Abstract
Background:
To investigate the possible association between serum 25(OH) vitamin D3 concentration and the severity of disease in Iranian patients with multiple sclerosis (MS) and to compare this concentration with a matched control group.
Methods:
This was an analytical cross-sectional study performed at Jondishapour Neurology Clinic in Tehran, Iran. Patients with relapsing–remitting MS were categorized by disease severity: mild [0≤ Expanded Disability Status Scale (EDSS) ≤3], moderate (3.5≤EDSS≤5.5), and severe (6≤EDSS). Serum concentrations of 25(OH) vitamin D3, calcium, phosphorus, magnesium, and parathyroid hormone were measured in 98 MS patients and 17 healthy age- and sex-matched controls. Fisher's exact, Kruskal–Wallis, Mann–Whitney U test, and independent t and Spearman rank correlation tests were used.
Results:
Serum 25(OH) vitamin D3 concentration was significantly lower in patients with MS, especially in the severe MS subgroup, compared with healthy controls (P=0.047). There was a statistically significant inverse correlation between 25(OH) vitamin D3 concentration and EDSS score (P=0.049, R=−0.168 by Spearman rank correlation test), which was observed in women only (P=0.044, R=−0.199).
Conclusions:
Our findings not only further disclose the lower level of vitamin D in MS patients in comparison with healthy controls, but also support the association between vitamin D and disease severity in MS.
Keywords: 25(OH) vitamin D3, disease severity, multiple sclerosis
INTRODUCTION
The prevalence of multiple sclerosis (MS) is increasing in many developing countries and this has drawn research attention toward various factors that might affect the incidence or severity of this disease. Indeed, one of the most striking epidemiological features of MS is a gradient of increasing prevalence with geographic latitude (i.e., greater prevalence with increasing distance from the Equator).[1] This gradient has been observed to persist in some regions even after adjusting for confounding factors such as migration patterns.[2,3,4] This inverse association between the intensity of solar radiation and the prevalence of MS was first observed in 1960.[5] In latitudes greater than 45o, during the winter months, even prolonged sunlight exposure is inadequate to support vitamin D synthesis. During these periods, general populations in these regions are at risk of developing vitamin D deficiency;[6,7] therefore, vitamin D represents one potential link to explain the geographic gradient of MS prevalence.
Research has suggested that an individual's vitamin D status may influence susceptibility to certain immune-mediated diseases.[8] Results from a number of studies on the relation between vitamin D and MS have revealed that vitamin D deficiency often coexists with established MS[9,10] and that oral supplementation may be associated with a lower risk of the disease.[11,12,13]
Iran is located nearer to the equator than are countries with a traditionally higher prevalence of MS. Nevertheless, the incidence of MS in Iran has recently increased.[14,15] Some clinicians believe that despite high solar radiation, Iranians do not generally receive adequate and effective radiation as a result of certain ethnic and cultural variables (including type of clothes, etc.) and consequently suffer from low vitamin D serum levels.[16] This study was therefore performed to compare serum 25(OH) vitamin D3 concentration between Iranian MS patients and healthy controls and to investigate further the association between 25(OH) vitamin D3 level and disease severity.
METHODS
Patients and controls
This analytical cross-sectional study was conducted at Jondishapour Neurology Clinic in Tehran, Iran. Eligible patients had relapsing–remitting MS (RRMS), as determined by the McDonald criteria (revision 2005).[17] Reasons for exclusion were: Use of digitalis or vitamin D supplementation; any condition predisposing to hypercalcemia, nephrolithiasis, or renal insufficiency; pregnancy; and unwillingness to restrict dietary calcium. Finally, 98 patients with RRMS were consecutively recruited. To compare the serum values of different variables (including vitamin D3) with normal concentrations of healthy population in the same area, 17 Iranian healthy controls who were matched to MS patients regarding age and sex distribution were studied. It must be noted that all the patients and healthy controls originated from the same ethnicity, with similar skin color and behavioral factors. Moreover, all the patients received similar standard protocol of disease-modifying treatment during their course of disease.
The study was approved by the ethics committee of Shaheed Beheshti University of Medical Sciences and was conducted in accordance with the Declaration of Helsinki. Moreover, an informed consent was also obtained from each patient before the recruitment for participation in study.
Clinical assessments
Neurological, clinical, and magnetic resonance imaging (MRI) assessments were conducted at the time of patient enrollment; all clinical assessments were performed by the same neurologist who was not aware of the vitamin D3 result beforehand. At enrollment, patients’ neurological impairment was assessed using the Expanded Disability Status Scale (EDSS).[18] Assessment of EDSS score was performed at almost the same time of day for all patients and when the patients were not in relapse or were not receiving steroids. The EDSS score is based on data from the neurological examination and the patient's ability to walk. Scores range from 0 (indicating no neurological abnormality) to 10 (death caused by MS). Patients were categorized by the severity of their disease: mild (0≤ EDSS ≤3), moderate (3.5≤ EDSS ≤5.5), and severe (6≤ EDSS).
Laboratory measurements
Serum concentrations of 25(OH) vitamin D3, calcium, phosphorus, magnesium, and parathyroid hormone (PTH) were measured during the summer months in both patient and control groups. Serum 25(OH) vitamin D3 levels were measured using a semi-automated solid-phase extraction reverse-phase high-performance liquid chromatography assay (Pars-Azmoon kit, Tehran, Iran).
Statistical analysis
The data were analyzed using SPSS v.15 software for Windows (SPSS Inc., Chicago, IL, USA). Fisher's exact test was used to compare gender distribution between two groups of study. The Kolmogorov–Smirnov test was performed to evaluate normal distribution of the quantitative variables. To test the differences between non-parametric variables and means in the two study groups and/or subgroups (patients vs. controls and/or mild to moderate vs. severe MS patients), the Mann–Whitney U test and independent t-test were used. The Kruskal–Wallis test was used to compare the differences between various levels of disease severity and control group (more than two-group comparisons). Associations between quantitative variables were investigated using the Spearman rank correlation test. A 5% probability of a type I error was considered in the analysis; therefore, a P-value less than 0.05 was considered statistically significant.
RESULTS
Baseline characteristics
A total of 98 patients with MS and 17 healthy individuals were evaluated. Among the MS patients, three quarters [75.5% (74/98)] were women, the mean [standard deviation (SD)] age was 34.19 (9.10) years, and the mean (SD) disease duration was 6.02 (5.14) years. The mean (SD) EDSS score was 2.76 (1.93); disease severity was mild in 71 patients (72.5%), moderate in 11 (11.2%), and severe in 16 (16.3%) patients. Almost similarly, 82.4% (14/17) of the controls were women with the mean age of 34.36 (8.12) years, which were not significantly different with regard to sex distribution (Fisher's exact P=0.758) and mean age of the patients (t-test P=0.850).
Comparison of laboratory characteristics between MS patients and controls
Serum concentrations of 25(OH) vitamin D3, calcium, phosphorus, magnesium, and PTH were measured in all patients and controls. The data are shown in Table 1.
Table 1.
Demographic, laboratory, and clinical characteristics of patients with multiple sclerosis and healthy control group
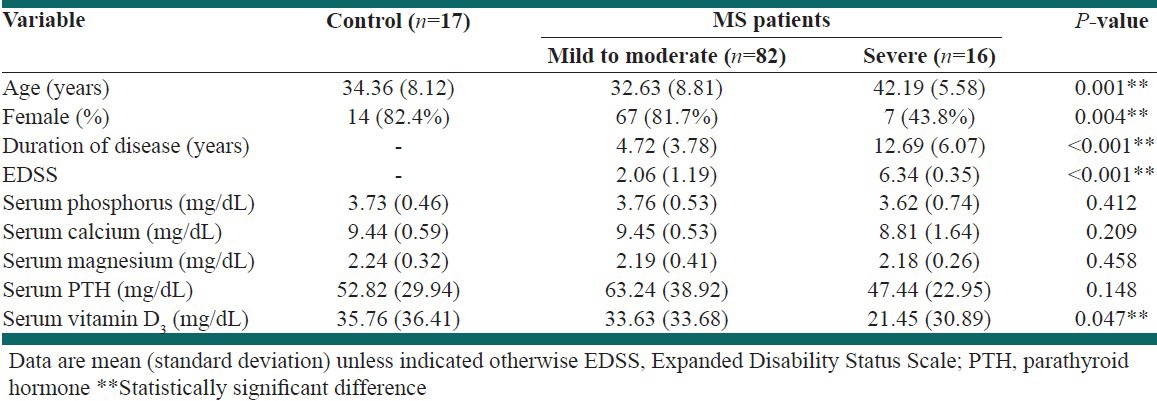
The mean (SD) of serum 25(OH) vitamin D3 concentration was 35.76 (36.41) mg/dL in healthy controls and 31.66 (33.40) mg/dL in MS patients. As illustrated in Figure 1, only the serum level of 25(OH) vitamin D3 was significantly different between controls and MS patients, especially severe MS subgroup (P=0.047).
Figure 1.

Comparison of serum concentration of 25(OH) vitamin D3 (mean±SE) in MS patients with different severities of disease and control group (P=0.047)
Correlation of laboratory measurements with patient characteristics
The results of Mann–Whitney U test showed that serum level of 25(OH) vitamin D3 was significantly lower in severe MS patients in comparison with mild/moderate cases [21.45 (30.89) mg/dL vs. 33.63 (33.68) mg/dL, P=0.011]. By contrast, other laboratory measurements were not significantly different between these two subgroups of MS patients (all P>0.05). Although patients with severe MS were significantly older than those with mild/moderate disease (P<0.001), there was no significant correlation between age and serum 25(OH) vitamin D3 concentration (P=0.180).
As shown in Figure 2, a statistically significant inverse correlation was found between 25(OH) vitamin D3 level and EDSS score (P=0.049, RSpearman=−0.168). Another statistically significant inverse correlation was also seen between serum calcium concentration and EDSS score (P=0.021, RSpearman=−0.206).
Figure 2.
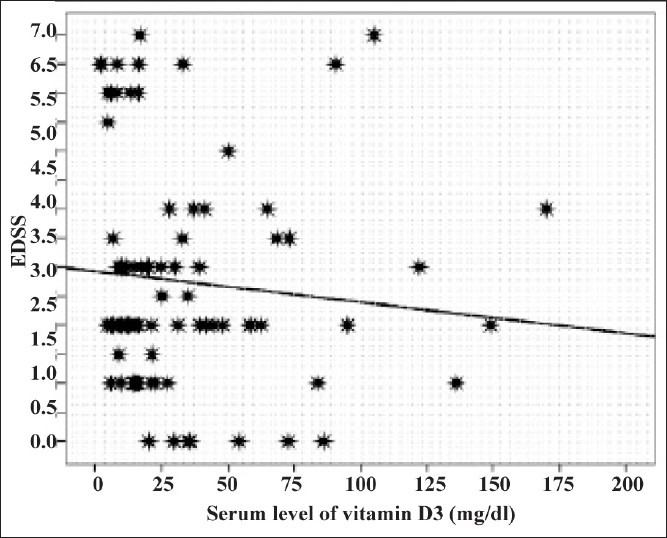
Inverse correlation between serum concentration of 25(OH) vitamin D3 and EDSS score in MS patients (RSpearman= −0.168, P=0.049)
Further analysis of the inverse correlation between serum 25(OH) vitamin D3 concentration and disease severity showed that this correlation was only observed in women (P=0.044, RSpearman=−0.199). On the other hand, there were no significant differences between women and men in either overall mean serum 25(OH) vitamin D3 concentration [31.25 (35.36) mg/dL vs. 32.95 (27.09) mg/dL, P=0.270] or EDSS score [2.49 (1.61) vs. 3.58 (2.57), P=0.080].
DISCUSSION
Our study emphasized the lower serum 25(OH) vitamin D3 concentration in MS patients in comparison with healthy controls and evaluated the association between serum 25(OH) vitamin D3 concentration and disease severity in Iranian patients with MS. We found a statistically significant inverse correlation between 25(OH) vitamin D3 level and EDSS score. Patient sex also appeared to be an important factor, as a statistically significant inverse relation was only found in female patients; this correlation was not affected by patient age. Our findings support the possible importance of vitamin D status in patients with MS and its association with disease severity.
The role of vitamin D in MS has been assessed over the last two decades. One of the first animal studies showed that vitamin D deficiency resulted in increased susceptibility to experimental allergic encephalomyelitis (EAE, an animal model of MS).[19] Some of the most direct evidence comes from a large prospective epidemiological study which demonstrated that the intake of vitamin D from multivitamin supplements led to a 40% reduction in the risk of MS among female nurses in the USA.[13] Other studies reported no difference in serum 25(OH) vitamin D3 levels between patients with MS at diagnosis and controls, when samples were obtained during the winter months, but found lower serum 25(OH) vitamin D3 concentrations in patients with MS during June to September.[20] In addition, patients had lower vitamin D levels during MS relapses than in remission, which suggests that vitamin D could be involved in the regulation of clinical disease activity.[20] An inverse correlation between brain MRI activity in patients with MS and serum 25(OH) vitamin D3 levels in the general population in southern Germany was demonstrated in another study.[21] Further, 25(OH) vitamin D3 levels were found to be lower in patients with progressive forms of MS compared with RRMS, and low levels were also associated with an increase in clinical MS severity, as measured by EDSS score and the occurrence of relapses.[22]
Another recent study was performed in Isfahan, Iran, a city with a similar amount of sun exposure by Shaygannejad et al.[23] Similar to our findings, they have also confirmed a lower level of serum vitamin D in MS patients than that of normal population. Both the cities of Tehran and Isfahan have lots of sunshine over days in almost four seasons, which is significantly higher in comparison with that in European and North American countries.
Effects of patient sex on the correlation between serum vitamin D concentration and MS severity have also been demonstrated in other studies. In EAE, dietary vitamin D delayed the onset and severity of the disease in female but not male mice.[24] In a study of women with and without MS, every 10 nmol/L increase in serum 25(OH) vitamin D3 concentration reduced an individual's odds of a diagnosis of MS by 19%. In the same study, a negative correlation was also found between EDSS score and serum 25(OH) vitamin D3 level in women (P=0.020, R=−0.29).[25] In contrast, a recent study reported no differences in serum 25(OH) vitamin D levels between patients with MS and controls, but demonstrated higher levels in female patients with MS than in male patients.[26] These results may provide some clues into the pathogenesis of the sex difference in the risk and clinical manifestations of MS, and in the nature of the environmental factors involved in MS.
The underlying mechanism for the association between serum 25(OH) vitamin D3 concentrations and MS severity is currently unknown. Although more serious disability in MS patients with higher EDSS and severe form of disease could potentially lead to a lesser sun exposure, the findings of such studies like ours emphasized the considerable lower serum level of vitamin D3 in these patients more. Methodologically, it is not possible to assess the causality inference between the two entities, severe MS and vitamin D3 deficiency, unless a longitudinal study could be performed with serial measurement of vitamin D3 in MS patients. As our study is designed as a cross-sectional research, similar to most previous researches in this subject, it is not logically possible to demonstrate whether severe MS cases are prone to vitamin D3 deficiency or the patients with low serum level of this vitamin are vulnerable to progress to a severe form of MS. In other words, it is only possible to interpret a correlation or an association between severe MS and lower concentrations of vitamin D3 with such cross-sectional studies. Also, as previously mentioned, there are only a few studies to compare vitamin D3 level between different groups of MS patients with regard to disease severity. However, the clues derived from these cross-sectional researches may lead to further achievement of causality relationships.
In vitro, 1,25(OH)2 vitamin D3, which is produced mainly by hydroxylation of 25(OH) vitamin D3 in the kidney,[27] is a potent immune modulator that inhibits pro-inflammatory cells and promotes anti-inflammatory cells and cytokines.[28] Patients with MS have shown changes in their cytokine profiles following dietary supplementation with vitamin D (1000 IU/day) plus calcium (800 mg/day).[29] However, more studies are needed to clarify the mechanism of the apparent modulating effect of vitamin D on MS pathology.
The current study has some limitations, including its cross-sectional design, small sample size, and uneven group sizes when patients were categorized by disease severity. Although the mean level of serum vitamin D3 was not significantly different between patients with moderate disease and the ones with mild severity, it must be noted that only 12 patients had moderate disease and this subgroup comparison has a low statistical power. Due to the low sample size of moderate group, we merged them with the mild MS cases in order to improve the statistical power and the merged group was named as “mild to moderate” MS cases. Further studies with a higher sample size of moderate cases are needed for better comparison of vitamin D3 level between mild and moderate cases. Moreover, as previously mentioned, an overall inverse correlation was found between 25(OH) vitamin D3 level and EDSS score, which could give more hints about the correlation between disease severity and vitamin D3 level when it is assessed quantitatively within all MS cases with a higher statistical power.
Our results may also be important for understanding the increasing incidence of MS in Iran, where recent reports show the prevalence of vitamin D deficiency as high as 86% in women, 53.6% in girls, and 75% in newborns during winter in some regions of Iran.[30,31]
In conclusion, our findings reveal a lower level of vitamin D in MS patients and suggest that vitamin D could be involved in the regulation of clinical disease activity in MS, based on its inverse correlation with disease severity, as measured using the EDSS score. Pilot studies have already been performed to evaluate the effects of vitamin D supplementation on cytokine levels and safety and tolerability in patients with MS.[29,32] We believe that trials of vitamin D supplements, both as a preventive agent for individuals at risk and as a therapeutic agent in female patients with MS, should be considered. In addition, it is still unknown if lowered vitamin D levels predispose to the disease or are a result of it and other studies designed to evaluate the possible mechanisms of the modulatory role of vitamin D in MS are warranted.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Ebers GC, Sadovnick AD. The geographic distribution of multiple sclerosis: A review. Neuroepidemiology. 1993;12:1–5. doi: 10.1159/000110293. [DOI] [PubMed] [Google Scholar]
- 2.Kurtzke JF. Geography in multiple sclerosis. J Neurol. 1977;215:1–26. doi: 10.1007/BF00312546. [DOI] [PubMed] [Google Scholar]
- 3.Compston A. Distribution of multiple sclerosis. In: Compston A, Ebers GC, Lassmann H, editors. McAlpine's multiple sclerosis. 3rd ed. London: Churchill Livingstone; 1998. pp. 63–100. [Google Scholar]
- 4.Hammond SR, McLeod JG, Millingen KS, Stewart-Wynne EG, English D, Holland JT, et al. The epidemiology of multiple sclerosis in three Australian cities: Perth, Newcastle and Hobart. Brain. 1988;111:1–25. doi: 10.1093/brain/111.1.1. [DOI] [PubMed] [Google Scholar]
- 5.Acheson ED. Some comments on the relationship of the distribution of multiple sclerosis to latitude, solar radiation, and other variables. Acta Neurol Scand. 1960;35:132–47. doi: 10.1111/j.1600-0447.1960.tb08674.x. [DOI] [PubMed] [Google Scholar]
- 6.Holick MF. Vitamin D: A millennium perspective. J Cell Biochem. 2003;88:296–307. doi: 10.1002/jcb.10338. [DOI] [PubMed] [Google Scholar]
- 7.Webb AR, Kline L, Holick MF. Influence of season and latitude on the cutaneous synthesis of vitamin D3: Exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. J Clin Endocrinol Metab. 1988;67:373–8. doi: 10.1210/jcem-67-2-373. [DOI] [PubMed] [Google Scholar]
- 8.Hyppönen E, Läärä E, Reunanen A, Järvelin MR, Virtanen SM. Intake of vitamin D and risk of type 1 diabetes: A birth-cohort study. Lancet. 2001;358:1500–3. doi: 10.1016/S0140-6736(01)06580-1. [DOI] [PubMed] [Google Scholar]
- 9.Hayes C, Cantorna M, DeLuca H. Vitamin D and multiple sclerosis. Proc Soc Exp Biol Med. 1997;216:21–7. doi: 10.3181/00379727-216-44153a. [DOI] [PubMed] [Google Scholar]
- 10.Hayes C. Vitamin D: A natural inhibitor of multiple sclerosis. Proc Nutr Soc. 2000;45:531–5. doi: 10.1017/s0029665100000768. [DOI] [PubMed] [Google Scholar]
- 11.Nieves J, Cosman F, Herbert J, Shen V, Lindsay R. High prevalence of vitamin D deficiency and reduced bone mass in multiple sclerosis. Neurology. 1994;44:1687–92. doi: 10.1212/wnl.44.9.1687. [DOI] [PubMed] [Google Scholar]
- 12.Cosman F, Nieves J, Komar L, Ferrer G, Herbert J, Formica C, et al. Fracture history and bone loss in patients with MS. Neurology. 1998;51:1161–5. doi: 10.1212/wnl.51.4.1161. [DOI] [PubMed] [Google Scholar]
- 13.Munger KL, Zhang SM, O’Reilly E, Hernán MA, Olek MJ, Willett WC, et al. Vitamin D intake and incidence of multiple sclerosis. Neurology. 2004;62:60–5. doi: 10.1212/01.wnl.0000101723.79681.38. [DOI] [PubMed] [Google Scholar]
- 14.Saadatnia M, Etemadifar M, Maghzi AH. Multiple sclerosis in Isfahan, Iran. Int Rev Neurobiol. 2007;79:357–75. doi: 10.1016/S0074-7742(07)79016-5. [DOI] [PubMed] [Google Scholar]
- 15.Sahraian MA, Khorramnia S, Ebrahim MM, Moinfar Z, Lotfi J, Pakdaman H. Multiple sclerosis in Iran: A demographic study of 8,000 patients and changes over time. Eur Neurol. 2010;64:331–6. doi: 10.1159/000321649. [DOI] [PubMed] [Google Scholar]
- 16.Bassir M, Laborie S, Lapillonne A, Claris O, Chappuis MC, Salle BL. Vitamin D deficiency in Iranian mothers and their neonates: A pilot study. Acta Paediatr. 2001;90:577–9. [PubMed] [Google Scholar]
- 17.Polman CH, Reingold SC, Edan G, Filippi M, Hartung HP, Kappos L, et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Ann Neurol. 2005;58:840–6. doi: 10.1002/ana.20703. [DOI] [PubMed] [Google Scholar]
- 18.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS) Neurology. 1983;33:1444–52. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 19.Cantorna MT, Hayes CE, Deluca HF. 1, 25-Dihydroxyvitamin D3 reversibly blocks the progression of relapsing encephalomyelitis, a model of multiple sclerosis. Proc Natl Acad Sci. 1996;93:7861–4. doi: 10.1073/pnas.93.15.7861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Soilu-Hanninen M, Airas L, Mononen I, Heikkila A, Viljanen M, Hanninen A. 25-Hydroxyvitamin D levels in serum at the onset of multiple sclerosis. Mult Scler. 2005;11:266–71. doi: 10.1191/1352458505ms1157oa. [DOI] [PubMed] [Google Scholar]
- 21.Embry AF, Snowdon LR, Vieth R. Vitamin D and seasonal fluctuations of gadolinium-enhancing magnetic resonance imaging lesions in multiple sclerosis. Ann Neurol. 2000;48:271–2. [PubMed] [Google Scholar]
- 22.Smolders J, Menheere P, Kessels A, Damoiseaux J, Hupperts R. Association of vitamin D metabolite levels with relapse rate and disability in multiple sclerosis. Mult Scler. 2008;14:1220–4. doi: 10.1177/1352458508094399. [DOI] [PubMed] [Google Scholar]
- 23.Shaygannejad V, Golabchi KH, Haghighi S, Dehghan H, Moshayedi A. A comparative study of 25 (OH) vitamin D serum levels in patients with multiple sclerosis and control group in Isfahan, Iran. Int J Prev Med. 2010;1:195–201. [PMC free article] [PubMed] [Google Scholar]
- 24.Spach KM, Hayes CE. Vitamin D3 confers protection from autoimmune encephalomyelitis only in female mice. J Immunol. 2005;175:4119–26. doi: 10.4049/jimmunol.175.6.4119. [DOI] [PubMed] [Google Scholar]
- 25.Kragt JJ, van Amerongen BM, Killestein J, Dijkstra CD, Uitdehaag BM, Polman CH, et al. Higher levels of 25-hydroxyvitamin D is associated with a lower incidence of multiple sclerosis only in women. Mult Scler. 2009;15:9–15. doi: 10.1177/1352458508095920. [DOI] [PubMed] [Google Scholar]
- 26.Barnes MS, Bonham MP, Robson PJ, Strain JJ, Lowe-Strong AS, Easton-Evans J, et al. Assessment of 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D3 concentrations in male and female multiple sclerosis patients and control volunteers. Mult Scler. 2007;13:670–2. doi: 10.1177/1352458506072666. [DOI] [PubMed] [Google Scholar]
- 27.Jongen MJ, van der Vijgh WJ, Lips P, Netelenbos JC. Measurement of vitamin D metabolites in anephric subjects. Nephron. 1984;36:230–4. doi: 10.1159/000183159. [DOI] [PubMed] [Google Scholar]
- 28.Smolders J, Damoiseaux J, Menheere P, Hupperts R. Vitamin D as an immune modulator in multiple sclerosis, a review. J Neuroimmunol. 2008;194:7–17. doi: 10.1016/j.jneuroim.2007.11.014. [DOI] [PubMed] [Google Scholar]
- 29.Mahon BD, Gordon SA, Cruz J, Cosman F, Cantorna MT. Cytokine profile in patients with multiple sclerosis following vitamin D supplementation. J Neuroimmunol. 2003;134:128–32. doi: 10.1016/s0165-5728(02)00396-x. [DOI] [PubMed] [Google Scholar]
- 30.Kazemi A, Sharifi F, Jafari N, Mousavinasab N. High prevalence of vitamin D deficiency among pregnant women and their newborns in an Iranian population. J Womens Health (Larchmt) 2009;18:835–9. doi: 10.1089/jwh.2008.0954. [DOI] [PubMed] [Google Scholar]
- 31.Rabbani A, Alavian SM, Motlagh ME, Ashtiani MT, Ardalan G, Salavati A, et al. Vitamin D insufficiency among children and adolescents living in Tehran, Iran. J Trop Pediatr. 2009;55:189–91. doi: 10.1093/tropej/fmn078. [DOI] [PubMed] [Google Scholar]
- 32.Wingerchuk DM, Lesaux J, Rice GP, Kremenchutzky M, Ebers GC. A pilot study of oral calcitriol (1,25-dihydroxyvitamin D3) for relapsing–remitting multiple sclerosis. J Neurol Neurosurg Psychiatry. 2005;76:1294–6. doi: 10.1136/jnnp.2004.056499. [DOI] [PMC free article] [PubMed] [Google Scholar]


