Abstract
Background:
Pre-hypertension is considered as a cardiovascular disease predicator. Management of pre-hypertension is an appropriate objective for clinicians in a wide range of medical centers. Treatment of pre-hypertension is primarily non-pharmacological, one of which is massage therapy that is used to control the BP. This study aimed to evaluate the survival effect of Swedish massage (face, neck, shoulders, and chest) on BP of the women with pre-hypertension.
Methods:
This was a single-blind clinical trial study. Fifty pre-hypertensive women selected by simple random sampling which divided into control and test groups. The test group (25 patients) received Swedish massage 10-15 min, 3 times a week for 10 sessions and the control groups (25 patients) also were relaxed at the same environment with receiving no massage. Their BP was measured before and after each session and 72 h after finishing the massage therapy. Analyzing the data was done using descriptive and inferential statistical methods (Chi- square, Mann-Whitney, paired t-test and Student t-test) through SPSS software.
Results:
The results indicated that mean systolic and diastolic BP in the massage group was significantly lower in comparison with the control group (P < 0.001). Evaluation of durability of the massage effects on BP also indicated that 72 h after finishing the study, still there was a significant difference between the test and control groups in systolic and diastolic BP (P < 0.001).
Conclusions:
Findings of the study indicated that massage therapy was a safe, effective, applicable and cost-effective intervention in controlling BP of the pre-hypertension women and it can be used in the health care centers and even at home.
Keywords: Durability, massage therapy, pre-hypertension
INTRODUCTION
One of the major causes of increase of cardiovascular diseases in the world is the prevalence of hypertension[1,2] which is considered as an important issue in public health and the risk of death all over the world.[3,4] Most of the people would realize High BP when they experience heart attack or stroke and/or diagnosis in a physical examination.[5] Today, in developed countries, one in every three adults has hypertension,[6,7] while approximately, 50 million of the adults (18 years old or more) in the United States are suffering from hypertension.[8,9] According to the statistics, one- fifths of Iranian people (18.6%) over 15 years old are suffering from this disease, which is a high figure.[10] The prevalence of hypertension in studies of other countries, was higher in men but, in the studied researches in Iran, it was higher in women.[11]
Prevalence of hypertension in the urban communities was higher than that of rural communities based on factors such as lifestyle, diet, environmental stresses, and etc.[12]
Prevalence of hypertension in Isfahan also has a high percentage and is unexpected.[13] Obtained statistics in Isfahan in 1997 indicated that prevalence of hypertension among the urban women was more than that in rural women and even urban men.[14]
BP is like a ticking bomb and should be treated seriously. It is a preventable disease.[15]
Recent studies showed that hypertension was not a definite biological process and it can be prevented or postponed through some certain measures.[16]
Public Health Institute of America in the 7th report of Joint National Institute attracted the attention of health staff to two changes; one of them: Developing a new classification of BP range in which pre-hypertensive group should be added to.[17] Previous terms such as “high-normal” which was used in this BP range was not so applicable for the health staff, but they focused on the medical treatment with the new classifications.[18]
If someone undergoes two separate BP control, each control at least two times, and average BP is lower than 140/90 and higher than 120/80, he/she would be placed in pre-hypertension group. Vasan et al. (2001) with a 10-year follow-up of the pre-hypertensive people and comparison of them with people with normal BP announced that the risk of cardiovascular disease in women and men with pre-hypertension was 2.5 and 1.6 times more than normal people, respectively.[19]
Furthermore, Qureshi et al. (2005) found that pre-hypertensive people are 3.5 times at the risk of myocardial infarction and 1.7 times at the risk of coronary disease.[20] Russel et al. also (2004) in a study stated that clients with pre-hypertension allocated 3.4% of the admissions, 6.2% of home nursing care and 8.5% of the deaths.[17] Osborn et al. (2010) stated that these people are two times more at the risk of hypertension than people with normal BP.[21]
Svetkey (2005) believed that clients with hypertension nearly in 19% of the cases, at the 4 subsequent years, would suffer from hypertension with clinical symptoms and this progression depends upon their BP levels. If these people suffer from BP with high pre-hypertension level (systolic = 130-139 and diastolic = 85-89 mm Hg) 43% and if suffer from BP with low pre-hypertension level (systolic = 120-129 and diastolic = 80-84 mm Hg), 20% of them will be placed in the hypertension group at the next 4 years.[19] Kaplan (2009) also pointed out the necessity of follow-up of the people with borderline hypertension that according to the information of the 3rd Summit of National Health and Nutrition, pre-hypertensive people and also those with microalbuminuria are at the risk of early death following cardiovascular diseases.[22]
Parikh (2008) believed those who are diagnosed as pre-hypertension must be the focus of treatment goals to prevent or delay the hypertension spread blast.[23]
Julius et al. (2006) in their studies suggested pharmacological methods for treating pre-hypertension.[24] whereas many researchers with criticizing the researchers who use pharmacological therapy to treat them stated that focusing on the lifestyle and using non-pharmacological methods are the first-line treatment of the hypertensive people.[1,25]
The majority of the physicians recommend changing the life-style and non-pharmacological treatments before prescription of the medications in the BP control.[5,26]
One of the non-pharmacological and life-style-based treatments is the complementary medicine.[21,27] Complementary and alternative medicine therapies have become a common part of health-care for a number of Americans.[28]
According to the studies researches, massage therapy is the most popular among the patients[29] and more researches for exploring its effects is continuing.[30] However, many of the results of the comparative articles indicated that nurses are more competent in control and management of the BP than other health staff team.[31]
Many researchers believed massage is effective on reduction of the systolic and diastolic BP, On the other hand, many studies have examined the durability effects of massage are not paid.
This study aimed to evaluate the survival effect of Swedish massage (face, neck, shoulders, and chest) on BP of the women with pre-hypertension.
METHODS
This was a two-group two-phase single-blind clinical trial study, Iranian Register clinical trial which was done with massage therapy intervention (independent variable) on BP changes (dependent variable). The study population included adult non-pregnant women (18-60 years) referred to Sedighe Tahereh Cardiovascular Center who were at the pre-hypertensive phase and had inclusion criteria. The inclusion criteria were:
Two separate BP measurements, each time at least two times, with the average BP of less than 140/90 and more than 120/80 mm Hg
Lack of diseases affecting the BP
Lack of skin disease in the massage area
Lack of taking medication affecting the BP
No specific diet, no obesity
No severe or acute stress and lack of using relaxing techniques.
After obtaining the written informed consent, all the subjects filled in the demographic data forms. The study subjects of control group were ensured that provided with effectiveness of the intervention and their willingness, massage therapy would also be done on them. They were asked not to change their life-style during the study and continue their daily and routine habits, work out and diet. The effective variable on BP were controlled as much as possible; however, individual differences, incidents and daily stress and also the way individuals adapted themselves with life affairs were the uncontrollable variables of the study.
The samples were selected by the simple sampling method. Therefore, they randomly divided into test and control groups. To do so, some cards written by control and test on were put in a box and they were asked to pick one, and consequently, the subjects with control cards and test cards were placed into the control and intervention groups, respectively. In the present study, by massage therapy we meant Swedish massage which was conducted using non-aromatic topical lotion on face, neck, shoulders and upper chest using superficial and deep stroking, three times a week (morning to noon, 8 to 12 A.M.) each 10-15 minutes for 10 sessions for 3.5 weeks in the supine state. One of the researchers sat near the sample and her hand was parallel to the heart; she measured and recorded the BP of the client form the right hand before and after each intervention in each session. The control group had all the criteria of the test group except receiving massage. They, during the massage therapy of the test group, lied down on the bed with the arbitrary condition, with deep breath, eyes closed and relaxation of the muscle. In addition, to assess durability of the intervention effect, 72 h after the study, all the study samples were called again to check their BP for the last time.
The data of the present study were collected through discussion, case studies and BP measurements. A Richter sphygmomanometer (made in: England) and a standard Littmann® stethoscope (made in: USA) which their reliability and validity had been confirmed and calibrated at the beginning and middle of the study were used by the researcher who was unaware of the samples, group (test or control).
Measurement was done with respect to the American Heart Association suggested tips to accurately measure the BP. Furthermore, demographic data of the samples such as age, educational level, occupation, marital status, and also, menstrual status and their height and weight were recorded. In order to estimate BMI, a unit of weight and a unit of meter were used; their reliability and validity had been confirmed and were similar for all the samples. In order to achieve study results, collected data were encoded and analyzed by SPSS software version 16. To do so, descriptive and inferential statistics methods were used. The obtained data were evaluated through descriptive statistics such as frequency, mean and standard deviation and also, inferential statistics such as Chi-square, Mann-Whitney, Fisher's exact test, paired t-test and independent t-test [Figure 1].
Figure 1.
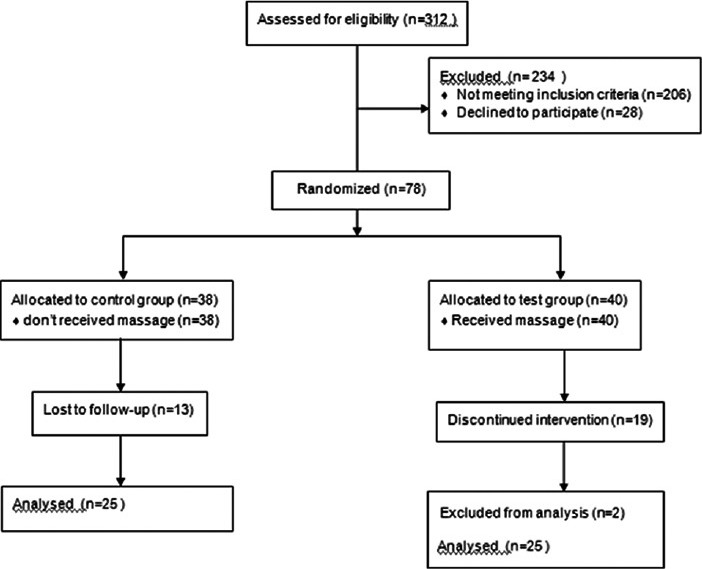
Consort of sampling
RESULTS
Reviewing the obtained results in the two groups indicated that there was no significant difference in terms of demographic data, menstrual status, and BMI between the two groups (P > 0.05).
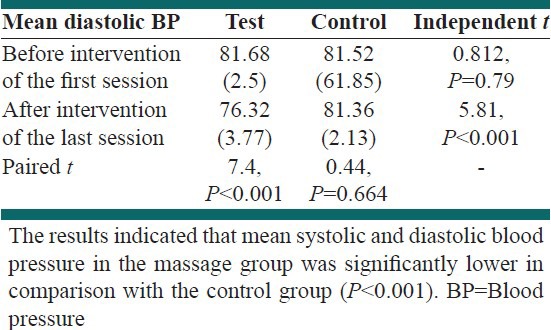
The objective-based results are shown in the Tables 1-3.
Table 1.
Comparing the average systolic blood pressure before and after the intervention in the test and control groups
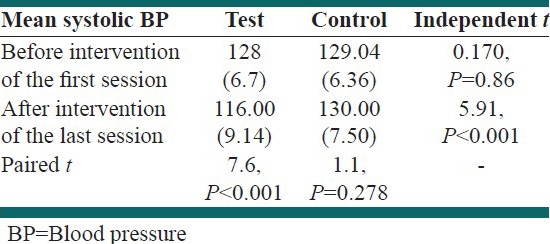
Table 3.
Comparing the average systolic and diastolic blood pressure in the test and control groups 72 h after the study
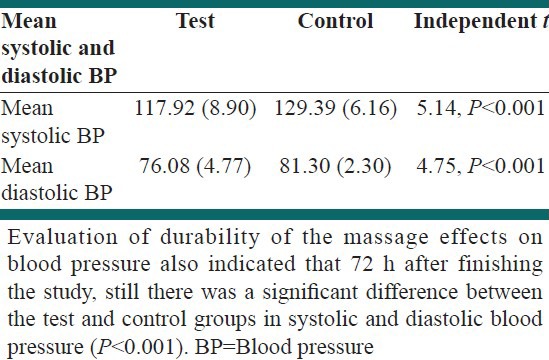
Table 2.
Comparing the average diastolic blood pressure before and after the intervention in the test and control groups
DISCUSSION
Generally, during 10 sessions of the intervention, average systolic and diastolic changes in the test group in comparison with the control group in this study showed a significant difference (P < 0.001).
Three days after the study, still there was a significant difference between the test and control groups in systolic and diastolic BP (P < 0.001).
This indicates that the effects of massage for at least 3 days after the intervention will remain.
Olney's study (2005) showed significant differences in systolic and diastolic BP between the two groups 48 h after the study.[9]
Many of the researchers also have considered the slight BP reduction worthwhile and believed it can cause immunization from the side effects. Now, according to the obtained findings of the present study, it can be concluded that massage therapy, regardless of its unknown mechanism can significantly reduce the BP of the clients and prevent from its side effects; so that average systolic and diastolic BP from the pre-hypertension range from the beginning of the study have been led to the normal BP. Furthermore, the effects of massage for at least 3 days after the intervention will remain. Therefore, the researchers introduced the massage therapy as an effective nursing intervention on adjusting BP of the pre-hypertensive clients.
Suggestion for further researches
It is suggested that the present study comparatively be repeated in men and women, in pre-hypertensive people and those with hypertension and also, the sustainability and durability of massage therapy effects on the BP of the pre-hypertensive clients at different times after the intervention be evaluated.
ACKNOWLEDGMENT
I thank all the clients and also employees at the Sedighe Tahereh Cardiovascular Center who co-operated with me.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 2.Hernandez-Reif M, Field T, Krasnegor J, Hossain Z, Theakston H, Burman I. High blood pressure and associated symptoms were reduced by massage therapy. J Bodyw Mov Ther. 2000;4:31–8. [Google Scholar]
- 3.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: Analysis of worldwide data. Lancet. 2005;365:217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 4.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ Comparative Risk Assessment Collaborating Group. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–60. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 5.Smeltzer SC, Bare BG, Hinkle JL, Cheever KH. Brunner and Suddarth's Textbook of Medical-Surgical Nursing. 11th ed. Philadelphia: Lippincott Williams and Wilkins; 2008. Chapter: Assessment and management of patients with hypertension; p. 1022. [Google Scholar]
- 6.Lewis SM, Heitkemper MM, Bucher L, O’Brien PG. Medical-surgical Nursing: assessment and Management of Clinical Problems. 7th ed. Philadelphia: Mosby Elsevier; 2007. Chapter: nursing management hypertension; p. 761. [Google Scholar]
- 7.Kaye AD, Kaye AJ, Swinford J, Baluch A, Bawcom BA, Lambert TJ, et al. The effect of deep-tissue massage therapy on blood pressure and heart rate. J Altern Complement Med. 2008;14:125–8. doi: 10.1089/acm.2007.0665. [DOI] [PubMed] [Google Scholar]
- 8.Black JM, Hawks JH. Medical-Surgical Nursing: Clinical Management for Positive Outcomes. 8th ed. Philadelphia: Saunders/Elsevier; 2009. Chapter: Assessment of the cardiac system; p. 1354. [Google Scholar]
- 9.Olney CM. The effect of therapeutic back massage in hypertensive persons: A preliminary study. Biol Res Nurs. 2005;7:98–105. doi: 10.1177/1099800405280827. [DOI] [PubMed] [Google Scholar]
- 10.Khosravi AR, Mohammadi Fard N, Shahrokhi SH, Shirani SH, Ansari R. Drugs to patients with hypertension in central areas of Iran. J Isfahan Med School. 2004;22:100–8. [Google Scholar]
- 11.Azizi A, Abbasi MR, Abdoli GR. The prevalence of hypertension and its relationship with age, sex and Body Mass Index in people over 15 years the population covered by community based medical education arena Kermanshah in 2003. J Endocrinol Metab. 2008;10:323–31. [Google Scholar]
- 12.Das SK, Sanyal K, Basu A. Study of urban community survey in India: Growing trend of high prevalence of hypertension in a developing country. Int J Med Sci. 2005;2:70–8. doi: 10.7150/ijms.2.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yosefei H. MSc Thesis. Tehran: Tarbiat Modares University; 1994. Effect of nonpharmacologic methods of reducing blood pressure in of high blood pressure patients. [Google Scholar]
- 14.Delavari AR, Hori N, Alikhani S, Ghoya MM, Mahdavi A, Hosseini SM, et al. Prevalence of hypertension in rural and urban population of over 20 years in 2004. J Mazandaran Univ Med Sci. 2007;17:79–86. [Google Scholar]
- 15.National Association of Iranian Students. One billion of high blood pressure patients. 2007. Available from: http://www.Daneshju.ir .
- 16.Cohen GD. Promoting mental health, treating mental illness. Broadening the focus on intervention. Geriatrics. 2002;57:47–8. [PubMed] [Google Scholar]
- 17.Russell LB, Valiyeva E, Carson JL. Effects of prehypertension on admissions and deaths: A simulation. Arch Intern Med. 2004;164:2119–24. doi: 10.1001/archinte.164.19.2119. [DOI] [PubMed] [Google Scholar]
- 18.Svetkey LP. Management of prehypertension. Hypertension. 2005;45:1056–61. doi: 10.1161/01.HYP.0000167152.98618.4b. [DOI] [PubMed] [Google Scholar]
- 19.Vasan RS, Larson MG, Leip EP, Evans JC, O’Donnell CJ, Kannel WB, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345:1291–7. doi: 10.1056/NEJMoa003417. [DOI] [PubMed] [Google Scholar]
- 20.Qureshi AI, Suri MF, Kirmani JF, Divani AA, Mohammad Y. Is prehypertension a risk factor for cardiovascular diseases? Stroke. 2005;36:1859–63. doi: 10.1161/01.STR.0000177495.45580.f1. [DOI] [PubMed] [Google Scholar]
- 21.Osborn KS, Wraa CE, Watson AB. Medical Surgical Nursing: Preparation for Practice. Boston: Pearson; 2010. Chapter: Management of hypertension; p. 489. [Google Scholar]
- 22.Kaplan NM, Bakris GL, Sheridan A, Rose BD. Prehypertension and borderline hypertension. 2009. [Last cited 2010 Jun 17]. Available from: http://www.uptodate.com .
- 23.Parikh NI, Pencina MJ, Wang TJ, Benjamin EJ, Lanier KJ, Levy D, et al. A risk score for predicting near-term incidence of hypertension: The Framingham Heart Study. Ann Intern Med. 2008;148:102–10. doi: 10.7326/0003-4819-148-2-200801150-00005. [DOI] [PubMed] [Google Scholar]
- 24.Julius S, Nesbitt SD, Egan BM, Weber MA, Michelson EL, Kaciroti N, et al. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N Engl J Med. 2006;354:1685–97. doi: 10.1056/NEJMoa060838. [DOI] [PubMed] [Google Scholar]
- 25.Schunkert H. Pharmacotherapy for prehypertension – Mission accomplished? N Engl J Med. 2006;354:1742–4. doi: 10.1056/NEJMe068057. [DOI] [PubMed] [Google Scholar]
- 26.Benson H, Klipper MZ. The Relaxation Response. Ohio: Avon; 2000. Chapter: Life style; p. 113. [Google Scholar]
- 27.Kamalifard M, Shahnazi M, Melli MS, Allahverdizadeh Sh, Tora-by Sh, Ghahvechi A. The efficacy of massage therapy and breathing techniques on pain intensity and physiological responses to labor pain. J Caring Sci. 2012;1:73–8. doi: 10.5681/jcs.2012.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bauer BA, Cutshall SM, Wentworth LJ, Engen D, Messner PK, Wood CM, et al. Effect of massage therapy on pain, anxiety, and tension after cardiac surgery: A randomized study. Complement Ther Clin Pract. 2010;16:70–5. doi: 10.1016/j.ctcp.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 29.Buttagat V, Eungpinichpong W, Chatchawan U, Kharmwan S. The immediate effects of traditional Thai massage on heart rate variability and stress-related parameters in patients with back pain associated with myofascial trigger points. J Bodyw Mov Ther. 2011;15:15–23. doi: 10.1016/j.jbmt.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 30.American Massage Therapy Association. Demand for massage therapy: use and acceptance increasing. 2004. Available from: http://www.amtamassage.org .
- 31.McClellan WM, Craxton LC. Improved follow-up care of hypertensive patients by a nurse practitioner in a rural clinic. J Rural Health. 1985;1:34–41. doi: 10.1111/j.1748-0361.1985.tb00125.x. [DOI] [PubMed] [Google Scholar]


