.3], p = 0.006), meeting a sex partner at work in the past 3 months (AOR, 3.6 [1.1–12.2], p = 0.04), methamphetamine use at the time of sex in the past month (AOR, 5.8 [1.5–21.9], p = 0.01), and non-Latino ethnicity (AOR, 9.3 [1.1–76.9], p = 0.04).
Comparison to Other Surveys
The population reported numbers of anal sexual partners consistent with other behavioral surveillance studies recently completed among MSM in Los Angeles: the NHBS, a CDC-funded survey that began in 2003 and separately targets MSM, IDU, and high-risk heterosexual populations in areas with high HIV incidence and prevalence using time–space (venue)-based sampling; and the Web-based HIV Behavioral Surveillance Study (WHBS), a CDC effort using an Internet-based sampling strategy in six health jurisdictions using a “direct marketing” strategy on web-site banner ads. Subsets from Los Angeles of the NHBS and WHBS are compared to the current sample for key parameters in Table 3.
Table 3.
Comparison of GRINDR Survey Population to other LA-based MSM survey populations†
| WHBS (LA) | NHBS-MSM2 (LA) | GRINDR | |
|---|---|---|---|
| Year of survey | 2007 | 2008 | 2010–11 |
| N | 1234 | 537 | 375 |
| Age | |||
| 18–29, n (%) | 771 (62.5)** | 201 (37.4)** | 349 (93.1) |
| Race/ethnicity**, n(%) | |||
| Caucasian | 691 (56.0) | 172 (32.0) | 159 (42.4) |
| Black/AA | 85 (6.9) | 105 (19.6) | 24 (6.4) |
| Latino | 352 (28.5) | 189 (35.1) | 126 (33.6) |
| Sexual risk behavior | |||
| Partners, last 12 months, median | 5.0 | 4.0 | 4.0 |
| UAI, any, % (horizon) | 61 (12 m) | 53 (12 m) | 46 (3 m) |
| Self-report HIV+ | 118 (9.6)* | 67 (12.5)** | 16 (4.3) |
| HIV testing behavior | |||
| Never HIV tested | 218 (17.7)** | 26 (4.8) | 16 (4.3) |
| Tested in last 24 month | 840 (68)** | 399 (74.3)** | 340 (90.7) |
*p = 0.004; **p < 0.001
†Carlos J, Bingham TA. A comparison of risk behaviors reported by online versus in-person MSM in Los Angeles County. Abstract A17-4 presented at the National HIV Prevention Conference, Atlanta, GA, August 2009
Discussion
The domestic HIV epidemic is characterized by a concentration in vulnerable populations, including YMSM, particularly YMSM of color. Prevention-focused studies have found it challenging to recruit YMSM. We used the GPS-based social networking application GRINDR—a smartphone app used by MSM for sexual partnering—to recruit a sample of YMSM for behavioral surveillance and were able to implement the technology to facilitate a time–space sampling methodology for epidemiologic or behavioral surveillance.
The recruited sample roughly parallels the racial/ethnic distribution of Los Angeles County (LAC),15 allaying concern that the race/ethnicity profile of our sample would be biased by the availability of the GRINDR platform being limited to Apple devices (iPhone, iPad, and iPod Touch) in addition to biases imposed by internet-based survey techniques.13 Although during the course of study conduct, the GRINDR platform became available on some Blackberry devices, no participants were recruited via a Blackberry device-based GRINDR contact. To clarify the contribution of socioceconomic bias, we used inflation-adjusted 2000 census data to estimate the median household income for study participants based on reported zip code of residence. Participants were found to be above the median household income level of Los Angeles County in 2009 dollars ($35,929 vs. $26,983)—suggesting a potential bias toward a more affluent population in the Apple-product using study population. The GRINDR platform is currently additionally available on Android devices, which may potentially expand access to a much larger and more economically diverse population.
HIV prevalence rates in the GRINDR sample appear lower than those of the NHBS and WHBS samples. It is important to note that rates in our study approximate the self-report rates of known HIV infection in the NHBS sample. Although the GRINDR sample did not acquire any biologic specimens for HIV or STI testing, self-reports of HIV-positive serostatus almost universally underestimate the true seroprevalence rate16 attributable primarily to occult and undiagnosed HIV infection and secondarily to the persistent stigma associated with reporting an HIV-positive diagnosis among MSM.17
Participants demonstrated a high rate of ongoing transmission-associated risk behavior, indicating that the sample is an excellent target for recruitment for and ultimate deployment of HIV prevention studies and interventions, respectively. In particular, although participants reported low rates of previous clinical trial participation, more than half of participants noted that they would be interested in participating in a future HIV prevention study, with an additional 25 % indicating that they might be interested in participating, depending on the details of the study, incentives, and various other parameters. A minority categorically indicated that they were not interested in participating in such studies. As increased emphasis is placed on targeting expensive HIV prevention interventions that will involve combinations of chemoprophylaxis and behavioral interventions, mechanisms for accessing YMSM will be critical. It is therefore reassuring that individuals recruited via GRINDR appear to be largely amenable to clinical study participation.
We found a contradiction between perception of HIV acquisition risk and actual risk based on reported behavior: 70 % of the population who reported UAI thought it was “unlikely” or “very unlikely” that they would become HIV infected. Similarly, over one half of the sample did not always ask sex partners about their HIV status; HIV-infected persons were less likely to inquire about partners’ serostatus than HIV-uninfected persons. This suggests that, in this population, HIV-positive individuals may not be using serosorting to protect HIV-uninfected potential partners and demonstrates that GRINDR and other types of social media may serve as a feasible platform for prevention education and interventions for HIV-positive YMSM. The unusual finding of an association between HIV-positive serostatus and having met a partner at a bookstore in the previous 3 months may be explained by the local geography particular to Los Angeles; there is a bookstore in the metropolitan West Hollywood area behind which MSM are known to congregate for sexual partnering after the close of bars and dance clubs in the surrounding area; however the confidence intervals around this finding are quite wide, at least raising the possibility of a spurious finding.
PEP for HIV prevention is available at three community-based sites in Los Angeles County; PrEP was not routinely available at the time of study conduct. PEP or PrEP use was reported by a limited number of participants and was interestingly associated with methamphetamine use in the past month—perhaps owing to an ongoing clinical study of PEP among MSM methamphetamine users in Los Angeles at the time of survey administration. PEP or PrEP use was also strongly associated with non-Latino race, suggesting an increased need for education on the availability and use of chemoprophylaxis strategy among LAC Latino populations.
GRINDR does not explicitly market itself as a mechanism for sexual partnering, instead emphasizing an MSM-focused social network that allows MSM to use proximity as a facilitator of socializing; however, in our survey, the three most commonly reported uses for GRINDR were friendship, dating, and one-on-one sex. For individuals who use GRINDR, the GRINDR platform is the most commonly reported mechanism for sexual partnering in the previous 3 months—out ranking the use of Internet sex-focused sites and “through friends,” which were the next two most frequently used modalities for sexual partnering. Consistent with the rapid evolution of technology, there are now also multiple look-a-like applications that similarly take advantage of the GPS functionality of smartphones to facilitate interaction among MSM, some further targeting subcultures within MSM communities (Scruff, Manhunt Mobile, and Jack’d), providing numerous platforms for recruitment/intervention.
GRINDR proved to be a feasible, innovative mechanism for recruiting a sample of 375 YMSM and YMSM/W; however, using GRINDR to recruit YMSM posed a number of challenges for the study team: The overwhelming majority of participants contacted via the application “chat” feature did not respond or demonstrated no interested in study participation making the recruitment process particularly time and effort intensive. The GPS feature of smartphones was frequently imprecise in reporting GRINDR users’ proximity, resulting in contacts to GRINDR users who were at significant distance from the study team making in-person questionnaire administration impossible. Performing venue-based research at locations where alcohol or illicit substances are often consumed further complicates recruitment—not uniquely to the GRINDR mechanism—as study staff were frequently forced to evaluate the ability of chemically altered participants to consent to participation and provide accurate and coherent survey responses. Others have lauded the relative ease and convenience of Internet-based recruitment, but contrasted the increased response rates afforded by face-to-face recruitment for MSM;11 the GRINDR strategy attempted to exploit the optimal aspects of both Internet-based (ease/rapid recruitment) and in-person (increased enrollment rates per contact) strategies.
An important limitation of the sample is that in order to be captured by GRINDR’s GPS functionality, a participant would have to be (or have been) proximate to one of the VDT venues in order to be in the sampling frame. This selects for participants who frequent MSM-associated or focused locations and may exclude an important risk group that would not attend events/locations identified as catering to MSM clientele. Our analysis is also limited by the inability to characterize GRINDR users who chose not to respond to our GRINDR-based recruitment efforts or who declined to participate in the survey nor is the population of GRINDR users necessarily representative of all YMSM populations.
GRINDR and other Internet sites and social networking applications offer advertising space for sale to both commercial interests and academic research; we are aware of groups using GRINDR and other non-GPS-based sex-focused websites successfully for recruitment and survey of MSM.10 Our findings show that such apps/sites are feasible as direct recruitment tools for study participation and facilitation of epidemiologic and behavioral surveillance of this difficult-to-access population. We have found the use of GPS-based social networking applications to be a feasible mechanism for recruiting YMSM and YMSM/W in Los Angeles County. This novel approach for recruiting YMSM should be incorporated into the design of future HIV prevention trials and trials to enhance treatment retention among those who are HIV infected. Additional potential applications of such GPS-based apps include the delivery of HIV testing and prevention messaging aimed at reducing HIV incidence.18
Acknowledgments
This work was funded by the City of Los Angeles AIDS Coordinator’s Office, contract C-118670. R. Landovitz is additionally supported by National Institute of Drug Abuse (K23 DA026308). Additional support was provided by a grant from the National Institute of Mental Health (P30 MH58107). We would like to acknowledge Trista Bingham and Juli-Ann Carlos for assistance with cross-study comparisons using the LA subsets of NHBS and WHSBS, as well as helpful discussions in preparation of this manuscript.
References
- 1.Centers for Disease Control and Prevention. HIV among gay, bisexual and other men who have sex with men (MSM), 2010. http://www.cdc.gov/hiv/topics/msm/index.htm. Accessed 4 Apr 2012.
- 2.Prejean J, Song R, Hernandez A, et al. Estimated HIV Incidence in the United States, 2006–2009. PLoS One. 2011;6(8):e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.HIV Epidemiology Program Los Angeles County Department of Public Health. 2010 Annual HIV Surveillance Report, 2011. http://publichealth.lacounty.gov/phcommon/public/reports/rptspubdisplay.cfm?unit=hiv&ou=ph&prog=hae. Accessed 4 Apr 2012.
- 4.Lenhart A, Purcell K, Smith A, K Z. Social media & mobile internet use among teens and young adults. http://pewinternet.org/Reports/2010/Social-Media-and-Young-Adults.aspx. Accessed 13 Mar 2012.
- 5.Smith A. Mobile Access 2010.http://pewinternet.org/Reports/2010/Mobile-Access-2010.aspx. Accessed 13 March 2012.
- 6.Research F. Forrester research finds that gay consumers are among the earliest technology adopters survey results suggest that marketers target untapped consumer group. Press Release, July 16, 2003.
- 7.Klausner JD, Wolf W, Fischer-Ponce L, Zolt I, Katz MH. Tracing a syphilis outbreak through cyberspace. JAMA. 2000;284(4):447–449. doi: 10.1001/jama.284.4.447. [DOI] [PubMed] [Google Scholar]
- 8.Horvath KJ, Rosser BR, Remafedi G. Sexual risk taking among young internet-using men who have sex with men. Am J Public Health. 2008;98(6):1059–1067. doi: 10.2105/AJPH.2007.111070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosser B, Oakes J, Horvath K, Konstan J, Danilenko G, Peterson J. HIV sexual risk behavior by men who use the Internet to seek sex with men: results of the Men’s INTernet Sex Study-II (MINTS-II) AIDS Behav. 2009;13:488–498. doi: 10.1007/s10461-009-9524-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burrell ER, Pines HA, Robbie E, et al. Use of the location-based social networking application GRINDR as a recruitment tool in rectal microbicide development research. AIDS Behav. 2012. doi:10.1007/s10461-012-0277-z. [DOI] [PMC free article] [PubMed]
- 11.Raymond H, Rebchook G, Curotto A, et al. Comparing Internet-based and venue-based methods to sample MSM in the San Francisco Bay Area. AIDS Behav. 2010;14(1):218–224. doi: 10.1007/s10461-009-9521-6. [DOI] [PubMed] [Google Scholar]
- 12.Elford J, Bolding G, Davis M, Sherr L, Hart G. Webbased behavioral surveillance among men who have sex with men: a comparison of online and offline samples in London, UK. J Acquir Immune Defic Syndr. 2004;35(4):421–6. [DOI] [PubMed]
- 13.Du Bois S, Johnson S, Mustanski B. Examining Racial and Ethnic Minority Differences Among YMSM During Recruitment for an Online HIV Prevention Intervention Study. AIDS Behav. 1–6. [DOI] [PMC free article] [PubMed]
- 14.Centers for Disease Control and Prevention. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings; 2006. [PubMed]
- 15.US Census Bureau. State and county QuickFacts. http://quickfacts.census.gov/qfd/states/06/06037.html. Accessed 4 Mar 2012.
- 16.Campsmith ML, Rhodes PH, Hall HI, Green TA. Undiagnosed HIV prevalence among adults and adolescents in the United States at the end of 2006. J Acquir Immune Defic Syndr. 2010;53(5):619–624. doi: 10.1097/QAI.0b013e3181bf1c45. [DOI] [PubMed] [Google Scholar]
- 17.Smit PJ, Brady M, Carter M, et al. HIV-related stigma within communities of gay men: a literature review. AIDS Care. 2011:1–8. [DOI] [PMC free article] [PubMed]
- 18.Gardner EM, McLees MP, Steiner JF, del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]