Abstract
The rationale for doing full mouth rehabilitation are, when occlusal forces become traumatic hampering the health of periodontal tissues, extensive occlusal diseases, trauma, temporomandibular joint disease and congenital disorders with malformed dentition. Literature exposes that full mouth fixed rehabilitation is one of the taxing procedures in the field of Prosthodontics. A critical aspect for successful occlusal rehabilitation is to determine the aetiology, correct sequence of treatment and most importantly the occlusal vertical dimension and centric relation in which to plan the treatment. A systematic approach in managing these patients can lead to a predictable and favourable prognosis. This article presents the stages of prosthodontic rehabilitation, from diagnosis to final treatment and follow-up, of a bruxer patient with severely worn dentition.
Keywords: Occlusal disease, Bruxism, Extra capsular, Load testing, Adapted centric, Sectional acrylic block
Introduction
Occlusal wear of teeth due to attrition is the result of friction by functional and parafunctional activities [1]. Frictional tooth wear alters the existing occlusal plane introducing deflective occlusal interferences. Literature indicates stress combined with tooth interferences in centric and eccentric occlusion as triggering factors of parafunctional activity. Glossary of Prosthodontic terms (GPT-8) defines Bruxism as “Parafunctional grinding of teeth or an oral habit consisting of involuntary rhythmic or spasmodic non functional gnashing, grinding or clenching of teeth in other than chewing movements of the mandible which may lead to occlusal trauma” [2]. Bruxism can occur during wakefulness (Diurnal Bruxism) or during sleep (Sleep Bruxism). The International Classification of Sleep Disorders (AASM, 2005) categorizes Sleep Bruxism as a sleep-related movement disorder and defines it as “An oral activity characterized by grinding or clenching of the teeth during sleep” [3].
Restitution of mutilated dentitions, as a result of functional and parafunctional occlusal wear is one of the arduous trials in Prosthodontics [1, 4, 5]. Hesitations in attempting to reconstruct debilitated dentitions are heightened by widely divergent views concerning the appropriate procedures for successful treatment. McCollum, D’Amico, Stuart and Stallard, Christensen, Pankey-Mann-Schuyler are the proponents whose concepts were debated, tried and tested over the years by the practicing gnathologists. This led to the evolution of a more organized approach in occlusal rehabilitation [1, 6, 7]. Occlusal rehabilitation is the correlation of all indicated and required dental treatment for a particular patient in order to restore his occlusion to normal function, to improve esthetics, and to preserve tooth and their supporting structures [8]. This case report elucidates the stage by stage full mouth rehabilitation of a patient with bruxism who presented with generalized attrition of his dentition. The importance of diagnosis and treatment planning in this scenario is thoroughly discussed.
Case Report
A 55 year old male patient reported to the department of Prosthodontics, Sri Ramakrishna Dental College & Hospital, Coimbatore, Tamil Nadu, with the complaint of generalized sensitivity of teeth and difficulty in chewing. Patient also reported jaw stiffness and joint pain, which was intense in the morning and reduced thereafter. Patient was an alcoholic and he did not report any compromising medical condition. Personal history revealed that patient was under considerable psychological stress due to financial constraints.
Extra Oral Clinical Examination
Patient exhibited mandibular deviation on normal mouth opening. Temporomandibular joint examination revealed tenderness in the periauricular region on both sides of the face. He also had tenderness in the muscles of mastication. Vertical dimension at rest and in occlusion was measured between two soft tissue landmarks; tip of the nose and prominent portion of chin. A difference of 5–6 mm was evident between VDR and VDO position. The rest position of the mandible is influenced by muscular equilibrium, so the patient was made to sit relaxed with head erect and unsupported. This technique of vertical dimension determination is considered physiologic as it avoids gravitational influence on the mandibular position, allows the muscles to be in minimal tonic contracture with the mandible passively suspended. The vertical dimension was further assessed by phonetic and aesthetic method.
Intra Oral Clinical Examination
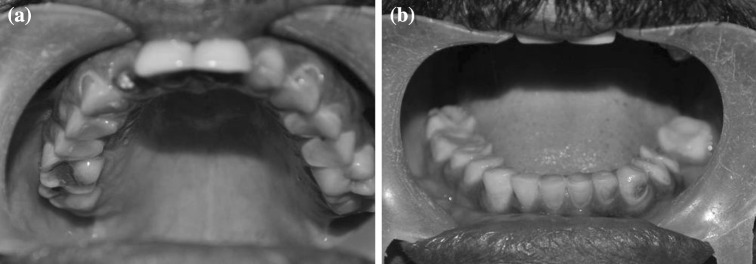
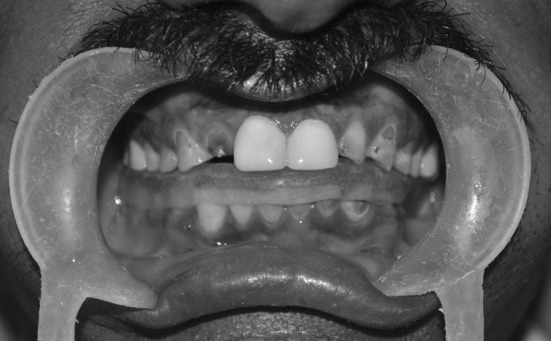
Patient was completely dentate except for 18, 36, 38, and 48. A generalized attrition with occlusal wear facets was evident. Maxillary central incisors were previously restored following endodontic treatment. The endodontically treated maxillary right lateral incisor was fractured (Figs. 1, 2). Occlusal evaluation revealed protrusive and balancing occlusal interferences.
Fig. 1.

Frontal view of the dentition depicting generalized attrition
Fig. 2.
Occlusal view of a maxillary and b mandibular dentition showing extensive attrition
Investigations
Orthopantomograph of the patient revealed generalized loss of enamel and dentin with the attrition very close to pulp in relation to most of the teeth.
Load testing was done to assess centric position.
Diagnosis and Treatment Planning: Stage I
Load testing was done to verify whether the condyles are completely seated when the mandible is gently manipulated to CR position. A comfortably seated condyle in centric position is essential for any dental treatment. Dawson refers a verifiable centric relation which is in harmony with maximum intercuspal position as Type I occlusal condition. In other words, occlusion is in harmony with condyle/disk assembly in the temporomandibular joint [1]. This relation is disturbed in the presence of occlusal interferences. Occlusal interferences initiate negative reflex actions and alter the path of mandibular movement. This creates muscle engram and interferes with complete seating of condyle in CR [1, 4]. Dawson refers such an occlusion as Type II occlusal condition i.e. occlusal contacts are not in harmony with condyle/disk assembly. Muscle deprogramming or occlusal correction erases the muscle engram and allows comfortable centric closure of condyles. Any signs of tension or tenderness on centric loading even after muscle deprogramming is an absolute indication that the condyles on the affected side is not fully seated and there is some form of intra-capsular structural disorder [1]. Since the treatment for a muscular etiology versus an intracapsular disorder varies, proper diagnosis and confirmation of the same is mandatory before commencing the treatment.
In the present case, cotton rolls [8–10] were placed between the anterior teeth and the patient was instructed to “bite” for 5 min ensuring that there was no contact on the posterior teeth. Following this anterior deprogramming procedure, the patient was able to repeatedly reproduce centric position, without any signs of discomfort. This clearly indicated that the source of pain is extra capsular due to muscle engram as a result of occlusal interferences. Therefore, the goal of treatment was elimination of tooth interferences that trigger muscle pain and rehabilitation of dentition in harmony with neuromusculature.
Diagnostic Mounting
Two sets of maxillary and mandibular diagnostic impressions were made with irreversible hydrocolloid (Tulip–Cavex, RW Harlem, The Netherlands). The maxillary cast was mounted on a semi adjustable articulator (Artex-NA, Amann Girrbach, Germany) using transfer bow. As the patient had reduced VDO, a wax interocclusal record of CR position was made at a VDO that will allow a normal freeway space of 3 mm. CR record was made after anterior deprogramming. The mandibular cast (first set) was related to the mounted maxillary cast using this CR record. This was removed and set aside and the second mandibular cast was mounted using this CR record again. The first mandibular cast was used for fabrication of occlusal splint and the second set was used for diagnostic evaluation.
Fabrication of Centric Stabilization Splint
Occlusal splint therapy was planned to free the neuromusculature from occlusal interferences and to assess patient’s response to increased vertical dimension. Wax pattern for occlusal splint was prepared on the mandibular cast in the recorded VDO and was processed with heat polymerizing clear acrylic resin (Veracril, Mangalore dental corporation, Karnataka, India). The fabricated diagnostic occlusal splint was assessed on the articulator mounting and refined to be free from interference in centric and eccentric position. The universal flat plane appliance was adjusted with equal intensity centric stops on all of the teeth. Immediate posterior disclusion, with shallow anterior guidance in lateral and protrusive movements was also perfected. The patient was advised to use the splint as much as possible (Fig. 3).
Fig. 3.
Removable occlusal splint on the mandibular arch
Diagnosis and Treatment Planning: Stage II
Review was done after 24 h and patient reported a mild reduction in symptoms. Further checkups, after a week and a month, revealed that the patient was responding favourably to the splint as the muscle and joint tenderness were satisfactorily controlled. This confirmed the necessity to correct the occlusal contacts to relieve the patient’s symptoms. Still more, the severely attrited teeth needed protection from further damage, so prosthodontic intervention in the form of full mouth occlusal rehabilitation was decided for the patient. After a permissive splint has been used, the challenge is to maintain this harmony in the final rehabilitation. Designing of occlusal scheme in relation to the condyle/disk assembly is the most challenging part in full mouth rehabilitation. Mock preparations and diagnostic wax ups were planned to decide the next phase of treatment.
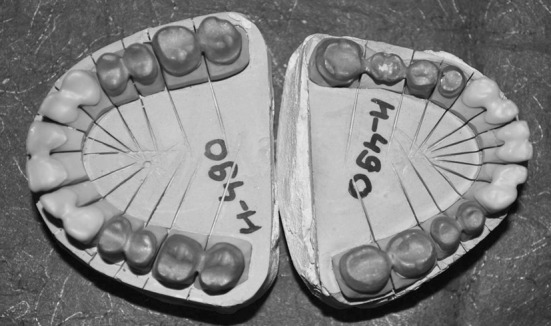
The second set of mandibular cast was secured back on the articulator for evaluation. Customized Broadrick flag assembly was set for the articulator to determine the Curve of Spee. Mock preparations of the anterior teeth were done and diagnostic wax up of these teeth was completed. With distal incisal edge of mandibular canine as the anterior survey point and articulator condylar element as the posterior survey point, long arc and short arc of 4 inch radii were scribed on the flag respectively (Fig. 4). The point of intersection of the arcs was used to draw a sagittal curve of 4 inch radius along the stone cast of mandibular posterior teeth. The procedure helped to differentiate between tooth surfaces requiring considerable tooth reduction from tooth surfaces requiring minimal reduction, to achieve an acceptable curve of Spee. Though Broadrick flag assembly will help to decide the curve of Spee on the diagnostic mounting, executing the required tooth reduction to achieve this clinically is a tricky task. The authors have designed a simple sectional acrylic bite block to solve this issue. Mock tooth preparations of maxillary and mandibular posterior teeth were done except for the second molars. On the articulator, auto polymerizing clear acrylic resin was used to make sectional bite blocks (DPI Cold Cure, The Bombay Burma Trading Corporation, Mumbai, India) in the established VDO between maxillary and mandibular second molars on either side separately. This was used as a vertical stop to guide in tooth preparations and temporization. Following this second molars were also prepared on the model and the diagnostic wax up of posteriors was carried out following the occlusal plane designed with the aid of customized Broadrick flag assembly. Silicone indexes were made to prepare the temporaries (Fig. 5). Thus the blue print of the treatment was designed on the diagnostic cast for each and every step and only then carried out on the patient.
Fig. 4.
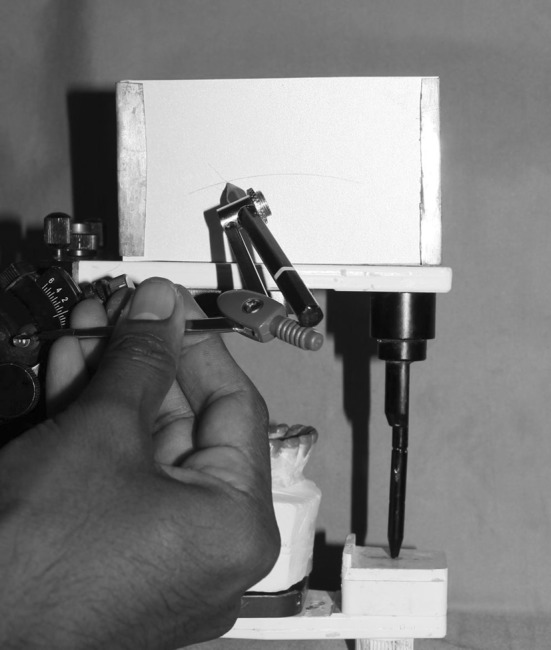
Customized broadrick flag assembly was set to determine the curve of spee
Fig. 5.

Diagnostic wax-up and silicon index for fabrication of temporary Crowns
The unopposed maxillary left third molar was indicated for extraction. Post and core was required in relation to maxillary right lateral and left central incisors which were previously endodontically treated. The tooth preparation was staged as preplanned on the articulator. Endodontic treatment of the attrited teeth was not required as the increase in vertical dimension required only very minimal incisal and occlusal tooth reduction.
Treatment Staging and Execution
Tooth preparations of anterior segment were carried out on the patient. Silicone index of the diagnostic wax up was used to make the provisional restorations (Cool temp, Coltene Whaledent, USA).
The sectional acrylic bite blocks were placed bilaterally between the second molars and the rest of the posterior teeth were prepared. (Fig. 6). Silicone indexes were used to fabricate the temporaries. Once the temporaries were all in place in the planned VDO, the sectional acrylic bite blocks were removed and tooth preparations on the second molars were completed (Fig. 7). Provisional restorations were placed full arch and luted with temporary cement (Fig.8). Patient was monitored periodically for one month. Once the provisional occlusal scheme and VDO proved to be comfortable for the patient, attempts were made to fabricate a duplicate of the same in the final restoration. A custom incisal table of the wax mockup was fabricated to duplicate the same incisal guidance in the final restoration.
Full arch maxillary and mandibular impressions of the tooth preparations were made (3 M ESPE Express, and Express XT Ultra-Light, Seefeld, Germany). Face bow transfer and articulation were completed using centric interocclusal record (Virtual, Ivoclar Vivadent, and Bendererstrasse, Liechtenstein).
All ceramic restorations (Lava 3 M ESPE Dental products, St.Paul, USA.) were planned for the anteriors and PFM restorations (IPS d.SIGN-Ivoclar Vivadent, Germany) for the posteriors. Zirconia and metal copings were fabricated (Fig. 9) and tried into assess the marginal fit.
The contours of the maxillary and mandibular anteriors were established using the silicone index of the diagnostic wax up and further refined with the custom incisal guide table. The anterior provisionals were removed for trial of anterior restorations (before final glazing) and presence of stable centric stops, esthetics and phonetics were evaluated. Labial contours were verified to be in harmony with lip closure path of the patient. The contact relation of maxillary and mandibular anteriors allowed satisfactory disclusion of the posterior provisionals during excursions. After satisfactorily deciding the anterior guidance, the posterior provisionals on either arch were removed retaining the anterior all ceramic restorations in place. Protrusive interocclusal record (Virtual, Ivoclar Vivadent, and Bendererstrasse, Liechtenstein) was made and the articulator was programmed.
In the laboratory, the occlusal plane of mandibular posterior PFM crowns was assessed with the help of the Broadrick flag assembly and then maxillary occlusal plane was designed to follow this. The entire ceramic buildups were refined on the articulator such that there was definite harmonious occlusal contacts in centric and disclusion in the posterior region during protrusion. Group function occlusion was developed for lateral excursions.
The restorations were tried on the patient and the occlusion was further confirmed. After the necessary adjustments, they were polished and glazed. Initial cementations of the final restorations were done with temporary cement (Temp bond-Kerr Corporation, Orange, Canada) and were then replaced with permanent cement (GC Asia Dental Pte Ltd) after a month of review (Fig. 10).
Patient was instructed to wear a soft splint at night as an additional measure to ensure occlusal stability and to protect the restorations from parafunctional wear. Soft splint use was discontinued after two months as there were no signs of evident occlusal wear during review.
Fig. 6.

Sectional acrylic bite blocks are placed on the second molars at the planned VDO
Fig. 7.

Anterior teeth were prepared to receive all ceramic restorations and posterior teeth were prepared for PFM restorations
Fig. 8.

Provisional restorations fabricated with the aid of diagnostic wax up
Fig. 9.
Zirconia copings for anteriors and metal copings for posteriors
Fig. 10.

Final restorations in place
Discussion
Extensive tooth wear is an impending threat for dentition and masticatory function [1, 3, 4]. The management of attritional tooth wear is becoming a subject of increasing interest in the prosthodontic literature, from both preventive and restorative point of view [5, 6]. Attrition is a tooth–tooth friction due to bruxism and empty mouth parafunction [1]. A systematic approach for managing tooth wear can lead to a predictable and favorable prognosis. This article presents the stages of prosthodontic rehabilitation, from diagnosis to final treatment and follow-up, of a bruxer patient with severely worn dentition.
Inspite of the existence of conflicting philosophy, the basis of successful full mouth rehabilitation is programmed treatment planning. All occlusal analysis should start with the examination of temporomandibular joint. In the presence of joint disorder, the choice of treatment is clearly related to the category of the TMD. The second parameter to be considered is a properly aligned condyle-disk assembly in centric relation which directs forces through the avascular, noninnervated central portion of discs that are designed to accept loading. This is only possible in the absence of deflective occlusal interferences to centric relation. Assessment of these essential factors allows creating harmonious posterior determinants in developing functional occlusion. [1, 4, 11].
The third important issue to be addressed in full mouth rehabilitation is deciding the correct occlusal vertical dimension in which full mouth rehabilitation can be planned [6, 11]. This is especially a confounding issue in dentitions showing extensive wear. Methods used to determine vertical dimension are still considered unempirical due to the number of factors influencing the rest position recording. In situations requiring alteration in VDO, to overrule this difficulty, two or more methods are always employed to decide vertical dimension and the changes should be tried with provisional restorations [6, 8]. In this present case, physiologic method, esthetics and phonetics were used to assess the VDO which was later found satisfactory with the short term use of provisionals.
The anterior determinants of mandibular movement are the contacting surfaces of maxillary and mandibular teeth. Of the teeth contact mentioned, the incisal guidance formed by the anterior teeth, has the most profound influence upon the mandibular movement [1, 11–13]. So the fourth step in oral rehabilitation soon after deciding VDO is to check for the presence of favourable incisal guidance and in its absence to develop the contours of anterior teeth in compliance with aesthetic and phonetic demands of the patient. The incisal guidance then controls the necessary steepness of all posterior tooth inclines.
Summarizing all the above, the salient features of optimum occlusion was stated by Peter Dawson [1] as “Dots in the back, lines in the front”, clinically visualized in an ideal occlusion, when occlusal contacts are assessed in centric and eccentric relations, with articulating paper interposed. This formula represents contact in centric relation (Dots in the back) and disclusion of all posterior teeth as the mandible moves from CR. The anterior guidance (lines in the front) assumes the responsibility of separating the posterior teeth during excursions providing mutual protection for each other [8]. This harmony between anterior and posterior teeth can be established by identifying the correct occlusal plane. The curve of Spee, which exists in the ideal natural dentition, allows harmony to exist between the anterior tooth and condylar guidance [14–16].
In the present case, the temporomandibular joints and centric relation assessment revealed the cause of the patient’s symptoms to be due to extracapsular reasons. Parafunctional wear due to psychological stress combined with occlusal interferences has triggered the muscular pain. Psychological Counseling and use of occlusal splint relieved the symptoms of the patient. Decision was made to increase the vertical dimension of occlusion. The contour of anterior teeth and their guidance were refined to be in compliance with the envelope of function. The customized Broadrick flag analyzer assisted in the reproduction of tooth morphology of posterior restorations, commensurate with the curve of Spee [17]. This method prevented protrusive interferences. The use of sectional acrylic bite block fabricated from the diagnostic mounting facilitated controlled conservative tooth reduction. In the clinical report presented, the bite block was a vital tool for transferring the designed VDO from the diagnostic wax-up on the articulator to the mouth. The bite block allowed accurate reduction of the tooth structure to the level of the redesigned occlusal plane. This ensured adequate clearance for prostheses fabrication in the laboratory. Due consideration was given for patient compliance and the entire treatment plan was tried first with provisional restorations and then duplicated in the final restoration. Occlusal protection of the final restorations with soft splint served to protect dental/periodontal structures against adverse effects of hyper-loading and parafunctional wear. [18].
Conclusion
Full mouth rehabilitation entails the performance of all the procedures necessary to produce a healthy, esthetic, well-functioning, self maintaining masticatory mechanism [19]. This clinical report illustrates the value of thorough diagnosis of the condyle/disk assembly in relation to the occlusion in treating a patient with severe parafunctional occlusal wear. Greater care was taken in diagnosing the cause before treating the effect. Without properly comparing and classifying the joint position to the occlusion, the development of neuromuscular harmony and concomitant pain resolution would have been virtually impossible.
The patient’s response to change in vertical dimension of occlusion was assessed first with occlusal stent, followed by provisionals and then implemented in the final restorations. Sectional acrylic bite blocks employed ensured that the required amount of occlusal clearance was attained during tooth preparation procedure. This is simple less time consuming procedure saved clinical chair time.
References
- 1.Dawson PE. Functional occlusion: from TMJ to smile design. Canada: Mosby; 2007. [Google Scholar]
- 2.The Academy of Prosthodontics The glossary of prosthodontic terms. J Prosthet Dent. 2005;94:10–92. doi: 10.1016/j.prosdent.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 3.Ferini-Strambi L, Pozzi P, Manconni M, Zuconni M, Oldani A. Bruxism and nocturnal groaning. Arch Ital Biol. 2011;149:1–11. doi: 10.4449/aib.v149i4.1358. [DOI] [PubMed] [Google Scholar]
- 4.Dylina TJ. Phase II therapy for a chronic pain patient: a clinical report. Cranio. 1999;17:126–131. doi: 10.1080/08869634.1999.11746086. [DOI] [PubMed] [Google Scholar]
- 5.Song M-Y, Park J-M, Park E-J. Full mouth rehabilitation of the patient with severely worn dentition: a case report. J Adv Prosthodont. 2010;2:106–110. doi: 10.4047/jap.2010.2.3.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pokorny PH, Wiens JP, Litvak H. Occlusion for fixed prosthodontics: a historical perspective of the gnathological influence. J Prosthet Dent. 2008;99:299–313. doi: 10.1016/S0022-3913(08)60066-9. [DOI] [PubMed] [Google Scholar]
- 7.Charles Becker S. Clinical procedures in occlusal rehabilitation. 2. Philadelphia: W. B. Saunders/ The University of Michigan; 1966. [Google Scholar]
- 8.Hotta TH, de Jesus L, Nunes AH, Quatrini CB, Nonaka O, Bezzon O. Tooth wear and loss: symptomatological and rehabilitating treatments. Braz Dent J. 2000;11:147–152. [PubMed] [Google Scholar]
- 9.Beohar G, Shrivastava S, Agarwal S, Katare U. A concise overview of various options of TMJ deprogrammers: part II. Arch Dent sci. 2011;2:8–11. [Google Scholar]
- 10.Dawson PE. Evaluation, diagnosis and treatment of occlusal problems. 2. St. Louis: Mosby; 1989. [Google Scholar]
- 11.Mccullock AJ. Making occlusion work: practical considerations. Dent Update. 2003;30:211–219. doi: 10.12968/denu.2003.30.4.211. [DOI] [PubMed] [Google Scholar]
- 12.Schuyler CH. The function and importance of incisal guidance in oral rehabilitation. J Prosthet Dent. 2001;86:219–231. doi: 10.1067/mpr.2001.118493. [DOI] [PubMed] [Google Scholar]
- 13.Steele JG, Nohl FSA, Wassell RW. Crowns and other extra-coronal restorations: occlusal considerations and articulator selection. Br Dent J. 2002;192:377–387. doi: 10.1038/sj.bdj.4801380. [DOI] [PubMed] [Google Scholar]
- 14.Craddock HL, Lynch CD, Franklin P, Youngson CC, Manogue M. A study of the proximity of the Broadrick ideal occlusal curve to the existing occlusal curve in dentate patients. J Oral Rehabil. 2005;32:895–900. doi: 10.1111/j.1365-2842.2005.01520.x. [DOI] [PubMed] [Google Scholar]
- 15.Small BW. Occlusal plane analysis using the Broadrick flag. Gen Dent. 2005;53:250–252. [PubMed] [Google Scholar]
- 16.Lynch CD, McConnell RJ. Prosthodontic management of the curve of Spee: use of the Broadrick flag. J Prosthet Dent. 2002;87:593–597. doi: 10.1067/mpr.2002.125178. [DOI] [PubMed] [Google Scholar]
- 17.Bedia SV, Dange SP, Khalikar AN. Determination of the occlusal plane using a custom-made occlusal plane analyzer: a clinical report. J Prosthet Dent. 2007;98:348–352. doi: 10.1016/S0022-3913(07)60118-8. [DOI] [PubMed] [Google Scholar]
- 18.Dao TTT, Lavingne GJ. Oral splints: the crutches for temporomandibular disorders and bruxism. Crit Rev Oral Biol Med. 1998;9:345–361. doi: 10.1177/10454411980090030701. [DOI] [PubMed] [Google Scholar]
- 19.Lucia VO. Modern gnathological concepts—updated. Ann Arbor: Quintessence Pub Co./ The University of Michigan; 1983. [Google Scholar]


