Abstract
Background:
Patients with diabetes experience some level of emotional distress varying from disease-specific distress to general symptoms of anxiety and depression. Since empirical data about symptom distress in relation to diabetes are sparse in Iran, this study was designed to assess the diabetes-specific distress in Iranian population.
Methods:
Persian version of Diabetes Distress Scale (DDS) questionnaire was completed by volunteer outpatients on a consecutive basis between February 2009 and July 2010, in Endocrine Research Center (Firouzgar Hospital). Then, scheduled appointments were made with a psychiatrist in the same week following completion of the questionnaire. The psychiatrist was not aware about the results of this questionnaire and patients were interviewed based on DSM-IV criteria.
Results:
One hundred and eighty-five patients completed the questionnaire and were interviewed by a psychiatrist. Fifty-two percent of the patients were females. The mean age was 56.06 (SD=9.5) years and the mean of duration of diabetes was 9.7 (SD=7.3) years. Sixty-five (35%) had distress. Among the patients with distress, 55% were females and 64% had lower grade of education. Eighty patients were diagnosed as having Major Depressive Disorder. There was a relation between Emotional Burden subscale and age (P=0.004), employment status (P=0.03), and also diabetes duration (P=0.02). The physician-related distress subscale was also related to the type of medication (P=0.009) and marital status (P=0.01). It has been shown that the regimen-related distress subscale was also related to age (P=0.003) and duration of diabetes (P=0.005).
Conclusions:
High prevalence rate of distress in the study highlights the significance of the need for identifying distress and also other mental health conditions in patients with diabetes in order to take collaborative care approaches.
Keywords: Type 2 diabetes, distress, depression, anxiety
INTRODUCTION
Type 2 diabetes mellitus (DM) is a disease with an increasing prevalence worldwide.[1,2,3] This metabolic disease is one of the most common endocrine disorders affecting almost 6% of the world's population.[4] The prevalence of type 2 DM ranges from 1.3 to 14.5% in Iran.[5,6] Emotional problems such as clinical depression and diabetes-specific distress are common in patients with type 2 DM, but often remain unrecognized and thus untreated.[7] These lead to poor disease management,[8] higher healthcare costs,[9] more days of missed work,[10] and mortality.[11]
It has been documented that diabetes distress, defined as patient concerns about disease management, support, emotional burden, and access to care, is an important condition distinct from depression.[12]
Previous studies have shown that most patients with diabetes who display high levels of depressive affect are not necessarily clinically depressed;[13,14] instead, they experience high levels of emotional distress stemming from concerns and worries associated with their diabetes and its management.[13,15]
Although there are a few reports about depression in patients with diabetes in Iran,[16] to our best knowledge, little is known about diabetes-related distress in patients with diabetes in Iran.
Therefore, the aim of this study was to determine diabetes-specific distress in patients with type 2 DM in Iranian population.
METHODS
This cross-sectional study was conducted at Institute of Endocrinology and Metabolism (IEM) affiliated to Tran University of Medical Sciences, Tehran, Iran. Ethics approval was obtained from the Ethics’ Board at IEM. Outpatients who attended diabetes specialty clinics at IEM were recruited on a consecutive basis between February 2009 and July 2010. Inclusion criteria included patients with type 2 diabetes, who could fluently read and speak Persian, and who had no severe diabetes complications and no history of psychological disorders. The study design was explained to all patients and informed consent was obtained.
We employed Diabetes Distress Scale (DDS) for this study. The DDS consists of 17 questions and comprises four domains: a) emotional burden (EB), b) physician-related distress (PD), c) regimen-related distress (RD), and d) interpersonal distress (ID). It yields a total diabetes distress scale score plus four subscale scores, each addressing a different kind of distress. The DDS is a 17-item measure (DDS17) that uses a Likert scale, with each item scored from 1 (no distress) to 6 (serious distress) concerning distress experienced over the last month.[17]
Using a standard “forward-backward” translation procedure, the English language version of the questionnaire (DDS) was translated into Persian (Farsi). Pilot test showed a statistically significant reliability (Cronbach's alpha = 0.91().
The details of the study were explained to patients by a trained nurse. Volunteer patients completed the DDS questionnaire. Then, scheduled appointments were made with a psychiatrist in the same week following completion of the questionnaire. The psychiatrist was not aware about the results of this questionnaire and patients were interviewed based on DSM-IV criteria (SCIDS).
Demographic and clinical information were gathered at the time of administering the questionnaire by that trained nurse.
Statistical analysis
Descriptive data are given as mean (±SD) and percentage. Comparison among subjects of groups was performed by Student's t-test for continuous variables as well as chi-square test for frequency of dichotomous variables. P < 0.05 was considered significant.
RESULTS
A total of 185 patients completed the questionnaire and were interviewed by a psychiatrist at IEM. The clinical and demographic characteristics of the study sample are presented in Table 1.
Table 1.
Demographic characteristics of the study sample
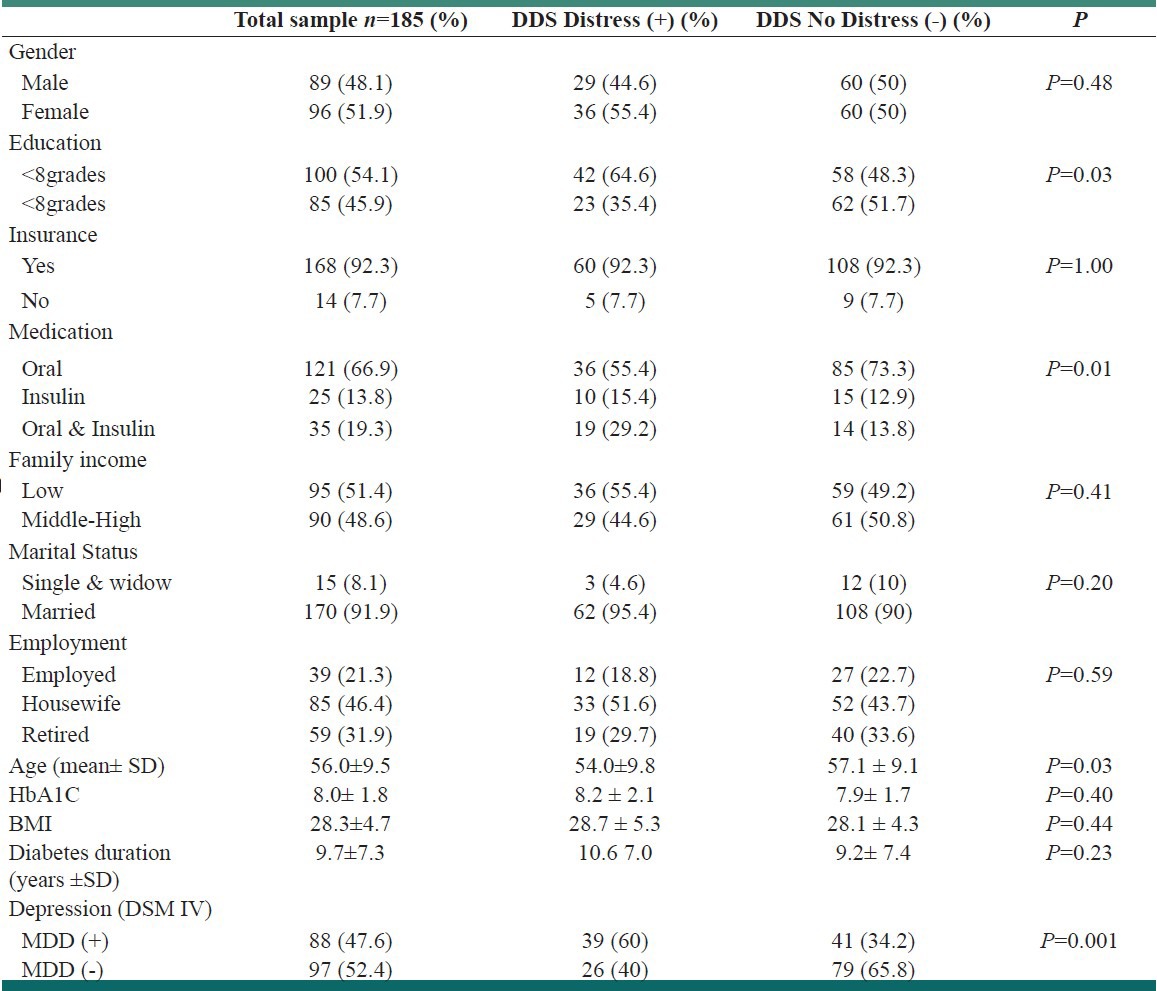
Approximately 52% of the patients were females. The mean age was 56.06 (SD=9.5) years, the mean of duration of diabetes was 9.7 (SD=7.3) years, and average mean of HbA1C was 8.03 (SD=1.89).
Of the 185 patients, 65 (35%) had distress based on DDS self-administered questionnaire. Among the patients with distress, 55% were females and 64% had lower grade of education.
Eighty patients (43.2%) were diagnosed as having Major Depressive Disorder (MDD) based on the clinical interview.
The reliability of four subscales was calculated to be: a) EB (Cronbach's alpha = 0.83(). b) PD (Cronbach's alpha = 0.84), c) RD (Cronbach's alpha = 0.82), and d) ID (Cronbach's alpha = 0.87).
None of the subscales was significantly related to patient gender, educational level, and income. There was a relation between EB subscale and age (P=0.004), employment status (P=0.03), and also diabetes duration (P=0.02). The PD subscale was also related to type of medication (P=0.009) and marital status (P=0.01). It was observed that the RD subscale was also related to age (P=0.003) and duration of diabetes (P=0.005). All subscales were positively associated with depression [Table 2].
DISCUSSION
To the best of our knowledge, there have been a few studies highlighting the significance of psychological aspects of diabetes in Iran. The results of this study show that patients with type 2 diabetes display high rates of distress and also depression (35% and 47.5%, respectively). However, other studies showed different rates. For example, Fisher and colleagues reported a rate of 18% of distress in their study.[18] One of the explanations of higher rate of distress in our sample may be due to the existing co-morbidity of other affective disorders such as depression. We reported a high rate of depression in patients with type 2 diabetes in another study.[16] Even in this study, the prevalence of depression was 47.5%, indicating that 60% of patients with distress were having depression (diagnosed by clinical interview).
The findings of this study show that education and age could have a relation to distress in patients with diabetes. Patients with lower level of education had higher rate of distress than patients with higher level of education. We do not have a clear-cut explanation of this finding; however, it might be justified that people with lower level of education have not learned how to cope with psychological distress. Other studies have shown a negative relationship between age and psychological distress.[19,20]
We found that younger patients had higher rate of distress than older people, which could be explained that younger adults may be more reactive to life stressors, they may experience chronic disease as more developmentally unexpected, and they may cope less effectively with these conditions than older adults.[21] These findings suggest that younger patients and those with much co-morbidity may require particular clinical attention to reduce distress and its negative impact on diabetes outcomes.
Diabetes-specific distress is a common condition that often includes high levels of negative affect. It is linked to poor biobehavioral disease management, and it can be easily confused with MDD or minor depression.[15] The co-occurrence of distress and depression is relatively high among these patients – about 60% of those with distress have depression. The treatment of such patients seems more difficult, with greater risk of relapse and poorer treatment response than either of them alone. Other studies also have shown similar results in the co-occurrence of anxiety and depression in patients with diabetes.[22,23] Thus, clinicians should explore the diagnosis of both conditions and be aware that co-occurring distress and MDD requires more complicated and intensive treatment than either of them separately.
In this study, we considered the possible relationship of various factors with four distress subscales. Our findings show that patients who used insulin had higher rate of PD in comparison with those on other types of medications. This could be justified that neither patients nor physicians know how to deal with using insulin as a stressor. The majority of patients in this study stated that their doctors did not take their concerns seriously enough or even they did not give clear enough directions on how to manage their diabetes.
The rate of EB as another subscale was seen higher in patients who were housewives. Since women as housewives spend most of their time at home, they have enough time to think about their diabetes and its complication and how to deal with it; therefore, their minds would be occupied with thoughts about diabetes and they would be overwhelmed.
EB and RD were higher in younger patients. The possible explanation of these findings has been mentioned earlier in this paper. The most valid justification could be the inadequate skill of coping with stressors in this age group.
Duration of diabetes is found to be an important factor having a strong relationship with EB, RD, and ID. These findings emphasize that overall, people with longer duration of diabetes have not learned how to cope and adapt with diabetes. Also, they do not receive the necessary social and family support.
Limitations
There are, however, a number of limitations to this study. First, this group of patients was included from a referred diabetes center, which may be not representative of patients with type 2 diabetes in a primary care setting. Second, longitudinal data are not yet available, so little can be said about the DDS's test–retest reliability or about the instrument's ability to detect change over time as a function of a clinical intervention.
CONCLUSION
The Iranian version of DDS is an easily scored screening instrument to detect diabetes-specific distress. Having a higher prevalence rate of distress across the study highlights the significance of need for identifying distress and also other mental health conditions in patients with diabetes in order to take collaborative care approaches. Further research is needed to determine the persistence of mood disorders in this group of patients to design an appropriate multidisciplinary care.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Gadsby R. Epidemiology of diabetes. Adv Drug Deliv Rev. 2002;54:1165–72. doi: 10.1016/s0169-409x(02)00094-7. [DOI] [PubMed] [Google Scholar]
- 2.Lusignan S, Sismanidis C, Carey IM, DeWilde S, Richards N, Cook DG. Trends in the prevalence and management of diagnosed type 2 diabetes 1994- 2001 in England and Wales. BMC Fam Pract. 2005;6:13. doi: 10.1186/1471-2296-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Passa P. Diabetes trends in Europe. Diabetes Metab Res Rev. 2002;18(suppl 3):S3–8. doi: 10.1002/dmrr.276. [DOI] [PubMed] [Google Scholar]
- 4.Adeghate E, Schattner P, Dunn E. An update on the etiology and epidemiology of diabetes mellitus. Ann N Y Acad Sci. 2006;1084:1–29. doi: 10.1196/annals.1372.029. [DOI] [PubMed] [Google Scholar]
- 5.Azizi F, Guoya MM, Vazirian P, Dolatshati P, Habbibian S. Screening for type 2 diabetes in the Iranian national programme: A preliminary report. East Mediterr Health J. 2003;9:1122–7. [PubMed] [Google Scholar]
- 6.Azizi F, Gouya MM, Vazirian P, Dolatshahi P, Habibian S. The diabetes prevention and control programme of the Islamic Republic of Iran. East Mediterr Health J. 2003;9:1114–21. [PubMed] [Google Scholar]
- 7.Pouwer F. Should we screen for emotional distress in type 2 diabetes mellitus? Nat Rev Endocrinol. 2009;5:665–71. doi: 10.1038/nrendo.2009.214. [DOI] [PubMed] [Google Scholar]
- 8.Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: Impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160:3278–85. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- 9.Egede L, Zheng D, Simpson K. Co-morbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care. 2002;25:464–70. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 10.Egede LE. Effects of depression on work loss and disability bed days in individuals with diabetes. Diabetes Care. 2004;27:1751–3. doi: 10.2337/diacare.27.7.1751. [DOI] [PubMed] [Google Scholar]
- 11.Katon WJ, Rutter C, Simon G, Lin EH, Ludman E, Ciechanowski PS, et al. The association of comorbid depression with mortality in patients with Type 2 diabetes. Diabetes Care. 2005;28:2668–72. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- 12.Fisher L, Glasgow RE, Mullan JT, Skaff MM, Polonsky WH. Development of a brief diabetes distress screening instrument. Ann Fam Med. 2008;6:246–52. doi: 10.1370/afm.842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fisher L, Skaff MM, Mullan JT, Arean P, Mohr D, Masharani U, et al. Clinical depression vs. distress among patients with type 2 diabetes: Not just a question of semantics. Diabetes Care. 2007;30:542–8. doi: 10.2337/dc06-1614. [DOI] [PubMed] [Google Scholar]
- 14.Grigsby AB, Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. Presence of anxiety in adults with diabetes: A systematic review. J Psychosom Res. 2002;53:1053–60. doi: 10.1016/s0022-3999(02)00417-8. [DOI] [PubMed] [Google Scholar]
- 15.Fisher L, Skaff MM, Mullan JT, Arean P, Glasgow R, Masharani U. A longitudinal study of affective and anxiety disorders, depressive affect and diabetes distress among adults with type 2 diabetes. Diabet Med. 2008;25:1096–101. doi: 10.1111/j.1464-5491.2008.02533.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khamseh ME, Baradaran HR, Rajabali H. Depression and diabetes in Iranian patients: A comparative study. Int J Psychiatry Med. 2007;37:81–6. doi: 10.2190/FP64-82V3-1741-842V. [DOI] [PubMed] [Google Scholar]
- 17.Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, et al. Assessing psychosocial stress in diabetes. Diabetes Care. 2005;28:626–31. doi: 10.2337/diacare.28.3.626. [DOI] [PubMed] [Google Scholar]
- 18.Fisher L, Mullan JT, Skaff MM, Glasgow RE, Arean P, Hessler D. Predicting diabetes distress in patients with Type 2 diabetes: A longitudinal study. Diabet Med. 2009;26:622–7. doi: 10.1111/j.1464-5491.2009.02730.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Charles ST, Reynolds CA, Gatz M. Age-related differences and change in positive and negative affect over 23 years. J Pers Soc Psychol. 2001;80:136–51. [PubMed] [Google Scholar]
- 20.Mirowsky J, Reynolds FR. Age, depression and attrition in the national survey of families and households. Sociol Methods Res. 2000;28:476–504. [Google Scholar]
- 21.Schieman S, Van Gundy K, Taylor J. The relationship between age and depressive symptoms: A test of competing explanator suppression influences. J Aging Health. 2002;14:260–85. doi: 10.1177/089826430201400205. [DOI] [PubMed] [Google Scholar]
- 22.Dombrovski AY, Blakesley-Ball RE, Mulsant BH, Mazumbar S, Houk PR, Szanto K. Speed of improvement in sleep disturbance and anxiety compared with core mood symptoms during acute treatment of depression in old age. Am J Geriatr Psychiatry. 2006;14:550–4. doi: 10.1097/01.JGP.0000218325.76196.d1. [DOI] [PubMed] [Google Scholar]
- 23.Hegel MT, Unutzer J, Tang L, Arean PA, Katon W, Noel PH, et al. Impact of co-morbid panic and posttraumatic stress disorder on outcomes of collaborative care for late-life depression in primary care. Am J Geriatr Psychiatry. 2005;13:48–58. doi: 10.1176/appi.ajgp.13.1.48. [DOI] [PubMed] [Google Scholar]


