Abstract
Background:
High level of semen reactive oxygen species is considered as an important factor in male infertility. Sesame has antioxidant properties, which could be effective on improvement of semen parameters. This study was designed to determine the effects of sesame on sperm quality.
Materials and Methods:
Twenty-five infertile men entered this clinical trial. They were treated with a 3-months course of taking 0.5 mg/kg sesame. The pre intervention sperm analysis (sperm count, motile sperm percentage and normal morphology sperm percentage) was compared with post treatment sperm analysis. Based on the post intervention seamen analysis, patients were advised to undergo either IVF or ICSI to assess their fertility status.
Results:
There was significant improvement in the sperm count (10.56 ± 5.25 vs. 22.71 ± 30.14 million per ml) and motility (15.32 ± 13.58 vs. 23.32 ± 20.61 percent) after treatment with sesame (P value: 0.04 and <0.0001 respectively), but there was no significant improvement in sperm morphology after the treatment (10.72 ± 6.66 vs. 13.20 ± 11.14 percent, P value: 0.10). Three patients (12%) underwent IUI, which resulted in 1 successful pregnancy. Two patients (8%) underwent ICSI, which was not successful; however 2 (8%) patients had spontaneous pregnancy. Fortunately, all pregnancies led to live birth. Except 1 case of diarrhea, no other major side effect was reported.
Conclusion:
Sesame improved sperm count and motility, and can be prescribed as an effective and safe method for male factor infertility.
Keywords: Male infertility, infertility, semen quality, sesame
INTRODUCTION
Approximately 8% of men seek medical help for fertility associated problems.[1] Male infertility is caused by a broad variety of etiologies; therefore, different of approaches are needed to resolve this problem.[2] Many investigations have been performed to find out new effective treatments, and important advances have been achieved in both diagnosis and treatment of male infertility.[3] ccording to the underlying cause, non-surgical or surgical treatments, including hormone therapy with testosterone, human chorionic gonadotropin (hCG), clomiphene citrate and bromocriptine;[4] or in vitro fertilization (IVF) and intra-cytoplasmic sperm injection (ICSI), may be used to treat an infertile man.[5,6,7,8]
In addition to the aforementioned treatments, several novel or traditional methods which are different from classic approaches have been used to treat male infertility. For instance, different methods of traditional Chinese medicine (TCM) including herbal remedies and acupuncture and various other traditional methods have been administered in animal models or in human for male infertility treatment.[9,10,11,12,13,14]
Some traditional physicians prescribe sesame to promote male fertility.[2] Animal studies showed that sesame can improve sperm quality and male fertility.[15,16]
Sesame is one of the richest sources of lignans including sesamin, episesamin, sesamolin, and tocopherol, which are known to have health benefits due to having anti-tumorigenic, estrogenic and/or anti-estrogenic and antioxidant properties.[15,17]
Although, there are several studies on animal models regarding the effects of sesame on male fertility and sperm quality,[15,16] no clinical trial has been performed yet to investigate this effect on human. For this reason, this study was designed to determine the effects of sesame on sperm quality.
MATERIALS AND METHODS
This self-controlled clinical trial was performed on 25 infertile men who were referred to the Shahid Beheshti infertility center, Isfahan, Iran between 2010 and 2011.
Two semen analyses were performed for all primary infertile couples with an 8-week interval, and men aged between 25-45 years who had 2 sperm analyses consisted with WHO criteria for male infertility (sperm count <20,000,000/ml, motile sperm <50%, normal morphology sperm <30%) entered the study.[18,19]
In addition to smokers and patients with azospermia, patient who had a previous history of taking sesame, sesame products or other infertility treatment at the same time; trauma to the testes, chemotherapy, urogenital surgery or radiotherapy; anatomic abnormality of the urogenital system confirmed by a urologist; or fertility problem in spouse confirmed by gynecologist were excluded from the study.
Consort diagram summarizes the participants’ flow [Figure 1].
Figure 1.
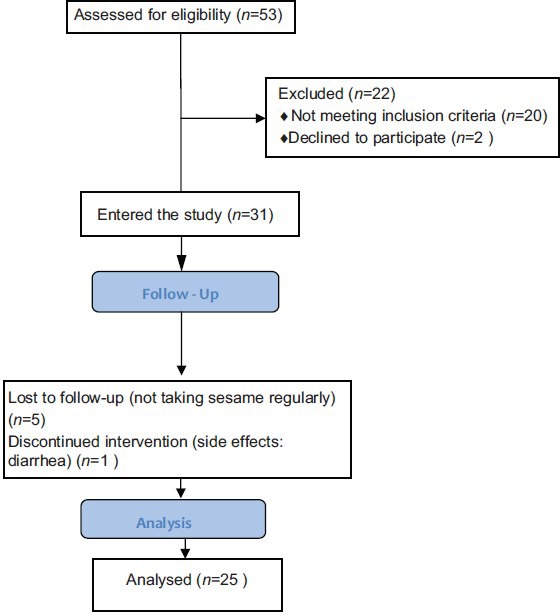
Consort diagram of participant flow
This study was approved by the ethics committee of Isfahan University of Medical Sciences (research project number: 390108), and informed consent was obtained from the men included in the study.
All sperm samples were taken after 3 days of abstinence. The baseline semen analyses (sperm count, motile sperm percentage and normal morphology sperm percentage) were recorded in the patient's file, and patient was commenced on oral powder of sesamum indicum sachets 0.5 mg/kg (prepared by Goldaru Company, Iran) for 3 months.
At the end of the 3rd month, another semen analysis was performed at the same lab.
After comparison of pre and post treatment sperm parameters, patients were categorized to 3 groups of improved (post treatment sperm parameters more than pretreatment values), no change (post treatment sperm parameters similar to the pretreatment values) or deteriorated (post treatment sperm parameters less than pretreatment values).
Then, based on the post treatment semen analysis patients were referred for IVF or ICSI.
IVF was considered feasible if >1 million normal spermatozoa were isolated, and ICSI was performed if <1 million normal spermatozoa were isolated,[20,21] total motility was reduced or teratozoosperima (4%> normal morphology spermatozoa) was found according to the WHO criteria.[20,21] Patients who had total motile sperm count more than or equal to 10 million per ml, and had normal morphology more than or equal to 4% were selected for intra uterine insemination (IUI).[20] IVF, ICSI or IUI was performed according to the standard protocols.[20,21]
Patients who had severe oligozoospermia (sperm count less than 5 million sperm per ml) were referred for karyotyping.
Normal distribution of data was checked by SPSS.16.5 software, Chicago, the USA, and then paired t-test and was used for analysis. Results of quantitative and qualitative variables are presented as mean ± SD and number (percent) respectively. P value less than 0.05 was considered as the level of significance.
RESULTS
Thirty-one patients entered the study, but only 25 patients completed the treatment by taking sesame for 3 months. Participants were aged between 27 and 40 years, and mean age was 33.87 ± 3.85 years. Mean of body mass index of patients was 25.82 ± 3.68 kg/m2 (minimum: 19.57 and maximum: 35.92 kg/m2).
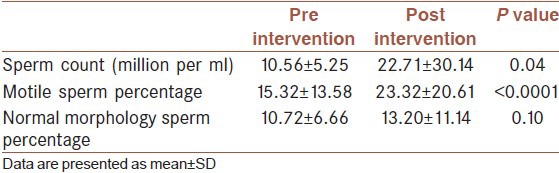
Comparison of pre and post treatment semen analysis showed significant improvement in the sperm count (10.56 ± 5.25 vs. 22.71 ± 30.14 million per ml) and motility (15.32 ± 13.58 vs. 23.32 ± 20.61 percent) after treatment with sesame (P value: 0.04 and <0.0001 respectively), but there was no significant improvement in sperm morphology after the treatment (10.72 ± 6.66 vs. 13.20 ± 11.14 percent, P value: 0.10) [Table 1].
Table 1.
Comparison of pre and post intervention semen analysis
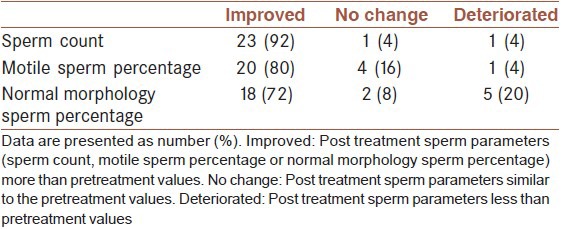
Based on changes in the sperm parameters, patients were divided to 3 groups of improved sperm parameter, no changes in the sperm parameters and deteriorated sperm parameters [Table 2]. It showed that most of the participants experienced improvement of the semen parameters (sperm count, motile sperm percentage and normal morphology sperm percentage) after treatment with sesame.
Table 2.
Sperm parameter change status
Four patients who had sperm count less than 5 million sperm per ml were referred for karyotyping. All karyotype results were normal.
Based on the post intervention sperm analysis, 3 (12%) patients were suitable for IUI. After performing IUI, only 1 (4%) patient had successful pregnancy. In addition, only 2 (8%) patients underwent ICSI, which did not result in successful pregnancy. Two patients (8%) had successful spontaneous pregnancy without IVF or ICSI. Fortunately, all pregnancies led to live birth.
One of the patients stopped taking sesame due to diarrhea. No other major side effect was reported.
DISCUSSION
We investigated the effects of sesame on semen parameters, and found that adding sesame to the patients’ diet for 3 months significantly improves sperm count and mobility. This is the first time, to our knowledge, that sesame effects on male factor infertility are evaluated in humans.
The previous study on animal subjects by Shittu et al., reported that sesame can improve epididymal sperm reserve, and increase spermatocyte size.[15]
Comparing to the control group, their study showed that epididymal lumens in the sesame treated rats were wider, had fewer irregular tubular formation and were significantly filled with spermatocytes. Then, they concluded that sesame improves epididymal sperm reserve, and leads to larger spermatocyte production in a dose related manner. This effect is considered to be through a complex hormonal interplay at the level of the male hypothalamic pituitarytesticular axis and estrogens receptors.[15]
Two other studies on rats by the same research team also confirmed our findings.[16,22] They found significantly higher sperm count in sesame groups than the control group in a dose related manner.
In addition, they reported that sesame treated group had significantly better sperm motility and morphology than the control group in a dose related manner.[16,23]
The only difference between our findings and aforementioned studies is the effect of sesame on the sperm morphology. This dissimilarity may be caused by inherent differences between rats and humans.
These beneficial effects of sesame on semen parameters may be attributed to the reactive oxygen species (ROS) and free radical scavenging moiety of sesame lignans. Sesame has a powerful anti-oxidant effect which inhibits lipid peroxidases, carnitine oxidase and other enzymes such as dismutase, which inhibit sperm motility and maturation in the epididymis.[16,24,25]
Sesame lignans have been shown to increase tissue tocopherol levels by inhibition of cytochrome P450 3A-dependent n-hydroxylase. Consequently, they potentiate the antioxidants activity of tocols in lipid peroxidation system.[24] Therefore, sesame lignans improve the quality of the produced sperm.[16]
An imbalance between production of reactive oxygen species (ROS) and ROS scavenging by seminal antioxidants results in seminal oxidative stress (OS). It is believed that seminal OS is one of the major factors, which cause sperm dysfunction and sperm DNA damage in male infertility.[26,27] Indeed, it is estimated that 25% of infertile men have high levels of semen ROS, whereas fertile men do not have high levels of semen ROS.[28,29] Although a controlled production of these ROS is necessary for sperm physiology (sperm hyperactivation, capacitation and acrosome reaction) and for natural fertilization,[28] the production of high level of ROS by immature germ cells and leukocytes leads to sperm dysfunction (lipid peroxidation, loss of motility and sperm DNA damage).[28]
Therefore, improvement of sperm parameters may be caused by antioxidant properties of sesame.
Unfortunately, majority of patients refused using assisted reproductive techniques. The main contributing factor for noncompliance was high expense of the procedure and patients’ economic problems. The small number of patients who underwent assisted reproductive technologies (ARTs) including IUI, IVF and ICSI prevents us to conclude about the efficacy of sesame on fertility improvement; however, there were 2 cases (8%) of spontaneous pregnancy and 1 (4%) case of ART pregnancy – a total number of 3 (12%) pregnancies- which is a promising outcome. In order to make a more accurate estimation about sesame effects on fertility, it is necessary to investigate a larger number of patients, and provide them with economic support to undergo ARTs to assess the effects of sesame on male factor infertility.
In summary, we conclude that taking sesame improves sperm count and motility in infertile men, and can be prescribed for these patients as an effective and safe treatment for male factor infertility.
ACKNOWLEDGMENT
We greatly thank and acknowledge our patients who helped us to perform this investigation, and staff of the infertility unit of Beheshti hospital for their collaboration.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Vital and Health Statistics, no. 26, CDC, 2002. [Last accessed on 2002]. Available from: http://www.cdc.gov .
- 2.Ashamu E, Salawu E, Oyewo O, Alhassan A, Alamu O, Adegoke A. Efficacy of vitamin C and ethanolic extract of Sesamum indicum in promoting fertility in male Wistar rats. J Hum Reprod Sci. 2010;3:11–4. doi: 10.4103/0974-1208.63115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Esteves SC, Miyaoka R, Agarwal A. An update on the clinical assessment of the infertile male. [corrected] Clinics (Sao Paulo) 2011;66:691–700. doi: 10.1590/S1807-59322011000400026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DeGroot LG, Jameson JL, editors. Endocrinology. 4th ed. Philadelphia: Saunders Company; 2001. Baker HWG 2001 Male infertility; pp. 3199–228. tePSC. [Google Scholar]
- 5.Friedl SR, Strassburger D, Schaster M, Soffer Y, Ron-El R. Factors influencing the outcome of ICSI in patients with obstructive and nonobstructive azoospermia: A comparative study. Hum Reprod. 2002;17:3114–21. doi: 10.1093/humrep/17.12.3114. [DOI] [PubMed] [Google Scholar]
- 6.Vernaeve V, Tournaye H, Osmanagaoglu K, Verheyen G, Van Steirteghem A, Devroey P. Intracytoplasmic sperm injection with testicular spermatozoa is less successful in men with nonobstructive azoospermia than in men with obstructive azoospermia. Fertil Steril. 2003;79:529–33. doi: 10.1016/s0015-0282(02)04809-4. [DOI] [PubMed] [Google Scholar]
- 7.Monzó A, Kondylis F, Lynch D, Mayer J, Jones E, Nehchiri F, et al. Outcome of intracytoplasmic sperm injection in azoospermic patients: Stressing the liaison between the urologist and reproductive medicine specialist. Urology. 2001;58:69–75. doi: 10.1016/s0090-4295(01)01012-3. [DOI] [PubMed] [Google Scholar]
- 8.Van Peperstraten AP, Johnson NP, Philipson G. Techniques for surgical retrieval of sperm prior to ICSI for azoospermia. Cochrane Database Syst Rev. 2006;3:CD002807. doi: 10.1002/14651858.CD002807.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Berkley M. Treating infertility: Differences between Western reproductive medicine and traditional Chinese medicine. Midwifery Today Int Midwife. 2011;97:25–6. [PubMed] [Google Scholar]
- 10.Chang DG. TCM treatment of male infertility. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2007;27:969. [PubMed] [Google Scholar]
- 11.Cheong Y, Nardo LG, Rutherford T, Ledger W. Acupuncture and herbal medicine in in vitro fertilisation: A review of the evidence for clinical practice. Hum Fertil (Camb) 2010;13:3–12. doi: 10.3109/14647270903438830. [DOI] [PubMed] [Google Scholar]
- 12.Lin T, Huang X. Treatment of male infertility. J Tradit Chin Med. 2007;27:119–23. [PubMed] [Google Scholar]
- 13.Tempest HG, Homa ST, Routledge EJ, Garner A, Zhai XP, Griffin DK. Plants used in Chinese medicine for the treatment of male infertility possess antioxidant and anti-oestrogenic activity. Syst Biol Reprod Med. 2008;54:185–95. doi: 10.1080/19396360802379073. [DOI] [PubMed] [Google Scholar]
- 14.Wang R, Xu L, Zhang WX, Wu YF, Shi JH, Zhang YX. Shengjing granule: An effective Chinese medicine for spermatogenic disturbance in mice. Zhonghua Nan Ke Xue. 2008;14:1046–9. [PubMed] [Google Scholar]
- 15.Shittu LA, Bankole MA, Oguntola JA, Ajala O, Shittu RK, Ogundipe OA, et al. Sesame leaves intake improve and increase epididymal spermatocytes reserve in adult male Sprague Dawley rat. Sci Res Essay. 2007;2:319–24. [Google Scholar]
- 16.Shittu LA, Adesite SO, Ajala MO, Bankole MA, Benebo AS, Tayo AO, et al. Sesame Radiatum Phytoestrogenic Lignans Enhances Testicular Activity In Adult Male Sprague Dawley Rat Testis. Int J Morphol. 2008;26:643–52. [Google Scholar]
- 17.Kizhiyedathu PS, Chami A. In vitro studies on antioxidant activity of lignans isolated from sesame cake extract. J Sci Food Agri. 2005;85:1779–83. [Google Scholar]
- 18.Department of Reproductive Health and Research of World Health Organization. WHO laboratory manual for the examination and processing of human semen. (5th ed) 2010 [Google Scholar]
- 19.Speroff Leon FM. 7th ed. Philadelphia: Lippincott Williams and Wilkins; 2005. Clinical Gynecologic Endocrinology and Infertility; p. 1144. [Google Scholar]
- 20.Brinsden PR. Textbook of in vitro fertilization and assisted reproduction. 3rd ed. United Kingdom: Taylor and Francis; 2005. Management of infertile men; p. 56. [Google Scholar]
- 21.WHO Laboratory Manual for the Examination and Processing of Human Semen. 5th ed. Geneva: World Health Organization; 2010. World Health Organisation. [Google Scholar]
- 22.Shittu Lukeman AJ. Ikeja, Nigeria: MSc Dissertation Lagos State University, College of Medicine; 2006. The effect of the aqueous crude leaves extract of Sesamum radiatum compared to Mesterolone (proviron) on the adult male Sprague Dawley rats testis and epididymis. [Google Scholar]
- 23.Amini Mahabadi JH, Nikzad H, Taherian A, Eskandarinasab M, Shaheir M. Effect of diet contain sesame seed on Adult Male Wistar Rat Testis. Feyz J Kashan Univ Med Sci. 2011;15:1–11. [Google Scholar]
- 24.Hemalatha SR, Raghunath M, Ghafoorunissa Dietary sesame oils inhibits iron-induced oxidative stress in rats. Br J Nutr. 2004;92:581–7. doi: 10.1079/bjn20041239. [DOI] [PubMed] [Google Scholar]
- 25.Jeng KCG, Hou RCW. Sesamin and Sesamolin: Natures Therapeutic Lignans. Current Enzyme Inhibition. 2005;1:11–20. [Google Scholar]
- 26.Zini A SG, Baazeem A. Antioxidants and sperm DNA damage: A clinical perspective. J Assist Reprod Genet. 2009;26:427–32. doi: 10.1007/s10815-009-9343-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aitken RJ, Finnie JM, Hedges A, McLachlan RI. Analysis of the relationships between oxidative stress, DNA damage and sperm vitality in a patient population: Development of diagnostic criteria. Hum Reprod. 2010;25:2415–26. doi: 10.1093/humrep/deq214. [DOI] [PubMed] [Google Scholar]
- 28.Zini A, Al-Hathal N. Antioxidant therapy in male infertility: Fact or fiction? Asian J Androl. 2011;13:374–81. doi: 10.1038/aja.2010.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agarwal A, Nallella KP, Allamaneni SS, Said TM. Role of antioxidants in treatment of male infertility: An overview of the literature. Reprod Biomed Online. 2004;8:616–27. doi: 10.1016/s1472-6483(10)61641-0. [DOI] [PubMed] [Google Scholar]


