Abstract
Background:
Blacks have a higher incidence of diabetes and its related complications. Self-rated health (SRH) and perceived stress indicators are associated with chronic diseases. The aim of this study was to examine the associations between SRH, perceived stress and diabetes status among two Black ethnicities.
Materials and Methods:
The cross-sectional study included 258 Haitian Americans and 249 African Americans with (n = 240) and without type 2 diabetes (n = 267) (n = 507). Recruitment was performed by community outreach.
Results:
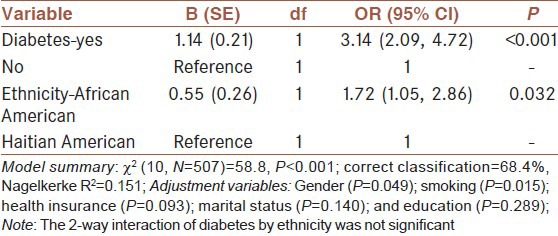
Haitian-Americans were less likely to report ‘fair to poor’ health as compared to African Americans [OR = 0.58 (95% CI: 0.35, 0.95), P = 0.032]; yet, Haitian Americans had greater perceived stress than African Americans (P = 0.002). Having diabetes was associated with ‘fair to poor’ SRH [OR = 3.14 (95% CI: 2.09, 4.72), P < 0.001] but not perceived stress (P = 0.072). Haitian-Americans (P = 0.023), females (P = 0.003) and those participants having ‘poor or fair’ SRH (P < 0.001) were positively associated with perceived stress (Nagelkerke R2 = 0.151).
Conclusion:
Perceived stress associated with ‘poor or fair’ SRH suggests that screening for perceived stress should be considered part of routine medical care; albeit, further studies are required to confirm our results. The findings support the need for treatment plans that are patient-centered and culturally relevant and that address psychosocial issues.
Keywords: African American, Haitian American, diabetes type 2, minority health, stress
INTRODUCTION
Diabetes, a metabolic disorder diagnosed by hyperglycemia, is a major cause of heart disease and kidney failure and is estimated to affect 8.3% of the US population.[1] Type 2 diabetes (90-95% of the cases of diabetes) requires adjustment to life-long care and management skills that can be emotionally overwhelming.[2,3] Poor glycemic control, diabetes-related complications and the stress of diabetes self-care have been implicated as causes of increased emotional and psychological distress for individuals with diabetes.[4] Non-Hispanic Blacks have 1.8 times higher age-adjusted rate of diabetes than Non-Hispanic Whites[1] (CDC). Diabetes related end-stage renal disease was nearly twice as likely for African Americans than Non-Hispanic Whites.[5]
Another measure related to several diseases and clinical outcomes is self-rated health (SRH).[6] It is a direct indicator of perception of health status and has been established as a marker of morbidity, largely from prospective studies during the past decades.[7] Having diabetes and diabetes-related complications can influence their quality of life and how they rate their health.[8] Operationally, SRH, as an ordinal question asking individuals to rank their health, has been demonstrated to be a strong indicator of the population's well-being throughout the literature.[9,10,11,12] This may be of particular importance for Blacks who have poorer health outcomes than Whites across socio-economic status.[13] Perceived stress was positively associated with health-related complaints for a worksite population.[14] Since stress has been shown to adversely affect health, it is likely that there will be a positive relationship between perceived stress and degree of poor SRH. Furthermore, perceived stress may differ by between Blacks (Haitian American versus African American) and diabetes status in the prediction of SRH.
Theoretical framework
Haitian Americans and African Americans have often been combined as one group (Blacks) for studies, yet their social beliefs and practices are likely to differ based on their distinct cultural backgrounds. Awareness of social factors and their relationship with stress may help in the prevention and treatment of type 2 diabetes. While most African Americans are born in the United States, Haitian Americans are generally immigrant minorities (born in Haiti). The dissimilarities of acculturation factors between African Americans and Haitian Americans, such as number of years of life lived in the United States and dominant language proficiency, influence their health beliefs and behaviors. Ethnicity has been defined, broadly, as a set of shared social beliefs and behaviors. As such, ethnicity may be viewed as part of the multi-dimensional environmental influences in accordance with an ecological perspective.[15] In applying an ecological model for this study, elements were borrowed from several sources.[15,16,17,18] The conceptual model of this study is depicted in Figure 1. Although health educators, for the most part, are aware that ethnic differences need to be taken into account, knowledge of possible intervention points for Haitian Americans versus African Americans is lacking. Since these two ethnicities have been combined and compared to Non-Hispanic Whites, rather than to each other for health studies there is no basis for speculating magnitude or direction of differences in outcomes. Therefore, this research aimed to assess 1) whether persons with diabetes would have higher stress than those without diabetes; 2) whether ‘fair or poor’ SRH would be associated with higher perceived stress than ‘good, very good, or excellent’ SRH; 3) whether perceived stress and SRH would differ by ethnicity: Haitian Americans versus African Americans; and, whether having diabetes is related to ‘fair or poor’ SRH.
Figure 1.
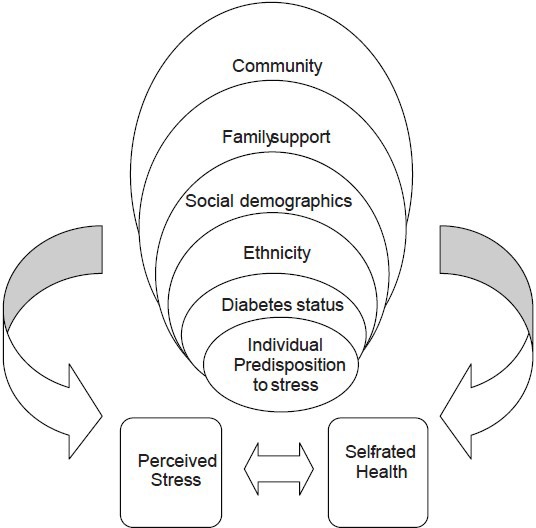
Conceptual model for perceived stress and self-rated health based on the ecological model. Elements of the conceptual model were borrowed from several sources.[19-21] The figure was composed by the authors of this paper, based on the idea of the ecological model applied to diabetes self-management by Fisher EB, Brownson CA, O’Toole ML, Shetty G, Anwuri VV, Glasgow RE. Ecological approaches to self-management: the case of diabetes. Am J Public Health. 2005;95(9): 1523-1535. Note: Community and family support were not measured in the current study
MATERIALS AND METHODS
Recruitment of participants
Study participants were recruited between the years 2008-2010. Sample size of 120 per group (ethnicity/ diabetes status), sufficient to determine a difference with a modest effect size (0.45) at 80% power and a type 1 error, α = 0.05, was based on in a similar study in Cuban-Americans. This was a cross-sectional study with complete data available for N = 507 participants: 120 African Americans and 120 Haitian Americans (n = 240) with type 2 diabetes and 129 African Americans and 138 Haitian Americans (n = 267) without type 2 diabetes. African American participants were initially recruited by randomly generated mailing lists. The lists of addresses (available for African Americans but not Haitian Americans) were purchased from Knowledge Base Marketing, Inc., Richardson, TX, U.S. This company provided two mailing lists generated from multiple databases of African Americans, identified as having or not having type 2 diabetes from Miami-Dade and Broward Counties, Florida, U.S. Recruitment of Haitian Americans from community-based sources included: Outreach to community health care professionals; the university community; advertisements in local Haitian newspapers and local radio ads. Recruitment was terminated when adequate sample size was reached for both Haitian Americans and African Americans.
Institutional review board (IRB) protocol and study design
The study protocol, a cross-sectional design, was approved by Florida International University's IRB, with approval based on the decision of an ethical committee composed of 21 members and allowing the recruitment of 550 participants. All participants who understood, agreed and signed the IRB's informed consent form were eligible to participate in the study. Eligibility was based on interviewers’ screening of age (≥35 years), self-reported ethnicity (either reporting being of African descent for African American or of Haitian descent for Haitian American) and diabetes status. Inquiry of ethnicity included questions of cultural identification and place of birth. Diabetes status (diagnosed with type 2 diabetes or not) was determined by reported year of diagnosis and then confirmed by laboratory reports. Individuals with fasted blood glucose ≥ 126 mg/dL were classified as having diabetes.[19]
Inclusion criteria for both those with and without diabetes consisted of male and female African Americans and Haitian Americans age ≥35 years, not pregnant or lactating, no thyroid disorders, no cancer, HIV/AIDS, no liver or kidney disease and no major psychiatric disorders. Respondents with diabetes were asked for the age of diagnosis with diabetes and initial treatment modalities (with or without insulin). Respondents were included with self-reported type 2 diabetes, for the group with diabetes and participants without diabetes met the same criteria, except they were free of diabetes. Participants self-reported as ‘without diabetes’ and whose fasted blood glucose levels and hemoglobin A1C were above the normal range were referred to their physician with their laboratory results. In addition, individuals whose fasted blood glucose levels and hemoglobin A1C were positive for diabetes were reclassified as having diabetes. This resulted in 8 Haitian Americans and 4 African Americans being reclassified as having type 2 diabetes. All data were collected in the principal investigator's research laboratory at a single time point, taking approximately 4 h. Participants read, understood and signed the informed consent form in English or Creole and were compensated for their time and travel to the research laboratory within the guidelines of the IRB.
Data collection procedures
This study adhered to the IRB's requirements on the use of human subjects. Trained interviewers bilingual in English and Creole administered the questionnaires. The socio-demographic check list was constructed by the principal investigator and included questions about age, gender, tobacco use, education, income, language preference, health insurance, and self-rated health (SRH). The variable, SRH, was in response to the question, “In general, would you say your health is: (Check one box).” Self-rated health was measured on a 5-point scale (excellent, very good, good, fair and poor).[6] We collapsed SRH to a binary variable (fair/poor versus good, very good, excellent) since there were less than 10 participants per category when comparing by ethnicity, diabetes status and gender. The binary variable has been found to be comparable to the 5-point ordinal variable. The two SRH variable (binary and ordinal) were found to have no statistical differences when comparing the proportion odds ratios of ordinal (all categories of SRH) to odds ratio of logistic regression (fair/poor versus good, very good, excellent).[20,21,22]
Perceived stress
To measure perceived stress, the Perceived Stress Scale (PSS-10)[23,24] was administered with permission from the John E. and Catherine MacArthur Research Network on Socioeconomic Status and Health. The PSS-10 is a newer, shorter version of the original PSS-14 derived by dropping four items with relatively low factor loadings. Little or no overlap was found between constructs and the internal reliability of the PSS-10 was reported as a Cronbach's alpha coefficient = 0.78.[24] Normality measures, based on a probability sample of the United States (Harris Poll), indicated that the groups “Black” “Hispanic” “other minority” had higher mean PSS scores than the group “White” but there was no significant difference in any combination of minority comparisons.[24] Invariance was found by age, gender, education, employment, household size, and marital status and smoking; whereas, frequency of drinking alcohol was not related to PSS.[24] A single composite score (0-40 points) was constructed to form the outcome variable, perceived stress. The response categories and their corresponding scores were ‘never’= 0, ‘almost never’ = 1, ‘sometimes’ = 2, ‘fairly often’ = 3, and ‘very often’ = 4. The four items that measured coping were reverse coded (where ‘never’ = 4, ‘almost never’ = 3, etc.) to reflect stress as per the questionnaire coding instructions.
Anthropometrics
Waist circumference was measured to the nearest 1 cm at a level midway between the lower rib margin and the iliac crest with a non-stretchable tape all around the body in horizontal position.[25] Height and weight were measured to the nearest 0.5 cm and 0.1 kg, respectively. Body mass index was calculated as weight (kg) divided by height (m) squared.[26]
Blood collection and analysis
Approximately 20 ml of venous blood was collected from each subject after an overnight fast (at least 8 h) by a certified phlebotomist using standard laboratory techniques. Blood samples were collected into a vacutainer serum separator tube for analysis of lipids and glucose and a tube with EDTA for hemoglobin A1C. After complete coagulation (30-45 min), the serum separator tube was centrifuged at 2500 RPM for 30 min. Glucose levels were measured by hexokinase enzymatic methods and lipid panel was assayed by enzymatic methods by Laboratory Corporation of America, Miami, FL (LabCorp®). Hemoglobin A1C percentages were measured from whole-blood samples using the Roche Tina Quant method (LabCorp®). For this study, blood glucose was used to confirm self-reported type 2 diabetes, where a blood glucose level of ≥126 mg/ml was classified as having diabetes.[19]
Statistical analysis
Prior to conducting analyses, all constructed composite scales and covariates were examined for normality by the Kolmogorv-Smirov test and linearity by Q-Q plots. Body mass index was natural logarithmically transformed to achieve a more normal distribution of values. Descriptive variables were compared by student t-test and categorical variables by Chi-squared. General linear models were performed with the independent variables, ethnicity, diabetes status, gender and self-reported health. Full models included socio-demographic covariates that have potential as confounders including age, gender, education, (body mass index and waist circumference in separate models due to collinearity), health insurance, marital status, and smoking, with the dependent variable perceived stress. Logistic regression models were performed for SRH as the dependent variable with ethnicity and diabetes status as the primary independent variables and socio-demographics as controls. All covariates with known clinical significance and P values <0.25 were retained for final models.[27] Even though a multitude of factors were invariant for perceived stress (tested with PSS-10) on a national population, the differences between minorities were not significant. Moreover, invariance among Black ethnicities has not been determined.[24] Age was retained for all models, regardless of P value since it has been shown to be associated with perceived stress across ethnic and racial groups throughout the literature and by Cohen and Williamson[24] using the same instrument (PSS-10) as in this study. All analysis was conducted with SPSS version 18 (Chicago, Il, USA) and P values <0.05 were considered significant.
RESULTS
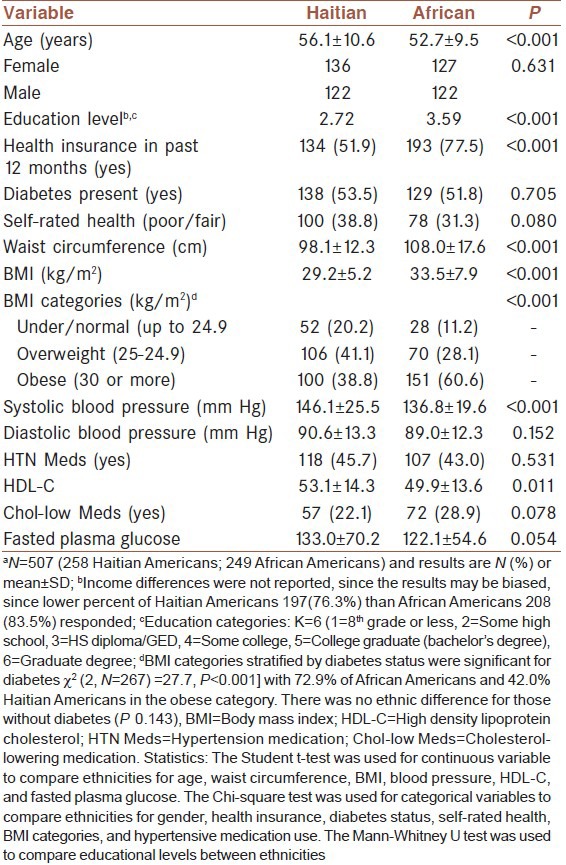
In contrast to the national statistic of approximately 59% of the population with Haitian ancestry reported being foreign born,[28] all Haitian Americans in our sample reported being born in Haiti, while less than 2% (4 out of 249) African Americans were born outside of the US. Moreover, 26.8% (68/258) of Haitian Americans reported living in the US 10 years or less and 39.1% (101/258) reported living in the US for 15 or less years. Thirty-eight percent (98/258) of Haitian Americans reported speaking no English. Additional characteristics of the study population are shown in Table 1. Compared to Haitian Americans, African Americans were younger, had a higher educational level, more likely to have health insurance, more likely to be currently smoking and less likely to be currently married. Of the combined study population (with and without diabetes), more African Americans had higher body mass indexes, waist circumferences and systolic blood pressure. For the combined study population, approximately twice the persons with diabetes [46.4% (124/267)] rated their health to be in the fair or poor category as compared to those without diabetes [22.5% (54/240)].
Table 1.
Characteristics of the study participantsa
Perceived stress
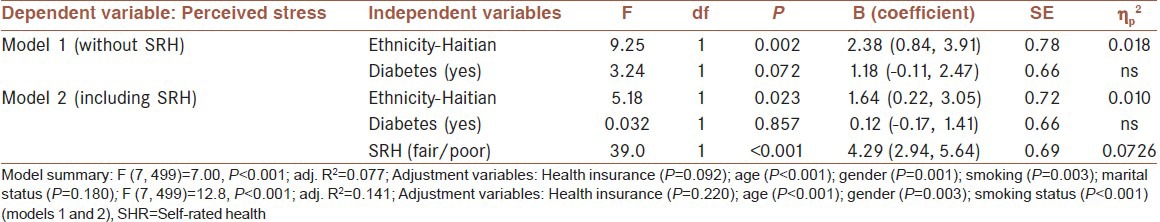
To test the primary hypothesis, that SRH would predict perceived stress, two hierarchical analysis with general linear models were conducted, first ethnicity and diabetes status without SRH (Model 1) and then adding SRH (Model 2) [Table 2]. The procedure for this analysis was to conduct full models with all the clinically significant controls based on the results of normative data by the developers of the perceived stress scale.[24] The final models were run with the hypothesized independent variables, clinically significant variables, and those controls with P < 0.25. For Model 1, education (P = 0.545) did not significantly change the hypothesized variables (ethnicity and diabetes status) so it was not retained for the final model. For Model 2, education (P = 0.656), then currently married (P = 0.331) were dropped since neither significantly changed the hypothesized variables. Hypothesis 1 was not supported, since being Haitian American, female and having ‘fair or poor’ SRH was positively associated with perceived stress; however, having diabetes was not associated with perceived stress. In addition to the hypothesized variables, several other socio-demographic covariates explained perceived stress.
Table 2.
Effect of ethnicity, diabetes status, self-rated health and socio-demographics on perceived stress
Self-rated health
Logistic regression models were performed to test the secondary hypothesis that self-rated health as ‘fair or poor’ will be explained by having diabetes independent of ethnicity and gender [Table 3]. A full model was run with the hypothesis variables and covariates that have been considered potential confounders in the literature: Age, education, having health insurance (yes/no), currently married (yes/no), currently smoking (yes/no) and body mass index. The hypothesis was partially supported, since individuals with diabetes had an increased likelihood of reporting fair to poor health. The hypothesis was not supported for ethnicity since Haitian Americans were less likely to report ‘fair to poor’ health as compared to African Americans. Current smokers were more likely while men were less likely to report ‘fair to poor’ health. There was no relationship between education level and having health insurance with respect to SRH.
Table 3.
Odds of ‘fair to poor’ self-rated health by ethnicity and diabetes status
DISCUSSION
Psychological stress has been considered a risk factor for coronary heart disease, along with other behavioral risk factors such as cigarette smoking, high alcohol consumption, and high sedentary/low physical activity.[29,30,31,32] In this study, those participants with fair to poor SRH had higher levels of perceived stress while controlling for ethnicity and diabetes status. Haitian Americans had higher levels of perceived stress as compared to African Americans; but African Americans were more likely to rate their health as fair to poor compared to Haitian Americans. The conceptual model was supported since factors such as ethnicity, gender, and diabetes status were associated with differences in health indicator: Stress and SRH. Higher perceived stress levels were found in women as compared to men independent of ethnicity and diabetes status. These findings were in congruence with a study in Whites, where more stress was also perceived by females than males.[33] In a study of older adults (>60 years) with cardiovascular disease (N = 502), women's level of functional health status was inversely associated with perceived stress and positively associated with self-esteem, whereas the relationship was not significant for men, even after adjustments for clinical factors.[33] Gender differences were reported in a race-related stress study[34] for a convenience sample of African American students (N = 183) attending a predominately White university in the Southeastern region of the United States. The authors found that women were more prone to stress induced anxiety and somatization symptoms from individual racism as compared to men; whereas, men reported more stress from institutional racism as compared to women.[34] Perceived racial discrimination and their associations with health were studied as a national probability sample by weighted clustered area design from households and hostile areas; data included 4,351 adults (76% African, 7% White, and 17% other) from the South African Stress and Health Study (SASH).[35] The authors reported that stress, measured by racial and non-racial discrimination and life events, was positively related to poor SRH (measured by the same 5-point scale question as in our study) and that perceived racial and non-racial discrimination were inversely related to psychological distress.[35]
We found that Haitian Americans were more likely to report ‘good to excellent’ health as compared to African Americans (controlling for diabetes status, age and marital status); yet they also had higher perceived stress. This may be due to a difference in the perception of levels of health between the groups depending on differences in cultural, economic or social expectations of health as well as less access to healthcare.[36] African Americans did not have the same frame of reference for perceived health as compared to Haitian Americans since African Americans were not directly exposed to medical, social and health conditions in Haiti. Their findings suggest Haitian Americans in our sample may be overestimating their health as compared to African Americans.[36] The inflated estimation may be due to health disparities for Haitian Americans with respect to African Americans in our study population. Differences in respondent characteristics may have caused a reporting bias of SRH for our sample since Haitian Americans were more likely to report not having health care in the past year and less education than African Americans. Race was an explanatory factor of SRH (5-point Likert scale) for a sample combining two Detroit metropolitan multistage area probability surveys with 700 women.[37] The authors reported that African American women had a lower mean SRH than White women, controlling for age, education and income and that this effect was significant when unfair treatment and acute life events were added to the model.[37]
There have been few studies to date comparing type 2 diabetes status, ethnicity, SHR and perceived stress for minorities at risk for diabetes complications. Nonetheless, several limitations of our study should be considered. First, the relationships cannot be considered causal since the study design was based on associations from a single-point data set. Second, although the major outcome variables, perceived stress and SRH, were from validated questionnaires, the measurements are from self-report and may contain subject, interviewer and instrumental biases. In particular, participants may not be aware of or may be unwilling to report certain health behaviors. Third, the study sample was recruited from multiple-outreach methods rather than by randomized selection; therefore, the sample may not be representative of Haitian Americans and African Americans living in South Florida. In addition, this study scheme may leave out people who are unwilling to drive to the research site or may not perceive the benefits of participation. Bias may have been introduced comparing ethnicities since we recruited African Americans by both community methods and a mailing list and Haitian Americans by community methods. We were not able to recruit Haitian Americans with a purchased mailing list because no company had a database specifically for the Haitian American community. Perceived stress differences may have been confounded by perceived discrimination and other individual differences which could not be captured by a statistical model. Lastly, a potential limitation is the omission of other social factors that may have an effect on SRH and stress such as neighborhood differences of the study participants. It has been suggested that neighborhoods exert a contextual force whereby a combination of social exchanges, social norms and stress processes may influence health behavior and outcomes.[38] Our study did not investigate the effect of community on health. In fact, community type and level of involvement may have been a confounder in assessing ethnic differences between African Americans and Haitian Americans. A subject bias may have been introduced since African Americans were recruited with letters of invitation and by community outreach; whereas, Haitian Americans were recruited only through community methods.
The results of this study support our conceptual model and has clinical and research implications that apply to public health. First and foremost, the findings indicate the need for future research comparing ethnicities across gender and diabetes status for health outcomes. Added to the layer of the individual and their predisposition toward stress is the influence of normative roles of gender and culture. These influences may differ by ethnicity and are further shaped by lifestyle choices such as being in a marital relationship or choosing to use tobacco. For our participants, smoking, not being married, and having no health insurance explained part of the variance of perceived stress. The association of currently smoking and higher levels of perceived stress than not smoking for participants, regardless of ethnicity, gender, and diabetes status, may indicate that tobacco use was a coping strategy, albeit ineffective, by our sample. Further research, including qualitative studies, is needed to assess the relationship between perceived stress and tobacco use among Black populations. Contrary to several studies, we did not find an association between education and perceived stress; however, previous studies were performed primarily with White populations.[14,39]
Although psychosocial factors, such as perceived stress, may be triggered by socio-economic hardship the relationship may differ by other group memberships such as gender, ethnicity, or diabetes status. Gender modified the relationship of lower socio-economic status and mortality in a Hungarian population.[40] Perceived stress was related to mortality from heart disease for younger, healthier Danish men[41] and was reported to be higher for females and those with a lower perceived social status as compared to their counterparts for a South African adult population.[42] Gender differences in behavior and physiological response to social stressors have been supported by the literature; yet few studies examined these relationships across ethnicities and disease states.
In summary, we found ethnicity, gender, and diabetes status differed in SRH and perceived stress. Further studies in these populations, as well as with other ethnicities, are needed to confirm these results. Investigations into coping strategies may uncover intervention points for health improvement and diabetes prevention in African Americans and Haitian Americans. The findings suggest that screening for stress should be considered as part of a routine medical care, since the likelihood of reporting ‘poor or fair’ SRH was positively associated with perceived stress. In addition, the findings support treatment plans that are patient-centered and culturally relevant. Considering the association of perceived stress with mortality found in prospective studies, patients presenting stress symptoms or scoring high on perceived stress questionnaires might benefit from appropriate therapies and interventions.
ACKNOWLEDGMENTS
This study was funded by a grant to the first author from the National Institutes of Health: NIH/NIDDK no. ISC1DK083060-03.
Footnotes
Source of Support: National Institutes of Health: NIH/NIDDK no. ISC1DK083060-03
Conflict of Interest: None declared.
REFERENCES
- 1.Atlanta, GA: U.S. Department of Health and Human Services; 2011. [Last accessed on 2012 March 07]. Centers for Disease Control and Prevention. National diabetes fact sheet: General information and national estimates on diabetes and prediabetes in the United States, 2011. Available from: http://www.cdc.gov/diabetes/pubs/factsheet11.htm . [Google Scholar]
- 2.Karlsen B, Oftedal B, Bru E. The relationship between clinical indicators, coping styles, perceived support and diabetes-related distress among adults with type 2 diabetes. J Adv Nurs. 2012;68:391–401. doi: 10.1111/j.1365-2648.2011.05751.x. [DOI] [PubMed] [Google Scholar]
- 3.Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, et al. Assessing psychosocial distress in diabetes: Development of the Diabetes Distress Scale. Diabetes Care. 2005;28:626–31. doi: 10.2337/diacare.28.3.626. [DOI] [PubMed] [Google Scholar]
- 4.Polonsky WH, Anderson BJ, Lohrer PA, Welch G, Jacobson AM, Aponte JE, et al. Assessment of diabetes-related distress. Diabetes Care. 1995;18:754–60. doi: 10.2337/diacare.18.6.754. [DOI] [PubMed] [Google Scholar]
- 5.Young BA, Maynard C, Boyko EJ. Racial differences in diabetic nephropathy, cardiovascular disease, and mortality in a national population of veterans. Diabetes Care. 2003;26:2392–9. doi: 10.2337/diacare.26.8.2392. [DOI] [PubMed] [Google Scholar]
- 6.Geneva: World Health Organization; 2002. [Last accessed on 15 Sep 2012]. World Health Survey 2002: Individual questionnaire. Website: Available from: http://www.who.int/bulletin/en . [Google Scholar]
- 7.Sheldon C, Kaplan GA, Salonen JT. The role of psychological characteristics in the relation between socioeconomic status and perceived health. J Appl Soc Psychol. 1999;29:445–68. [Google Scholar]
- 8.Vadstrup ES, Frølich A, Perrild H, Borg E, Røder M. Health-related quality of life and self-related health in patients with type 2 diabetes: Effects of group-based rehabilitation versus individual counselling. [Last accessed on 15 Sep 2012];Health Qual Life Outcomes. 2011 9:110. doi: 10.1186/1477-7525-9-110. Available from: http://www.hqlo.com/content/9/1/110 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Salvo KB, Fan VS, McDonnell MB, Fihn SD. Predicting mortality and healthcare utilization with a single question. Health Serv Res. 2005;40:1234–46. doi: 10.1111/j.1475-6773.2005.00404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 11.Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. 2009;69:307–16. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 12.Tsai J, Ford ES, Li C, Zhao G, Balluz LS. Physical activity and optimal self-rated health of adults with and without diabetes. [Last accessed 14 Mar 2012];BMC Public Health. 2010 10:365. doi: 10.1186/1471-2458-10-365. [online journal]: Available from: http:/www.biomedcentral.com/1471-2458/10/365 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. J Behav Med. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Limm H, Angerer P, Heinmueller M, Marten-Mittag B, Nater UM, Gundel H. Self-perceived stress reactivity is an indicator of psychosocial impairment at the workplace. BMC Public Health. 2010;10:252. doi: 10.1186/1471-2458-10-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glanz K, Rimer BK, Lewis FM. 3rd ed. San Francisco: Jossey-Bass; 2002. Health Behavior and Health Education; p. 583. [Google Scholar]
- 16.Bronfenbrenner U. Cambridge, MA: Harvard University Press; 1979. The Ecology of Human Development: Experiments by Nature and Design; p. 330. [Google Scholar]
- 17.Sallis J, Owen N, Fisher E. Ecological Models of Health Behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. 4th ed. United States: Jossey-Bass; 2008. pp. 465–82. [Google Scholar]
- 18.Fisher EB, Brownson CA, O’Toole ML, Shetty G, Anwuri VV, Glasgow RE. Ecological approaches to self-management: The case of diabetes. Am J Public Health. 2005;95:1523–35. doi: 10.2105/AJPH.2005.066084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Diabetes Association Standards of medical care in diabetes-2011. Diabetes Care. 2011;34:S11–61. doi: 10.2337/dc11-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Breidablik HJ, Meland E, Lydersen S. Self-rated health in adolescence: A multifactorial composite. Scand J Public Health. 2008;36:12–20. doi: 10.1177/1403494807085306. [DOI] [PubMed] [Google Scholar]
- 21.Manor O, Matthews S, Power C. Dichotomous or Categorical Response? Analyzing self-rated health and lifetime social class. Int J Epidemiol. 2000;29:149–57. doi: 10.1093/ije/29.1.149. [DOI] [PubMed] [Google Scholar]
- 22.Strully KW. Job Loss and Health in the U.S. Labor Market. Demography. 2009;46:221–46. doi: 10.1353/dem.0.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 24.Cohen S, Williamson G. Perceived stress in a probability sample of the U.S. In: Spacapam S, Oskamp S, editors. The social psychology of health: Claremont Symposium on Applied Social Psychology. California: Newbury Park CA: Sage; 1988. pp. 99–125. [Google Scholar]
- 25.Callaway CW, Chumlea WC, Bouchard C. Circumferences. In: Lohman TG, Roche AF, Marorell R, editors. Anthropometric standardization reference manual. Campaign, IL, USA: Human Kinetics Books; 1988. pp. 28–80. [Google Scholar]
- 26.Keys A, Fidanza F, Karvonen MJ, Kiura N, Taylor HL. Indices of relative weight and obesity. J Chronic Dis. 1972;25:329–43. doi: 10.1016/0021-9681(72)90027-6. [DOI] [PubMed] [Google Scholar]
- 27.Hosmer DW, Lemeshow S. New York: John Wiley and Sons; 2000. Applied Logistic Regression; p. 95. [Google Scholar]
- 28.U.S. Census Bureau The population with Haitian ancestry in the United States: 2009. US Department of Commerce. Economics and statistics administration. [Last accessed on 2012 Mar 12]. Available from: http://www.census.gov/prod/2010pubs/acsbr09-18.pdf .
- 29.Nielsen NR, Kristensen TS, Prescott E, Larsen KS, Schnohr P, Gronbaek M. Perceived stress and risk of ischemic heart disease: Causation or bias? Epidemiol. 2006;17:391–7. doi: 10.1097/01.ede.0000220556.86419.76. [DOI] [PubMed] [Google Scholar]
- 30.Rod NH, Gronbaek M, Schnohr P, Prescott E, Kristensen TS. Perceived stress as a risk factor for changes in health behavior and cardiac risk profile: A longitudinal study. J Inter Med. 2009;266:467–75. doi: 10.1111/j.1365-2796.2009.02124.x. [DOI] [PubMed] [Google Scholar]
- 31.Theorell T, Kristensen TS, Kornitzer M, Marmot M, Orth-Gomer K, Steptoe A. Brussels, Belgium: European Heart Network; 2006. Stress and Cardiovascular Disease 2006; p. 35. [Google Scholar]
- 32.Ranjit N, Diez-Roux AV, Shea S, Cushman M, Seeman T, Jackson SA, et al. Psychosocial factors and inflammation in the multi-ethnic study of atherosclerosis. Arch Intern Med. 2007;167:174–81. doi: 10.1001/archinte.167.2.174. [DOI] [PubMed] [Google Scholar]
- 33.Forthofer MS, Janz NK, Dodge JA, Clark NM. Gender differences in the associations of self esteem, stress and social support with functional health status among older adults with heart disease. J Women Aging. 2001;13:19–37. doi: 10.1300/J074v13n01_03. [DOI] [PubMed] [Google Scholar]
- 34.Greer TM, Laseter A, Asiamah D. Gender as a moderator of the relation between race-related stress and mental health symptoms for African Americans. Psychol Women Q. 2009;33:295–307. [Google Scholar]
- 35.Williams DR, Gonzalex HM, Williams S, Mohammed SA, Moomal H, Stein DJ. Perceived discrimination, race and health in South Africa. Soc Sci Med. 2008;67:441–52. doi: 10.1016/j.socscimed.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Charasse-Pouele CC, Fournier M. Health disparities between racial groups in South Africa: A decomposition analysis. Soc Sci Med. 2006;62:2897–914. doi: 10.1016/j.socscimed.2005.11.020. [DOI] [PubMed] [Google Scholar]
- 37.Schulz A, Israel B, Williams D, Parker E, Becker A, James S. Social inequalities, stressors and self reported health status among African American and white women in Detroit metropolitan area. Soc Sci Med. 2000;51:1639–53. doi: 10.1016/s0277-9536(00)00084-8. [DOI] [PubMed] [Google Scholar]
- 38.Stimpson JP, Ju H, Raji MA, Eschbach K. Neighborhood deprivation and health risk behaviors in NHANES III. Am J Health Behav. 2007;31:215–22. doi: 10.5555/ajhb.2007.31.2.215. [DOI] [PubMed] [Google Scholar]
- 39.Nielsen L, Curtis T, Kristensen TS, Nielsen NR. What characterizes persons with high levels of perceived stress in Denmark? A national representative study. Scand J Public Health. 2008;36:369–79. doi: 10.1177/1403494807088456. [DOI] [PubMed] [Google Scholar]
- 40.Kopp M, Skrabski Á, László K, Janszky I. Gender patterns of Socioeconomic differences in premature mortality: Follow-up of The Hungarian Epidemiological Panel. Int J Behav Med. 2011;18:22–34. doi: 10.1007/s12529-010-9126-5. [DOI] [PubMed] [Google Scholar]
- 41.Nielsen NR, Kristensen TS, Schnohr P, Gronbaek M. Perceived stress and cause-specific mortality among men and women: Results from a prospective cohort study. Am J Epidemiol. 2008;168:481–91. doi: 10.1093/aje/kwn157. [DOI] [PubMed] [Google Scholar]
- 42.Hamad R, Fernald LC, Karlan DS, Zinman J. Social and economic correlates of depressive symptoms and perceived stress in South African adults. Epidemiol Community Health. 2008;62:538–44. doi: 10.1136/jech.2007.066191. [DOI] [PubMed] [Google Scholar]


