Abstract
Several dental materials have been used for core build-up procedures. Most of these materials were not specifically developed for this purpose, but as a consequence of their properties, have found application in core build-up procedures. Improvements in composites and the development of nanocomposites have led to their use as a core build up material due to their superior mechanical properties, optical properties and ease of handling. However it is not clear if they have better mechanical properties than the conventional core build up materials like amalgam, GIC and dual cure composite core build up material. The strength of the core material is very important and this study was undertaken to compare the mechanical properties of materials used for direct core foundations. The differences between the compressive strength and flexural strength of Filtek Z350 nanocomposite with conventional core build up materials like Amalgam, Vitremer GIC and Fluorocore were tested. Cylindrical plexi glass split molds of dimension 6 ± 1 mm [height] x4 ± 1 mm [diameter] were used to fabricate 15 samples of each core material for testing the compressive strength and rectangular plexi glass split molds of dimension 25 ± 1 mm [length] x 2 ± 1 mm[height] x2 ± 1 mm [width] used for fabricating samples for flexural strength. The samples were stored a water bath at 250 °C for 24 h before testing. The samples were tested using a Universal Instron testing machine. The results of the study showed that Fluorocore had the highest compressive strength and flexural strength followed by Filtek Z350 [nanocomposite] Amalgam had the least flexural strength and Vitremer GIC had the least compressive strength. Thus flurocore and nanocomposite are stronger than other core build up materials and hence should be preferred over other conventional core build up materials in extensively damaged teeth.
Keywords: Nanocomposite, Core build up, Compressive strength, Flexural strength, Filtek Z350, Vitremer
Introduction
A core build- up is a restoration placed in a badly broken down tooth to restore the bulk of the coronal portion so as to facilitate the subsequent restoration by means of an indirect extra coronal restoration. A core restoration should provide satisfactory strength and resistance during crown preparation and impression procedures and therefore contribute to the retention and support of the temporary crown and in long term the definitive restoration. The core material should have compressive strength to resist intraoral forces and flexural strength to prevent core dislodgement during function. Materials used for core restoration after endodontic treatment include amalgam, glass ionomer, hybrid glass ionomer, and resin composites [1–7]. Each of these core materials have their own advantages and disadvantages, a thorough knowledge of which helps in selection of the appropriate material for a particular clinical situation. With the advent of composite resin many of the desirable properties were combined into one material. They have adequate strength, ease of handling and they can be bonded to the tooth structure. Hence, they are one of the commonly used materials for core build up. Their compressive strength is comparable to amalgam cores. Fluoride releasing composites are also available. Also, improvement in composites and enamel and dentin bonding systems has stimulated trends toward more conservative techniques. Apart from esthetics, resin composite cores have a number of advantages over amalgam. Due to the immediate polymerization, teeth can be prepared for a crown restoration at the same appointment. Resin composites can also be bonded to dowels and crowns whenever appropriate bonding techniques are used. However, their disadvantages include their higher coefficient of thermal expansion relative to that of enamel and the possible contamination by eugenol containing provisional cements [1, 3, 4, 7, 8, 9, 10, 12]. The comparison of the physical properties like compressive strength and flexural strength of nanohybrid composite resin core materials with conventional core restorative materials would help the clinician to choose the appropriate and best core material available for the restoration of weakened tooth structure.
Materials and Methods
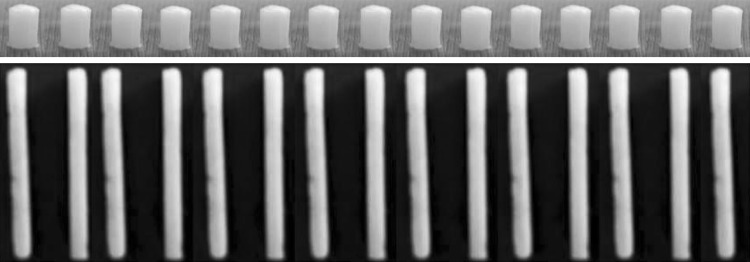
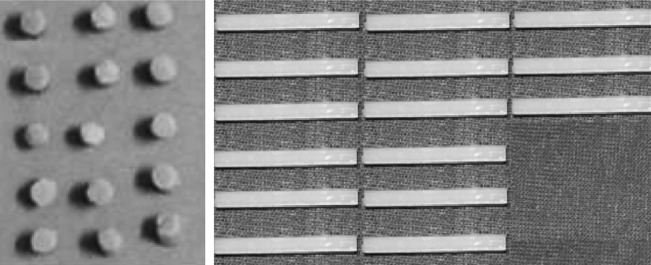
Four commercially available brands of core materials were used [Table 1]. Cylindrical plexi glass split molds of dimension 6 ± 1 mm [height] x4 ± 1 mm [diameter] (Fig. 1) were used to fabricate 15 samples of each core material for testing the compressive strength and rectangular plexi glass split molds of dimension 25 ± 1 mm{length}x 2 ± 1 mm{height}x2 ± 1 mm{width}(Fig. 2) [14–17]were used for fabricating samples for flexural strength. A total of 60 samples were fabricated with 15 samples of each type of core material namely amalgam [DPI Alloy] (Fig. 3), Vitremer [3M] (Fig. 4), Fluorocore [DENTSPLY, Caulk] (Fig. 5), Nanocomposite, Filtek Z350 [3M] (Fig 4) were fabricated to test the compressive strength and flexural strength respectively. The samples were stored a water bath at 37 ± 10 C for 24 h before testing. The samples were tested using a Universal Instron testing machine (Fig 6). This was connected to a load measuring cell, which continuously recorded the load applied to the samples at a crosshead speed of 0.75 ± 0.25 mm min-1 till the samples fracture.
Table 1.
Four commercially available brands of core materials
| Group | Test done | Material used | Brand name | Number of samples |
|---|---|---|---|---|
| AC | Compressive strength | High copper amalgam | DPI Alloy | 15 |
| AF | Flexural strength | High copper amalgam | 15 | |
| IC | Compressive strength | Resin modified glass ionomer | Vitremer [3 M] | 15 |
| IF | Flexural strength | Resin modified glass ionomer | 15 | |
| FC | Compressive strength | Fluoride releasing composite | Fluorocore [DENTSPLY] | 15 |
| FF | Flexural strength | Fluoride releasing composite | 15 | |
| NC | Compressive strength | Nanohybrid composite resin | Filtek Z350 [3 M] | 15 |
| NF | Flexural strength | Nanohybrid composite resin | 15 |
Fig. 1.
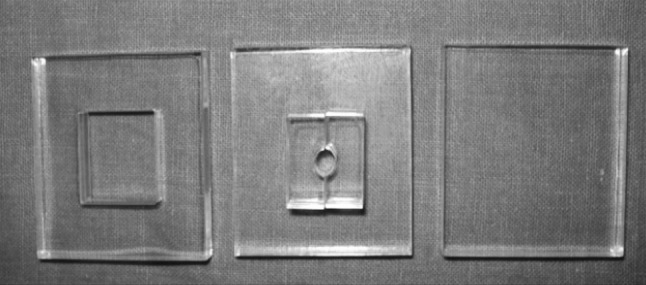
Plexi Glass Molds for fabrication of cylindrical compressive strength samples
Fig. 2.
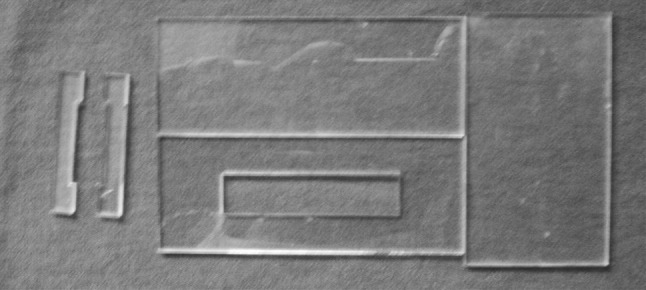
Plexi Glass Molds for fabrication of rectangular flexural strength samples
Fig. 3.
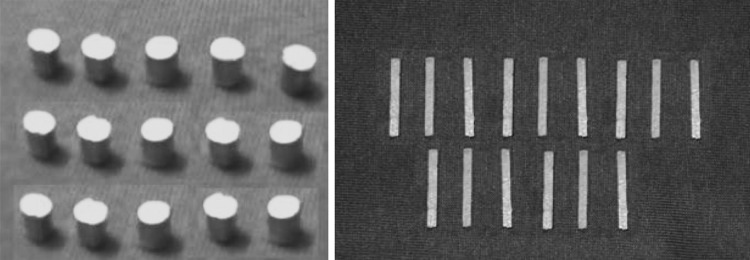
15 Samples of amalgam [dpi alloy]
Fig. 4.
15 Samples of vitremer [3 M]
Fig. 5.
15 Samples of flouorocore [DENTSPLY]
Fig. 6.
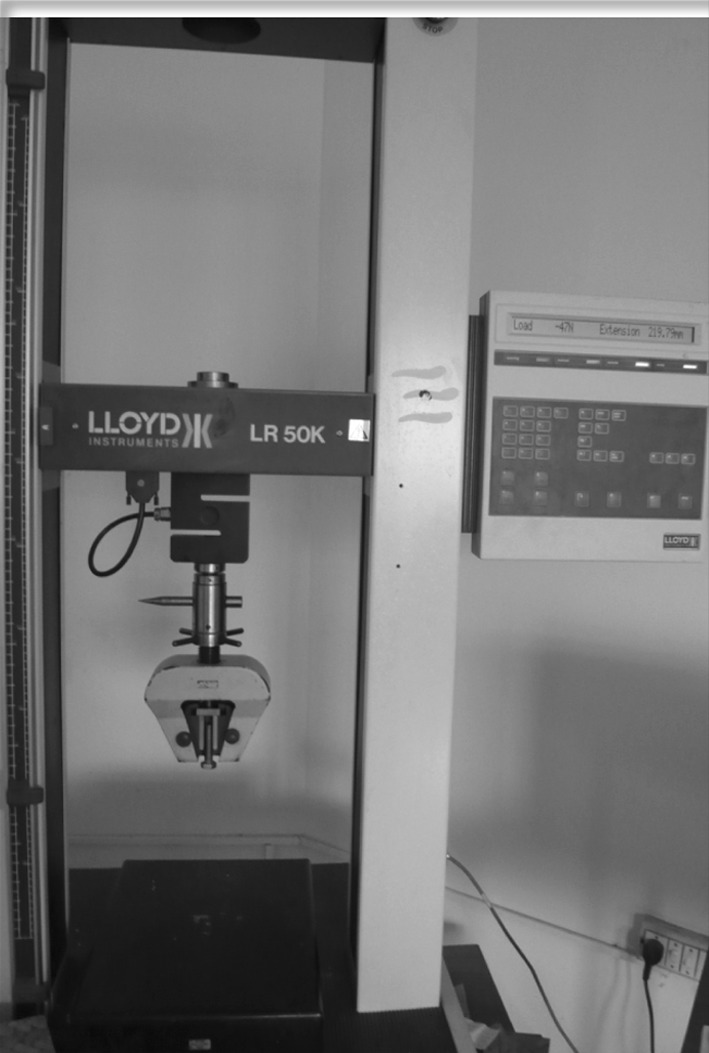
Universal instron testing machine
Results
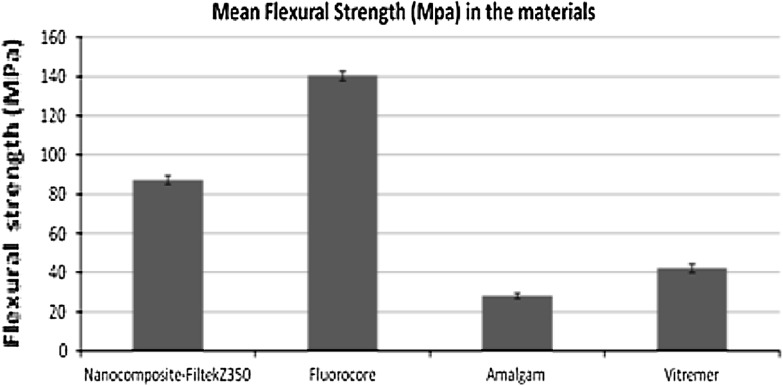
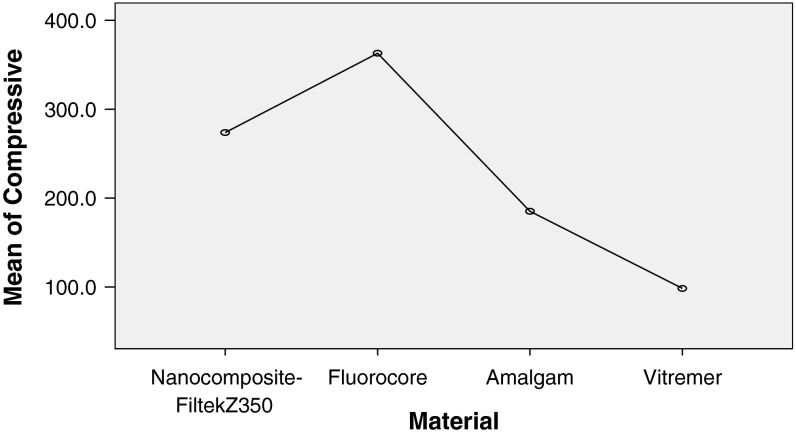
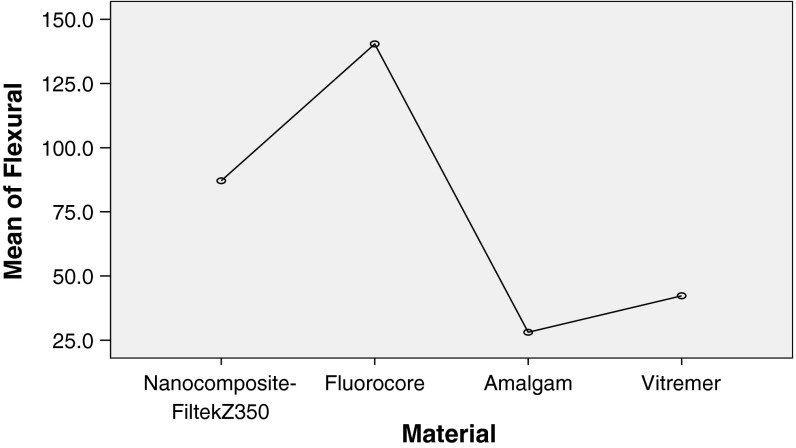
The values were recorded for compressive strength and flexural strength [MPa] in the four groups AC, IC, FC and NC which are Amalgam [DPI], Vitremer [3 M], Fluorocore[DENTSPLY, Caulk] and Nanocomposite Filtek [3 M] respectively. The observations were then subjected to statistical analysis.[Tables 2, 3, 4, 5, 6 and 7]. Comparison of Compressive Strength and Flexural Strength (MPa) between the four materials (Nanocomposite-FiltekZ350, Fluorocore, Amalgam and Vitremer) was done. The Null Hypothesis 1 was that there is no significant difference in the mean compressive strength and flexural strength (in MPa) of the 4 materials i.e. μ1 = μ2 = μ3 = μ4.The Alternate Hypothesis was that there is a significant difference in the mean compressive strength and flexural strength (in MPa) of the 4 materials i.e. μ1 ≠ μ2 ≠ μ3 ≠ μ4.. The Level of Significance considered for values to be significant was α = 0.05 In order to compare the means of the 4 materials ANOVA analysis was used. The P value was compared with the level of significance. If P < 0.05, the alternate hypothesis was accepted and concluded that there is a significant difference in the mean compressive strength and flexural strength of the materials. Otherwise the null hypothesis is accepted. If there is a significant difference between the materials then multiple comparisons (Post—Hoc tests) using Bonferroni test is carried out. Higher mean compressive strength was recorded for Fluorocore [FC group] followed by Nanocomposite-FiltekZ350 [NC] and Amalgam [AC] respectively. Lowest compressive strength was recorded for Vitremer [IC group]. The difference in mean compressive strength between the four materials was found to be statistically significant (P < 0.001). In order to find out among which pair of materials there exists a significant difference with respect to the compressive strength, multiple comparisons was done using Bonferroni test. The results are as given in Table 5. The difference in mean compressive strength between Nanocomposite-Filtek Z350 and the other materials was found to be statistically significant (P < 0.001). Similarly the difference in mean compressive strength between Fluorocore, Amalgam, Vitremer with the other materials was also found to be statistically significant (P < 0.001) [Figs. 7,8]. Higher mean flexural strength was recorded for Fluorocore[FF] followed by Nanocomposite-FiltekZ350 [NF] and Vitremer [IF] respectively as seen in Table 6. Lowest flexural strength was recorded for Amalgam [AF]. The difference in mean flexural strength between the different materials was found to be statistically significant (P < 0.001). In order to find out among which pair of materials there exists a significant difference, Bonferroni test was done [Table 7]. The difference in mean flexural strength between Nanocomposite-FiltekZ350 and the other materials was found to be statistically significant (P < 0.001). The difference in mean flexural strength between Fluorocore, Amalgam, Vitremer and the other materials was also found to be statistically significant (P < 0.001) [Figs. 9,10].
Table 2.
Compressive strength [MPa]
| Group | Material | Mean | Std dev |
|---|---|---|---|
| NC | Nanocomposite-FiltekZ350 | 273.71 | 8.27 |
| FC | Fluorocore | 363.01 | 5.40 |
| AC | Amalgam | 185.14 | 3.91 |
| IC | Vitremer | 98.35 | 1.13 |
Table 3.
Compressive strength [MPa]
| Group | Material | Mean | Std dev |
|---|---|---|---|
| NF | Nanocomposite-FiltekZ350 | 87.12 | 2.11 |
| FF | Fluorocore | 140.42 | 2.32 |
| AF | Amalgam | 28.09 | 1.15 |
| IF | Vitremer | 42.30 | 2.12 |
Table 4.
ANOVA - Compressive strength [MPa]
| Material Group | n | Mean | Std dev | Min | Max | F | P value |
|---|---|---|---|---|---|---|---|
| Nanocomposite-FiltekZ350 NC | 15 | 273.71 | 8.27 | 260.30 | 289.30 | 7040.214 | <0.001 |
| Fluorocore FC | 15 | 363.01 | 5.40 | 352.20 | 371.70 | ||
| Amalgam AC | 15 | 185.14 | 3.91 | 177.70 | 190.30 | ||
| Vitremer IC | 15 | 98.35 | 1.13 | 95.90 | 100.20 |
Table 5.
Bonferroni test multiple comparisons: compressive strength [MPa]
| Group | Material[I] | Material [J] | Mean difference [I-J] | Std. error | Sig | 95 %confidence interval | |
|---|---|---|---|---|---|---|---|
| Lower bond | Upper bond | ||||||
| NC | Nanocomposite-Filtek Z350 | Fluorocore | −89.3000 | 1.8965 | 0.000 | −94.475 | −84.125 |
| Amalgam | 88.5710 | 1.8684 | 0.000 | 83.473 | 93.669 | ||
| Vitremer | 175.3596 | 1.9278 | 0.000 | 170.099 | 180.620 | ||
| FC | Fluorocore | Nanocomposite-Filtek Z350 | 89.3000 | 1.8684 | 0.000 | −93.669 | −83.473 |
| Amalgam | 177.8710 | 1.8684 | 0.000 | −182.969 | −172.773 | ||
| Vitremer | 86.7886 | 1.9278 | 0.000 | 81.604 | 91.973 | ||
| AC | Amalgam | Nanocomposite-Filtek Z350 | −88.5710 | 1.8684 | 0.000 | −93.669 | −83.473 |
| Fluorocore | −177.8710 | 1.8684 | 0.000 | −182.969 | −172.773 | ||
| Vitremer | 86.7886 | 1.9002 | 0.000 | 81.604 | 91.973 | ||
| IC | Vitremer | Nanocomposite-Filtek Z350 | −175.3596 | 1.9278 | 0.000 | −180.260 | −170.099 |
| Fluorocore | −264.659 | 1.9278 | 0.000 | −269.920 | −259.399 | ||
| Vitremer | −86.7886 | 1.9002 | 0.000 | −91973 | −81.604 | ||
Table 6.
ANOVA—flexural strength [MPa]
| Material Group | N | Mean | Std dev | Min | Max | F | P value |
|---|---|---|---|---|---|---|---|
| Nanocomposite-FiltekZ350 NF | 15 | 87.12 | 2.11 | 84.10 | 92.03 | 10463.013 | <0.001 |
| Fluorocore FF | 15 | 140.42 | 2.32 | 135.50 | 144.20 | ||
| Amalgam AF | 15 | 28.09 | 1.15 | 26.00 | 29.80 | ||
| Vitremer IF | 15 | 42.30 | 2.12 | 37.69 | 45.80 |
Table 7.
Bonferroni test multiple comparisons: flexural strength [MPa]
| Group | Material[I] | Material [J] | Mean difference [I-J] | Std. error | Sig | 95 % Confidence interval | |
|---|---|---|---|---|---|---|---|
| Lower bond | Upper bond | ||||||
| NF | Nanocomposite-Filtek Z350 | Fluorocore | −53.052 | 0.6759 | 0.000 | −55.147 | −51.463 |
| Amalgam | 59.0317 | −6987 | 0.000 | 57.127 | 60.936 | ||
| Vitremer | 44.8233 | −6867 | 0.000 | 42.952 | 46.695 | ||
| FF | Fluorocore | Nanocomposite-Filtek Z350 | 53.052 | 0.6759 | 0.000 | 51.463 | 55.147 |
| Amalgam | 112.2369 | 0.7080 | 0.000 | 110.407 | 114.266 | ||
| Vitremer | 98.1285 | 0.6961 | 0.000 | 96.231 | 100.026 | ||
| AF | Amalgam | Nanocomposite-Filtek Z350 | −59.0317 | 0.6987 | 0.000 | −60.936 | −57.127 |
| Fluorocore | −112.3369 | 0.7080 | 0.000 | −114.266 | −110.407 | ||
| Vitremer | −14.2083 | 0.7183 | 0.000 | −16.166 | −12.251 | ||
| IF | Vitremer | Nanocomposite-Filtek Z350 | −44.8233 | 0.6867 | 0.000 | −46.695 | −42.952 |
| Fluorocore | −98.1285 | 0.6961 | 0.000 | −100.026 | −96.231 | ||
| Vitremer | 14.2083 | 0.7183 | 0.000 | 12.251 | 16.166 | ||
Fig. 7.
Mean compressive strength [MPa]
Fig. 8.
Mean flexural strength [MPa]
Fig. 9.
Mean compressive strength [MPa]
Fig. 10.
Mean flexural strength [MPa]
Discussion
A core build-up is a restoration placed to provide the foundation for a restoration that will endure the masticatory stress that occurs in the oral cavity for prolonged periods and to provide satisfactory strength and resistance to fracture before and after crown preparation [1]. The selection of materials is based primarily on ease of handling with due consideration being given for mechanical properties and manipulative variables. Among mechanical properties compressive strength of core materials is important because cores usually replace a large bulk of tooth structure and they should provide sufficient strength to resist intraoral compressive and tensile forces that are produced in function and parafunction. Flexural strength is used to evaluate the strength of the material and the amount of the distortion expected under bending stress [43]. Core build up materials are used to reconstruct endodontically treated teeth with cast post and cores, pin retained core build ups, dowel and core and prefabricated post which retain a core that can be used to support the definitive prosthesis. Amalgam, glass-ionomer cements (GICs) and resin composites have found application in core build-up procedures; even if most of them were not specifically developed for this purpose [27]. Among the three direct core buildup materials which are amalgam, GIC and composite, amalgam had the greatest compressive strength according to earlier studies. It also has a safe, successful clinical history. A study by Kovarik et al. compared amalgam, GIC and composite direct build up materials and they found that amalgam cores had the lowest failure rate, and that more than one million cycles were required to produce the median fatigue life of the amalgam cores. Composite resin cores experienced 83.3 % failure and required only 385,212 cycles to achieve their median fatigue life. All the glass-ionomer cores failed during the cycling period. Hence due to its superior mechanical properties and longer function, amalgam is used for direct core build up procedures [8]. The advantages of Glass-ionomer cement are that they do not require extra procedures for consistent retention or adhesion, as they adhere directly to the dental hard tissues [23, 38]. However various studies have shown that conventional GIC’s do not have the physical properties suitable for a core build up material as they are susceptible to moisture contamination and they have low early strength [6, 8, 11]. Simmons is known to have developed miracle mix which was a modified form of GIC with amalgam alloy powders incorporated into it. However esthetics was poor and the strength was not comparable to that of amalgam [38]. Cermet ionomer cements, introduced by McLean by sintering metal and glass powders together to be used as core build up material had lower strength which confines its usage to low stress bearing areas[47]. The search for a material that has the fluoride releasing capability of GIC and durability of composites led to the introduction of polyacid modified composite or compomer [43]. They are indicated when more than half the tooth is missing, and a buildup of the tooth is needed. Resin modified GIC’s are conventional glass ionomer cements with the addition of HEMA. They are also known as hybrid ionomers and they overcame the drawbacks of conventional GIC. They are considered dual cure cements if only one polymersiation mechanism is used like light cure or chemical cure [11, 18, 41]. A recent modification in Resin Modified GIC is the Tricure GIC where there are three reactions, which are Acid–base glass ionomer reaction (initiated when powder and liquid are mixed and can proceed in the dark) photo initiated free radical methacrylate cure and dark cure free radical methacrylate cure (initiated when powder and liquid are mixed and can proceed in the dark). In recent years composites due to their rapid rate of polymerization and better strength properties have become the popular choice for core build up of teeth. The advantages are, the tooth maybe built up, prepared and impressioned all in the same appointment. However there have been reported undesirable properties of composites like dimensional changes when exposed to moisture, which are found to be substantial as they affect the seating of cast restorations [1–8, 10–13, 18–22, 24–26, 30–39]. There are many composite build-up materials available; most of them are either self cured or light cured or dual- cured. As the core build up restorations are thicker restorations, the chemical curing capability is considered as an added advantage. On light curing, however, the intensity of the light is greatest at the surface and generally decreases as it penetrates deeper within the material. For each product, the manufacturer usually recommends the thickness or depth to which the material will completely cure. ADA Specification no. 27, however, requires that this depth is not more than 1.5–2 mm when the composite is light cured [44, 45, 49]. Fluorocore is a dual cure composite which core build up material and has the desirable property of fluoride release. It is available in two shades blue and white. The tooth colored shade can be used where esthetics and show-through of the core are of primary concern [50].Dental composites are polymeric materials and developments in filler technology have led to significant reductions in filler size and improvements in filler packing, reducing the wear and degradation associated with the polymer matrix, and enhancing the clinical usefulness of these materials. The advent of nano fillers with their broad particle distribution in nanocomposites helps to obtain high filler loading, desirable handling characteristics and physical properties [14]. The composition of Filtek Z350 is BIS-GMA, BIS-EMA and UDMA with small amounts of TEGDMA as the resin matrix and the filler contains a combination of a non-agglomerated/non-aggregated, 20 nm nanosilica filler, and loosely bound agglomerated zirconia/silica nanocluster, consisting of agglomerates of primary zirconia/silica particles with size of 5–20 nm fillers. The cluster particle size range is 0.6–1.4 microns. The filler loading is 78.5 % by weight. The compressive strength and flexural strength of the nanocomposite has been shown to be equivalent to or higher than those of the hybrid or microhybrid composites [14, 17, 42, 46]. In the present study the compressive strength and flexural strength of the nanocomposites was compared with other conventional core build up materials. Considerable difference was found in the compressive and flexural strength among the various core materials. Fluorocore which is formulated to be used as a core material was significantly stronger than the other core materials in terms of both compressive and flexural strength followed by Filtek Z350 a nanocomposite. However this was not in accordance with the study done by Mitra et al. According to the study done by Mitra et al. the FS and CS test values of nanocomposites were found to be superior than hybrid, microhybrid or microfill materials.The high flexural strength was reported to be due to the higher filler concentration. The Nanomeric[NM] particles and Nanoclusters [NC] are fundamentally different from particles in microfill fillers. The use of spheroidal NC fillers with their broad particle distribution helps to obtain high filler loading, desirable handling characteristics and physical properties comparable with those of commercial hybrid composites. The NM particles in these formulations fill the interstitial spaces between the clusters. The resultant surface, thus, is densely packed with fillers. Hence when subjected to abrasion only nanosized particles are plucked away, leaving the surfaces with defects which are smaller [14, 17, 29, 31, 36]. In the present study the better performance of Fluorocore when compared to the nanocomposite could be attributed to the composition of monomer used in Fluorocore. Fluorocore uses UDMA as the monomer whereas Filtek Z350 nanocomposite uses TEGDMA monomer. A study done by Erik Asmussen, Anne Peutzfeldt on the influence of UDMA, BisGMA and TEGDMA on mechanical properties of experimental resin composites showed that the monomer containing BisGMA or TEGDMA substituted by UDMA resulted in an increase flexural strength, and that substitution of BisGMA by TEGDMA reduced the flexural strength. TEGDMA monomer used in nanocomposite could be the reason for lower strength obtained in this study when compared to Fluorocore. These results are in accordance with the studies done by Yuzugullu et al. where the properties of nanocomposites though was comparable to packable composites, but still lesser than packable composites [3, 17]. The results of the present study wherein the compressive and flexural strength of Fluorocore was shown to be higher than amalgam and GIC is in accordance with a study done by Levartovsky which compared the diametral tensile strength, flexural strength, and compressive strength of core materials like light-activated glass ionomer cement (VariGlass VLC) and a fluoride-release dual cure composite resin (FluoroCore), with those of a conventional silver-reinforced glass-ionomer cement (Miracle Mix). The results of this study showed that diametral tensile strength, flexural strength, and compressive strength of the FluoroCore and VariGlass VLC materials were significantly higher than those of the conventional Miracle Mix [4, 28]. The CS value for amalgam was lower than that of composites tested and higher than Vitremer. Amalgam cores are certainly to be preferred over glass ionomer cement (GIC) cores. This result is in accordance with the results of the study by Cho et al. [2]. The FS value for amalgam was the least when compared to all the materials tested. This could be due the fact that the modulus of elasticity of composites is approximately one-third the modulus of elasticity of amalgam; that is, amalgams are three times more rigid. Glass ionomer-based materials were markedly weaker than the other materials in CS and FS tests used in the study, which is in accordance with the results of other studies on physical and mechanical properties of core build-up materials wherein FS and CS values of dualcure composite resin were higher than that of GIC core materials. Vitremer had the least strength among materials tested which is also in accordance to another study done by Yuzugullu et al. where similar results were seen. Thus, the role of glass ionomers and glass ionomer-based materials as cores must be questioned [1–6, 8, 28, 32, 37, 40, 48]. However all four materials tested were found to have mean CS values (>100 MPa) greater than the minimum value (50 MPa) recommended for dental amalgam. The use of standardized protocols in this study, such as ISO 4049, allows the results from different studies to be compared. Despite such standardization, these data demonstrate variation, as limitations still exist when trying to extrapolate these results to the clinical performance of materials, since the ISO 4049 standards for compressive and flexural strength testing recommend submerging the specimen in distilled water for only 24 h at 37 ± 1° C prior to testing. Furthermore, the specimen is submitted to only one mechanical cycle before submitting to fracture and also the material is cured in an ideal condition sans the oral cavity condition difficulties like saliva, visibility issues, operator handling of material etc. which could play an important role in curing and setting of the material which would influence the strength of the material greatly. Thus these specifications do not reflect the material’s long-term performance. Despite these considerations, the compressive strength test and the 3-point bending test used according to ISO 4049 is considered a standard test. Strength is the most important aspect for selection of a core material as stronger the material better is their ability to resist deformation and fracture. The results obtained from this study prove that the strength of Fluorocore material is higher than the nanocomposite Filtek Z350. However both of these materials have better strength and mechanical properties as compared to the conventional core build up materials, amalgam & GIC. Hence the core material selection must include the understanding of materials’ properties and no one material may be considered ideal and capable of truly replacing lost tooth structure. The clinicians should have a clear knowledge of the mechanical properties of the materials in order to obtain the best clinical outcome.
Conclusion
Within the limitations of this in vitro study, the following conclusions were drawn:
Fluorocore had the highest compressive strength and flexural strength of the four materials tested in this study.
The strength of Filtek Z350 was less than Fluorocore but higher than other conventional core build up materials like amalgam and vitremer GIC.
As reported in many other earlier studies the strength of GIC in the present study was found to be inadequate to be used as core build up material as its compressive strength was very less in comparison to composite and amalgam.
Amalgam can be used as a core build up material in situations where the tooth structure loss is minimal as it had the least flexural strength and its usage is limited to posterior teeth as the dark color of amalgam precludes its use in the anterior esthetic zone.
References
- 1.Combe EC, Shaglouf AM, Watts DC, Wilson NHF. Mechanical properties of direct core materials. Dent Mat. 1999;15:158–165. doi: 10.1016/S0109-5641(99)00027-5. [DOI] [PubMed] [Google Scholar]
- 2.Cho GC, Kaneko LM, Donovan TE, White SN. Diametral and compressive strength of dental core materials. J Prosthet Dent. 1999;82:272–276. doi: 10.1016/S0022-3913(99)70079-X. [DOI] [PubMed] [Google Scholar]
- 3.Yuzugully B, Ciftci Y, Saygili G, Canay S. Diametrical tensile and compressive strength of several core materials. J Prosthet Dent. 2008;17:102–107. doi: 10.1111/j.1532-849X.2007.00269.x. [DOI] [PubMed] [Google Scholar]
- 4.Levartovsky S, Kuyinu E, Georgescu M, Goldstein GR. A comparison of the diametral tensile strength, the flexural strength, and the compressive strength of two new core materials to a silver alloy-reinforced glass ionomer material. J Prosthet Dent. 1994;72:481–485. doi: 10.1016/0022-3913(94)90118-X. [DOI] [PubMed] [Google Scholar]
- 5.Bonilla ED, Mardirossian G, Caputo AA. Fracture toughness of various core build-up materials. J Prosthet Dent. 2000;9:14–18. doi: 10.1111/j.1532-849x.2000.00014.x. [DOI] [PubMed] [Google Scholar]
- 6.Saygili G, Sahmali SM. Comparative study of the physical properties of core materials. Int J Periodontics Restorative Dent. 2002;22:355–363. [PubMed] [Google Scholar]
- 7.Santos GC, Jr, El-Mowafy O, Rubo JH. Diametrical tensile strength of a resin composite core with non metallic prefabricated posts: an invitro study. J Prosthet Dent. 2004;91(4):335–341. doi: 10.1016/j.prosdent.2004.01.017. [DOI] [PubMed] [Google Scholar]
- 8.Kovarik RE, Breeding LC, Caughman WF. Fatigue life of three core materials under simulated chewing conditions. J Prosthet Dent. 1992;68:584–590. doi: 10.1016/0022-3913(92)90370-P. [DOI] [PubMed] [Google Scholar]
- 9.Lo CS, Millstein PL, Nathanson D. In vitro shear strength of bonded amalgam cores with and without pins. J Prosthet Dent. 1995;74:385–391. doi: 10.1016/S0022-3913(05)80379-8. [DOI] [PubMed] [Google Scholar]
- 10.Olivia RA, Lowe JA. Dimensional stability of silver amalgam and composite used as core materials. J Prosthet Dent. 1987;57:554–559. doi: 10.1016/0022-3913(87)90335-0. [DOI] [PubMed] [Google Scholar]
- 11.Piwowarczk A, Ottl P, Lauer HC, Buchler A. Laboratory strength of glass ionomer cement, compomers and resin composites. J Prosthet Dent. 2002;11:86–91. [PubMed] [Google Scholar]
- 12.Manhart J, Kunzelmann KH, Chen HY, Hickel R. Mechanical properties and wear behavior of light-cured packable composite resins. Dent Mater. 2000;16:33–40. doi: 10.1016/S0109-5641(99)00082-2. [DOI] [PubMed] [Google Scholar]
- 13.Leinfelder KF, Bayne SC, Swift ED., Jr Packable composites: overview and technical considerations. J Esthet Dent. 1999;11:234–249. doi: 10.1111/j.1708-8240.1999.tb00405.x. [DOI] [PubMed] [Google Scholar]
- 14.Mitra SB, Wu D. Holmes BN an application of nanotechnology in advanced materials. J Am Dent Assoc. 2003;134:1382–1390. doi: 10.14219/jada.archive.2003.0054. [DOI] [PubMed] [Google Scholar]
- 15.Core materials: laboratory testing methods. ADA Prod Rev (2008) 3(4): 1–12
- 16.Posterior composites: laboratory testing methods. ADA Prod Rev (2006) 1(1): 3–9
- 17.Monteiro GQM, Montes MAJRM. Evaluation of linear polymerization shrinkage, flexural strength and modulus of elasticity of dental composites. Mater Res. 2010;13(1):51–55. doi: 10.1590/S1516-14392010000100012. [DOI] [Google Scholar]
- 18.Filho LER, Burger LADS, Kenshima S, Bauer JRDO, Medeiros IS. Effect of light-activation methods and water storage on the flexural strength of two composite resins and a compomer. Braz Oral Res. 2006;20(2):143–147. doi: 10.1590/s1806-83242006000200010. [DOI] [PubMed] [Google Scholar]
- 19.Roberto Sorrentinob R, et al. Three-dimensional finite element analysis of strain and stress distributions in endodontically treated maxillary central incisors restored with different post, core and crown materials. Dental Mater. 2007;23:983–993. doi: 10.1016/j.dental.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 20.Nurray A, Ozel Y. A comparison of the flexural strength and modulus of elasticity of different resin composites. J Hacettepe. 2007;31:26–35. [Google Scholar]
- 21.Cohen BI, Pagnillo M, Newman I, Musikant BL, Deutsch AS. Cyclic fatigue testing of five endodontic post designs supported by four core materials. J Prosthet Dent. 1997;78:458–464. doi: 10.1016/S0022-3913(97)70060-X. [DOI] [PubMed] [Google Scholar]
- 22.Cohen BI, Pagnillo M, Newman I, Musikant BL, Deutsch AS. Fracture strength of three core restorative materials supported with or without a prefabricated splint shank post. J Prosthet Dent. 1997;78:560–565. doi: 10.1016/S0022-3913(97)70006-4. [DOI] [PubMed] [Google Scholar]
- 23.Gateau P, Sabek M, Dailey B. In vitro fatigue resistance of glass ionomer cements used in post and core restorations. J Prosthet Dent. 2001;86:149–155. doi: 10.1067/mpr.2001.114882. [DOI] [PubMed] [Google Scholar]
- 24.Sidoli GE, King PA, Setchell DI. An in vitro evaluation of a carbon fiber-based post and core system. J Prosthet Dent. 1997;78:5–9. doi: 10.1016/S0022-3913(97)70080-5. [DOI] [PubMed] [Google Scholar]
- 25.Shaini FJ, Fleming GJP, Shortall ACC, Marquis PM. A comparison of the mechanical properties of a gallium based alloy with a spherical high copper amalgam. Dent Mater. 1999;17:142–148. doi: 10.1016/S0109-5641(00)00054-3. [DOI] [PubMed] [Google Scholar]
- 26.Rafiee MA, Rafiee J (2009) Strength properties of light cured dental restorative composites. http://www.rafiee.us/files/Biomaterials_NEBEC.pdf
- 27.Ahn SG, Sorenson JA. Comparison of mechanical properties of various post and core materials. J Korean Acad Prosthodont. 2003;41:288–296. [Google Scholar]
- 28.Levartovsky S, Goldstein GR, Georgescu M, Goldstein GR. Shear bond strength of several new core materials. J Prosthet Dent. 1996;75:154–158. doi: 10.1016/S0022-3913(96)90092-X. [DOI] [PubMed] [Google Scholar]
- 29.Rodrigues SA, Jr, Ferracane JL, Della Bona A. Flexural strength and Weibull analysis of a microhybrid and a nanofill composite evaluated by 3- and 4-point bending tests. Dent Mater. 2008;24:426–431. doi: 10.1016/j.dental.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 30.Huysmans MCDNJM, Van der Varst PGT. Mechanical longevity estimation model for post-and-core restorations. Dent Mater. 1995;11:252–257. doi: 10.1016/0109-5641(95)80058-1. [DOI] [PubMed] [Google Scholar]
- 31.Rodrigues SA, Jr, Scherrer SS, Ferracane JL, Bona DI. Microstructural characterization and fracture behavior of a microhybrid and a nanofill composite. Dental Mater. 2008;24:1281–1288. doi: 10.1016/j.dental.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 32.Stober T, Rammelsberg P. The failure rate of adhesively retained composite core build-ups in comparison with metal-added glass ionomer core build-ups. J Dent. 2005;33:27–32. doi: 10.1016/j.jdent.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 33.Arksornnukit M, Takahash HJ. Thermo-hydrolytic stability of core foundation and restorative composites. J Prosthet Dent. 2004;92(4):348–353. doi: 10.1016/j.prosdent.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 34.Yamazaki T, Scheicker SR, Brantley WA, Culbertson BM, Johnston W. Viscoelastic behavior and fracture toughness of six glass ionomer cements. J Prosthet Dent. 2006;96:266–272. doi: 10.1016/j.prosdent.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 35.Satish G, Nainan MT. Invitro evaluation of flexural strength and flexural modulus of elasticity of different composite restoratives. J Conserv Dent. 2006;9:140–147. doi: 10.4103/0972-0707.42316. [DOI] [Google Scholar]
- 36.Moraes RR, Goncalves LS, Lancellotti, Consani S, Sobrinho LC. Nanohybrid resin composites : nanofiller loaded materials or traditional microhybrid resins? J Operative Dent. 2009;34:551–557. doi: 10.2341/08-043-L. [DOI] [PubMed] [Google Scholar]
- 37.Lakshmi S, Krishna VG, Sivagami Prosthodontic considerations of endodontically managed teeth. J Conserv Dent. 2006;9:104–109. doi: 10.4103/0972-0707.42355. [DOI] [Google Scholar]
- 38.Upadhyay NP, Kishore G. Glass ionomer cements—the different generations. Trends Biomater Artif Organs. 2005;18:158–165. [Google Scholar]
- 39.Fukui Y, Komada W, Yoshida K, Otake S, Okada D, Miura H. Effect of reinforcement with resin composite on fracture strength of structurally compromised roots. Dent Mater. 2009;28:602–609. doi: 10.4012/dmj.28.602. [DOI] [PubMed] [Google Scholar]
- 40.Shenoy A. End of road for amalgam. J Conserv Dent. 2008;11:99–107. doi: 10.4103/0972-0707.45247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kerby RE, Knobloch L, Thakur A. Strength properties of visible light cured resin modified glass ionomer cements. J Operative Dent. 1997;22:79–83. [PubMed] [Google Scholar]
- 42.Asmussen E, Peutzfeldt A. Influence of UEDMA, BisGMA and TEGDMA on selected mechanical properties of experimental resin composites. Dent Mater. 1998;14(1):51–56. doi: 10.1016/S0109-5641(98)00009-8. [DOI] [PubMed] [Google Scholar]
- 43.Annusavice KJ (2004). In: Phillips’ Sciences of Dental Materials, 11th edn. Elsevier, St. Louis (1st Indian reprint)
- 44.Arrais CAG, Kasaz AC, Albino LGB, Rodrigues JA, Reis AF. Effect of curing mode on the hardness of dual-cured composite resin core build-up materials. Braz Oral Res. 2010;24(2):245–249. doi: 10.1590/S1806-83242010000200019. [DOI] [PubMed] [Google Scholar]
- 45.Resin-based composites J Am Dent Assoc (2003) 134;510–512 134 [DOI] [PubMed]
- 46.3M/ESPE–Filtek™ Z350 Universal Restorative System—Technical Product Profile
- 47.McLean JW. Cermet cements. J Am Dent Assoc. 1990;120:43–47. doi: 10.14219/jada.archive.1990.0021. [DOI] [PubMed] [Google Scholar]
- 48.Akkayan B, Gulmez T. Resistance to fracture of endodontically treated teeth restored with different post systems. J Prosthet Dent. 2002;87:431–437. doi: 10.1067/mpr.2002.123227. [DOI] [PubMed] [Google Scholar]
- 49.American National Standards Institute and American Dental Association (1993) Specification no. 27: Resin-based filling materials. American Dental Association, Chicago
- 50.Rathke BK. Using core markers to enhance visualization of the core material/tooth interface. J Am Dent Assoc. 2001;132:778–779. doi: 10.14219/jada.archive.2001.0275. [DOI] [PubMed] [Google Scholar]