Abstract
Background:
The most fundamental way to decrease the burden of noncommunicable diseases (NCDs) is to identify and control their related risk factors. The goal of this study is to determine socioeconomic inequalities in risk factors for NCDs using concentration index based on Non-Communicable Disease Surveillance Survey (NCDSS) data in Kurdistan province, Islamic Republic of Iran in 2005 and 2009.
Methods:
The required data for this study are taken from two NCDSSs in Kurdistan province in 2005 and 2009. A total of 2,494 persons in 2005 and 997 persons in 2009 were assessed. Concentration index was used to determine socioeconomic inequality. To assess the relationship between the prevalence of each risk factor and socioeconomic status (SES), logistic regression was used and odds ratio (OR) was calculated for each group, compared with the poorest group.
Results:
The concentration index for hypertension was -0.095 (-0.158, -0.032) in 2005 and -0.080 (-0.156, -0.003) in 2009. The concentration index for insufficient consumption of fruits and vegetables was -0.117 (-0.153, -0.082) in 2005 and -0.100 (-0.153, -0.082) in 2009. The concentration index for the consumption of unhealthy fat and oil was -0.034 (-0.049, -0.019) in 2005 and -0.108 (-0.165, -0.051) in 2009. The concentration index for insufficient consumption of fish was -0.070 (-0.096, -0.044) in 2005. The concentration index for physical inactivity was 0.008 (-0.057, 0.075) in 2005 and 0.139 (0.063, 0.215) in 2009. In all the cases, the OR of the richest group to the poorest group was significant.
Conclusion:
Hypertension, insufficient consumption of fruits and vegetables, consumption of unhealthy fat and oil, and insufficient consumption of fish are more prevalent among poor groups. There was no significant socioeconomic inequality in the distribution of smoking, excess weight, and hypercholesterolemia. Physical inactivity was more prevalent among the rich groups of society in 2009. The reduction of socioeconomic inequalities must become a main goal in health-care policies.
Keywords: Concentration index, inequality, Iran, non communicable diseases, socioeconomic status
INTRODUCTION
Nowadays, noncommunicable diseases (NCDs) are the most common causes of mortality in developing and developed countries. In 2008, more than 33 million out of 57 million cases of mortality all over the world, that is, 67% were caused by these diseases.[1,2] It is estimated that eight out of 10 main causes of mortality globally will have been caused by noncommunicable and chronic diseases by 2030.[3] The burden of such diseases in low- and middle-income countries is rapidly increasing.[4] It is estimated that 70% of all deaths will have been caused because of NCDs by 2030 from which more than 80% will have been happened in low- and middle-income countries.[5]
The behavioral and metabolic risk factors are the causes of NCDs. The main risk factors include smoking, hypertension, unhealthy diet, physical inactivity, excess weight and obesity, hypercholesterolemia, diabetes and high blood sugar, and the consumption of alcohol. It is estimated that smoking kills more than six million people annually. Excess weight provides a base for stroke, diabetes, and cancer.[6] Physical inactivity is the cause of 7% of the disease burden in developed countries[7] and hypertension is the cause of 13 % of mortality cases globally.[8] Avoiding an unhealthy diet, having sufficient physical activity, and not smoking can prevent 80% of the heart diseases, cerebral stroke, and type 2 diabetes, and 40% of cancers.[1,9] Consumption of fish and physical activity can reduce the risk of NCDs significantly.[6]
Like other developing countries, the burden of NCDs is rapidly increasing in Iran. Because of rapid demographic changes in Iran, these diseases which caused 27% of the mortalities in 1981, resulted in 47% of the mortalities in 1995.[10] Metabolic risk factors like excess weight, high blood pressure, and high fasting blood sugar are among the main causes of mortality in Iran.[11]
Because of epidemiological transition effect and increase of the burden of NCDs, more attention has been paid to these diseases. Therefore, Iran and many other countries have special surveillance system for the risk factors for NCDs. These systems identify and monitor the risk factors. Although experts and the World Health organization (WHO) have emphasized the importance of measuring socioeconomic inequalities related to health-care outcomes for more than a decade, many countries all over the world do not follow these instructions.[12]
Therefore, health-care equity has become an important issue and much attention has been paid to the determination of socioeconomic inequalities in health-care outcomes.[13] Determination of socioeconomic inequalities is a crucial concern and it can be used as a tool for assessing some aspects of health-care policies.[14] All members of the society within different socioeconomic groups must be able to access health-care services. Being in a unique socioeconomic group must not prevent people from accessing health-care services.[15] Nowadays, setting equity in health care is accepted as a moral and human right and it has been mentioned in the health-care goals of many countries.[14,16]
A lot of attention has been paid to general equality as well as health-care equity in the current major national programs of Iran. Based on a national five-year program, the number of poor and socioeconomic inequalities ought to be reduced.[17] Such insights have affected Iranian researchers and consequently many studies about inequalities in health care have been conducted in Iran.[15,16,17,18,19,20]
Although there has been a lot of emphasis on measuring inequalities in risk factors for NCDs, there is little information about these inequalities in the various socioeconomic status (SES) groups. The methods of interpretation and explanation of inequality for the risk factors for NCDs is different from other health-care outcomes. As these risk factors are greatly dynamic in their distribution among different socioeconomic groups within societies, their distribution patterns are rapidly changing and they are assuming different patterns within different societies.[12] Although NCDs have a high burden in Iran, to the best of our knowledge, no study has been conducted yet to measure socioeconomic inequalities in risk factors for NCDs in the country. The goal of this study is to determine socioeconomic inequalities in risk factors for NCDs using concentration index based on the Non-Communicable Disease Surveillance Survey (NCDSS) data in Kurdistan in 2005 and 2009.
METHODS
The main data used in this study was taken from the 2005 and 2009 NCDSSs conducted in Kurdistan province. In the survey conducted in 2009, a questionnaire for measuring the SES of participants was added by researchers of this study. The methodology and details of the NCDSSs are described elsewhere.[21,22]
NCDSS was conducted based on the WHO STEPS program (The WHO STEPwise approach to Surveillance) for risk factors for NCDs in Iran since 2005. Through this approach, risk factors for NCDs are investigated in different steps. In this approach, a questionnaire is used in the first step, physical measures are used in the second step, and finally using blood samples, biomedical measures are used as the third step of investigation.[23] The data collected in 2005 included the measures of all three steps; however, the data collected in 2009 included only the results of the first two steps and did not include biomedical measures of blood samples.
The study population included all 15- to 64-year-old residents of Kurdistan province in 2005 and 2009. The sampling method was stratified probability cluster sampling through household family members. The postal codes which are updated annually were chosen as the sampling frame. A sample size of 2,500 people aged between 15 and 64 years were chosen and classified in 125 clusters in 2005, and for the study conducted in 2009, a sample size of 1,000 people in the same age group were classified in 50 clusters. Each cluster included 20 people divided in five age groups, and each age group covered an age range of 10 years comprising both sexes, two persons from each sex. Following existing protocols, their height, weight, and waist size were measured by means of standard tools. The members of the research team were trained before starting their assessments. They contacted households the day before the visit to provide information about the time and conditions of visit. The variables used in this study were defined as follows:
Hypertension was defined as a systolic blood pressure of 140 mmHg or higher or a diastolic blood pressure of 90 mmHg or higher. In addition, people under any kind of treatment for hypertension were included. Those who smoking any kind of cigarette currently, called current smokers, were included in the smoking group. Excess weight was defined as a body mass index of 25 kg/m2 or more. Based on the 2009 definition, physically inactivity was defined as a low level of activity, that is, less than 150 minutes of normal physical activity per week or less than 60 minutes of intense activity per week at home, at work, during leisure, or during outdoor activities and travel. Based on the 2005 definition, physical inactivity was defined as a low level of activity, that is, no or low level of physical activity at home, at work, during leisure, or during outdoor activities and travel. For unhealthy diet, three measures were defined. Insufficient consumption of fruits and vegetables: Less than four day servings of fruits and vegetables per week. Insufficient consumption of fish: Less than one serving of fish per week. Consumption of unhealthy fat and oil: Common use of any one of the saturated oils including the following fats or oils for cooking foods (solid oil, fat or animal oil, suet). Hypercholesterolemia: Blood cholesterol 200 or higher.
To determine SES in the 2005 survey, the following parameters were assessed: The condition of living place, type of home owned, number of persons per room, car ownership, any record of travel in recent years, and educational and occupational status. In the data collected in 2009, SES was determined based on assets and conditions of the living place. In this period, it was possible to add an extra questionnaire, and therefore, the following assets and living conditions were considered to determine the SES of the people. The assets and other items included having a separate bathroom, separate kitchen, vacuum cleaner, computer, refrigerator, washing machine, colored television, liquid-crystal display (LCD) television, cell phones, furniture, dish washer, microwave oven, internet access, personal car, phone line, home ownership, condition of living place, number of rooms, heating equipment, and gas stove. Using the principal component analysis (PCA), these assets and conditions of living place and other items were used to calculate wealth indexes and then to classify the socioeconomic groups.[24,25,26]
The first principal component formed the wealth index for households, and 18% of the variability in 2005 and 20% of the variability in 2009 was caused by this component. This index was put into five household quintiles. The concentration index was used to measure socioeconomic inequalities. It can be computed as twice the (weighted) covariance of the health variable and a person's relative rank in terms of economic status, divided by the variable mean. The concentration index value can vary between -1 and 1. The negative value represents the concentration of variables among the disadvantaged people, and the positive value shows the opposite. The concentration index is zero in case of no inequality. Inequality is shown by a concentration curve. Concentration index and curve have been used largely in the last decade to determine health-care inequalities; the details are described fully in various studies.[17,27,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30]
Logistic regression was used for investigating relation of risk factors among different SES groups. Odds ratio (OR) of each quintile was based on the first quintile. The stratification and sampling weights as well as household clustering effects were used for analysis.
RESULTS
In 2005, a total of 2,494 people participated in the study and the response rate was 99.8%, whereas in 2009, a total of 997 people were involved in the study and the response rate was 99.7%. The mean age of the participants of the study conducted in 2005 was 39.08 years (SD=14.37), and in 2009 it was 39.77 years (SD=14.24).
Based on PCA results, in 2005, a total of 2,491 people were divided into five socioeconomic quintiles. From all, 758 people (30.43%) were included in the first quintile or the poorest group, 489 people (19.63%) in the second quintile or poor group, 455 people (18.27%) in the third quintile, 379 people (15.21%) in the fourth quintile or rich group, and 410 people (16.46%) in the fifth quintile or the richest group. In addition, based on PCA results, in 2009, a total of 963 people were divided into five socioeconomic quintiles. From all, 224 people (23.26%) were included in the first quintile, 186 people (19.31%) in the second quintile, 183 people (19%) in the third quintile, 186 people (19.31%) in the fourth quintile, and 184 people (19.11%) in the fifth quintile.
Table 1 presents the prevalence of risk factors for NCDs in 2005 and 2009 among Kurdistan residents aged 15 to 64 years. The prevalence shown in Table 1 are weighted percentage of risk factors. Based on the results presented in this table, the prevalence of risk factors of hypertension, smoking, excess weight, and consumption of unhealthy fat and oil had decreased during this time period. However, the prevalence of risk factors of insufficient consumption of fish, insufficient consumption of fruits and vegetables, and physical inactivity had increased. The prevalence of hypercholesterolemia was 38.5% in 2005, whereas it had not been measured in 2009.
Table 1.
Prevalence of risk factors for NCDs in 2005 and 2009 in Kurdistan
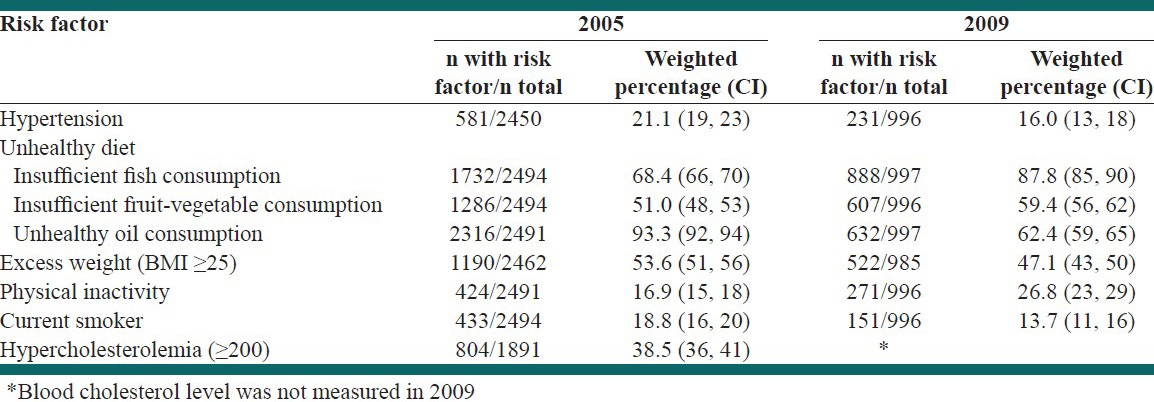
Table 2 presents the distribution of risk factors for NCDs among socioeconomic groups. This table contains the OR for risk factors among different socioeconomic groups in 2005 and 2009. The first quintile involves the poorest group and the fifth quintile involves the richest group. To calculate OR, the first quintile in the table was considered as the base group and the ORs for other groups were calculated by comparing them with the first group.
Table 2.
Distribution of risk factors for NCDs among SES groups in 2005 and 2009 in Kurdistan
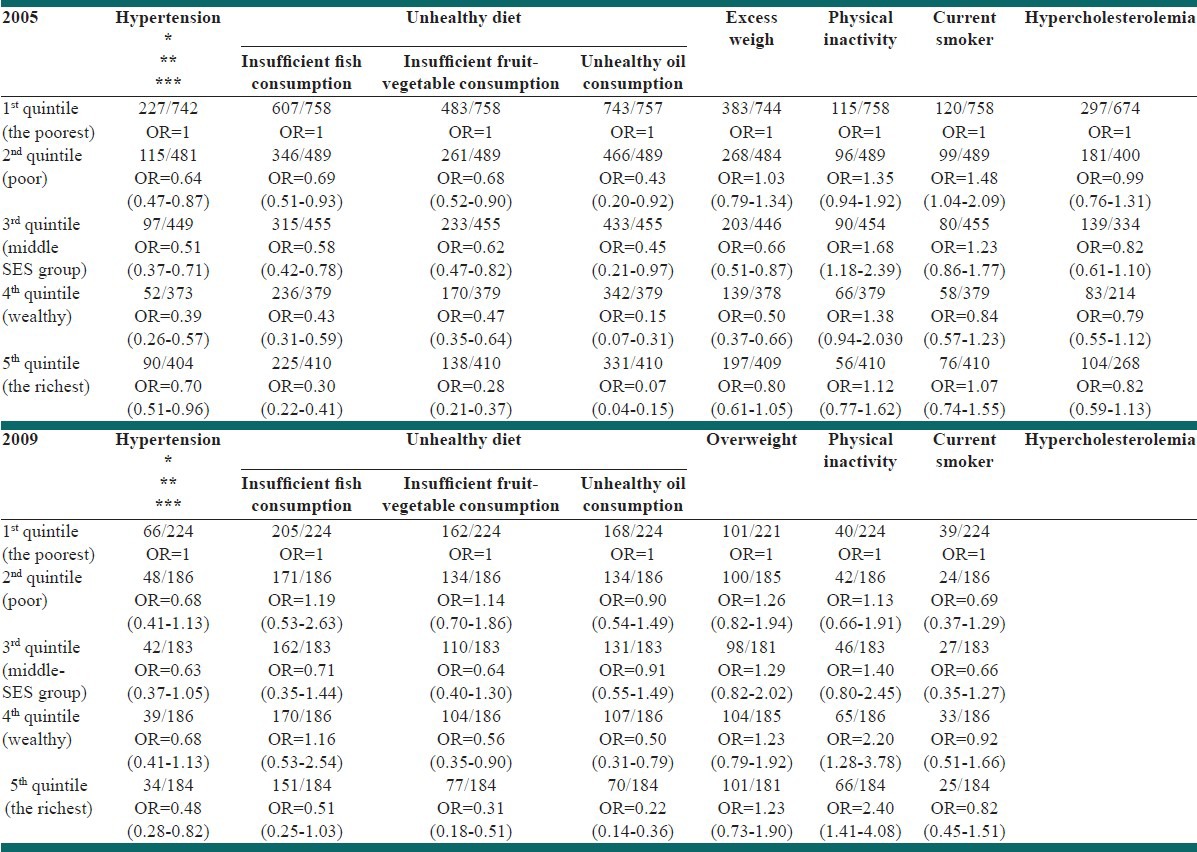
As rank of the quintiles increased, hypertension OR decreased in both 2005 and 2009. The OR for the richest group compared with the poorest group was 0.70 (0.96, 0.51) in 2005; it was 0.48 (0.28, 0.82) in 2009. As rank of the quintiles increased, the OR of insufficient consumption of fruits and vegetables, OR of insufficient consumption of fish, and OR of consumption of unhealthy fat and oil decreased in 2005. The same results were found regarding consumption of insufficient fruits and vegetables and unhealthy oil in 2009. The OR of insufficient consumption of fruits and vegetables for the richest group compared with the poorest group was 0.28 (0.21, 0.37) in 2005 and it was 0.31 (0.18, 0.51) in 2009. The OR of consumption of unhealthy fat and oil for the richest group compared with the poorest group was 0.07 (0.04, 0.15) in 2005 and it was 0.31 (0.18, 0.51) in 2009. The OR of insufficient consumption of fish for the richest group compared with the poorest group was 0.30 (0.22, 0.41) in 2005 and it was 0.31 (0.25, 1.03) in 2009.
The OR of physical inactivity for the richest group compared with the poorest group was 1.12 (0.77, 1.62) in 2005 and it was 2.40 (1.41, 4.08) in 2009. As rank of the quintiles increased, the OR of excess weight, smoking, and hypercholesterolemia were not significant in 2005 and 2009. The OR of excess weight for the richest group compared with the poorest group was 0.80 (0.61, 1.05) in 2005 and it was 1.23 (0.73, 1.90) in 2009. The OR of smoking for the richest group compared with the poorest group was 1.07 (0.74, 1.55) in 2005 and it was 0.82 (0.45, 1.51) in 2009. The OR of hypercholesterolemia for the richest group compared with the poorest group was 0.82 (0.59, 1.13) in 2005.
Table 3 shows the concentration index for the risk factors for NCDs in 2005 and 2009. Based on the results presented in this table, concentration index for risk factors for hypertension, insufficient consumption of fruits and vegetables and consumption of unhealthy fat and oil were negative in both 2005 and 2009. The concentration index for insufficient consumption of fish in 2005 shows the inequality and higher prevalence of these risk factors among poor socioeconomic groups. The confidence interval of concentration index for physical inactivity was not significant in 2005, but it became positive and significant in 2009 which is a sign of inequality. It shows this kind of inequality is more prevalent among high SES groups.
Table 3.
Concentration index of risk factors for NCDs in 2005 and 2009
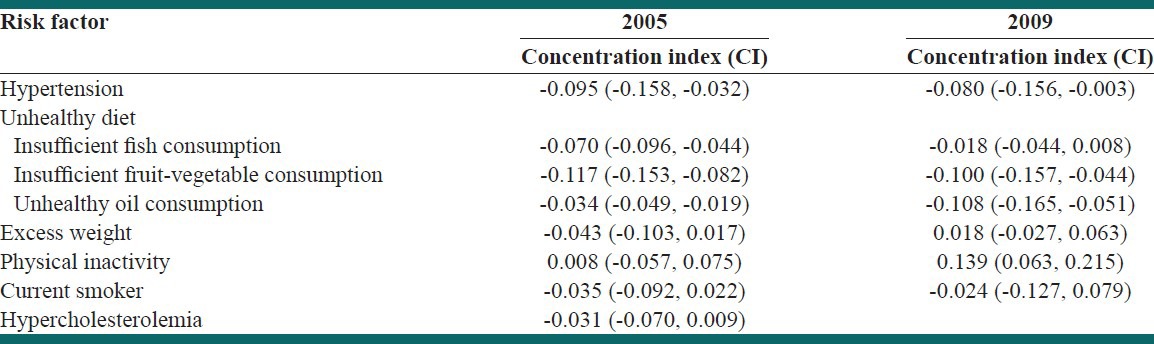
Based on the results presented in the table, the concentration index for smoking and excess weight in both years and hypercholesterolemia in 2005 were not significant. There was no significant inequality in the distribution of these risk factors within the society based on our study.
Figure 1 depicts and compares the concentration curves for risk factors of hypertension, insufficient consumption of fruits and vegetables, insufficient consumption of fish, consumption of unhealthy fat and oil, and physical inactivity that had significant concentration index in 2005 and 2009. The concentration curves for the risk factors of insufficient consumption of fruits and vegetables and insufficient consumption of fish in 2005 and 2009 are above the equality line; it represents the distribution of these risk factors among the poor groups in this time period. The concentration index for physical inactivity had gone under the equality line in the same time period and was directed toward inequality among richer groups.
Figure 1.
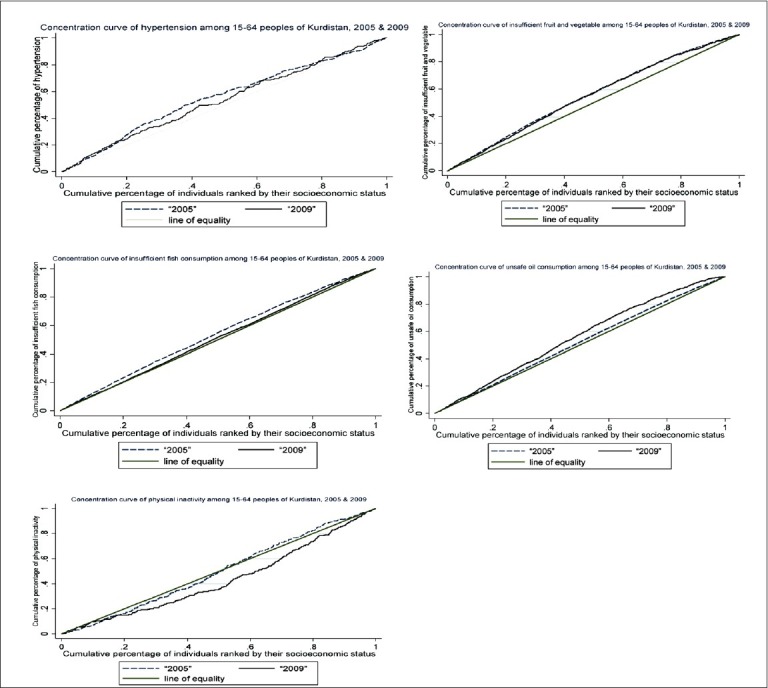
Concentration curves of risk factors for NCDs in 2005 and 2009
DISCUSSION
To the best of our knowledge, this is the first study about socioeconomic inequalities related to risk factors for NCDs which are assessed based on concentration indexes in the Iranian population. The results of the study showed that the prevalence of hypertension, smoking, excess weight, and consumption of unhealthy fat and oil had decreased from 2005 to 2009. However, the prevalence of insufficient consumption of fish, insufficient consumption of fruits and vegetables, and physical inactivity had increased. The results mentioned in this study are in line with other studies conducted in developed countries. Over a specific period of time, the prevalence of risk factors in developed countries decreases. It is directly related to improvement of the economic status of countries.[31]
In this study, the concentration indexes indicated that there are socioeconomic inequalities in hypertension, unhealthy diet (insufficient consumption of fish, insufficient consumption of fruits and vegetables, and consumption of unhealthy fat and oil) from 2005 to 2009. It means that these risk factors are more prevalent among the low SES groups. In addition, the inequality had not been eliminated in this time period. It shows that policies and health-care interventions had not been successful in reducing inequality. Nonetheless, inequality in insufficient consumption of fish had a slight decrease in 2009. In this study, the concentration indexes showed that there are no overt socioeconomic inequalities in smoking, excess weight, and hypercholesterolemia. As there has not been any inequality in three parameters during this period, it can be seen as a positive sign of the performance of the health-care system. Positive concentration index of physical inactivity shows a higher prevalence of this risk factor among the high SES groups. Therefore, the health-care system must not ignore high SES groups in its policies and interventions.
Our findings about inequalities in risk factors have some points of agreement and disagreement with other studies. In the following discussion, we present these points for every risk factor.
Hypertension: The results of our study about inequality in hypertension are in line with the results of most of the other studies which had assessed the relationship between hypertension and SES. Many studies show that there is an inverse relation between hypertension and SES, that is, hypertension is more prevalent among low SES people. Such a condition is extensively reported in developed countries and countries with high per capita income.[32,33,34,35] Such a finding is related to the factors of education and income. Nevertheless, some studies reported opposite findings, that is, they reported a lower prevalence of hypertension among low SES groups.[36,37]
Unhealthy diet: In line with other studies, our findings show that unhealthy diet is more common among low SES people. Many of the studies that introduced a general measure about the relationship between SES and unhealthy diet reported an inverse relation between them.[38,39] We used three consumption habits as signs of an unhealthy diet; in the following paragraphs, we present a comparison of our findings with other studies.
Insufficient consumption of fruits and vegetables: Our findings about inequality in consumption of fruits and vegetables are in line with most of the studies conducted in other countries. People with high SES consume more fruits and vegetables, whereas low SES people consume less fruits and vegetables.[40,41,42,43,44,45] In developed countries, both income and education are directly related to fruit and vegetable consumption.[43,44,45,46,47]
Contrary to our findings, in areas in which fruits and vegetables are easily and cheaply accessible, consumption is more prevalent among low SES people.[48]
Insufficient consumption of fish: The results of our study about inequality in the consumption of fish are in line with other studies. Regular consumption of fish reduces the risk of coronary diseases. A study conducted in European countries showed that regular consumption of fish—more than twice a week—is directly related to SES. People with higher education eat more fish.[49] Another study found a direct relationship between income and educational level and fish consumption.[50]
Consumption of unhealthy oil and fat: The results of our study about consumption of unhealthy oil and fat are in line with other studies. Consumption of unhealthy oil and fat is directly related to SES.[51,52]
Smoking: Many other studies represent inequality in smoking; we did not find inequality in smoking. Although the results of our study are not in line with many of the other studies, the existing literature can help us to verify our findings. Review of existing articles shows that inequalities in smoking and relationship with SES are connected with the level of smoking epidemic in each region or country. This relationship has different patterns.[53]
Based on the results of a systematic review, smoking patterns in many countries follow the diffusion model of tobacco epidemic. This model show that the highest level of socioeconomic inequality is in the last phase of the smoking epidemic. Inequality remains stable in the last phase, whereas in the previous phases, there is a variation among different SES groups. Although, prior to 1990, smoking was more prevalent among higher SES groups, in 2000, smoking became more prevalent among lower SES groups and especially the youth in western and developed countries. This situation has become stable since then.[54,55,56,57]
In developed countries, smoking is related to gender as well. Compared with men, there are more inequalities in the initiation and cessation of smoking in women.[58] In the last phase of the smoking epidemic, smoking is more prevalent among young women with high SES.[59]
Two studies in Korea showed that smoking inequality existed in all educational groups among both sexes and it had increased over time. In this country, smoking is more prevalent among low SES groups. The pattern of smoking in this country is different from western countries, that is, in western and developed countries, smoking epidemic is in its last phases and smoking is more prevalent among women with higher SES.[60,61]
The two factors of education and income are rapidly improving among Iranian people. It is expected to result in different patterns of smoking among different SES groups. Although there is no inequality in smoking, it is expected to be present in the future. Smoking will be more prevalent among women with high SES and young men with low SES in the future. Most of the studies used educational level as a socioeconomic measure and they rarely used income or assets as their measures; this may affect the results.[54]
As we found no inequality in smoking, it can be attributed to the good performance of the health-care system.
Excess weight: The results of previous studies about inequality in excess weight can help to interpret the results of our study. The prevalence of excess weight among different SES groups is related to annual per capita income, and development level of each country. In low-income countries, excess weight is directly related to the SES of the people. However, in upper- and middle-income developing economies, lower SES groups are more exposed to excess weight. Excess weight is more prevalent among low SES groups. In many upper- and middle-income economies and part of the lower- and middle-income economies, Gross domestic product (GDP) growth is positively related to excess weight in low socioeconomic groups.[62,63] When income is used instead of education as a measure for SES, it is likely to have some changes in the relationship between SES and excess weight.[63] Social insights into excess weight in developed countries has reversed this relationship.[64]
In a study conducted in 2005 in Thailand, improvement in SES was positively related to excess weight among men and inversely related to overweight among women younger than 40. This pattern has been observed in other developing countries as well. The pattern previously observed in developed countries, is gradually emerging in developing countries. This pattern is augmented by improvements in education and income.[65]
As Iranian people are experiencing a transition phase regarding SES factors, inequality patterns in excess weight may be various among different SES groups. as the fact that we did not find any inequality in excess weight can be attributed to good performance of the health-care system.
Physical inactivity: The result of our study about physical inactivity is in line with some studies and contrary to some other studies. The studies about inequality in physical inactivity have reported two opposing findings. The first group of studies involves those which reported a direct relationship between SES and physical inactivity especially among women.[66] Another group of studies shows that in developed countries, low SES is concurrent with excess weight and physical inactivity. These studies found a connection between sufficient physical activity and high SES; when education is used as a measure for SES, it has a direct relationship with physical activity especially during leisure time.[66,67,68,69,70]
A study reported that there is no relationship between physical activity and SES based on education and income.[69] Using different definitions and measures for assessing physical inactivity has led to varying and even opposing results for this risk factor. However, our finding about inequality in excess weight in high SES groups is in line with some of the studies mentioned. Owning cars, an urban life style, and working in sedentary jobs are among the factors contributing to more physical inactivity among high SES groups.
Hypercholesterolemia: Our findings about hypercholesterolemia are in line with the results of some studies. The hypercholesterolemia inequality—with a slight variation—is not significant in our study. This can be interpreted using existing literature. The prevalence of hypercholesterolemia among SES groups is related to the developmental phase of the country, national gross national product (GNP) per capita, and time. Based on a study, prevalence of hypercholesterolemia had decreased in the United States as a developed country between 1971 and 2002. During this period, people with better SES had reduced their cholesterol level more and hypercholesterolemia had become more prevalent among the low SES groups.[71] Nonetheless, developed countries are different from developing countries regarding this kind of inequality. Based on a study, the total cholesterol level among children in Brazil has a direct relationship with their SES.[72] The inequality distribution pattern of hypercholesterolemia among SES groups is related to time, phase of development, age group, and some other factors.[31]
Generally, the results of this study demonstrated inequality in some risk factors for NCDs and the stability of inequality during this five-year period. As is reported in other studies as well, the distribution pattern of inequality in risk factors for NCDs is related to time, phase of development, age group, and some cultural, social, and political factors in each country.[31] This shows that SES is related to the prevalence of risk factors, and to plan and implement proper interventions, it is necessary to pay attention to this relationship. The nature of the risk factors makes some of them more prevalent among high SES groups; however, most of these risk factors are more prevalent among low SES groups. Therefore, some of the actions that can be taken to decrease socioeconomic inequalities include: Reduction of poverty, improvements in educational level, providing more support for the poor within health-care policies, improving accessibility of services for the deprived people, and planning special programs to decrease inequality. Equality and promotion of justice are among the main goals of Iranian politicians and governors. This provides a base to health-care managers in Iran to reduce inequalities in health care. Reduction of socioeconomic inequalities must be included in main health-care goals. More attention must be paid to those risk factors which are more prevalently distributed; it is necessary to provide more training, presentational, and clinical facilities to eliminate these risk factors. To decrease socioeconomic inequalities related to an unhealthy diet, as an intervention method, poor people may be granted subsides. As elimination of inequalities is among the goals of the health-care system, it is recommended to assess measures for risk factor inequality in the country at proper time intervals. Because of problems of urbanization and the fact that physical inactivity is more prevalent among the richer groups of society, it may be helpful to promote public training within the society.
Our study had some limitations. The socioeconomic data in 2005 was limited. As the number of assets in that year was limited, we included education and income status to determine SES. The limited number of assets decreases the variability of the first factor of PCA which is used for calculating asset factors. The small sample size of the survey in 2009 was another limitation for our study and the results had less precision. It is not possible to monitor lifelong SES (SES lifetime) and it adds another limitation to our study. It was not possible to use exactly identical definitions for some of the variables. The questionnaire used in these two years for some variables like physical inactivity and consumption of fruits and vegetables were different and it was not possible to use exactly similar definitions for them. Some measures were self-reported and recall bias was probable. It was likely that participants reported what they socially accepted. This study involved only the population of Kurdistan and cannot be generalized for the country.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.WHO. Global status report on noncommunicable diseases 20102011 2011. Report No.: 978 92 4 156422 9 [Google Scholar]
- 2.Alwan A, Maclean DR, Riley LM, d’Espaignet ET, Mathers CD, Stevens GA, et al. Monitoring and surveillance of chronic non-communicable diseases: Progress and capacity in high-burden countries. Lancet Nov. 2010;376:1861–8. doi: 10.1016/S0140-6736(10)61853-3. [DOI] [PubMed] [Google Scholar]
- 3.Ambati J. Age-related macular degeneration and the other double helix. The Cogan Lecture. Invest Ophthalmol Vis Sci. 2011;52:2165–9. doi: 10.1167/iovs.11-7328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geneva: World Health Organization; 2005. WHO. Preventing chronic diseases: A vital investment. [Google Scholar]
- 5.Samb B, Desai N, Nishtar S, Mendis S, Bekedam H, Wright A, et al. Prevention and management of chronic disease: A litmus test for health-systems strengthening in low-income and middle-income countries. Lancet. 2010;376:1785–97. doi: 10.1016/S0140-6736(10)61353-0. [DOI] [PubMed] [Google Scholar]
- 6.Boutayeb A. The double burden of communicable and non-communicable diseases in developing countries. Trans R Soc Trop Med Hyg. 2006;100:191–9. doi: 10.1016/j.trstmh.2005.07.021. [DOI] [PubMed] [Google Scholar]
- 7.Sugiyama T, Leslie E, Giles-Corti B, Owen N. Physical activity for recreation or exercise on neighbourhood streets: Associations with perceived environmental attributes. Health Place. 2009;15:1058–63. doi: 10.1016/j.healthplace.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 8.Gulliford MC, Mahabir D, Rocke B. Socioeconomic inequality in blood pressure and its determinants: Cross-sectional data from Trinidad and Tobago. J Hum Hypertens. 2004;18:61–70. doi: 10.1038/sj.jhh.1001638. [DOI] [PubMed] [Google Scholar]
- 9.Wagner KH, Brath H. A global view on the development of non communicable diseases. Prev Med. 2012;54(Suppl):S38–41. doi: 10.1016/j.ypmed.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 10.Sarraf-Zadegan N, Boshtam M, Malekafzali H, Bashardoost N, Sayed-Tabatabaei FA, Rafiei M, et al. Secular trends in cardiovascular mortality in Iran, with special reference to Isfahan. Acta Cardiologica. 1999;54:327–33. [PubMed] [Google Scholar]
- 11.Farzadfar F, Danaei G, Namdaritabar H, Rajaratnam JK, Marcus JR, Khosravi A, et al. National and subnational mortality effects of metabolic risk factors and smoking in Iran: A comparative risk assessment. Popul Health Metr. 2011;9:55. doi: 10.1186/1478-7954-9-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.WHO maps noncommunicable disease trends in all countries: Country profiles on noncommunicable disease trends in 193 countries. Cent Eur J Public Health. 2011;19:130. 8. [PubMed] [Google Scholar]
- 13.Braveman P, Gruskin S. Defining equity in health. Journal of epidemiology and community health. 2003;57:254–8. doi: 10.1136/jech.57.4.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gwatkin DR. Health inequalities and the health of the poor: What do we know? What can we do? Bull World Health Organ. 2000;78:3–18. [PMC free article] [PubMed] [Google Scholar]
- 15.Hosseinpoor AR, Van Doorslaer E, Speybroeck N, Naghavi M, Mohammad K, Majdzadeh R, et al. Decomposing socioeconomic inequality in infant mortality in Iran. Int J Epidemiol. 2006;35:1211–9. doi: 10.1093/ije/dyl164. [DOI] [PubMed] [Google Scholar]
- 16.Wagstaff A. Poverty and health sector inequalities. Bull World Health Organ. 2002;80:97–105. [PMC free article] [PubMed] [Google Scholar]
- 17.Nedjat S, Hosseinpoor AR, Forouzanfar MH, Golestan B, Majdzadeh R. Decomposing socioeconomic inequality in self-rated health in Tehran. J Epidemiol Community Health. 2012;66:495–500. doi: 10.1136/jech.2010.108977. [DOI] [PubMed] [Google Scholar]
- 18.Emamian MH, Zeraati H, Majdzadeh R, Shariati M, Hashemi H, Fotouhi A. The gap of visual impairment between economic groups in Shahroud, Iran: A Blinder-Oaxaca decomposition. Am J Epidemiol. 2011;173:1463–7. doi: 10.1093/aje/kwr050. [DOI] [PubMed] [Google Scholar]
- 19.Hosseinpoor AR, Mohammad K, Majdzadeh R, Naghavi M, Abolhassani F, Sousa A, et al. Socioeconomic inequality in infant mortality in Iran and across its provinces. Bull World Health Organ. 2005;83:837–44. [PMC free article] [PubMed] [Google Scholar]
- 20.Hosseinpoor AR, Naghavi M, Alavian SM, Speybroeck N, Jamshidi H, Vega J. Determinants of seeking needed outpatient care in Iran: Results from a national health services utilization survey. Arch Iran Med. 2007;10:439–45. [PubMed] [Google Scholar]
- 21.Alikhani S, Delavari A, Alaedini F, Kelishadi R, Rohbani S, Safaei A. A province-based surveillance system for the risk factors of non-communicable diseases: A prototype for integration of risk factor surveillance into primary healthcare systems of developing countries. Public Health. 2009;123:358–64. doi: 10.1016/j.puhe.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 22.Kelishadi R, Alikhani S, Delavari A, Alaedini F, Safaie A, Hojatzadeh E. Obesity and associated lifestyle behaviours in Iran: Findings from the First National Non-communicable Disease Risk Factor Surveillance Survey. Public Health Nutr. 2008;11:246–51. doi: 10.1017/S1368980007000262. [DOI] [PubMed] [Google Scholar]
- 23.Organization WH. The WHO STEPwise approach to Surveillance of chronic noncommunicable diseases risk factors. 2008 [Google Scholar]
- 24.O’Donnell O vDE, Wagstaff A. Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and Their Implementation. 2008 [Google Scholar]
- 25.Vyas S, Kumaranayake L. Constructing socio-economic status indices: How to use principal components analysis. Health Pol Plann. 2006;21:459–68. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- 26.Gwatkin DR, Rutstein S, Johnson K, Suliman E, Wagstaff A, Amouzou A. Socio-economic differences in health, nutrition, and population within developing countries: An overview. Niger J Clin Pract. 2007;10:272–82. [PubMed] [Google Scholar]
- 27.Clarke PM, Gerdtham UG, Connelly LB. A note on the decomposition of the health concentration index. Health Econ. 2003;12:511–6. doi: 10.1002/hec.767. [DOI] [PubMed] [Google Scholar]
- 28.Zhang Q, Wang Y. Using concentration index to study changes in socio-economic inequality of overweight among US adolescents between 1971 and 2002. Int J Epidemiol. 2007;36:916–25. doi: 10.1093/ije/dym064. [DOI] [PubMed] [Google Scholar]
- 29.Wagstaff A, Paci P, van Doorslaer E. On the measurement of inequalities in health. Soc Sci Med. 1991;33:545–57. doi: 10.1016/0277-9536(91)90212-u. [DOI] [PubMed] [Google Scholar]
- 30.Honjo K, Kawakami N, Takeshima T, Tachimori H, Ono Y, Uda H, et al. Social class inequalities in self-rated health and their gender and age group differences in Japan. J Epidemiol. 2006;16:223–32. doi: 10.2188/jea.16.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fuentes R, Uusitalo T, Puska P, Tuomilehto J, Nissinen A. Blood cholesterol level and prevalence of hypercholesterolaemia in developing countries: A review of population-based studies carried out from 1979 to 2002. Eur J Cardiovasc Prev Rehabil. 2003;10:411–9. doi: 10.1097/01.hjr.0000085247.65733.4f. [DOI] [PubMed] [Google Scholar]
- 32.Colhoun HM, Dong W, Poulter NR. Blood pressure screening, management and control in England: Results from the health survey for England 1994. J Hypertens. 1998;16:747–52. doi: 10.1097/00004872-199816060-00005. [DOI] [PubMed] [Google Scholar]
- 33.Bell AC, Adair LS, Popkin BM. Understanding the role of mediating risk factors and proxy effects in the association between socio-economic status and untreated hypertension. Soc Sci Med. 2004;59:275–83. doi: 10.1016/j.socscimed.2003.10.028. [DOI] [PubMed] [Google Scholar]
- 34.Gorman BK, Sivaganesan A. The role of social support and integration for understanding socioeconomic disparities in self-rated health and hypertension. Soc Sci Med. 2007;65:958–75. doi: 10.1016/j.socscimed.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 35.Hickson DA, Diez Roux AV, Wyatt SB, Gebreab SY, Ogedegbe G, Sarpong DF, et al. Socioeconomic position is positively associated with blood pressure dipping among African-American adults: The Jackson Heart Study. Am J Hypertens. 2011;24:1015–21. doi: 10.1038/ajh.2011.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Spruill TM, Gerin W, Ogedegbe G, Burg M, Schwartz JE, Pickering TG. Socioeconomic and psychosocial factors mediate race differences in nocturnal blood pressure dipping. Am J Hypertens. 2009;22:637–42. doi: 10.1038/ajh.2009.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stepnowsky CJ, Jr, Nelesen RA, DeJardin D, Dimsdale JE. Socioeconomic status is associated with nocturnal blood pressure dipping. Psychosom Med. 2004;66:651–5. doi: 10.1097/01.psy.0000138124.58216.6c. [DOI] [PubMed] [Google Scholar]
- 38.Bhargava A. Socio-economic and behavioural factors are predictors of food use in the National Food Stamp Program Survey. Br J Nutr. 2004;92:497–506. doi: 10.1079/bjn20041210. [DOI] [PubMed] [Google Scholar]
- 39.Mead E, Gittelsohn J, Roache C, Sharma S. Healthy food intentions and higher socioeconomic status are associated with healthier food choices in an Inuit population. J Hum Nutr Diet. 2010;23(Suppl 1):83–91. doi: 10.1111/j.1365-277X.2010.01094.x. [DOI] [PubMed] [Google Scholar]
- 40.Smith AM, Baghurst KI. Public health implications of dietary differences between social status and occupational category groups. J Epidemiol Community Health. 1992;46:409–16. doi: 10.1136/jech.46.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rasmussen M, Krolner R, Klepp KI, Lytle L, Brug J, Bere E, et al. Determinants of fruit and vegetable consumption among children and adolescents: A review of the literature. Part I: Quantitative studies. Int J Behav Nutr Phys Act. 2006;3:22. doi: 10.1186/1479-5868-3-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ricciuto L, Tarasuk V, Yatchew A. Socio-demographic influences on food purchasing among Canadian households. Eur J Clin Nutr. 2006;60:778–90. doi: 10.1038/sj.ejcn.1602382. [DOI] [PubMed] [Google Scholar]
- 43.Riediger ND, Moghadasian MH. Patterns of fruit and vegetable consumption and the influence of sex, age and socio-demographic factors among Canadian elderly. J Am Coll Nutr. 2008;27:306–13. doi: 10.1080/07315724.2008.10719704. [DOI] [PubMed] [Google Scholar]
- 44.Azagba S, Sharaf MF. Disparities in the frequency of fruit and vegetable consumption by socio-demographic and lifestyle characteristics in Canada. Nutr J. 2011;10:118. doi: 10.1186/1475-2891-10-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Irala-Estevez JD, Groth M, Johansson L, Oltersdorf U, Prattala R, Martinez-Gonzalez MA. A systematic review of socio-economic differences in food habits in Europe: Consumption of fruit and vegetables. Eur J Clin Nutr. 2000;54:706–14. doi: 10.1038/sj.ejcn.1601080. [DOI] [PubMed] [Google Scholar]
- 46.Dehghan M, Akhtar-Danesh N, Merchant AT. Factors associated with fruit and vegetable consumption among adults. J Hum Nutr Diet. 2011;24:128–34. doi: 10.1111/j.1365-277X.2010.01142.x. [DOI] [PubMed] [Google Scholar]
- 47.Billson H, Pryer JA, Nichols R. Variation in fruit and vegetable consumption among adults in Britain. An analysis from the dietary and nutritional survey of British adults. Eur J Clin Nutr. 1999;53:946–52. doi: 10.1038/sj.ejcn.1600877. [DOI] [PubMed] [Google Scholar]
- 48.Roos G, Johansson L, Kasmel A, Klumbiene J, Prattala R. Disparities in vegetable and fruit consumption: European cases from the north to the south. Public Health Nutr. 2001;4:35–43. doi: 10.1079/phn200048. [DOI] [PubMed] [Google Scholar]
- 49.Pieniak Z, Verbeke W, Scholderer J. Health-related beliefs and consumer knowledge as determinants of fish consumption. J Hum Nutr Diet. 2010;23:480–8. doi: 10.1111/j.1365-277X.2010.01045.x. [DOI] [PubMed] [Google Scholar]
- 50.Petrenya N, Dobrodeeva L, Brustad M, Bichkaeva F, Menshikova E, Lutfalieva G, et al. Fish consumption and socio-economic factors among residents of Arkhangelsk city and the rural Nenets autonomous area. Int J Circumpolar Health. 2011;70:46–58. doi: 10.3402/ijch.v70i1.17798. [DOI] [PubMed] [Google Scholar]
- 51.Ordovas JM, Kaput J, Corella D. Nutrition in the genomics era: Cardiovascular disease risk and the Mediterranean diet. Mol Nutr Food Res. 2007;51:1293–9. doi: 10.1002/mnfr.200700041. [DOI] [PubMed] [Google Scholar]
- 52.Erkkila AT, Sarkkinen ES, Lehto S, Pyorala K, Uusitupa MI. Diet in relation to socioeconomic status in patients with coronary heart disease. Eur J Clin Nutr. 1999;53:662–8. doi: 10.1038/sj.ejcn.1600829. [DOI] [PubMed] [Google Scholar]
- 53.Cavelaars AE, Kunst AE, Geurts JJ, Crialesi R, Grotvedt L, Helmert U, et al. Educational differences in smoking: International comparison. BMJ. 2000;320:1102–7. doi: 10.1136/bmj.320.7242.1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schaap MM, Kunst AE. Monitoring of socio-economic inequalities in smoking: Learning from the experiences of recent scientific studies. Public Health. 2009;123:103–9. doi: 10.1016/j.puhe.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 55.Genereux M, Roy M, Montpetit C, Azzou SA, Gratton J. Regional surveillance of social and geographic inequalities in smoking: The case of Montreal, Canada. Health Place. 2012;18:240–9. doi: 10.1016/j.healthplace.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 56.Bernat DH, Lazovich D, Forster JL, Oakes JM, Chen V. Area-level variation in adolescent smoking. Prev Chronic Dis. 2009;6:A42. [PMC free article] [PubMed] [Google Scholar]
- 57.Laaksonen M, Prattala R, Helasoja V, Uutela A, Lahelma E. Income and health behaviours. Evidence from monitoring surveys among Finnish adults. J Epidemiol Community Health. 2003;57:711–7. doi: 10.1136/jech.57.9.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Legleye S, Khlat M, Beck F, Peretti-Watel P. Widening inequalities in smoking initiation and cessation patterns: A cohort and gender analysis in France. Drug Alcohol Depend. 2011;117:233–41. doi: 10.1016/j.drugalcdep.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 59.Fukuda Y, Nakamura K, Takano T. Socioeconomic pattern of smoking in Japan: Income inequality and gender and age differences. Ann Epidemiol. 2005;15:365–72. doi: 10.1016/j.annepidem.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 60.Khang YH, Cho HJ. Socioeconomic inequality in cigarette smoking: Trends by gender, age, and socioeconomic position in South Korea, 1989-2003. Prev Med. 2006;42:415–22. doi: 10.1016/j.ypmed.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 61.Cho HJ, Song YM, Smith GD, Ebrahim S. Trends in socio-economic differentials in cigarette smoking behaviour between 1990 and 1998: A large prospective study in Korean men. Public Health. 2004;118:553–8. doi: 10.1016/j.puhe.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 62.Monteiro CA, Conde WL, Lu B, Popkin BM. Obesity and inequities in health in the developing world. Int J Obes Relat Metab Disord. 2004;28:1181–6. doi: 10.1038/sj.ijo.0802716. [DOI] [PubMed] [Google Scholar]
- 63.Fernald LC. Socio-economic status and body mass index in low-income Mexican adults. Soc Sci Med. 2007;64:2030–42. doi: 10.1016/j.socscimed.2007.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sobal J, Stunkard AJ. Socioeconomic status and obesity: A review of the literature. Psychol Bull. 1989;105:260–75. doi: 10.1037/0033-2909.105.2.260. [DOI] [PubMed] [Google Scholar]
- 65.Seubsman SA, Lim LL, Banwell C, Sripaiboonkit N, Kelly M, Bain C, et al. Socioeconomic status, sex, and obesity in a large national cohort of 15-87-year-old open university students in Thailand. J Epidemiol. 2010;20:13–20. doi: 10.2188/jea.JE20090014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Najman JM, Toloo G, Siskind V. Socioeconomic disadvantage and changes in health risk behaviours in Australia: 1989-90 to 2001. Bull World Health Organ. 2006;84:976–84. doi: 10.2471/blt.05.028928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nedo E, Paulik E. Association of smoking, physical activity, and dietary habits with socioeconomic variables: A cross-sectional study in adults on both sides of the Hungarian-Romanian border. BMC Public Health. 2012;12:60. doi: 10.1186/1471-2458-12-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fong CW, Bhalla V, Heng D, Chua AV, Chan ML, Chew SK. Educational inequalities associated with health-related behaviours in the adult population of Singapore. Singapore Med J. 2007;48:1091–9. [PubMed] [Google Scholar]
- 69.Pitsavos C, Panagiotakos DB, Lentzas Y, Stefanadis C. Epidemiology of leisure-time physical activity in socio-demographic, lifestyle and psychological characteristics of men and women in Greece: The ATTICA Study. BMC Public Health. 2005;5:37. doi: 10.1186/1471-2458-5-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dowler E. Inequalities in diet and physical activity in Europe. Public Health Nutr. 2001;4:701–9. doi: 10.1079/phn2001160. [DOI] [PubMed] [Google Scholar]
- 71.Kanjilal S, Gregg EW, Cheng YJ, Zhang P, Nelson DE, Mensah G, et al. Socioeconomic status and trends in disparities in 4 major risk factors for cardiovascular disease among US adults, 1971-2002. Arch Intern Med. 2006;166:2348–55. doi: 10.1001/archinte.166.21.2348. [DOI] [PubMed] [Google Scholar]
- 72.Bergmann ML, Bergmann GG, Halpern R, Rech RR, Constanzi CB, Alli LR. Associated factors to total cholesterol: school based study in southern Brazil. Arq Bras Cardiol. 2011;97:17–25. doi: 10.1590/s0066-782x2011005000065. [DOI] [PubMed] [Google Scholar]


