Abstract
Background:
Clinical risk management focuses on improving the quality and safety of health care services by identifying the circumstances and opportunities that put patients at risk of harm and acting to prevent or control those risks. The goal of this study is to identify and assess the failure modes in the ICU of Qazvin's Social Security Hospital (Razi Hospital) through Failure Mode and Effect Analysis (FMEA).
Methods:
This was a qualitative-quantitative research by Focus Discussion Group (FDG) performed in Qazvin Province, Iran during 2011. The study population included all individuals and owners who are familiar with the process in ICU. Sampling method was purposeful and the FDG group members were selected by the researcher. The research instrument was standard worksheet that has been used by several researchers. Data was analyzed by FMEA technique.
Results:
Forty eight clinical errors and failure modes identified, results showed that the highest risk probability number (RPN) was in respiratory care “Ventilator's alarm malfunction (no alarm)” with the score 288, and the lowest was in gastrointestinal “not washing the NG-Tube” with the score 8.
Conclusions:
Many of the identified errors can be prevented by group members. Clinical risk assessment and management is the key to delivery of effective health care.
Keywords: Risk assessment, failure mode and effect analysis, Intensive care unit
INTRODUCTION
Intensive care of critically ill patients in the high-technology units those are well equipped units is an essential components of modern care. For the first time, intensive care unit (ICU) was used in a polio epidemic in Copenhagen in 1952. Mortality rate was declined from 90% to 40% by respiratory care of polio patients, then, the ICU has been developed to the current form with modern equipment.[1]
In the ICU, aggressive diagnostic and therapeutic procedures are used for critically ill patients. In normal conditions that patients who are not experiencing complications during hospitalization, mortality rate is more than 25%, while it reaches more than 40% in case of complications.[1] Therefore, patient safety and risk management is very important in the ICU.
Patient safety is one of the nation's most pressing health care challenges, which are in the domain of clinical risk management; in fact clinical risk management is a principal element of clinical governance.[2,3] In other words, besides error detection capabilities, establishing effective clinical risk management depends on institutionalizing the culture of error reporting based on trust.[4,5] Reducing the probability of clinical risks in hospitals is very important to improve: Health care quality, having effective hospital staff and patients relationship, patient satisfaction and also to limit complaints on medical errors and nursing care.[2,3]
Using an acuity tool to assess risk of death in patients admitted to an intensive care unit (ICU) has become a standard parameter for research and quality improvement studies.[6]
Failure mode and effect analysis (FMEA) is a very useful technique to identify and reduce errors which was first used in 1960 in aerospace industry.[2,3] It is a systematic, bottom-up and teamwork-based tool which is utilized in defining, detecting, preventing, eliminating or controlling failures, reasons and effects of potential errors in a service system. Before delivering final services to customers, it manages the implementation and documentation of these activities.[7,8]
The most important achievement of this method is detection of the system's vulnerable elements and critical points,[9] which requires error prediction and prevention. The prediction is done by well-experienced professionals with enough knowledge and experiences about the process or service. Therefore, selecting the team, planning and full implementation of FMEA are very important.[10]
The primary application of this technique in health care dates back in 1990, which was related to the production and consumption of drugs and prevention of medical errors in hospitals.[2,3] For the first time, The National Center of Military Affairs in U.S introduced health failure mode and effect analysis (HFMEA) in 2008.[11] In the same year, The Technical Committee of the International Organization for Standardization (ISO) licensed a technical specification for medical laboratories suggesting FMEA as a method for prospective risk analysis of high-risk processes.[2,3] The aim of FMEA is to detect and correct failure modes. There are two phases in FMEA. The first phase is about the detection of errors and their effects and the second is about the analysis of critical points to determine the severity of each error through risk priority number (PRN) ranking.[8] In fact, FMEA has five main stages:
Selection of the process or the care that should be studied
Formation of multi-task teams
Collection and organization of information about process or activities
Risk analysis and proposed actions
Follow-up actions and the risk reanalysis[2]
In the last decades, there has been an increasing development in intensive care medicine, where the goal is to provide the best outcome for critically ill patients. Indeed, a worldwide expansion occurred in the number of intensive care units (ICUs). Despite the great importance of critically ill patients care in the ICUs and high mortality of inpatients in these units, according to our review, it seems that no comprehensive study has been performed in the world to determine risk factors and reasons for mortality of inpatients in the ICU.[12] FMEA is an effective method to prevent problems. This technique is one of the most meticulous tools of measurement, assessment and finally management of the risks. This study is concerned with the identifying and assessment of available risks in clinical cares of the ICU of Razi Hospital by FMEA.
METHODS
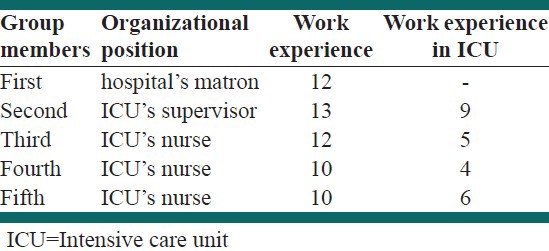
This was a qualitative-quantitative research by focus discussion group (FDG) performed in Qazvin Province, Iran during 2011. The study population included process owners and those who were completely familiar with the ICU processes. Sampling method was purposeful and the FDG group members were selected by the researcher. Due to the specialized nature of clinical care in the ICU, FDG members consisted of hospital matron, head nurse of the ICU, and three well-experienced nurses selected by the head nurse [Table 1]. First of all, printed and electronic documents related to the topic research and were reviewed, after that some professional consultation were done, and then information about current activities of the ICU in clinical cares were collected.
Table 1.
Members of focus discussion group
We listed all activities related to clinical care during two weeks through direct observation and then reviewedpatients history, the nursingteam views, finally key activities were chosen in respect to head nurse’ opinion and FMEA team agreement. Throughout the research, team members were trained FMEA technique, teamwork principles and brainstorming methods by researchers.
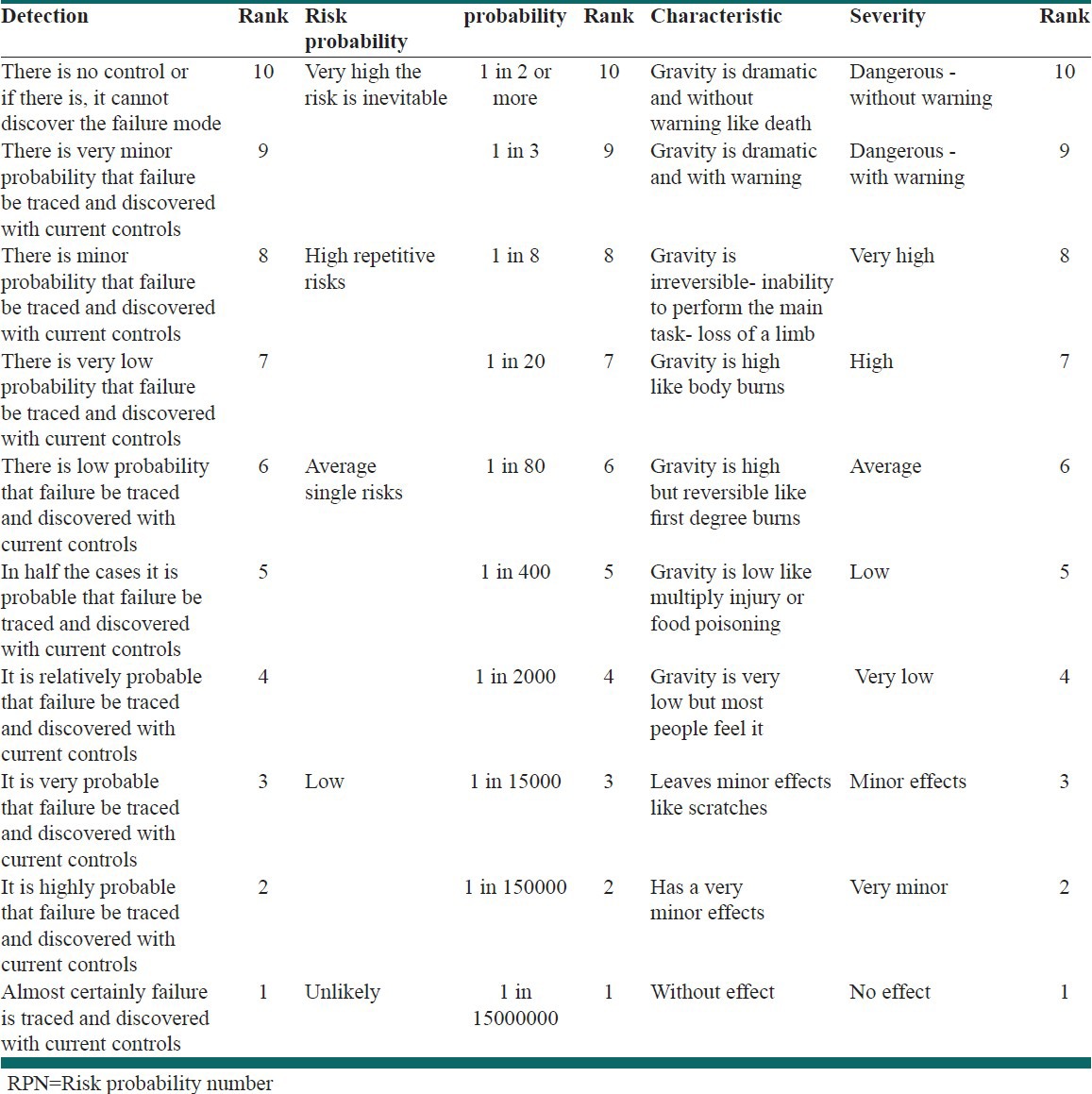
Team members were selected based on their skill and experiences accordance with the head nurse's opinion. Key activities were defined by FMEA team in 10 sessions up to 22 h, and failure modes and effects were detected. Then degree of severity, occurrence and detection of RPN were identified through brainstorming [Table 2].
Table 2.
RPN elements
In order to collect data, standard worksheets of failure mode and effects analysis technique were used[13] and all the team members reached an agreement to comment and score. Although this method gives the most accurate number, but it is too time-consuming.
At the end of each session, the researcher revised and summarized the whole discussion-faithful to the discussion- and calculated RPN for each failure mode.
Data analysis consisted of following steps:
Reviewing opinions of team members
Summarizing and classifying data through coding and refining opinions, and rewriting team members’ views in related columns of FMEA form
Returning opinions to participants in order to reliability of the findings
Weighting opinions of the participant in final forms
Final decision making about proposed actions
To confirm the validity and reliability of this research, after formatting FDGs and completing related checklists by group members, the researcher showed the results to group members and they confirmed their accuracy.
RESULTS
Firstly, 138 clinical care processes of ICU are identified and they classified in 8 general categories, then 23 critical cares of these were selected by group members for risk assessment through the study of care processes, patient's history and group brainstorming. Selected critical cares have high risk score and team members believed them to be of higher sensitivity. They also suggested that these cares had a higher RPN compared to other cares. After focused group discussions on each clinical care for the ICU patients, 48 failure modes were detected. Effects and potential causes, current state of controls, proposed actions, responsible person, and the time of performance were determined by team members for each failure mode. Given the consensus presented to the team, members were not required to complete worksheets individually and they were unanimous on a topic at the end of the discussion. Results showed that out of 48 detected clinical errors, the highest risk probability number was in respiratory care sector “Ventilator's alarm malfunction (no alarm)” with the score 288, and the lowest was in gastrointestinal care sector “not washing the NG Tube” with the score 8 [Table 3]. Ventilator's alarm malfunction has a high probability and severity, and it has a high RPN despite its low degree of discovery of this failure mode.
Table 3.
The highest priorities of detected potential errors of the ICU nursing cares
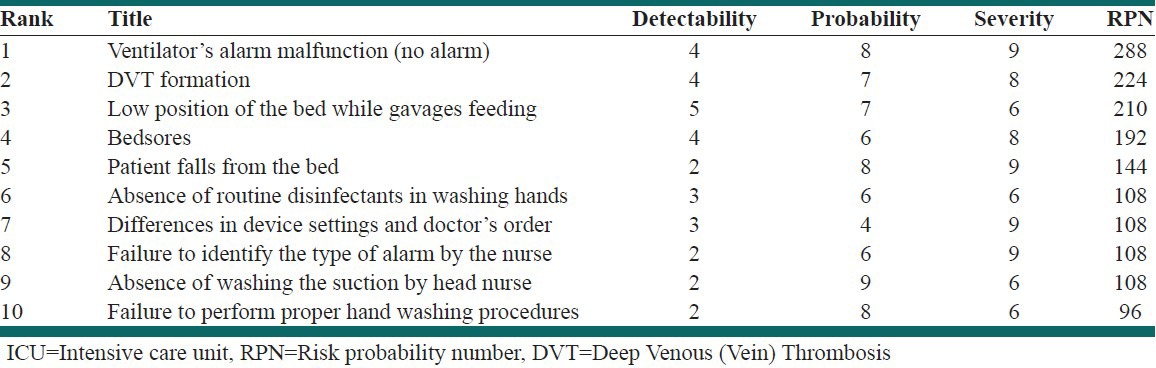
As a whole, it was determined that most of potential errors had low discovery number showing that the ICU nurses were familiar with potential errors of cares and would discover their causes immediately. It is noteworthy, nursing failure and neglect is not the only causes of ICU potential errors, there are many factors caused errors such as patients’ sensitivity, patient with complex conditions and underlying disease, lack or malfunction of equipment, negligence and malpractice of physicians and other personnel, lack of proper training to the nurses, fatigue due to sensitivity and high volume of workload in ICU. Team members also proposed some actions to control and eliminate each of detected clinical errors which were classified in four general categories:
Actions related to training and improving of clinical cares
Actions related to shift work scheduling and use of motivational techniques for nurses
Actions related to hiring experienced, enthusiastic and skillful work forces
Actions related to purchase, maintenance, repair and calibration of medical equipment
Totally, our results showed that actions related to training and improving clinical cares and also proper shift scheduling to minimize nurses’ fatigue are very important factors to reduce potential risks, therefore proper planning for these factors will have significant effects on clinical risk management and improvement of patient safety.
DISCUSSION
Failure modes and effect analysis method is used to assess different consequences and processes in health care.[14] The strengths of this method are multi-task teams, patients’ involvement and improved understanding of the process.[14,15] Faye also says that the advantage of such techniques is that they do not blame staff, but seek to create a safe and stress-free environment for them through finding how errors, especially human ones, occur during work processes and assist organizations in reducing complaints and improving customers’ satisfaction.[16]
Using FMEA technique in ICU, we find out clinical errors, their causes and potential effects then proposed actions are identified by team members and each action is assigned to a person to follow-up.
Tofighi's findings showed that FMEA methodology has a high degree of efficiency and effectiveness in detecting and prioritizing improvable points of current triage processes in a complicated section such as ED and also in predicting effective actions to reduce risks.[5] In a study performed in 2007, Naseri stated that techniques such as FMEA which can be utilized based on teamwork with a proactive approach would enhance staff's precision, focus on potential weaknesses and try to eliminate those.[16] The main principle in implementing FMEA is team formation teamwork. The combination of team members is an important factor in successful implementation of FMEA. Findings of Dominici's study in 2006 as “implementation of HFMEA in bariatric surgery” showed the importance of a multidisciplinary team of different professionals, particularly managers involvement for detection and classification of failure modes, in enhancing the results of HFMEA implementation in patient care.[16,17] Tilburg's findings in 2005 about proactive assessment of failure modes in Pediatric Oncology section also showed that hospital manager's support for the team has an important role in fulfilling their suggestions.[16,18]
The results also showed that the composition and diversity of focus discussions group is very important to identify and assess risks in ICU. If group members have not team spirit, it has not any consequences.
Apkon conducted FMEA of the process of continuous drug infusion delivery in a pediatric ICU attempt to redesign the intravenous (IV) delivery process and to improve patient safety and efficiency in staff work flow.[14,19]
Weaknesses include the time necessary to complete a PRA Wetterneck for example, reported that the FMEA of an adult inpatient medication system required more than 46 h of meetings for nearly five months. FMEA have also been criticized because of the tedious process involved in and difficulty of the analysis, problems with the scoring system,[21,22] and unreliability of scoring.[14,22]
This study also confirms that, despite support from senior managers to implement this technique and group members collaboration, this technique was very time consuming so recognizing the 45 failure modes require the five meeting (in 22 h) for 3 months.
On the other hand, risk number is an important criterion in determining the most substantial clinical errors in the system. Therefore, the use of more accurate methods with higher sensitivity to the degree of severity leads to better results in FMEA Table.[7] In this regard, Sankar also has indicated that failure modes with high RPNs have a higher priority and are of greater importance.[23] But it is important to note that during the implementation of FMEA in health section, the overemphasis on RPN would lead to the ignorance of errors with low RPN and high severity, or with high probability and/or low discoverability.
Results show that many of the causes of these failure modes, not only caused by negligence of nurses and nursing care but also other factors involved. For example, the patient's sensitivity in the ICU, complex situation and the underlying disease, lack of proper equipment or equipment failure, medical negligence and malpractice of doctors and other personnel, lack of proper training to ICU's nurses and fatigue due to the sensitivity and high workload in this ward can be mentioned in this section.
According to Reason's opinion, despite overt errors (especially human errors) which are often predicted and corrected hardly, the latent conditions that underlie human errors could be detected and corrected before any occurrence of traumatic events. The understanding of this process would lead the path of error detection towards proactive rather than retrospective risk management.[4,5] Benjamin also believes that inadequate written or oral communication is the reason for many errors, especially medication errors. He states that achievement of safe operation depends on establishing safe systems, and proposes the implementation of FMEA in preventing system errors and detecting safe networks (with effective communications) in health system.[5,24] Weber in his study in 2006 also emphasizes that FMEA provides a proactive mechanism for enhancing processes to prevent deviations.[16,25] Due to the wide range of clinical errors in health system, most researchers have conducted many case studies. This study is intended to examine all nursing care processes, and then detect probable errors to manage all risk factors. Holding continuous training courses on risk assessment and management, enhancement of proper work shift scheduling with motivational techniques for nurses, hiring well-experienced and enthusiastic work forces, and also maintenance, repair and calibration of medical equipment are important actions which could eliminate, reduce or control clinical errors to a great extent. On the other hand, an efficient management system would reduce negative effects of clinical errors to and lead to maximal efficiency of health care services using the minimum possibilities and human powers through well-organized activities.[26]
CONCLUSIONS
For several reasons, the intensive care unit (ICU) potentially is an attractive setting for early adoption of FMEA; however, successful implementation of FMEA in ICUs is likely to require strong, effective leadership and a sustained commitment to prevent errors that may have occurred rarely or never before in the local setting.[27]
Many of the detected errors can be prevented by group members and risk management requires the ICU health care processes be controlled more to improve the efficiency and quality of the care.
This technique was implemented based on the Hospital's clinical governance plan. Finally, the results were presented to the Qazvin's deputy ofmedcare insocial security organization and was appointed this technique also be used for risk assessment and management in ED, operating room and the CCU.
Suggestions
As highly importance of clinical governance, it is necessary to implement risk management to health care quality improvement. For this end, it is recommended that using risk assessment techniques such as implied here and also by use of FMEA standard worksheet, failure modes of clinical care be detected, assessed and proposed actions will be taken to reduce their probability, severity and detectability. Then, we would see improved quality of nursing cares in hospitals.
ACKNOWLEDGMENTS
We would like to thank Dr. Babaei (vice-chancellorof the Qazvin's deputy ofmedcare insocial security organization, Mr Zolghadr (Razi Hospital's Matron), and Ms. Salari (ICU head nurse), Ms. Houshmand, Ms. Yaghoubi and Ms. Ebrahimi (ICU nurses).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Singer M, Little R. ABC of intensive care. Cutting edge. BMJ. 1999;319:501–4. doi: 10.1136/bmj.319.7208.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chiozza ML, Ponzetti C. FMEA: A model for reducing medical errors. Clin Chim Acta. 2009;404:75–8. doi: 10.1016/j.cca.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 3.Morelli P, Vinci A, Galetto L, Magon G, Maniaci V, Banfi G. FMECA methodology applied to two pathways in an orthopaedic hospital in Milan. J Prev Med Hyg. 2007;48:54–9. [PubMed] [Google Scholar]
- 4.Reason J. Human error: Models and management. BMJ. 2000;18:768–70. doi: 10.1136/bmj.320.7237.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tofi ghi SH, Maleki AR, Khoshkam M, Atarjannesar F. Using the prospective method “Failure Modes and Effect Analysis” To improve the triage processin emergency department. J Forensic Med. 2009;15:161–70. [Google Scholar]
- 6.6 Morris PE. Assessing ICU transfers at night: A call to reduce mortality and readmission risk. Am J Crit Care. 2009;18:6–8. doi: 10.4037/ajcc2009944. [DOI] [PubMed] [Google Scholar]
- 7.Maleki AR. Designand modeling of a monolithic structure“QFD/FMEA” in Health care centers. Payesh J. 2010;9:117–30. [Google Scholar]
- 8.Sharma RK, Kumar D, Kumar P. Systematic failure mode effect analysis (FMEA) using fuzzy linguistic modelling. Int J Qual Reliab Manage. 2005;22:986–1004. [Google Scholar]
- 9.Hojatnejad A. LPG spherical tank safety assessmentusing FMEA techniques and ETBA. Behbood J. 2008;12:180–9. [Google Scholar]
- 10.Sedaghat A. Assessmentand risk management of an emergency military field using the FMEA method. J Milit Med. 2008;10:167–74. [Google Scholar]
- 11.Trucco P. Cavallin M.A quantitative approach to clinical risk assessment: The CREA method. J Saf Sci. 2006;44:491–513. [Google Scholar]
- 12.Chen YC, Lin SF, Liu CJ, Jiang DD, Yang PC, Chang SC. Risk factors for ICU mortality in critically ill patient. Journal of the formosan medical association. 2001;100:656–61. [PubMed] [Google Scholar]
- 13.Ericson C. Hoboken, New Jersey: Wiley and Sons Publication; 2005. Hazard analysis techniques for system safety. [Google Scholar]
- 14.Faye H, Rivera-Rodriguez AJ, Karsh BT, Hundt AS, Baker C, Carayon P. Risk and event assessment: Involving intensive care unit nurses in a proactive risk assessment of the medication management process. Jt Comm J Qual Patient Saf. 2010;36:376–84. doi: 10.1016/s1553-7250(10)36056-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.BurgMeier J. Failure mode and effect analysis: An application in reducing the risk of blood transfusion. Jt Comm J Qual Improv. 2002;28:331–9. doi: 10.1016/s1070-3241(02)28033-5. [DOI] [PubMed] [Google Scholar]
- 16.Yarmohammadian MH, Tofighi SH, Saghaiannejad Esfahanib S, Naseribooriabadi T. Risks Involved in Medical Records Processes of Al-Zahra Hospital. Health Inf Manag. 2008;4:51–9. [Google Scholar]
- 17.Dominici L, Brams D. Implementation of HFMEA in a bariatric surgery program improves the quality and culture of care. Surg Obes Relat Dis. 2006;2:346–7. [Google Scholar]
- 18.Tilburg C. Health Care Mode and Effect Analysis: A useful proactive risk analysis in a proactive oncology ward. quality and safety in health care. 2005;15:58–64. doi: 10.1136/qshc.2005.014902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Apkon M, Leonard J, Probst L, DeLizio L, Vitale R. Design of a safer approach to intravenous drug infusions: Failure mode effects analysis. Qual Saf Health Care. 2004;13:265–71. doi: 10.1136/qshc.2003.007443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wetternecka T, Skibinskib K, Schroederc M, Robertsd T, Carayone P. Challenges with the Performance of Failure Mode and Effects Analysis in Healthcare Organizations: An IV Medication Administration HFMEA. Proceedings of the Human Factors and Ergonomics Society Annual Meeting. 2004;48:1708–12. [Google Scholar]
- 21.Wetterneck TB, Skibinski KA, Roberts TL, Kleppin SM, Schroeder ME, Enloe M, et al. Using failure mode and effects analysis to plan implementation of smart i.v. Pump technology. Am J Health Syst Pharm. 2006;63:1528–38. doi: 10.2146/ajhp050515. [DOI] [PubMed] [Google Scholar]
- 22.Shebl NA, Barber N, Franklin BD. Is failure mode and effect analysis reliable? J Patient Saf. 2009;5:86–94. doi: 10.1097/PTS.0b013e3181a6f040. [DOI] [PubMed] [Google Scholar]
- 23.Sankar NR, Prabhu BS. Modified approach for prioritization of failures in a system failure mode and effects analysis. International Journal of Quality and Reliability Management. 2001;18:324–35. [Google Scholar]
- 24.Benjamin DM. Reducing medication errors and increasing patient safety: Case studies in clinical pharmacology. J Clin Pharmacol. 2003;43:768–83. [PubMed] [Google Scholar]
- 25.Weber S. Kansas: Clinical and Laboratory Standards Institute Institute, University of Kansas Hospital; 2006. Utilizing failure mode and effects analysis to examine the processes of patient identification and specimen labeling. [Google Scholar]
- 26.Yarmohamadian MH, Atighechian G, Shams L, Haghshenas A. Are hospitals ready to response to disasters? Challenges, opportunities and strategies of Hospital Emergency Incident Command System (HEICS) J Res Med Sci. 2011;16:1070–7. [PMC free article] [PubMed] [Google Scholar]
- 27.Beau D, Barry D. Failure mode and effects analysis application to critical care medicine. critical care clinics. 2005;21:21–30. doi: 10.1016/j.ccc.2004.07.005. [DOI] [PubMed] [Google Scholar]


