Abstract
Background:
In some studies, the level of adenosine deaminase (ADA) in sputum and effusion liquids was used for the diagnosis of tuberculosis (TB). But it is not always possible to access these materials. The goal of this study is to assess the diagnostic value of serum ADA levels in pulmonary TB patients.
Materials and Methods:
In this study, 40 sputum smear-positive TB patients who were hospitalized and 40 non-TB patients who referred for surgeries were selected. A serum sample was collected and serum ADA level was measured by ADA kit.
Results:
The average (SD) of serum ADA in TB and non-TB patients were 20.88 (±5.97) and 10.69 (±2.98) U/L, respectively (P value < 0.05). The best cut-off point was 14 U/L. The calculated area under the receiver operating characteristic (ROC) curve was 0.955 (95% CI, 0.914-0.995); sensitivity was 92.7% (95% CI, 84.7-100) and specificity was 88.1% (95% CI, 78.3-97.8) (P < 0.001).
Conclusion:
Serum ADA level may be proposed as a proper index for TB diagnosis.
Keywords: Adenosine deaminase, diagnosis, tuberculosis
INTRODUCTION
Tuberculosis (TB) is one of the main reasons of mortality and morbidity globally and it kills about two million people annually.[1,2] Recent studies showed extensive delay in TB diagnosis.[3,4] There are different diagnostic methods but they have some drawbacks. To prepare mycobacterium culture, which is the golden standard for TB diagnosis, it may take 8 weeks. Finding acid-fast bacilli is the quick screening method for pulmonary TB diagnosis; nevertheless, its sensitivity is low. The polymerase chain reaction (PCR) test for TB diagnosis is expensive and it requires skilled personnel and lot of equipments. Therefore, in recent years, there has been a great demand for finding new microbiological, genetic, immunological, and biomedical diagnostic methods to diagnosis TB quickly and accurately. Measuring of adenosine deaminase (ADA) activity is a biomedical method.[5,6] ADA is an enzyme which contributes in purin metabolism.[7] ADA is essential for proliferation and differentiation of lymphoid cells, especially T cells, and helps in the maturation of monocytes to macrophages. It seems ADA is an index for cellular immunity[5] and previous studies have proved its value in TB diagnosis, even for assessing TB effusions.[8,9] Activity of this enzyme increases in TB patients.[9] In some studies, the level of ADA in sputum and serum was used for diagnosis of TB, and it was monitored during TB treatment.[10,11,12] However, previous studies used effusion fluids and a very limited number of studies used patients’ serum.[5,6,7,8,9,10,12] It is not always possible to access effusion liquids everywhere in pulmonary and extra-pulmonary TB; therefore, it would be helpful to take advantage of serum levels. The goal of this study is to assess the diagnostic value and cut-off point of serum ADA levels in pulmonary TB patients.
MATERIALS AND METHODS
It was a cross-sectional study (2011), which is conducted in Tohid Hospital (University Referral Hospital) in Sanandaj in Iran. In our study, case group included 40 sputum smear-positive TB patients who were admitted in infectious disease ward of the hospital. Inclusion criteria for TB patients were: “Having 2 or 3 sputum positive smears,” or “one sputum positive smear and one positive sputum culture,” or “one positive TB microbe smear sputum and suspected chest radiography.”[13]
In addition, 40 non-TB patients, referred to Tohid Hospital in Sannandaj for surgeries, were selected as the control group. Inclusion criteria for control group were: Not having any TB patient in their family, not having history of close contact with TB patients, not having any infectious disease (according to the interview and their records), not having fever or any symptom of illness or of being toxic, normal cell blood count, and normal chest radiography.
After diagnosis of TB (before initiation of treatment), blood samples and patients’ approval of consent form (research project number: 1387/87) were taken from TB group (at 7 AM). Then samples were centrifuged and serum ADA levels were measured by ADA kit manufactured by Diazyme Laboratories Company. In the first step, adenosine was affected by ADA and it becomes de-ammonized and shifted to inosine and then ammoniac was released. In the second reaction, because of glometat, released NH3 had become dehydrogenized and when it got close to allosteric activators, it combined with Nicotinamide adenine dinucleotide phosphate Hydrogen (NADPH) and released Nicotinamide adenine dinucleotide phosphate (NADP). Consequently, there was a direct relationship between activity (density) of ADA enzyme and speed reduction of radiation absorption in 340 nanometer wavelength (as NADPH changed to NADP+); it was measured by Diazyme Adenosine Deaminase Assay Kitt (Diazyme Laboratory; USA). Then, data were analyzed using Statistical Package for the Social Sciences (SPSS) 11.5 (Chicago, USA) software and ROC curve was plotted. In addition, sensitivity, specificity, and confidence interval of 95% were calculated.
RESULTS
From all 40 TB patients who participated in this study, 16 were males and 24 were females. From 42 participants in control group, 22 were males and 20 were females. The most common age group for TB patients was 50s and for control group, it was 40s. Age average was 59 (±13.5) in TB patients and it was 49 (±15.6) for non-TB patients. The average of serum ADA in TB patients group and control group was 20.88 (±5.97) and 10.69 (±2.98), respectively. The best cut-off point was 14 U/L in which sensitivity and specificity were 92.7% (95% CI, 84.7-100) and 88.1% (95% CI, 78.3-97.8), respectively. The positive and negative predicative values were 88.4% (95% CI, 75-95.1) and 92.5% (95% CI, 79.6-98.4), respectively [Figure 1]. The calculated area under the ROC curve was 0.955 (95% CI, 0.914-0.995) (P < 0.001).
Figure 1.
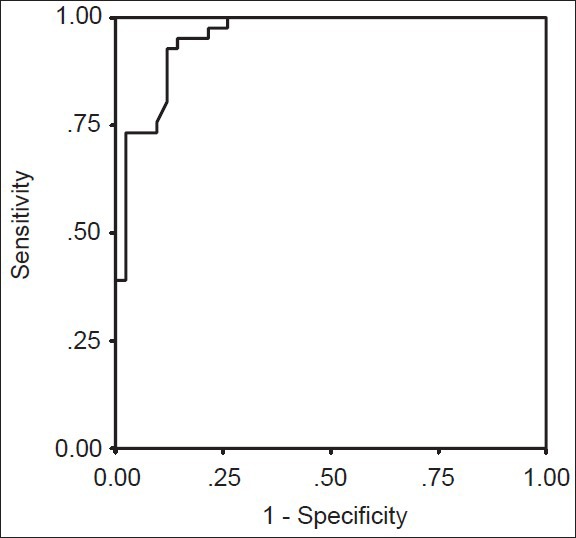
Receiver operating characteristic curve for serum adenosine deaminase in tuberculosis diagnosis. Area under curve was 0.955
DISCUSSION
In this study, serum ADA level was an appropriate index for diagnosing smear-positive TB. High sensitivity and specificity were observed in serum level of 14 U/L. Therefore, serum ADA could be also used for diagnosis of pulmonary TB. Moreover, in this study, all TB patients had a serum level of more than 22.5 U/L. Hence, for suspicious cases of TB, increased levels of ADA could facilitate diagnosis.
Diagnostic value of serum ADA in pulmonary TB has been assessed only in few numbers of studies. Pairs et al.[7] reported an increase in ADA level in TB pleural effusion; other studies have also confirmed such an increase in TB pericardial effusions, peritoneum, and central nervous system (CNS).[11,14,15] The main reason for the increased ADA levels in pleural effusion is the movement of T lymphocytes toward this area. Increase in ADA level is the result of a tropical inflammatory reaction caused by monocytes and macrophages.[11,16] When alveolar macrophages are infected by mycobacterium, this enzyme could be found in serum during active pulmonary disease. When TB infection is controlled, growth-markers of lymphocytes decrease; leucocytes will decrease in serum ADA levels concurrent with the decrease in lymphocytes. Because of this, serum ADA level could be utilized as a treatment response index.[10,11,12]
In Agarwal et al.'s study,[17] ADA level was 15.3 (±0.23) in healthy people, 19 (±0.68) in non-pulmonary TB cases, and 38.48 (±1.56) in pulmonary TB patients. In Jhamaria et al.'s study,[6] the average of serum ADA level was 19.9 U/L (±2.99) in control group, 43.95 U/L (±2.48) in sputum smear-positive people with typical or progressive disease, and 42.09 U/L (±1.46) and 40.02 U/L (±2.58) in negative sputum patients with mild or typical disease. In their study, in the cut-off point of 33 U/L, sensitivity and specificity were 98% and 100%, respectively. It seems that as the disease progresses, ADA levels increase; this subject was not considered in our study. In another study with an ADA level of 26.2 U/L, sensitivity, specificity, and positive predictive value were 95%, 83.3%, and 79.2%, respectively.[18]
In Gupta et al.'s study,[19] sensitivity, specificity, positive predictive value, and negative predictive value were 92.8%, 90%, 92.8%, and 90%, respectively, for diagnosis of TB in pleural effusion with an ADA level of more than 40. In Conde et al.'s study,[20] ADA level of 14 U/L was chosen as cut-off point. Stevanovic et al.[12] assessed serums of extra-pulmonary TB patients and in a cut-off point of 24, sensitivity and specificity were 94.3% and 92.2%, respectively; in their study, serum ADA level decreased as treatment started. In Dilmac et al.'s study,[21] serum ADA level in pulmonary TB patients was reported as 27.5 (±11) and it was 23.9 (±24) in Chronic Obstructive Pulmonary Disease (COPD) patients. In Rasolinejad's study,[22] serum ADA level was 21.51 in pulmonary TB patients and 11.47 in healthy people; in cut-off point of 14.5 U/L, sensitivity and specificity were 82% and 80.6%, respectively. In Lakshmi et al.'s study,[23] average ADA level was 13.3 U/L in negative smear and negative tuberculin patients, 33.52 (±15.22) in smear-positive and purified protein derivative (PPD) positive patients, and 16.5 (±3.18) in volunteer healthy people. Such differences may be due to TB severity, age groups, genetic differences, and dissimilarities in control groups. Therefore, further studies for identifying normal ADA levels in different societies may be useful.
Fortunately, in some autoimmune patients like rheumatoid arthritis, synovial ADA level is normal and it is similar to control group.[24] Thus, in autoimmune diseases that involve lung, ADA level could be used for TB differentiation. In some studies, ADA2 was also considered a useful tool for diagnosis;[16] it needs further studies.
CONCLUSIONS
According to this study, serum ADA level is proposed as a proper index for TB diagnosis; in a cut-off point of 14, its sensitivity and specificity are calculated as 92.7% and 88.1%, respectively.
ACKNOWLEDGMENTS
This study was financially supported by vice chancellor for research affairs, Kurdistan University of Medical Sciences (through M.D thesis belongs to Dr. Kaveh Aftabi). We thank Mr. Fardin Garibi and Dr. Ebrahim Ghaderi for their consultants in statistical analysis and paper preparation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Raviglione MC, Snider DE, Jr, Kochi A. Global epidemiology of tuberculosis. Morbidity and mortality of a worldwide epidemic. JAMA. 1995;273:220–6. [PubMed] [Google Scholar]
- 2.Global Tuberculosis Control: WHO Report 2010. Geneva: World Health Organization; 2010. World Health Organization. The global burden of TB; p. 7. [Google Scholar]
- 3.World Health Organization. Diagnostic and Treatment Delay in Tuberculosis. World Health Organization, Regional Office for the Eastern Mediterranean. 2006:21. [Google Scholar]
- 4.Storla DG, Yimer S, Bjune GA. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC Public Health. 2008;8:15. doi: 10.1186/1471-2458-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuyucu N, Karakurt C, Bilaloğlu E, Karacan C, Teziç T. Adenosine deaminase in childhood pulmonary tuberculosis: Diagnostic value in serum. J Trop Pediatr. 1999;45:245–7. doi: 10.1093/tropej/45.4.245. [DOI] [PubMed] [Google Scholar]
- 6.Jhamaria JP, Jenaw RK, Luh SK, Mathur DK, Parihar HL, Sharma SK. Serum adenosine deaminase (ADA) in differential diagnosis of pulmonary tuberculosis and common non tubercular respiratory diseases. Ind J Tub. 1988;35:25–7. [Google Scholar]
- 7.Piras MA, Gakis C, Budroni M, Andreoni G. Adenosine deaminase activity in pleural effusions: An aid to differential diagnosis. Br Med J. 1978;2:1751–2. doi: 10.1136/bmj.2.6154.1751-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garcia-Zamalloa A, Taboada-Gomez J. Diagnostic accuracy of adenosine deaminase and lymphocyte proportion in pleural fluid for tuberculous pleurisy in different prevalence scenarios. PLoS One. 2012;7:e38729. doi: 10.1371/journal.pone.0038729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sakuraba M, Masuda K, Hebisawa A, Sagara Y, Komatsu H. Pleural effusion adenosine deaminase (ADA) level and occult tuberculous pleurisy. Ann Thorac Cardiovasc Surg. 2009;15:294–6. [PubMed] [Google Scholar]
- 10.Collazos J, España P, Mayo J, Martínez E, Izquierdo F. Sequential evaluation of serum adenosine deaminase in patients treated for tuberculosis. Chest. 1998;114:432–5. doi: 10.1378/chest.114.2.432. [DOI] [PubMed] [Google Scholar]
- 11.Çimen F, Çiftçi TU, Berktafl BM, Sipit T, Hoca NT, Dulkar G. The relationship between serum adenosine deaminase level in lung tuberculosis along with drug resistance and the category of tuberculosis. Turk Respir J. 2008;9:20–3. [Google Scholar]
- 12.Stevanovic G, Pelemis M, Pavlovic M, Lavadinovic L, Dakic Z, Milosevic I, et al. Significance of adenosine deaminase serum concentration in the diagnosis of extra-pulmonary tuberculosis. J IMAB. 2011;17:130–4. [Google Scholar]
- 13.Treatment of Tuberculosis: Guidelines. 4th ed. Geneva: World Health Organization; 2010. World Health Organization. Case definitions; pp. 24–6. WHO/HTM/TB/2009.420. [Google Scholar]
- 14.Saleh MA, Hammad E, Ramadan MM, Abd El-Rahman A, Enein AF. Use of adenosine deaminase measurements and QuantiFERON in the rapid diagnosis of tuberculous peritonitis. J Med Microbiol. 2012;61:514–9. doi: 10.1099/jmm.0.035121-0. [DOI] [PubMed] [Google Scholar]
- 15.Tuon FF, Silva VI, Almeida GM, Antonangelo L, Ho YL. The usefulness of adenosine deaminase in the diagnosis of tuberculous pericarditis. Rev Inst Med Trop Sao Paulo. 2007;49:165–70. doi: 10.1590/s0036-46652007000300006. [DOI] [PubMed] [Google Scholar]
- 16.Mohammadtaheri Z, Mashayekhpour S, Mohammadi F, Mansoori D, Masjedi MR. Diagnostic value of adenosine deaminase isoenzyme (ADA2) and total ADA in tuberculous pleural effusion. Tanaffos. 2005;4:37–42. [Google Scholar]
- 17.Agarwal MKN, Mukerji PK, Srivastava VML. A study of serum adenosine deaminase activity in sputum negative patients of pulmonary tuberculosis. Ind L Tub. 1991;38:139. [Google Scholar]
- 18.Hassanein K, Hosny H, Mohamed R, Abd El-Moneim W. Role of adenosine deaminase (ADA) in the diagnosis of pulmonary tuberculosis. Egypt J Bronchol. 2010;4:11–8. [Google Scholar]
- 19.Gupta BK, Bharat V, Bandyopadhyay D. Sensitivity, specificity, negative and positive predictive values of adenosine deaminase in patients of tubercular and non-tubercular serosal effusion in India. J Clin Med Res. 2010;2:121–6. doi: 10.4021/jocmr2010.05.289w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Conde MB, Marinho SR, Pereira Mde F, Lapa e Silva JR, Saad MH, Sales CL, et al. The usefulness of serum adenosine deaminase 2 (ADA2) activity in adults for the diagnosis of pulmonary tuberculosis. Respir Med. 2002;96:607–10. doi: 10.1053/rmed.2001.1273. [DOI] [PubMed] [Google Scholar]
- 21.Dilmaç A, Uçoluk GO, Uğurman F, Gözü A, Akkalyoncu B, Eryilmaz T, et al. The diagnostic value of adenosine deaminase activity in sputum in pulmonary tuberculosis. Respir Med. 2002;96:632–4. doi: 10.1053/rmed.2002.1321. [DOI] [PubMed] [Google Scholar]
- 22.Rasooli Nejad M. The value of serum adenozine deaminase in diagnosis of pulmonary tuberculosis. Iran J Infect Dis. 2003;8:15–9. [Google Scholar]
- 23.Lakshmi V, Rao RR, Joshi N, Rao PN. Serum adenosine deaminase activity in bacillary or paucibacillary pulmonary tuberculosis. Indian J Pathol Microbiol. 1992;35:48–52. [PubMed] [Google Scholar]
- 24.Yuksel H, Akoğlu TF. Serum and synovial fluid adenosine deaminase activity in patients with rheumatoid arthritis, osteoarthritis, and reactive arthritis. Ann Rheum Dis. 1988;47:492–5. doi: 10.1136/ard.47.6.492. [DOI] [PMC free article] [PubMed] [Google Scholar]


