Abstract
Ceramic restorations have been widely used in dentistry. These restorations often require intraoral adjustment with diamond burs after their cementation causing increasing roughness of the ceramic surface. Consequently some finishing and polishing methods have been used to minimize this occurrence. The aim of this study is to evaluate the roughness of the ceramic surfaces submitted to different finishing and polishing methods. 144 specimens of VITAVM®7, VM®9 and VM®13 (VITA Zahnfabrik) ceramics were fabricated and submitted to grinding using diamond burs. They were then divided into 15 groups (five of each ceramic type). Groups 1, 6 and 11—positive control (Glaze); Groups 2, 7 and 12—negative control (no polishing); Groups 3, 8 and 13—polished with abrasive rubbers (Edenta), felt disc and diamond polishing past; Groups 4, 9 and 14—polished with abrasive rubbers (Shofu), felt disc and diamond polishing past; Groups 5, 10 and 15—polished with aluminum oxide discs (Sof-Lex, 3M-ESPE), felt disc and diamond polishing paste. The roughness of the samples surfaces were measured using the rugosimeter Surfcorder SE 1700 and the data were submitted to statistical analysis using ANOVA and Tukey test at a level of significance of 5 %. There was statistically significance difference between the positive control groups and the other groups in all the ceramic types. Mechanical finishing and polishing methods were not able to provide a surface as smooth as the glazed surface for the tested ceramics. To assist dental practitioners to select the best finishing and polishing methods for the final adjustment of the ceramic restorations.
Keywords: Fixed prosthodontics, Ceramic, Occlusal adjustment, Dental finishing and polishing
Introduction
Dental ceramics are able to mimic natural teeth due to their excellent physical properties such as esthetics, biocompatibility, low thermal conductibility, and wear resistance [1, 2]. Because of these features, dental ceramics have been extensively used in several rehabilitation procedures, including inlays, onlays, crowns, and porcelain veneers [3–5]. Nevertheless, as with any other restorative material, it has some disadvantages, such as fragility under superficial stress, friability before cementation and potential wear of the antagonist tooth or restorative material [6, 7].
The ceramic surface is traditionally subjected to a superficial treatment known as glazing. A surface finishing is performed with abrasive burs followed by a heat treatment that melts the superficial layer [1]. The glazing treatment seals the open pores on its surface after the firing process [8], which provides excellent optical properties and greater surface smoothness [9]. Thus, the ideal is to keep the restoration glazed surface intact in order to maintain its mechanical strength and to reduce the biofilm accumulation [8, 10]. However the restoration adjustment with diamond points after cementation is frequently necessary [9, 11]. This adjustment is usually performed for occlusal adjustments, finishing the margins of cemented restorations, improving esthetic appearance or correcting shape, texture and contour imperfections, thereby altering the ceramic glazed surface [3, 4, 9, 12].
After performing these adjustments with diamond points, the ceramic surface becomes rough and extremely abrasive, possibly causing abrasion on the adjacent teeth and on other restorative materials in the opposing arch, in addition to promoting biofilm retention and mechanical irritation of the adjacent soft tissue [5, 8, 9, 12, 13].
One of the alternatives to compensate for abrasiveness created on the ceramic restorations after their adjustment is to perform new glazing, which involves an additional clinical session, since it is not common practice to have a ceramic firing oven in dental offices. Furthermore, although the glaze is an important factor in esthetics, with respect to light reflection, it can frequently change the color value of the restorations, reflecting more light than the natural teeth, thus creating an artificial effect on these restorations [9, 14].
In order to solve these problems, a direct finishing and polishing procedure on the restoration surface has been widely used intraorally, and it can be performed with abrasive rubbers, aluminum oxide discs, or felt and siliconized rubber discs in conjunction with diamond polishing pastes [9]. This procedure produces more uniform surfaces, it saves working time and it is used after glazing to remove excessive brightness, creating a more natural appearance on the restoration [15].
However, there are controversies regarding the best finishing and polishing method to obtain a smooth ceramic surface [5]. Thus, this study assessed the surface roughness of feldspathic ceramic linings VITAVM®7, VITAVM®9 e VITAVM®13 (VITA Zahnfabrik, Germany) submitted to different finishing and polishing methods.
Materials and Methods
The methodology applied to develop the study covered six distinct and consecutive stages.
Fabrication of Test Specimens
Ceramics discs were fabricated using a rectangular aluminum matrix with seven perforations (5 mm-diameter and 2 mm-thick), which determined the specimen dimensions (Fig. 1). The matrix was made of aluminum to provide a smooth surface without retention to facilitate removal of samples. The measures used for making the holes were set to provide samples that had dimensions that allow the handling and procedures of wear and polishing.
Fig. 1.
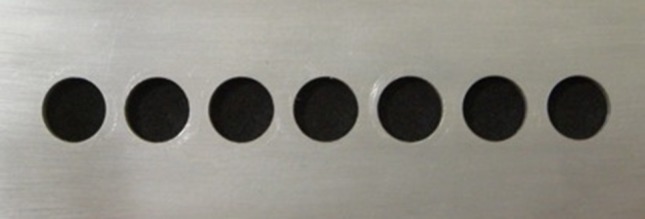
Aluminum matrix with perforations
One hundred and four ceramic test specimens were fabricated by the same dental technician: 48 ceramic lining VITAVM®7, 48 VITAVM®9 and 48 VITAVM®13 (VITA Zahnfabrik, Germany), in the dentin type 3M2 shade. These ceramics were selected because are feldspathic ceramics for crowns coverage. For all the samples, the ceramic powder was incorporated into distilled water and manipulated until it attained dough consistency, according to the manufacturer’s instructions. The mixture was then dried with absorbent paper to remove excessive water and it was taken to matrix perforations until they were completely filled. After 1 min, the test specimens were removed from the perforations with particular caution to avoid fracture, and then it was taken to the VACUMAT 40T (VITA Zahnfabrik, Germany) oven for firing at an initial temperature of 500 °C and final temperature of 910 °C under complete vacuum.
Simulated Occlusal Wear
Afterwards, surface wear was performed with diamond point 2135 F (KG Sorensen, Baureri, SP, Brazil) fitted to a high speed handpiece (Kavo of Brazil Ind. Com. LTDA, Joinville, SC, Brazil) to simulate occlusal wear. The wear was performed by the same operator, using gentle movements for 10 s with air/water cooling. The same diamond point was used for each 06 test specimens and then discarded.
Assessment of Initial Surface Roughness
After performing the occlusal wear, the test specimens were placed in the Ultra-sound appliance (THORNTON, T740, Impec Eletrônica Ltda., SP, Brazil) with distilled water for 10 min to remove residues from their surfaces. Then they were all dried with absorbent paper to have their surface roughness read subsequently.
Each specimen was submitted to reading by a Surfcorder SE 1700 roughness meter (KOSAKA, Japan) to determine initial surface roughness (Fig. 2). The value considered was the arithmetic mean (Ra) between the peaks and depressions traveled by the active tip of the device, in which the measurement run was 1.25 mm with a wavelength of 0.25 mm. The mean obtained for each test specimen corresponded to three readings, one performed in the direction of the test specimen diameter, the others perpendicular and in the oblique direction of the first reading.
Fig. 2.

Initial roughness measurement
Thus, each type of ceramic had 48 test specimens with their initial surface roughness measurements (Ra). A mean of initial surface roughness values obtained for each four test specimens was taken, thus creating a representative negative group control for each ceramic, consisting of 12 measurements, representing the test specimens that received only initial wear with diamond points.
Afterwards, the test specimens of each type of ceramic were randomly distributed into groups (each one containing 12 samples).
Division of Groups
| Group | Ceramic | Polishing method |
|---|---|---|
| G1—positive contol | VITAVM®7 | Glaze |
| G2—negative control | VITAVM®7 | Wear with a fine diamond point |
| G3 | VITAVM®7 | Abrasive rubbers (EDENTA), felt discs and diamond polishing paste |
| G4 | VITAVM®7 | Abrasive rubbers (SHOFU), felt discs and diamond polishing paste |
| G5 | VITAVM®7 | Aluminum oxide discs (Sof-Lex), felt discs and diamond polishing paste |
| G6—positive control | VITAVM®9 | Glaze |
| G7—negative control | VITAVM®9 | Wear with a fine diamond point |
| G8 | VITAVM®9 | Abrasive rubbers (EDENTA), felt discs and diamond polishing paste |
| G9 | VITAVM®9 | Abrasive rubbers (SHOFU), felt discs and diamond polishing paste |
| G10 | VITAVM®9 | Aluminum oxide discs (Sof-Lex), felt discs and diamond polishing paste |
| G11—positive contol | VITAVM®13 | Glaze |
| G12—negative control | VITAVM®13 | Wear with a fine diamond point |
| G13 | VITAVM®13 | Abrasive rubbers (EDENTA), felt discs and diamond polishing paste |
| G14 | VITAVM®13 | Abrasive rubbers (SHOFU), felt discs and diamond polishing paste |
| G15 | VITAVM®13 | Aluminum oxide discs (Sof-Lex), felt discs and diamond polishing paste |
Polishing of Samples
Groups 1 (VITAVM®7), 6 (VITAVM®9) and 11 (VITAVM®13) constituted the positive control groups which were submitted to the application of glaze at the dental laboratory. While Groups 2, 7 and 12 represented the negative control groups for each ceramic, which were worn with a fine diamond point, representing only the mean values of initial roughness, as previously explained.
Groups 3, 8 and 13 were submitted to polishing with Edenta abrasive rubbers (Edenta Ag Dental Products, Haupstrasse, Switzerland). Each specimen was polished with rubbers of three different grains, beginning with the most abrasive one for the pre-polishing (EXA CERAPOL, white-grey color), then an intermediate one for polishing (EXA CERAPOL ROSA, pink color) and the last, a less abrasive one for high brightness polishing (CERAPOL SUPER, grey color). All the rubbers were fitted to a low speed, counter-angle handpiece, (Kavo of Brazil Ind. Com. LTDA, Joinville, SC, Brazil) which was coupled to an LB-100 bench motor (Beltec Ind. e Com. of Dental Equipment, Brazil), calibrated at a speed of 15,000 rpm to control the speed of the handpiece according to the manufacturer’s recommendations. Each rubber was used with light and intermittent movements for 30 s. Afterwards, diamond felt discs (FGM, Joinville, SC, Brazil) were used with a diamond polishing paste (Diamond Excel, FGM, Joinville, SC, Brazil), also at low speed (counter-angle) for 30 s.
Groups 4, 9 and 14 were polished with the Shofu abrasive rubber system sequence (Shofu Porcelain Adjustment Kit—SHOFU, Kyoto, Japan) composed of CERAMISTÉ STANDART rubbers used for pre-polishing, ULTRA for polishing and ULTRA II for high brightness polishing. Afterwards, the diamond felt disc (FGM, Joinville, SC, Brazil) and diamond polishing paste (Diamond Excel, FGM, Joinville, SC, Brazil) were used. The movements performed for the Shofu System and for the felt disc with diamond polishing paste, were the same as those for the previous groups, for 30 s at low speed.
Groups 5, 10 and 15 were polished with aluminum oxide discs (Sof-Lex Discs 3M ESPE, SP, Brazil) of the three different types of grains beginning with the larger grain and going to the smaller grain and polishing with the diamond felt disc (FGM, Joinville, SC, Brazil) and diamond polishing paste (Diamond Excel, FGM, Joinville, SC, Brazil) for the same amount of time and with the same movement used for the previously mentioned groups.
Assessment of Final Roughness
After performing finishing and polishing procedures, the test specimens were placed in the ultra-sound appliance with distilled water for 10 min to remove residues from their surfaces and they were dried with absorbent paper. And then it was followed by the measurement of all test specimens final roughness, including the glazed ones, measured in the same manner as previously described. The means of the values obtained were recorded, tabulated and submitted to statistical analysis.
Results
In this study the different finishing and polishing methods for dental ceramics and the interaction between different factors of variation were compared. In Table 1 the values of mean surface roughness in μm (Ra) and the standard deviations for ceramics VM7, VM9 and VM13 are presented, considering the different finishing and polishing methods. The mean values for each group ranged between 0.3758 and 2.5208.
Table 1.
Means surface roughness (in μm) and standard deviations of the different groups
| Groups | Ra | dp |
|---|---|---|
| G1 | 0.3758 | 0.1434 |
| G2 | 2.5208 | 0.5733 |
| G3 | 1.9187 | 0.4791 |
| G4 | 1.6314 | 0.3255 |
| G5 | 2.4263 | 0.7655 |
| G6 | 1.0318 | 1.0712 |
| G7 | 2.5093 | 0.2386 |
| G8 | 2.1803 | 0.4608 |
| G9 | 1.6718 | 0.3321 |
| G10 | 2.1986 | 0.4568 |
| G11 | 0.7039 | 0.2484 |
| G12 | 2.4878 | 0.3295 |
| G13 | 2.1863 | 0.6492 |
| G14 | 1.8876 | 0.4029 |
| G15 | 2.3765 | 0.8316 |
These values were submitted to the analysis of variance for one criterion (ANOVA), at a level of significance of 5 %, and statistically significant differences (p = 0.00) were found among the groups.
Thus, the Tukey test for multiple comparisons was performed, showing a significant difference between the control groups (1, 6 and 11) which received the application of glaze, and the other groups. However, these control groups presented statistically equivalent results among them with the lowest roughness values (Ra).
When analyzing each type of ceramic, it was observed that the ceramics VM7 and VM9, the groups which were submitted to polishing with the Shofu system, presented lower Ra values in comparison with the other systems, with statistically significant difference (Tables 2, 3). However in the ceramic VM13, there was no statistically significant difference among the systems (Table 4). And the control groups presented the lowest Ra values.
Table 2.
Means surface roughness (in μm) and standard deviations for ceramic VM7
| Group | Ra | dp |
|---|---|---|
| G1 | 0.3758a | 0.1434 |
| G2 | 2.5208b | 0.5733 |
| G3 | 1.9187b | 0.4791 |
| G4 | 1.6314c | 0.3255 |
| G5 | 2.4263b | 0.7655 |
Table 3.
Means surface roughness (in μm) and standard deviations for ceramic VM9
| Group | Ra | dp |
|---|---|---|
| G6 | 1.0318a | 1.0712 |
| G7 | 2.5093b | 0.2386 |
| G8 | 2.1803b | 0.4608 |
| G9 | 1.6718c | 0.3321 |
| G10 | 2.1986b | 0.4568 |
Table 4.
Means surface roughness (in μm) and standard deviations for ceramic VM13
| Group | Ra | dp |
|---|---|---|
| G11 | 0.7039a | 0.2484 |
| G12 | 2.4878b | 0.3295 |
| G13 | 2.1863b | 0.6492 |
| G14 | 1.8876b | 0.4029 |
| G15 | 2.3765b | 0.8316 |
Finally, each type of finishing and polishing method was assessed to verify whether there was statistically significant difference among the different ceramics. The results of the statistical analysis showed that there was no statistical difference among the ceramics for the different finishing and polishing methods, with the values of p = 0.388, 0.180 and 0.709, respectively for the abrasive rubbers (EDENTA), Shofu System (SHOFU) and the aluminum oxide discs (Sof-Lex, 3M).
Discussion
It is usually necessary to adjust the ceramic restorations after cementation to ensure that their surface contour and texture are similar to the natural teeth, and also to maintain proper occlusion [4, 9, 12, 13]. These adjustments usually make the surface of this material incompatible with the oral tissues [5, 8, 9, 12]. Thus, it is imperative for the ceramic to receive some type of finishing and polishing procedures in order to obtain a smooth surface [5, 16].
The use of fine grain diamond points to perform the adjustments of these restorations is indicated [9, 11–13]. Nevertheless, these instruments produce roughness on the surface of the restorative material, which must be minimized by the use of intra-oral polishers [13]. This may be observed in the present study, as shown in Table 1, in which high mean surface roughness values (Ra) were found in the negative control groups that were not polished, but only worn with the fine grain diamond point, presenting mean values of 2.5208, 2.5093 and 2.4878 for the ceramics VM7, VM9 and VM13, respectively.
There are several variations of finishing and polishing methods in the literature, particularly regarding the polishing agents used and their application time. Therefore, this study adopted the use of materials and kits indicated for intra-oral finishing and polishing of dental ceramics, which are easily found in the national market and are easy to operate [5, 9, 11, 17–19]. Furthermore, the choice of material used must be also based on the type of abrasive particle and the application method, because the smaller the size of the particles and the larger number of steps (3 or 4) used the better will be the final polishing result [13]. All the systems used in this study had small abrasive particles and were performed in four different steps.
According to Barghi et al. [10] and Karaksi et al. [4], the ideal is to keep the glazed surface intact because the glaze producing smooth and regular surfaces which provide greater mechanical strength to the material, less wear of antagonist dental enamel and less biofilm accumulation [8]. The data obtained in this study revealed that the glazed specimens presented the lowest surface roughness values (Ra) when compared with the other finishing and polishing systems, for all the types of ceramics. These findings are in agreement with those of Patterson et al. [20] and Al-Wahadni [21] in which the glaze produced lower surface roughness, when compared with different finishing and polishing systems. However, Kelly et al. [22] and Sarac et al. [11] affirmed that there was no statistically significant difference between the surface roughness values found for the glazed ceramics and the ceramics polished with different polishing systems. Moreover, other studies reported lower surface roughness values for the polished ceramics [17, 19, 23].
Manual polishing of ceramic restoration has become a viable option and it can produce smooth and uniform surfaces, presenting the advantage of saving working time because it is not necessary to send the restoration back to the dental laboratory to be glazed. Furthermore if it’s used after glazing, it removes excessive brightness providing a restoration with a more natural appearance [15].
Polishing may be performed with the aid of abrasive rubbers, aluminum oxide discs, felt discs and diamond polishing pastes [9]. Some of the most used systems found in the literature for performing this procedure are the Sof-lex aluminum oxide discs and the abrasive rubber system sequence (Shofu). For Hulterströn and Bergman [17] and Gomis et al. [12] the Sof-lex discs present better results in reducing surface roughness, although Hoelscher et al. [24] have shown that they do not adapt well to convex surfaces, occlusal surface irregularities and the areas of depression caused by wear during adjustments, making it difficult to perform an adequate polishing. Currently, the sequence of abrasive rubbers (Edenta) is also being used for intra-oral polishing of ceramic restorations [19].
There is no consensus in the literature about the efficiency of different finishing and polishing methods to obtain greater surface smoothness on the ceramics [9, 19]. According to Barghi et al. [10] and Karaksi et al. [4] the polishing/finishing systems are considered effective for reducing surface roughness, but they must not substitute the glaze, because they are unable to offer a sufficiently smooth surface after the action of a diamond point. In this study, the mean surface roughness values (Ra) found for the ceramics submitted to different finishing and polishing systems presented no statistically significant differences in comparison with the groups that were not polished, except the groups polished with the abrasive rubber system sequence (Shofu) in VM7 and VM9 ceramics, while the groups that received the glaze presented lower surface roughness values for all the ceramics.
The abrasive rubber system sequence (Shofu) has presented lower surface roughness values when compared with the other materials [17, 25, 26] and therefore, as it is for the case with the majority of the systems used, they must be associated with a diamond polishing paste to produce a smoother surface and a more biocompatible surfaces for the dental and gingival tissues [25–28]. According to the results of this study, the abrasive rubber system sequence (Shofu) presented the lowest mean surface roughness values (Ra) with a statistically significant difference in comparison with the groups polished with abrasive rubbers (Edenta) and aluminum oxide discs (Sof-Lex) for the VM7 and VM9 ceramics.
In this experiment, the dental ceramic factor was not shown to be responsible for variations in surface roughness values (Ra) when submitted to the same finishing and polishing methods. This indicates that the compositional alterations in the three ceramics were not responsible for creating differences in their clinical behavior.
The differences in results found in several of the mentioned studies are probably due to the different commercial brands of the products, methodologies used and variables within the studies, in addition to the way in which the handling and firing process of the ceramic body was performed interfering with the quality and the presence of porosity within each specimen [19, 21]. Thus, further studies are required, with similar and standardized methodologies to verify the efficiency of these materials.
Conclusions
Within the limitations of this in vitro study, it may be concluded that mechanical finishing and polishing methods were not able to provide a surface as smooth as the glazed surface for the tested ceramics. The ceramics behaved in a similar manner in regards to the finishing and polishing methods.
References
- 1.Yilmaz C, Korkmaz T, Demirköprulu H, Ergün G, Özkan Y. Color stability of glazed and polished dental porcelains. J Prosthodont. 2008;17:20–24. doi: 10.1111/j.1532-849X.2007.00237.x. [DOI] [PubMed] [Google Scholar]
- 2.Metzer KT, Woody RD, Miller AW. In vitro investigation of the wear of human enamel by dental porcelain. J Prosthet Dent. 1999;81:356–364. doi: 10.1016/S0022-3913(99)70280-5. [DOI] [PubMed] [Google Scholar]
- 3.Klausner LH, Cartwright CB, Charbeneau GT. Polished versus autoglazed porcelain surfaces. J Prosthet Dent. 1982;47:157–162. doi: 10.1016/0022-3913(82)90180-9. [DOI] [PubMed] [Google Scholar]
- 4.Karaksi AOE, Shehab GI, Eskander ME. Effect of reglazing and of polishing on the surface roughness of new ceramic restoration (Hi Ceran) Egypt Dent J. 1993;39:485–490. [PubMed] [Google Scholar]
- 5.Camacho GB, Vinha D, Panzeri H, Nonaka T, Gonçalves M. Surface roughness of a dental ceramic after polishing with different vehicles and diamond pastes. Braz Dent J. 2006;17:191–194. doi: 10.1590/S0103-64402006000300003. [DOI] [PubMed] [Google Scholar]
- 6.Bessing C, Wiktorsson A. Comparison of two different methods of polishing porcelain. Scand J Dent Res. 1983;91:482–487. doi: 10.1111/j.1600-0722.1983.tb00849.x. [DOI] [PubMed] [Google Scholar]
- 7.Oliveira MCS, Santos GAG, Siqueira DVS, Vieira AC, Oliveira VMB. Qualitative evaluation of the surface roughness of a dental porcelain after three different polishing systems. Odontol Clin-Cient. 2010;9:151–154. [Google Scholar]
- 8.Al-Wahadni A, Martin M. Glazing and finishing dental porcelain: a literature review. J Can Dent Assoc. 1998;64:580–583. [PubMed] [Google Scholar]
- 9.Benetti AR, Miranda CB, Ramos L., Jr Avaliação da porosidade superficial da porcelana submetida a diferentes métodos de acabamento e polimento. PCL. 2002;4:489–493. [Google Scholar]
- 10.Barghi N, King CJ, Draughn RA. A study of porcelain surfaces as utilized in fixed prosthodontics. J Prosthet Dent. 1975;34:314–319. doi: 10.1016/0022-3913(75)90109-2. [DOI] [PubMed] [Google Scholar]
- 11.Sarac D, Sarac YS, Yuzbasiogl E, Bal S. The effects of porcelain polishing systems on the color and surface texture of feldspathic porcelain. J Prosthet Dent. 2006;96:122–128. doi: 10.1016/j.prosdent.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 12.Gomis JM, Bizar J, Anglada JM, Samsó J, Peraire M. Comparative evaluation of four finishing systems on one ceramic surface. Int J Prosthodont. 2003;16:74–77. [PubMed] [Google Scholar]
- 13.Patterson CJW, McLundie AC, Stirrups DR, Taylor WG. Efficacy of a porcelain refinishing system in restoring surface finish after grinding with fine and extra-fine diamond burs. J Prosthet Dent. 1992;68:402–406. doi: 10.1016/0022-3913(92)90400-5. [DOI] [PubMed] [Google Scholar]
- 14.McPhee ER. Extrinsic coloration of ceramometal restorations. Dent Clin North Am. 1985;29:645–666. [PubMed] [Google Scholar]
- 15.Ward MT, Tate WH, Powers JM. Surface roughness of opalescent porcelains after polishing. Oper Dent. 1990;20:106–110. [PubMed] [Google Scholar]
- 16.Nakazato T, Takahashi H, Yamamoto M, Nishimura F, Kurosaki N. Effect of polishing on cyclic fatigue strength of CAD/CAM ceramics. Dent Mater J. 1999;18:395–402. doi: 10.4012/dmj.18.395. [DOI] [PubMed] [Google Scholar]
- 17.Hulterström AK, Bergman M. Polishing systems for dental ceramics. Acta Odontol Scand. 1993;51:229–234. doi: 10.3109/00016359309040571. [DOI] [PubMed] [Google Scholar]
- 18.Chu FCS, Frankel N, Smales RJ. Surface roughness and flexural strength of self-glazed, polished, and reglazed in-ceram/vitadur Alpha porcelain laminates. Int J Prosthodont. 2000;13:66–71. [PubMed] [Google Scholar]
- 19.Netto Júnior BA, Inoue RT, Ribeiro FC, Feltrin PP. Estudo da rugosidade das superfícies metálica e porcelana mediante acabamento e polimento com sistemas de borrachas para polimento. Revista de Odontologia da UFES. 2006;8:6–18. [Google Scholar]
- 20.Patterson CJW, McLundie AC, Stirrups DR, Taylor WG. Refinishing of porcelain by using a refinishig kit. J Prosthet Dent. 1991;65:383–388. doi: 10.1016/0022-3913(91)90229-P. [DOI] [PubMed] [Google Scholar]
- 21.Al-Wahadni A. An in vitro investigation into the surface roughness of 2 glazed, unglazed, and refinished ceramic materials. Quintessence Int. 2006;37:311–317. [PubMed] [Google Scholar]
- 22.Kelly JA, Nishimura I, Campbell SD. Ceramics in dentistry: historical roots and current perspectives. J Prosthet Dent. 1996;75:18–38. doi: 10.1016/S0022-3913(96)90413-8. [DOI] [PubMed] [Google Scholar]
- 23.Wright MD, Masri R, Driscoll CF, Romberg E, Thompson CGA, Runyan CD. Comparison of three systems for the polishing of an ultra-low fusing dental porcelain. J Prosthet Dent. 2004;92:486–490. doi: 10.1016/j.prosdent.2004.07.021. [DOI] [PubMed] [Google Scholar]
- 24.Hoelscher DC, Neme AML, Pink FE, Hughes PJ. The effect of three finishing systems on four esthetic restorative materials. Oper Dent. 1998;23:36–42. [PubMed] [Google Scholar]
- 25.Raimondo RL, Jr, Richardson JT, Wiedner B. Polished versus autoglazed dental porcelain. J Prosthet Dent. 1990;64:553–557. doi: 10.1016/0022-3913(90)90126-W. [DOI] [PubMed] [Google Scholar]
- 26.Oliveira AB, Matson E, Marques MM. The effect of glazed and polished ceramics on human enamel wear. Quintessence Int. 2006;19:547–548. [PubMed] [Google Scholar]
- 27.Ancowitz IS, Torres T, Rostami H. Texturing and polishing. Dent Clin North Am. 1998;2:607–612. [PubMed] [Google Scholar]
- 28.Jung M. Finishing and polishing of a hybrid composite and a heat-pressed glass ceramic. Oper Dentist. 2002;27:175–183. [PubMed] [Google Scholar]


