Abstract
This study advances Community-based Participatory Research (CBPR) by presenting a set of triangulated procedures (steps and actions) that can facilitate participatory research in myriad international settings. By using procedural triangulation—the combination of specific steps and actions as the basis for the International Participatory Research Framework (IPRF)—our approach can improve the abilities of researchers and practitioners worldwide to systematize the development of research partnerships. The IPRF comprises four recursive steps: (i) contextualizing the host country; (ii) identifying collaborators in the host country; (iii) seeking advice and endorsement from gatekeepers and (iv) matching partners’ expertise, needs and interests. IPRF includes the following sets of recursive participatory actions: (A1) becoming familiar with local languages and culture; (A2) sharing power, ideas, influence and resources; (A3) gathering oral and written information about partners; (A4) establishing realistic expectations and (A5) resolving personal and professional differences. We show how these steps and actions were used recursively to build a partnership to study the roles of community health workers (CHWs) in Brazil's Family Health Program (PSF). The research conducted using IPRF focused on HIV prevention, and it included nearly 200 CHWs. By using the IPRF, our partnership achieved several participatory outcomes: community-defined research aims, capacity for future research and creation of new policies and programs. We engaged CHWs who requested that we study their training needs, and we engaged CHWs’ supervisors who used the data collected to modify CHW training. Data collected from CHWs will form the basis for a grant to test CHW training curricula. Researchers and community partners can now use the IPRF to build partnerships in different international contexts. By triangulating steps and actions, the IPRF advances knowledge about the use of CBPR methods/procedures for international health research.
Keywords: CBPR, international research, community health workers, HIV prevention
Globally, 33 million people live with HIV. In 2009, an estimated 92 000 people became infected with HIV in Latin America, compared with 99 000 in 2001. One-third of all HIV-positive individuals in Latin American reside in Brazil. In 2009, the estimated prevalence rate in adults between the ages of 15–49 in Brazil was 0.3–0.6% and the incidence was <0.1% (UNAIDS, 2009). Early and ongoing HIV prevention efforts have helped contain the epidemic in Brazil. One key effort was the creation of a Unified National Health System in the 1990s and the implementation of universal access to AIDS medicines, starting in 1996–1997 (Parker, 2003; Teixeira, 2003; Berkman et al., 2005; Remien et al., 2007). Community health workers (CHWs), most of whom are women with a high school education, are an integral part of the Brazil Unified National Health System. The estimated number of CHWs employed in local communities by the Family Heath Program (PSF) is nearly 300 000 countrywide. CHWs are each responsible for registering, counseling some 1000 families and acting as a liaison between neighborhood families and the local PSF clinics. During home visits and in community-wide presentations, CHWs provide HIV/AIDS prevention services and help HIV-positive individuals with medical daily needs, including medication adhence (Ministério da Saúde Brazil, 2011).
To help halt the spread of HIV in developing countries, such as Brazil, prevention scientists have forged partnerships with other researchers, services providers, politicians, clergy and members of local communities. In 2009 alone, the United States National Institutes of Health spent USD 368 million on international HIV research (Kaiser Reports, 2009). Nonetheless, specific procedures for forging collaborative partnerships and conducting participatory research are still lacking in the literature. Therefore, this paper proposes the International Participatory Research Framework (IPRF), grounded in a procedural triangulation framework, described below, framed by specific steps and actions that may facilitate international participatory research. Our framework responds to Wright et al.'s call for an International Collaboration on participatory research (Wright et al., 2010).
Wright et al. contend that simply by examining the principles of participatory research (Israel et al., 1998), one can see a lack of cohesion and standardization among research claiming to be participatory. Many studies characterized as ‘participatory’ violate some of the principles proposed in Israel et al.'s seminal work (Israel et al., 1998). With only a set of principles to guide participatory research, the scientific evidence arising from such research is sometimes deemed less credible and non-replicable. By moving beyond a set of principles and by standardizing procedures for forging partnerships, the scientific basis of participatory research will gain further support.
The most influential review of the existing literature on Community-based Participatory Research (CBPR) (Viswanathan et al., 2004) concludes that implementation of CBPR varied widely across the studies in the review. The review regrettably does not provide a set of procedures to initiate participatory research. Lacking this information, researchers are unable to standardize how they go about forming partnerships and producing scientific evidence, guided only by a set of principles, which are widely and diversely interpreted. Moreover, participatory research has been developed, practiced and studied based on a set of principles that arose out of domestic research in the USA. There is a dearth of literature about how to apply those principles in an international context. Lacking well-articulated steps and actions to follow, partnerships between researchers in the USA and partners abroad may fail to thrive.
This study therefore moves CBPR beyond the extant literature by presenting a set of triangulated procedures (steps and actions), exemplified through a case illustration that can facilitate participatory research in international contexts. By using the concept of procedural triangulation (Maxwell, 2005; Alasuutari et al., 2008; Creswell, 2009)—the combination of specific steps and actions as the basis for our framework we have created a novel approach that can improve researchers’ and practitioners’ abilities to systematize the development of partnerships and to enhance community participation by converging different procedures. By combining steps and actions, the framework advances our knowledge about procedural requirements for international participatory research.
The IPRF represents a contribution to the literature that has not yet been articulated. The IPRF emphasizes the accomplishment of participatory outcomes: community-defined research aims, capacity building for research and new policies and programs. The case illustration presented herein is intended to describe how the IPRF was used to develop a research partnership between individuals in Brazil and the USA. The paper is not intended to show causation between IPRF participatory steps and actions and the outcomes achieved. Rather, it identifies, by reflecting upon the experience outlined in the case illustration, specific procedures that helped a research partnership pursue goals defined collaboratively with a local community, build capacity for future research and develop policies and programs guided by research findings. This unique contribution will help other partnerships in varied international contexts.
INTERNATIONAL PARTICIPATORY RESEARCH
Language and cultural differences may impede communication between researchers and local partners (e.g. residents and service providers). Differences in expectations around ethical issues (e.g. incentives and human rights) may prevent the formation of, or cause the early termination of partnerships. The fluctuation of currencies in developing countries causes variations in local staff salaries and may result in irreconcilable budgetary difficulties. Local politics and rapid turnover of appointed staff within health care systems may affect participant recruitment, data collection, intervention implementation and the community's willingness or ability to use research findings. If unattended, these issues may also aggravate vulnerable communities’ suspicions and negative attitudes toward research and researchers (Lo and Bayer, 2003; Baptiste et al., 2006). CBPR seeks to address these issues through a transformative process of collaboration wherein research partners (e.g. researchers, community residents and service providers) are involved in multiple aspects of research, from determining goals to developing methods and procedures to disseminating results (Pinto et al., 2011).
The CBPR literature shows that community-researcher collaboration can help partners achieve participatory outcomes, including community-defined research aims; capacity for long-term partnership and research and policies and programs based upon research findings (Israel et al., 2003; Viswanathan et al., 2004; McKay et al., 2007). However, the CBPR literature lacks specificity regarding how to initiate, employ and sustain participation when working with partners internationally in developing countries. The participatory research literature has indeed described numerous international projects, particularly focused on HIV prevention (Mosavel et al., 2005; Guerin et al., 2009). However, these studies contain disparate conceptions of participatory principles, theory and practice. A lack of systematized approaches for community-researcher collaboration in international research has left researchers and community partners without a framework from which to initiate community engagement and incorporate participatory principles into research. Without clearly defined steps and actions, participatory research methods and procedures may become unpredictable and thus less rigorous.
The CBPR literature suggests an approach to research that is grounded in a philosophical orientation favoring equal participation between community and researchers. This philosophy is built on principles that do not prescribe specific actions or steps for developing and maintaining partnerships. Instead, this literature offers a set of values toward which research partners ought to aspire. Therefore, CBPR is an approach to research, rather than a method in itself (Israel et al., 2005). Whereas the CBPR literature in the USA favors shifting the ownership of research aims and outcomes to the community (Minkler and Wallerstein, 2003), it is still unknown how to put these principles into practice in an international context. CBPR is in its nascent stages and has been practiced in myriad different ways, making it difficult to evaluate and replicate specific steps and actions.
International CBPR needs to be rigorously studied, documented and systematized in order to keep pace with the science that drives it, and to make research findings useful to international partners. To this end, the IPRF is grounded in CBPR principles as a guiding force from which specific steps and actions arise. The IPRF below is comprised of steps and actions that research partners may undertake to conduct participatory research. This framework is crucial for scholars, researchers and community partners worldwide seeking to conduct research collaboratively because it can be tailored for use in diverse contexts. A careful review of the literature in the past 5 years (2006–2011) generated a handful of articles about CBPR partnerships. However, none articulated a framework that guided specific procedures that other partnerships might follow or were based on an international CBPR partnership. We therefore present an implementation framework for participatory research in an international context that represents a novel contribution to the literature.
INTERNATIONAL PARTICIPATORY RESEARCH FRAMEWORK
The IPRF is built on previous work articulating participatory steps that, when used recursively, can facilitate community-researcher collaboration (Pinto et al., 2007). The IPRF is grounded in the Balance Theory of Coordination (Litwak and Meyer, 1966; Litwak et al., 1977) stating that research partners (e.g. researchers, service providers and community residents) can best define research goals and attain results useful to all parties by capitalizing upon each partner's unique knowledge and skills (Pinto, 2009). This suggests that it is not necessary for all partners to perform the same tasks, but rather to use their strengths in a way that combines the unique skill sets that they possess to create new knowledge. For example, it is not necessary for all partners to analyze data, since some partners may not have the training to do so. However, it is possible for researchers to include member checks and other forms of consultation throughout the analysis of both qualitative and quantitative data (Cashman et al., 2008). Therefore, IPRF steps and actions require that research partners work closely together so as to learn new skills from one another and to develop research methods that incorporate all partners’ knowledge and skill sets. IPRF is novel because it uses a procedural triangulation (Maxwell, 2005; Alasuutari et al., 2008; Creswell, 2009) combining steps and actions.
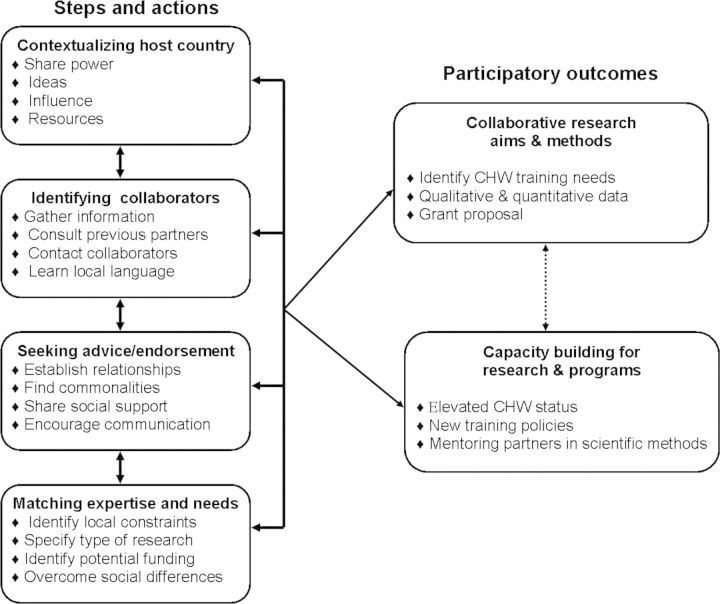
IPRF steps are: (i) contextualizing the host country; (ii) identifying collaborators in the host country; (iii) seeking advice and endorsement from gatekeepers and (iv) matching partners’ expertise, needs and interests. In order to complete these steps, five participatory sets of actions are recommended alongside these steps: (A1) becoming familiar with local languages and cultural norms by interacting socially and professionally with local partners and community residents; (A2) sharing power, ideas, influence and resources; (A3) gathering oral and written information about partners; (A4) defining collaboratively the scope of the research in order to establish realistic expectations and (A5) resolving personal and professional differences by communicating openly and honestly.
Figure 1 below depicts how recursive participatory steps and actions can facilitate participatory outcomes. Each component of framework is exemplified by a case illustration of how IPRF was used by a partnership between researchers in Brazil and the USA and community-based partners in Brazil.
Fig. 1:
International participatory research framework.
Case illustration: community health workers and HIV prevention in Brazil
The IPRF can help systematize the processes needed to establish international research partnerships. To demonstrate the implementation of the IPRF, this case illustration highlights a partnership between Universities X and Y in the USA and Brazil, respectively, and PSF nurse coordinators and CHWs. The study for which this partnership was developed aimed to explore how CHWs integrate indigenous and scientific knowledge to help low-income families prevent HIV/AIDS. It is noteworthy that CHWs reside in the communities where they work, thus making their participation in the research partnership doubly important. The summary narration of partnership-building below reflects the input of several collaborators and has been organized around IPRF's participatory steps and sets of actions. Table 1 provides a timeline for the 3-year duration of this project. Table 1 shows IPRF steps and actions as they occurred and the challenges we faced each step of the way.
Table 1:
Case illustration: IPRF Timeline, steps, challenges faced and solutions
| Timeline | Research process | Participatory steps | Challenges | Participatory actions |
|---|---|---|---|---|
| Pre-research | Identifying partners | (i) Contextualizing host country | Unfamiliar with local cultures | A1: Become familiar with local languages and cultural norms by interacting socially and professionally with local partners and community residents |
| Obtaining funds | Limited time/funds to address local needs | |||
| Defining study aims | ||||
| Year 1 | Training interviewers | (ii) Identifying collaborators in the host country | Community mistrust/skepticism about research | A2: Share power, ideas, influence and resources |
| Professional differences | ||||
| Year 1 and 2 | Identifying and recruiting participants | (iii) Seeking advice/endorsement from gatekeepers | Changes in administration and political parties | A3: Gather oral and written information about partners |
| Differences in salaries and currencies | ||||
| Year 2 and 3 | Data collection and analysis | (iv) Matching partners’ expertise, needs and interests | Achieving consensus about research aims | A4: Define collaboratively the scope of the research in order to establish realistic expectations |
| Differences in interpretation of data | A5: Resolve personal and professional differences by communicating openly and honestly |
The pre-research period lasted 1 year and the research itself took 3 years to be completed.
Steps were used recursively, but all were used during the pre-research period. Steps should be repeated as many times as needed.
Challenges were present at different times and are not necessarily directly connected to one or another step.
Participatory actions helped prevent and/or resolve challenges. Actions were used recursively several times.
Contextualizing the host country
Our initial partnership was established between a Brazilian and American, US-based researcher, and one physician and one nurse in one of the PSF clinics, and the local Secretary of Health. The US-based researcher contacted several possible partners in Brazilian universities. Through a process of identifying mutual research interests and availability of time to pursue this project, he chose to work with a Brazilian researcher who was familiar with the PSF and had an interest in CBPR. Subsequently, the researchers included CHWs in two other cities in decision-making around study aims, data collection and dissemination. All partners helped identify funding sources in Brazil and the USA. We collaboratively wrote a grant proposal which funded data collection and all supplies and materials. All partners made in-kind contributions to the project and/or spent out-of-pocket money. For example, in order to hold the initial meetings with potential collaborators, the researcher from the USA paid his own airfare to Brazil. Brazil-based partners donated many hours of work to the project, outside of their regular, paid work.
Because this project followed CBPR principles, all partners, including the physician and the nurse, performed the role of research at different times. These roles included training of interviewers, recruiting CHWs and data collection and analysis. Although both principal researchers had command of the native language, they were not well versed in the local cultures. They visited the focal communities several times over the course of the 3-year duration of this study and shadowed CHWs on home visits to learn how CHWs provided HIV prevention information (participatory action A1). Community residents, including CHWs, had never been exposed to researchers and were skeptical about their intentions. Researchers spent work time (e.g. conducting workshops) and social time (e.g. sharing meals) with local partners (A1 and A2). This helped create a sense of belonging for the researchers, and helped the community get to know them. In workshops and in conversations, researchers spoke openly about ethical issues, answered questions about exploitation of research participants and racial, cultural and class differences between researchers, medical staff and CHWs (A5). Because the formative research involved in-depth interviews with CHWs, issues of confidentiality were addressed vigorously. This required training on human subject protection for PSF staff and for seven Master's level students from Brazil involved in data collection (A2).
Identifying collaborators in the host country
Initially the partnership focused on one PSF clinic, but soon expanded to several others. In each, we identified a research partner, usually a nurse who supervised and trained CHWs and who expressed interest in conducting research (A3). CHWs identified among themselves those most interested in research who would help shape the aims of the research, develop data collection strategies and disseminate findings (A3). Fluency in Portuguese helped researchers advance professional and social interactions with all local partners (A4). Researchers acknowledged openly their privileges vis-à-vis the fact that CHWs came from low-income backgrounds and earned approximately one minimum wage monthly salary, BRL580.00 (Brazilian reais) = USD366. By involving different constituencies as partners and by addressing social differences, researchers could share ownership of both the partnership-building process and the project's specific aims (A4). This improved researchers’ understanding of local needs and resources and communication with local partners (A3).
Seeking advice and endorsement from gatekeepers
Our partnership grew as we identified common interests (A4). Establishing relationships with administrators and politicians also helped; their endorsements gave research partners more certainty that research findings would be used to develop local policies (A4). For example, CHWs and their supervisors used in-depth interviews to develop survey questions about training needs. Based on these qualitative and quantitative data, supervisors have changed the content and format of CHW training (A2). Before the research, CHW training content was typically decided by nurses, and based exclusively on epidemiological data. After the research, nurses began to address training needs identified by CHWs. Nurses scheduled a weekly case presentation and discussion series for CHWs to learn new skills to address specific needs of the local population. The partnership decided by consensus that an effort would be made to hire women, including some CHWs, from underrepresented ethnic groups to work on several phases of the research (A4). We hoped that by learning participatory principles and methods, CHWs would use them to pursue social justice (e.g. civic engagement and advocacy) while providing health-related services (Pérez and Martinez, 2008).
Matching partners’ expertise needs and interests
We agreed to involve PSF staff and CHWs in all phases of research, including specification of aims. Several meetings were held which included community residents. Lay and scientific knowledge were exchanged in these meetings and capacity was built to conduct the current and future projects (A2). Through systematized means of communication (e.g. oral, meeting agendas and Memoranda of Understanding), research partners maximized common interests and minimized social and professional differences (A5). We engaged in different types of agreements. Initially, a contractual agreement was signed by the two universities (one in Brazil and another in the USA) stating the commitment of the two key researchers to conducting research in ways that would benefit both universities. The researchers then engaged in negotiations with PSF coordinators, in order to gain access to CHWs. During the negotiation phase, there were both oral and written agreements specifying the nature of data collection and how the data would be used. After the formative research involving in-depth interviews with CHWs, researchers proposed to conduct focus groups to discover how CHWs performed their duties and contributed to PSF outcomes. However, CHWs argued instead that assessing their training needs should be a key focus of the research. They asserted that in-depth interviews should be used to inform the development of a survey to be administered to all CHWs. This would best reveal their training needs (A4). By consensus we agreed to collect survey data from CHWs and also from physicians and nurses (A2). This decision was documented and included in all IRB protocols.
Collaborative research aims and outcomes
As we implemented the IPRF, our research partners agreed to pursue research aims useful to CHWs and the families they served and to build capacity for future research. Researchers proposed to study how CHWs’ knowledge and practice wisdom guided the strategies CHWs used to educate community members about HIV prevention. CHWs argued that research should focus on assessing their training needs and asserted that quantitative data from all workers would best reveal those needs. This difference of opinion was resolved by facilitating communication between 21 health workers, three administrators and university partners. Guided by the IPRF, we discussed the use of research funds, methods and rigor, and the time each partner could dedicate to research. We agreed to collect survey data from CHWs, physicians and nurses. Data that we collected subsequent to IPRF implementation were used to both identify strategies for best practices and to inform CHW training.
Capacity building for research and programs
Our framework helped build capacity by the presence of researchers in the community. By demonstrating an interest in the needs of CHWs and emphasizing the importance of their work, researchers helped elevate their professional status while galvanizing CHWs’ supervisors around CHW training needs. We acknowledge that the presence of researchers in communities is not always welcomed due to histories of abuses and exploitative practices targeting vulnerable populations that have been the subjects of research. However, guided by participatory principles and the IPRF framework, researchers may mitigate the negative perceptions or attitudes that they may initially encounter and successfully form and maintain partnerships.
Guided by the IPRF and using iterative processes, researchers mentored community partners in survey development and data collection (scientific knowledge) while researchers were taught how to interpret community norms, values and needs (local knowledge). In order to create an iterative process, we held multiple in-person meetings involving the US-based researcher and maintained contact via e-mail during the entire project. Ongoing communication within and across steps helped all parties to develop trust and to establish consensus around research methods. Iteration also occurred across participatory steps in that each proposed action was repeated in order to achieve agreed-upon research goals. Each repetition of steps and actions was used as the starting point for the next iteration. By endorsing CHWs’ priorities, researchers helped advance policies and programs. Using the data collected from CHWs, their supervisors revised the content, depth and delivery of training curricula. Subsequent to IPRF implementation, our participatory research project expanded to include two Brazilian towns, and data have been collected from nearly 200 CHWs. These data will form the basis for a grant proposal to develop and test a curriculum for training CHWs.
CONCLUSIONS
The IPRF addresses the critical need for systematizing the development of partnerships between researchers in resource-rich countries and communities in developing countries. Lacking replicable and empirically supported models for establishing international partnerships, the scientific community is only beginning to document the use of CBPR in the global arena. This paper helped close this gap by demonstrating the significance of using a framework, built from participatory steps and actions, in order to facilitate partnership-building between researchers in a resource-rich country and partners in a developing country. This paper shows that formative research helps researchers, practitioners and local political figures develop strategies for accessing gatekeepers and research participants, and identify relevant research topics. Moreover, we recommend that steps and actions of the IPRF be used to evaluate existing CBPR projects. Steps and actions can be used recursively to reassess commitments and assimilate new information.
In the aforementioned example, both the collection and analysis of formative qualitative data were appealing to community-based partners. Indeed, qualitative methods—interviewing, participant observation, focus groups, community mapping and reviewing local surveillance data—allow for exchanges of ideas and dialogue. Using qualitative data in formative research is thus recommended because it allows for more interaction between researchers and community partners. Moreover, qualitative data can be used to develop surveys and provide direction for research that requires complex methods of randomization and intervention testing.
The IPRF has limitations worth mentioning. The IPRF has been implemented in a few different contexts, but has not been fully evaluated in terms of partnership longevity. Even though the partnership described here has lasted many years and continues to thrive, further evaluations of the IPRF will be needed to appraise how useful it is for maintaining partnerships over time, sustainability of community changes and how useful it is for building partnerships to study diseases and conditions other than HIV/AIDS. It is recommended that research partners build on the lessons identified below to test this framework in other international environments. As more partnerships use the IPRF, we will be able to evaluate and improve participatory steps and actions, further standardize the framework, and show the relative impact of each step and set of actions. Though we did not intend to show causation between steps and actions in the IPRF and the participatory outcomes achieved, future research is needed to further demonstrate how the IPRF can be used to build and maintain partnerships in international research contexts.
Lessons learned
International projects often present several challenges highlighted above. We overcame challenges by adhering to the IPRF steps while maintaining a stance of cultural humility (Wallerstein, 1999; Wallerstein et al., 2005). We used ‘member checking’ to regularly ask follow-up questions to our partners about our process of collaboration (Maxwell, 2005). We learned that demonstration of empathy to local residents and integration of local priorities into research agendas helped generate community-defined research and services. Establishing trusting relationships with local communities helped secure funding for further research and inspired local partners to use findings to develop training curricula. It is unwise to launch projects at the ends of politicians’ terms since many programs are funded by the government and run by political appointees. However, seeking advice from gatekeepers may help research partners transcended power differences by developing trust, reciprocity and communication (Christopher et al., 2005; Mosavel et al., 2005; Castleden et al., 2008). We recommend that researchers outline their research agendas, including prior research, time available for international projects and all restrictions from funders and institutions with which they were affiliated. By understanding one another's interests, all partners can establish realistic expectations about research aims (Cargo et al., 2008).
The IPRF can help evaluate existing projects that have not been developed by using IPRF steps and actions. Engaging in the IPRF steps may help research partners redefine partnership goals and research questions. IPRF steps and actions can help new partners develop participatory bonds to maintain trust and continue research-related work. Partners ought to use a Memorandum of Understanding (MOU) in order to outline and specify the roles and responsibilities of all partners. The process of drafting the MOU may prove beneficial to eliciting important information about partners’ expectations and may also help to crystallize partners’ commitments to the project by engaging their participation in articulating their own roles.
It is worth mentioning that the IPRF has been used by other partnerships in different countries. In Mongolia, the application of the IPRF facilitated the training of local partners in randomized control trial procedures and motivational interviewing. As a result, local community providers are delivering evidence-based services. In Kazakhstan, the IPRF helped researchers build a Global Health Research Center and train local staff in research methods and bio-ethics. Through yet another project in Tajikistan, local community members were hired as field workers and research staff was trained in quantitative methods. These partnerships involved in these projects presented their work at the Twelfth World Congress on Public Health, 2008, Istanbul, Turkey and at the Society for Social Work and Research, 2008, Washington, DC, USA (A. Brisson; S. Witte; M. Riedel; L. Gilbert). Box 1 below summarizes key lessons based on the Brazil project and which also reflect the application of IPRF in other countries.
Box 1. Summary lessons learned box: international participatory research framework.
To what extent did the IPRF help accomplish participatory outcomes?
• Contextualizing the host country included learning the local language, historical/political context, cultural/religious norms and sociocultural factors affecting behavior and social structures.
• Identifying collaborators in host country built capacity for long-term research. Politicians provided access to health care systems and community gatekeepers. Knowing local language was helpful for establishing professional and social bonds.
• Seeking advice/endorsement from gatekeepers generated research meaningful to local partners. For example, endorsements of politicians helped access Family Health Program staff that influenced research questions, recruitment and survey development. Some partners doubted researchers’ abilities to empathize with communities. Thus, an informal social style and sharing social support helped us build trust.
• Matching partners’ expertise, needs and interests generated community-focused questions and built capacity for research. Researchers shared knowledge and provided training. This helped partners draw local funding for services and training.
How helpful is it to use the IPRF to evaluate existing projects?
• Steps and actions are recursive and should be revisited to reassess commitments and assimilate new information. Engaging in the IPRF steps may help research partners redefine partnership goals and research questions.
How helpful is the IPRF to partnerships whose configurations have changed?
• IPRF can be used to engage new partners. New researchers and staff often join existing partnerships, and can use the framework to facilitate smooth transitions.
How to draw up the contents of a Memorandum of Understanding (MOU)
• MOU is a formal document describing general and specific ways in which each partner contributes. At a minimum, MOUs should list needs and resources available to partnerships, roles and commitments expressed by, and agreed upon, all partners, main goals of collaboration, a vision statement and the signatures of partners.
REFERENCES
- Alasuutari P., Bickman L., Brannen J., editors. The SAGE Handbook of Social Research Methods. Thousand Oaks, CA: SAGE Publications; 2008. [Google Scholar]
- Baptiste D., Bhana A., Petersen I., McKay M. M., Voisin D., Bell C., et al. Community collaborative youth-focused HIV/AIDS prevention in South Africa and Trinidad: preliminary findings. Journal of Pediatric Psychology. 2006;31:905–916. doi: 10.1093/jpepsy/jsj100. [DOI] [PubMed] [Google Scholar]
- Berkman A., Garcia J., Munoz-Laboy M., Paiva V., Parker R. A critical analysis of the Brazilian response to HIV/AIDS: lessons learned for controlling and mitigating the epidemic in developing countries. Public Health Matters. 2005;95:1162–1172. doi: 10.2105/AJPH.2004.054593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cargo M., Delormier T., Levesque L., Horn-Miller K., McComber A., Macaulay A. C. Can the democratic ideal of participatory research be achieved? An inside look at an academic-indigenous community partnership. Health Education Research. 2008;23:904–914. doi: 10.1093/her/cym077. [DOI] [PubMed] [Google Scholar]
- Cashman S. B., Adeky S., Allen A. J., Corburn J., Israel B. A., Montano J., et al. The power and the promise: working with communities to analyze data, interpret findings, and get to outcomes. American Journal of Public Health. 2008;98:1–11. doi: 10.2105/AJPH.2007.113571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castleden H., Garvin T. Huu-ay-aht First Nation. Modifying photovoice for community-based participatory indigenous research. Social Science and Medicine. 2008;66:1393–1405. doi: 10.1016/j.socscimed.2007.11.030. [DOI] [PubMed] [Google Scholar]
- Christopher S., Burhansstipanov L., Gun-McCormick A. Using a CBPR approach to develop an interviewer training manual with members of the Apsaalooke Nation. In: Israel B. A., Eng E., Schulz A. J., Parker E. A., editors. Methods in Community-based Participatory Research for Health. San Francisco, CA: John Wiley & Sons Inc.; 2005. pp. 128–145. [Google Scholar]
- Creswell J. W. Research Design: Qualitative, Quantitative and Mixed Methods Approach. 2nd edition. Thousands Oaks, CA: Sage Publications; 2009. [Google Scholar]
- Guerin P. B., Allotey P., Elmi F. H., Baho S. Advocacy as a means to an end: assisting refugee women to take control of their reproductive health needs. Women and Health. 2009;43:7–25. doi: 10.1300/J013v43n04_02. [DOI] [PubMed] [Google Scholar]
- Israel B. A., Schulz A. J., Parker E. A., Becker A. B. Review of community-based research: assessing partnership approaches to improve public health. Annual Review of Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- Israel B. A., Schulz A. J., Parker E. A., Becker A. B., Allen A. J., III, Guzman R. J. Critical issues in developing and following community based participatory research principles. In: Minkler M., Wallerstein N., editors. Community Based Participatory Research for Health. San Francisco, CA: Jossey-Bass; 2003. pp. 53–76. [Google Scholar]
- Israel B. A., Eng E., Schulz A. J., Parker E. A. Methods in Community-based Participatory Research for Health. San Francisco, CA: John Wiley & Sons, Inc.; 2005. [Google Scholar]
- Kaiser Reports. The U.S. Global Health Initiative: overview and budget analysis. 2009. Retrieved 15 January 2009, from http://kff.org/globalhealth/8009.cfm .
- Litwak E., Meyer H. A balance theory of coordination between bureaucratic organizations and community primary groups. Administrative Science Quaterly. 1966;11:31–58. [Google Scholar]
- Litwak E., Meyer H. J., Hollister C. D. The role of linkage mechanisms between bureaucracies and families: education and health as empirical cases in point. In: Lievert R. J., Immershein A. W., editors. Power, Paradigms, and Community Research. Beverly Hills, CA: Sage Publications; 1977. pp. 121–152. [Google Scholar]
- Lo B., Bayer R. Establishing ethical trials for treatment and prevention of AIDS in developing countries. British Medical Journal. 2003;327:337–339. doi: 10.1136/bmj.327.7410.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell J. A. Qualitative Research Design: An Interactive Approach. Vol. 41. Thousand Oaks, CA: SAGE Publications; 2005. [Google Scholar]
- McKay M. M., Pinto R. M., Bannon J. W. M., Guillamo-Ramos V. Understanding motivators and challenges to involving urban parents as collaborators in HIV prevention research efforts. Health and Social Work. 2007;5:169–185. doi: 10.1300/J200v05n01_08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministério da Saúde Brazil B. Saúde da familia. 2011 Retrieved 15 January 2011, from http://dtr2004.saude.gov.br/dab/atencaobasica.php . [Google Scholar]
- Minkler M., Wallerstein N. Community-based Participatory Research for Health. San Francisco, CA: Jossey-Bass; 2003. [Google Scholar]
- Mosavel M., Simon C., Stade D., Buchbinder M. Community based participatory research (CBPR) in South Africa: engaging multiple constituents to shape the research question. Social Science and Medicine. 2005;61:2577–2587. doi: 10.1016/j.socscimed.2005.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker R. Building the foundations for the response to HIV/AIDS in Brazil: the development of HIV/AIDS policy, 1982_1996. Debates on Health Issues. 2003;27:143–183. Rio de Janeiro: Centro Brasileiro de Estudos de Saúde. [Google Scholar]
- Pérez L. M., Martinez J. Community health workers: social justice and policy advocates for community health and well-being. American Journal of Public Health. 2008;98:11–14. doi: 10.2105/AJPH.2006.100842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto R. M. Community perspectives on factors that influence collaboration in public health research. Health Education and Behavior. 2009;36:930–947. doi: 10.1177/1090198108328328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto R. M., Schimdt C. N. T., Rodriguesz P. S. O., Solano R. Using principles of community participatory research: groundwork for collaboration in Brazil. International Social Work. 2007;50:53–65. doi: 10.1177/0020872807071482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto R. M., Spector A. Y., Valera P. A. Exploring group dynamics for integrating scientific and experiential knowledge in Community Advisory Boards for HIV research. AIDS Care. 2011;23:1006–1013. doi: 10.1080/09540121.2010.542126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remien R., Bastos F. I., Terto V., Jr, Raxach J. C., Pinto R. M., Parker R. G., et al. Adherence to antiretrovial therapy (ART) in a context of universal access, in Rio de Janeiro, Brazil. AIDS Care. 2007;19:740–748. doi: 10.1080/09540120600842516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teixeira P. R. Universal access to AIDS medicines: the Brazilian response. Debates on Health Issues. 2003;27:184–191. Rio de Janeiro: Centro Brasileiro de Estudos de Saúde. [Google Scholar]
- UNAIDS. 2008 Report on the Global AIDS Epidemic. 2009. from http://www.unaids.org/en/KnowledgeCentre/HIVData/GlobalReport/2008/
- Viswanathan M., Ammerman A., Eng E., Gartlehner G., Lohr K. N., Griffith D., et al. Rockville, MD: U.S. Department of Health and Human Services; 2004. Community-based Participatory Research: Assessing the Evidence. Evidence Report/Technology Assessment No. 99. (AHRQ Publication No. 04–E022–2) [PMC free article] [PubMed] [Google Scholar]
- Wallerstein N. Power between evaluator and community: research relationships within New Mexico's Healthier Communities. Social Science and Medicine. 1999;49:39–52. doi: 10.1016/s0277-9536(99)00073-8. [DOI] [PubMed] [Google Scholar]
- Wallerstein N., Duran B., Minkler M., Foley K. Developing and maintaining partnerships with communities. In: Israel B., Eng E., Schulz A., Parker E., editors. Methods in Community-based Participatory Research for Health. San Francisco: John Wiley & Sons, Inc.; 2005. pp. 31–51. [Google Scholar]
- Wright M. T., Roche B., Von Unger H., Block M., Gardner B. A call for an international collaboration on participatory research in health. Health Promotion International. 2010;25:115–122. doi: 10.1093/heapro/dap043. [DOI] [PubMed] [Google Scholar]