Abstract
Background:
Increased intra-abdominal pressure (IAP) results in dysfunction of vital organs. The aim of the present study was to evaluate the effect of mechanical ventilation mode on IAP.
Methods:
In a cohort study, a total of 60 patients aged 20-70 years who were admitted to the ICU and underwent mechanical ventilation were recruited. Mechanical ventilation included one of the three modes: Biphasic positive airway pressure (BIPAP) group, synchronize intermittent mandatory ventilation (SIMV) group, or continuous positive airway pressure (CPAP) group. For each patient, mechanical ventilation mode and its parameters, blood pressure, SpO2, and status of tube feeding and IAP were recorded.
Results:
Our findings indicate that the study groups were not significantly different in terms of anthropometric characteristics including age (64.5 ± 4, P = 0.1), gender (male/female 31/29, P = 0.63), and body mass index (24 ± 1.2, P = 0.11). Increase IAP was related to the type of respiratory mode with the more increased IAP observed in SIMV mode, followed by BIPAP and CPAP modes (P = 0.01). There were significant correlations between increased IAP and respiratory variables including respiratory rate, pressure support ventilation, and inspiratory pressure (P < 0.05). Tube feeding tolerance through NG-tube was lower in SIMV group, followed by BIPAP and CPAP groups (P < 0.05).
Conclusions:
There is a significant relationship between respiratory modes and IAP; therefore, it is better to utilize those types of mechanical ventilation like CPAP and BIPAP mode in patients who are prone to Intra-abdominal hypertension.
Keywords: Abdominal compartment syndrome, intra-abdominal pressure, mechanical ventilation mode
INTRODUCTION
Intra-abdominal pressure (IAP) and its impact on abdominal viscera has been a focus of interest for researchers as far back as 19th century.[1,2] The term abdominal compartment syndrome (ACS) is coined to describe the pathophysiologic manifestations secondary to increased IAP.[3,4,5] Many studies have suggested that IAP of even 10 mmHg may have injurious impacts on organ functions.[6,7] IAP of over 12 mmHg plus ischaemia in at least one organ is termed intra-abdominal hypertension (IAH).[2,8,9,10,11,12,13,14] Increased IAP plays a pivotal role in the development of multi-organ dysfunction syndrome, which is a major cause of mortality in intensive care unit (ICU).[15,16] The World Society of the Abdominal Compartment Syndrome (WSACS) recommends baseline IAP measurements for all patients on entry into ICU, as well as in patients with at least 2 risk factors for IAH.[8,17,18,19] In the Shamimi study, it was shown that routine measurement of IAP is necessary in high-risk patients.[9] Also, in Sheikhei study, implementing education on methods of early diagnosis of IAP for medical team was stressed.[10] The present study investigated the relationship between increased IAP and type of mechanical ventilation, including the most commonly used types of continuous positive airway pressure (CPAP), biphasic positive airway pressure (BIPAP), and synchronize intermittent mandatory ventilation (SIMV), with their respective parameters to decrease IAH and ACS incidence in susceptible patients.
METHODS
After approval of University Ethics Committee and acquisition of informed consent from patients’ relatives, cases who were admitted to ICU were recruited into this Cohort study from November 2010 through November 2011. Inclusion criteria included patients aged 20-70 years and requiring mechanical ventilation in ICU. Patients who were not included into the study were patients with abdominal or chest trauma, patients with intra-abdominal pathologies, patients who had received more than 10 units of red blood cells or more than 5 liters of intravenous liquids over the last 24 h, patients with sepsis or hepatic, pulmonary or renal dysfunction, body mass index (BMI) of over 30, and patients in positions other than supine. With a review of previous studies on medical database, we calculated a sample size of at least 54 patients, (α = 0.05, β = 10%, study power 90%). Thus, 60 patients were recruited through convenience sampling from patients under mechanical ventilation in ICU of Emam Reza Hospital and with respect to patients’ needs for ventilator support (in other words respiratory failure of patients) including SIMV, BIPAP, and CPAP mechanical ventilation mode. After 24 h, we measured patients’ IAP. Since previous studies[6,7] as well as the WSACS guidelines[8] recommend indirect measurement of intra-abdominal pressure intravesically using a Foley catheter, we used it as the standard method. The procedure is quite safe and does not increase the risk of urinary infection.[20,21] First, the patient's bladder was voided and the urine bag was detached from Foley catheter. Subsequently, according to the current guidelines,[8] the bag was filled with 25 cc normal saline and attached to Foley catheter via a serum microset. The zero point was set at the level of midaxillary line. One minute delay was provided to allow the bladder muscles to relax, and then the fluid level was read at the end of expiration to ensure relaxation of abdominal muscles. The procedure was repeated three times for each patient with 30 min time interval and the mean of these numbers divided by 1.36 (to convert cmH2O to mmHg) was recorded as the patient's IAP [Figure 1]. Moreover, anthropometric characteristics of patients (i.e., age, sex, BMI) as well as their blood pressure, SpO2, and status of tube feeding were recorded every 30 min on data sheets.
Figure 1.
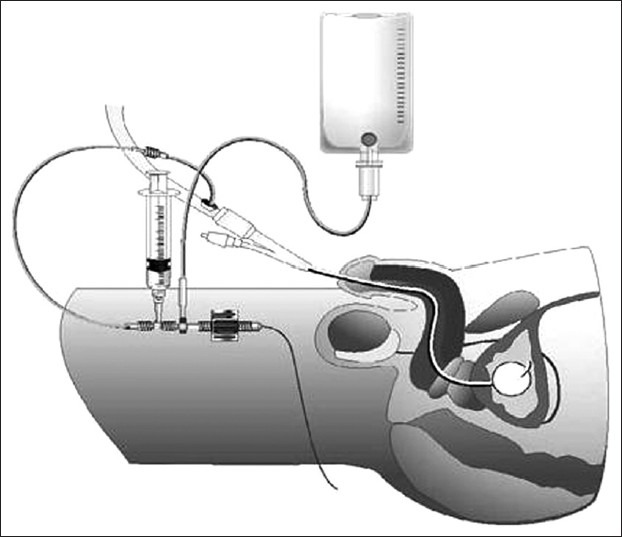
Measurement of intra-abdominal pressure
Pearson's correlation coefficient was used to investigate any relationship between IAP as the dependent variable and respiratory parameters of ventilator as independent variables. Furthermore, ANOVA and Chi-square tests were utilized to compare the quantitative and qualitative anthropometric characteristics among the three groups respectively. Those parameters with greatest impact on the three groups were determined using Post hoc test. Fischer's exact test was used to assess the expected frequencies.
Statistical analysis was performed on SPSS software version 18. Quantitative data are expressed as mean ± standard deviation and qualitative data are expressed as frequency. Frequency data are expressed as count (%) and P < 0.05 were considered significant.
RESULTS
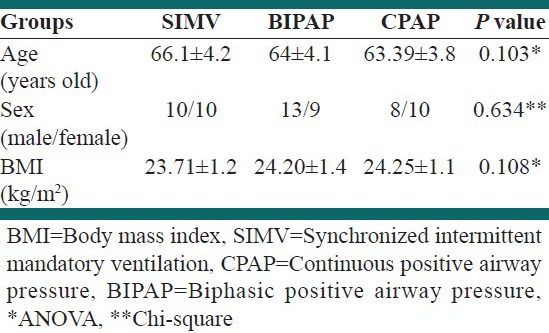
This was a cohort study on 60 patients, consisting of (36.7%) in BIPAP group, (33.3%) in SIMV group and (30%) in CPAP group. Patients comprised of 31 (51.7%) men and 29 (48.3%) women (P = 0.643). The recruited patients’ age ranged from 53-70 years, with a mean age of 64.5 ± 4.2 years (P = 0.103). The mean BMI of patients indicated no significant difference among the three groups (P = 0.257) [Table 1].
Table 1.
Anthropometric characteristics of three groups
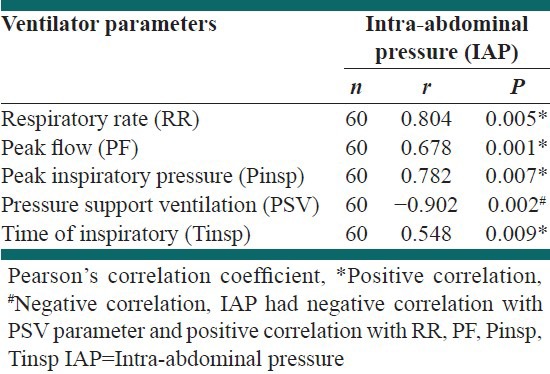
Our findings indicate that increased IAP and decreased APP were related to type of respiratory mode [Table 2]. Also, correlation of IAP with pressure support ventilation (PSV) was negative [Table 3]. NG-Tube feeding tolerance (gastric residual volume lower than 250 cc during lavage),[22] was better in CPAP group than others [Table 2]. The mean arterial pressure of patients did not show any significant difference among the three groups [Table 2].
Table 2.
Comparison of evaluated variables between three ventilator modes
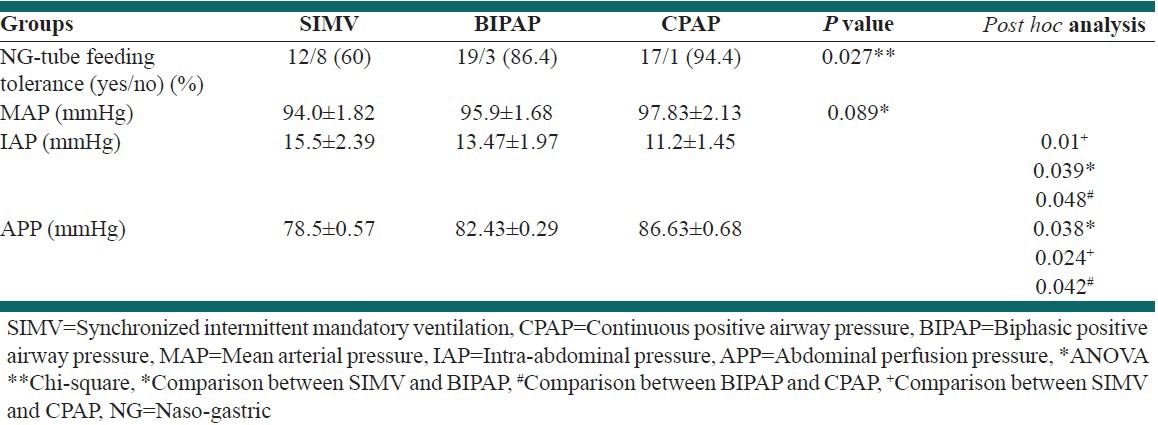
Table 3.
Correlation between ventilator parameters and intra-abdominal pressure in all patients
DISCUSSION AND CONCLUSION
IAP is an important physiologic parameter for patients admitted to ICU, and its measurement is becoming more frequent in many ICUs.[23] Previous studies have revealed the impact of increased IAP on respiratory function of ill patients.[24] In the present study, we investigated the effect of mechanical ventilation mode on increased IAP to determine the optimal mechanical ventilation mode with the optimal settings on ventilator for patients susceptible to increased IAP. In our study, the anthropometric parameters of age, gender, and BMI were not significantly different among the three groups, and since our study population had normal distribution, these factors could not affect our findings [Table 1]. On the other hand, a study by Walker et al. conducted on 14 patients consisted of 93% male patients and 7% female patients.[12] Previous studies have suggested a correlation between increased IAP and BMI.[25] Since previous studies have established the impact of PEEP on increased IAP, we set the PEEP value equal to 5 for all our patients.[23]
Our findings indicate that increased IAP is mostly affected by SIMV, followed by BIPAP and CPAP. Similarly, peak flow (a parameter used in SIMV mode) showed positive correlation with increased IAP. Also, the positive correlation between Peak inspiratory pressure (Pinsp) (a parameter used in BIPAP mode) and increased IAP accounts for the greater liability of BIPAP compared to CPAP.
Our study demonstrates that PSV has a negative correlation with IAP in different respiratory modes, as with increasing PSV, the IAP is less likely to increase. Moreover, as mentioned above, the SIMV, BIPAP, and CPAP modes had the greatest impact on increased IAP, in decreasing order. On the other hand, the PSV value is highest in CPAP, BIPAP, and SIMV modes, in decreasing order. Previous studies have indicated that PSV improves oxygenation and increases the mixed venous blood oxygen, which may be a result of reduced oxygen consumption by respiratory muscles. Moreover, PSV corrects blood redistribution through improving the ventilation to perfusion ratio in different regions of the lung.[26,27,28]
Two studies by Bailey and Malbrain et al. revealed that increased IAP leads to tissue ischemia in all abdominal viscera except the adrenals. Human studies are rare; nevertheless, animal studies have been suggested that when IAP reaches 20 mmHg, perfusion of intestinal mucosa is compromised, thus jeopardizing the physiologic function of intestinal mucosa as a protective barrier, resulting in infiltration of colon bacteria into bloodstream and septic shock, as well as reduction of nutrient absorption.[2,6] In our study, tube feeding was better tolerated in CPAP, BIPAP, and SIMV groups, in decreasing order. This may be partially accounted for the equation APP = MAP-IAP, where abdominal perfusion pressure (APP) is the difference between mean arterial pressure (MAP) and IAP. Since MAP was not significantly different among our three groups, the APP is only related to IAP changes. Better perfusion of the gastrointestinal tract translates as better absorption of nutrients, thus accounting for the difference in tube feeding tolerance among the three groups.[8] In addition, some studies suggest that the digestive tract is most sensitive to IAH and its injury precedes cardiac, pulmonary, and renal symptoms [Table 2].[29,30]
Our findings could indicate a significant relationship between respiratory modes and changes in IAP, as well as between ventilator settings (i.e., respiratory rate, PSV, Pinsp, and peak flow) and increased IAP. Therefore, it could be advisable to use those respiratory modes and ventilator settings which are least likely to increase IAP in patients who are at risk of IAH or those who do not tolerate tube feeding [Table 3].
The most important limitation of our present study is the fact that it has only addressed SIMV, BIPAP and CPAP modes in adults, and its results cannot be applied to other modes and children. Thus, we recommend future studies to deal with these issues.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Van Hee R. Historical highlights in concept and treatment of abdominal compartment syndrome. Acta Clin Belg Suppl. 2007:9–15. [PubMed] [Google Scholar]
- 2.Bailey J, Shapiro MJ. Abdominal compartment syndrome. Crit Care. 2000;4:23–9. doi: 10.1186/cc646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kimball EJ, Rollins MD, Mone MC, Hansen HJ, Baraghoshi GK, Johnston C, et al. Survey of intensive care physicians on the recognition and management of intra-abdominal hypertension and abdominal compartment syndrome. Crit Care Med. 2006;34:2340–8. doi: 10.1097/01.CCM.0000233874.88032.1C. [DOI] [PubMed] [Google Scholar]
- 4.Sugerman HJ. Effects of increased intra-abdominal pressure in severe obesity. Surg Clin North Am. 2001;81:1063–75. doi: 10.1016/s0039-6109(05)70184-5. [DOI] [PubMed] [Google Scholar]
- 5.Sanchez NC, Tenofsky PL, Dort JM, Shen LY, Helmer SD, Smith RS. What is normal intra-abdominal pressure? Am Surg. 2001;67:243–8. [PubMed] [Google Scholar]
- 6.Malbrain ML, Deeren D, De Potter TJ. Intra-abdominal hypertension in the critically ill: It is time to pay attention. Curr Opin Crit Care. 2005;11:156–71. doi: 10.1097/01.ccx.0000155355.86241.1b. [DOI] [PubMed] [Google Scholar]
- 7.Fusco MA, Martin RS, Chang MC. Estimation of intra-abdominal pressure by bladder pressure measurement: Validity and methodology. J Trauma. 2001;50:297–302. doi: 10.1097/00005373-200102000-00016. [DOI] [PubMed] [Google Scholar]
- 8.World Society of the Abdominal Compartment Center. [Last accessed on 2010 Feb 04]. Available from: http://www.wsacs.org .
- 9.Shamimi K, Aminian A, Moazami F, Jalali M. Intra-abdominal hypertension and abdominal compartment syndrome in the surgical intensive care unit of Imam Khomeini Hospital; a 12 months study. Tehran Univ Med J. 2007;64:76–83. [Google Scholar]
- 10.Sheikhei RA, Heydari M, Shahbazi S. Comparison of intra-abdominal pressure measurment and physical exam for diagnosis of surgery indication in patients with abdominal compartment syndrome due to blunt trauma. Kerman Univ Med J. 2011;18:271–8. [Google Scholar]
- 11.Smith C, Cheatham ML. Intra-abdominal hypertension and abdominal compartment syndrome in the medical patient. Am Surg. 2011;77:S67–71. [PubMed] [Google Scholar]
- 12.An G, West MA. Abdominal compartment syndrome: A concise clinical review. Crit Care Med. 2008;36:1304–10. doi: 10.1097/CCM.0b013e31816929f4. [DOI] [PubMed] [Google Scholar]
- 13.Kim IB, Prowle J, Baldwin I, Bellomo R. Incidence, risk factors and outcome associations of intra-abdominal hypertension in critically ill patients. Anaesth Intensive Care. 2012;40:79–89. doi: 10.1177/0310057X1204000107. [DOI] [PubMed] [Google Scholar]
- 14.Gallagher JJ. How to recognize and manage abdominal compartment syndrome. Nurs Manage. 2004;(Suppl):36–42. doi: 10.1097/00152193-200405001-00011. [DOI] [PubMed] [Google Scholar]
- 15.Cheatham ML. Abdominal compartment syndrome: pathophysiology and definitions. Scand J Trauma Resusc Emerg Med. 2009;17:10. doi: 10.1186/1757-7241-17-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ivatury RR. Abdominal compartment syndrome: A century later, isn’t it time to accept and promulgate? Crit Care Med. 2006;34:2494–5. doi: 10.1097/01.CCM.0000235680.83667.EE. [DOI] [PubMed] [Google Scholar]
- 17.Shah SK, Jimenez F, Letourneau PA, Walker PA, Moore-Olufemi SD, Stewart RH, et al. Strategies for modulating the inflammatory response after decompression from abdominal compartment syndrome. Scand J Trauma Resusc Emerg Med. 2012;20:25. doi: 10.1186/1757-7241-20-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luckianow GM, Ellis M, Governale D, Kaplan LJ. Abdominal compartment syndrome: Risk factors, diagnosis, and current therapy. Crit Care Res Pract 2012. 2012 doi: 10.1155/2012/908169. 908169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Atighechian G, Asefzadeh S, Yarmohammadian MH, Nikpey A. Clinical risk assessment in intensive care unit by FMEA. Int J Prev Med. 2013 In press. [PMC free article] [PubMed] [Google Scholar]
- 20.Cheatham ML, Fowler J. Measuring intra-abdominal pressure outside the ICU: Validation of a simple bedside method. Am Surg. 2008;74:806–8. [PubMed] [Google Scholar]
- 21.Gudmundsson FF, Viste A, Gislason H, Svanes K. Comparison of different methods for measuring intra-abdominal pressure. Intensive Care Med. 2002;28:509–14. doi: 10.1007/s00134-001-1187-0. [DOI] [PubMed] [Google Scholar]
- 22.Mallampalli A, McClave SA, Snider HL. Defining tolerance to enteral feeding in the intensive care unit. Clin Nutr. 2000;19:213–5. doi: 10.1054/clnu.2000.0137. [DOI] [PubMed] [Google Scholar]
- 23.Malbrain ML, Cheatham ML, Kirkpatrick A, Sugrue M, Parr M, De Waele J, et al. Results from the international conference of experts on intra-abdominal hypertension and abdominal compartment syndrome. I. Definitions. Intensive Care Med. 2006;32:1722–32. doi: 10.1007/s00134-006-0349-5. [DOI] [PubMed] [Google Scholar]
- 24.Valenza F, Chevallard G, Porro GA, Gattinoni L. Static and dynamic components of esophageal and central venous pressure during intra-abdominal hypertension. Crit Care Med. 2007;35:1575–81. doi: 10.1097/01.CCM.0000266589.58118.F0. [DOI] [PubMed] [Google Scholar]
- 25.Wilson A, Longhi J, Goldman C, McNatt S. Intra-abdominal pressure and the morbidly obese patients: The effect of body mass index. J Trauma. 2010;69:78–83. doi: 10.1097/TA.0b013e3181e05a79. [DOI] [PubMed] [Google Scholar]
- 26.Reintam Blaser A, Parm P, Kitus R, Starkopf J. Risk factors for intra-abdominal hypertension in mechanically ventilated patients. Acta Anaesthesiol Scand. 2011;55:607–14. doi: 10.1111/j.1399-6576.2011.02415.x. [DOI] [PubMed] [Google Scholar]
- 27.Aghadavoudi O, Kamran M, Masoudifar M. Comparison of two modes of ventilation after fast-track cardiac surgery: Adaptive support ventilation versus synchronized intermittent mandatory ventilation. Pak J Med Sci. 2012;28:303–8. [Google Scholar]
- 28.Krebs J, Pelosi P, Tsagogiorgas C, Alb M, Luecke T. Effects of positive end-expiratory pressure on respiratory function and hemodynamics in patients with acute respiratory failure with and without intra-abdominal hypertension: A pilot study. Crit Care. 2009;13:R160. doi: 10.1186/cc8118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Malbrain ML, Vidts W, Ravyts M, De Laet I, De Waele J. Acute intestinal distress syndrome: The importance of intra-abdominal pressure. Minerva Anestesiol. 2008;74:657–73. [PubMed] [Google Scholar]
- 30.Björck M, Wanhainen A. Nonocclusive mesenteric hypoperfusion syndromes: Recognition and treatment. Semin Vasc Surg. 2010;23:54–64. doi: 10.1053/j.semvascsurg.2009.12.009. [DOI] [PubMed] [Google Scholar]


