Abstract
Background:
Dental practice presents opportunities for cross-contamination. The dentist's face is at high-risk of infection transmission. The purpose of this study was to evaluate the risk of contamination in different areas of dentist's face during dental practices.
Methods:
The visible splashes of materials that accumulated on cellulose face shields during 144 prosthetics and periodontal procedures were evaluated. The splashes were detected on 14 areas (each 1 cm2) of the dentist's face including around nose, mouth, eyes, and zygoma by a magnifier (×2). One way Analysis of variance, Duncan and t-test were used for data analysis (α = 0.05).
Results:
Contamination of different areas of dentist's face was significantly different (P < 0.05). The areas around nose and the inner corner of eyes were the most contaminated areas. Zygoma was the least contaminated area. The contaminated areas during periodontal treatments were significantly more than prosthetic treatments (P < 0.05). There was no significant difference between contamination on left and right sides of the face.
Conclusions:
During dental practice, central areas of the face such as inner part of the eyes and around the nose were most contaminated areas. These parts are the important areas for transmission of infection. It is recommended to use protective means like glasses, mask, and protective shield, which have more protection field in these areas.
Keywords: Aerosols, dentists, infection control, risk
INTRODUCTION
Healthcare staff especially dentists and the other dental personnel are endangered by infectious diseases.[1,2,3] For most of the last century, dental practitioners did not use any protectors for eyes, nose, and mouth; however, the prevalence of infectious diseases has emphasized the need of infection control principles.[4] Among occupational threats for this group, transmission of infections especially viral diseases such as Hepatitis B, Hepatitis C and acquired immune deficiency syndrome is more critical.[5] The previous studies showed that the number of healthcare staff contaminated in developing countries has increased 5.84% yearly.[2,3] World health organization has reported 2.5% of human immunodeficiency virus (HIV) and 40% of Hepatitis B and Hepatitis C infections in healthcare staff by occupational contacts.[6] This issue is of great importance for dentists, because they have to work with sharp and high-speed instruments daily, accompanied by constant contact with hazardous microorganisms.[7] In addition, the specific form of oral cavity and close contact with a large number of patients makes dental team susceptible to different dangerous infections. The oral cavity is a unique environment with moist, proper temperature, and internal and external metabolites, which promote bacterial growth.[8] It has been shown that most human pathogens could be obtained from the oral cavity.[9] Thus, health organizations developed guidelines to prevent or minimize threat to dental team's health[10] among which, the use of personal protective equipment's is critical.[7] For example, the guidelines proposes mask and shield for protection of critical areas of the face against dangerous microorganisms.[11] Blood as a main source of transmission[12] and saliva, despite its bactericidal nature, are potential microorganism carriers.[13] They can both be found in tiny particles including solid particles, vapors, and liquid droplets, which were produced during dental procedures. Solid particles can float in the air for hours[13] and vapors tend to come down on surfaces after 5-15 min.[14] The particles can carry pathogenic microorganisms, leading to Hepatitis B,[15,16,17] conjunctivitis, contact dermatitis, and respiratory system infections.[18]
Sotiriou et al.[19] suggested that dental drilling procedures aerosolize saliva and produce particles small enough to penetrate deep into the lungs. Bentley et al.[14] evaluated the distribution of spatter and aerosols generated by high-speed instrumentations, showing that contamination from spatter and aerosol dissemination remains a significant hazard for dental personnel. Checchi et al.[20] showed that exposed areas of the dentist's face are at risk with contaminated particles.
The aim of this study was to evaluate the risk of contamination in high-risk areas of dentist's face during dental practice. The null hypothesis was that there is no significant difference among risk of contamination in different areas of the dentist's face.
METHODS
This experimental study was carried out on 72 prosthetic and 72 periodontal visits in private and public clinics. To evaluate the contamination rate of different areas of dentist's face, transparent sheets (8.27 In × 11.69 In) were provided. A piece of rectangular prism sponge (11.69 In × 1 × 1 In) was glued to one length of the sheet for comfort placement on the face. A piece of rubber band was attached to these compartments, making a face shield. Placement of the shields was performed by one person for all dentists. The dentists did dental procedures, including scaling by ultrasonic scaling unit (Cavitron, Dentsply, Addlestone, UK) on mandibular arch as the periodontal treatment and tooth preparation with high-speed hand piece (Sirona, Bensheim, Germany) for fixed prosthesis as the prosthetic treatment, also in mandibular arch. All the participated dentists in this study were right handed. Each procedure took between 40 and 50 min to perform, with an average time of 44 min. The type of procedure and its area were recorded. At the end of procedure, the shield was taken from dentist's face and let it dry in room temperature. The sponge was detached from the shield, making it ready for analysis. Fourteen squares with 1 cm2 surface area were determined on a checked A4 paper as a pattern. For each side of the face, three squares were located around the eye (inner corner, outer corner and middle of the eye), one on the cheek, one lateral to the ala and two around the mouth (commissure and middle of lips). The squares were numbered 1-7 on right side and lettered A to G on left side of the face [Figure 1]. The borders of the shield were matched with the borders of the checked paper. Each shield was investigated separately, in a way that visible particles on it were counted, using a magnifier equipped with a small light (×2). Particles contaminating 1 mm2 were scored 1 and those of smaller sized were scored 0.5. The scores of different studied areas were analyzed by one-way analysis of variance and Duncan tests (α = 0.05). Student t-test was used to compare contamination level of prosthetic and periodontal procedures.
Figure 1.
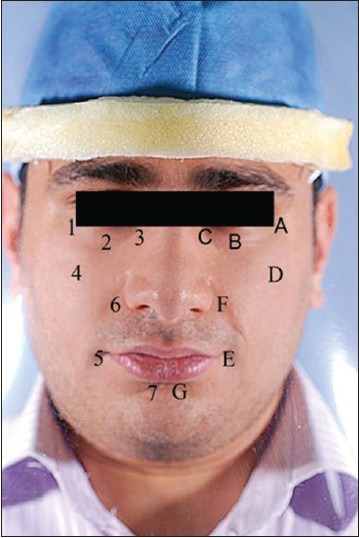
Studied areas of the face: 1, A - Outer corner of the eyes. 2, B - Middle of the eyes. 3, C - Inner corner of the eyes. 4, D - Cheeks. 5, E - Lip commisures. 6, F - Lateral ala, 7, G - Middle of lips
RESULTS
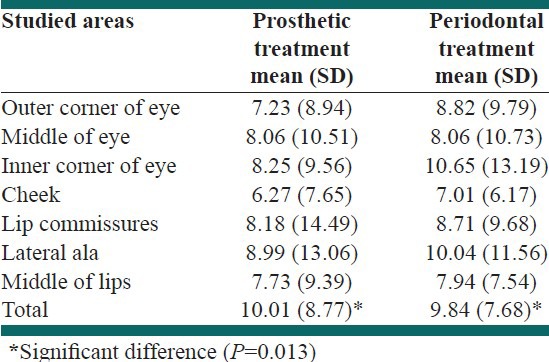
Table 1 presents the mean scores of splashes on the studied areas in both sides of the face. There was a significant difference between contamination values of different areas of the face (P < 0.05) [Table 2]. The areas lateral to ala and inner corner of eye were more contaminated than the other areas, but there was only a significant difference between these areas and cheeks (P < 0.05). There was no significant difference between right and left side of the face (P = 0.415). Contamination values of periodontists’ face were significantly more than prosthodontists’ faces (P < 0.05) [Table 3].
Table 1.
Mean (standard deviation) and Duncan groups of splashes scores on studied areas in both sides of the face
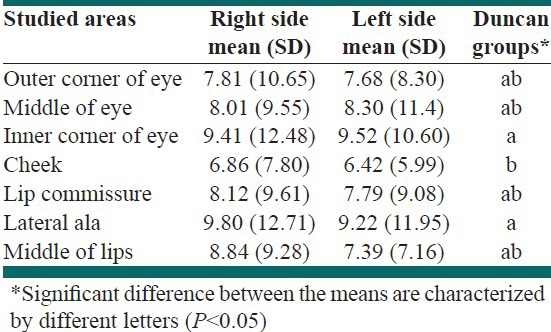
Table 2.
Analysis of variance of mean values of contamination in the studied areas
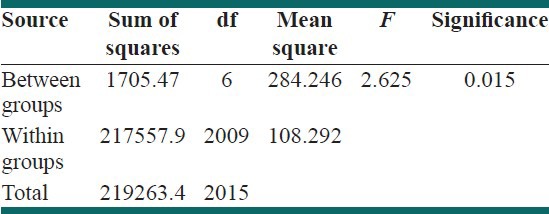
Table 3.
Mean facial splashes score of the studied areas during prosthetic and periodontal treatments
DISCUSSION
Dentists are exposed to different types of infectious microorganisms daily. A large number of pathogens are localized in the oral cavity, which can be transmitted in different ways during dental procedures,[8] usually by means of air/water syringe and high-speed instruments.[19] Two basic ways for spreading pathogenic microorganisms in a dental practice are blood and saliva through droplet aerosol of infected patients.[21] The greatest risks for the dentist are hepatitis B and C viruses, and HIV virus that spread through blood and cause life-threatening diseases.[5,21,22] Type B viral liver infections occur in dentists at least 3 times more often than in the general population.[23] Risk-factors spread via the saliva include a vast range of microorganisms, such as cytomegalovirus, Epstein-Barr virus, and human herpes viruses.[21] Herpes simplex virus is among the important risk-factors transmitted in this way.[24] Saliva may become infected with the virus not only through blood but also through gingival fluid.[21]
The results of this study showed that the areas around nose and inner corner of eyes are significantly at higher risk of contamination (P < 0.05). Thus, the null hypothesis that there is no significant difference among risk of contamination in different areas of the dentist's face was rejected. This may be because of the dentist's position and his direct view during operation on mandibular jaw. In addition, it is more difficult to manage the saliva during dental practice on mandible. Since the dentist gets closer to the patient to have a better view, it is not surprising to have more contamination in central areas of the face.
Checchi et al.[20] investigated the facial areas, which were most susceptible to infections during surgical procedures. They did not find a significant difference among different areas of the face except the area above right eye and left side of the chin. This contrast is partly due to different investigated areas of the face in the two studies. On the other hand, in their study, the patients had undergone a periodontal surgery with osseous resection in maxilla or mandible, while in present study scaling and teeth preparation in mandibular arch were investigated. Periodontal surgery exposes the operator's face to a greater risk. Findings of the present study and Checchi et al.[20] showed that there is no significant difference between left and right side of the face.
Comparing prosthetic and periodontal procedures, the latter caused more contamination in the present study. This could be because of more bleeding and soft-tissue irritation during scaling.[25] It has been shown that the most intensive aerosol and splash production occurs during the work of an ultrasonic scaling unit and high-speed hand piece.[26,27,28] However, higher levels of oral microorganisms were generated during particular dental procedures, especially during scaling.[27] In the present study, the periodontists used ultrasonic scaling unit, which leads to production of tiny particles.[29]
Water droplets in splash are from 50 μm to several millimeters in diameter and move 15-120 cm from a patient's oral cavity.[26,27,28,30] Splatter shows limited penetration into the respiratory system,[27] but can come into contact with the mucosa of nostrils, open mouth, eyes, and skin. They are deposited on hair, clothes and in the immediate surroundings of the splatter source. Correct working technique and behavior can protect the dentist and his or her assistant from the threat resulting from dental aerosols and should include: (1) the use of personal protective equipments; (2) rinsing the oral cavity of a patient with chlorhexidine before dental procedure; (3) the use of high-performance sucking devices during aerosol production; (4) the use of good ventilation in a dental office.[28,31]
CONCLUSIONS
Within the limitations of this study the followings can be drawn:
The central areas of face are at high-risk of contamination during dental practice.
Periodontists are more at risk of face contamination compared to prosthodontists.
Both sides of the face are equally contaminated during dental procedures.
ACKNOWLEDGMENT
This study was supported by Isfahan University of Medical Sciences Research Grant #83011. The manuscript was based on a thesis submitted to the undergraduate school of Isfahan University of Medical Sciences in partial fulfillment of the requirement for the Doctor in Dental Surgery Degree.
Footnotes
Source of Support: This study was supported by Isfahan University of Medical Sciences Research Grant # 83011
Conflict of Interest: None declared
REFERENCES
- 1.Molinari JA. Dental infection control at the year 2000. Accomplishment recognized. J Am Dent Assoc. 1999;130:1291–8. doi: 10.14219/jada.archive.1999.0399. [DOI] [PubMed] [Google Scholar]
- 2.Singru SA, Banerjee A. Occupational exposure to blood and body fluids among health care workers in a teaching hospital in mumbai, India. Indian J Community Med. 2008;33:26–30. doi: 10.4103/0970-0218.39239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MacCannell T, Laramie AK, Gomaa A, Perz JF. Occupational exposure of health care personnel to hepatitis B and hepatitis C: Prevention and surveillance strategies. Clin Liver Dis. 2010;14:23–36. doi: 10.1016/j.cld.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Leonard RH, Crawford JJ., Jr . Infectioin control. In: Heymann HO, Swift EJ Jr, Ritter AV, editors. Sturdevant's Art and Science of Operative Dentistry. 6th ed. London: Mosby; 2012. p. e98. [Google Scholar]
- 5.Ayatollahi J, Ayatollahi F, Ardekani AM, Bahrololoomi R, Ayatollahi J, Ayatollahi A, et al. Occupational hazards to dental staff. Dent Res J (Isfahan) 2012;9:2–7. doi: 10.4103/1735-3327.92919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Geneva: WHO; 2002. World Health R. Reducing Risks, Promoting Healthy Life; pp. 1–167. [Google Scholar]
- 7.Kanjirath PP, Coplen AE, Chapman JC, Peters MC, Inglehart MR. Effectiveness of gloves and infection control in dentistry: Student and provider perspectives. J Dent Educ. 2009;73:571–80. [PubMed] [Google Scholar]
- 8.Decraene V, Ready D, Pratten J, Wilson M. Air-borne microbial contamination of surfaces in a UK dental clinic. J Gen Appl Microbiol. 2008;54:195–203. doi: 10.2323/jgam.54.195. [DOI] [PubMed] [Google Scholar]
- 9.Molinari JA, Molinari GE. Is mouthrinsing before dental procedures worthwhile? J Am Dent Assoc. 1992;123:75–80. doi: 10.14219/jada.archive.1992.0079. [DOI] [PubMed] [Google Scholar]
- 10.Matsuda JK, Grinbaum RS, Davidowicz H. The assessment of infection control in dental practices in the municipality of São Paulo. Braz J Infect Dis. 2011;15:45–51. [PubMed] [Google Scholar]
- 11.Kohn WG, Collins AS, Cleveland JL, Harte JA, Eklund KJ, Malvitz DM, et al. Guidelines for infection control in dental health-care settings– 2003. MMWR Recomm Rep. 2003;52:1–61. [PubMed] [Google Scholar]
- 12.Ishihama K, Koizumi H, Wada T, Iida S, Tanaka S, Yamanishi T, et al. Evidence of aerosolised floating blood mist during oral surgery. J Hosp Infect. 2009;71:359–64. doi: 10.1016/j.jhin.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 13.Micik RE, Miller RL, Mazzarella MA, Ryge G. Studies on dental aerobiology. I. Bacterial aerosols generated during dental procedures. J Dent Res. 1969;48:49–56. doi: 10.1177/00220345690480012401. [DOI] [PubMed] [Google Scholar]
- 14.Bentley CD, Burkhart NW, Crawford JJ. Evaluating spatter and aerosol contamination during dental procedures. J Am Dent Assoc. 1994;125:579–84. doi: 10.14219/jada.archive.1994.0093. [DOI] [PubMed] [Google Scholar]
- 15.Kew MC. Possible transmission of serum (Australia- antigen-positive) hepatitis via the conjunctiva. Infect Immun. 1973;7:823–4. doi: 10.1128/iai.7.5.823-824.1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pattison CP, Boyer DM, Maynard JE, Kelly PC. Epidemic hepatitis in a clinical laboratory. Possible association with computer card handling. JAMA. 1974;230:854–7. [PubMed] [Google Scholar]
- 17.Molinari JA, Merchant VA, Gleason MJ. Controversies in infection control. Dent Clin North Am. 1990;34:55–69. [PubMed] [Google Scholar]
- 18.Neuman H. Occupational hazards in dentistry. Refuat Hapeh Vehashinayim. 2011;28:72. [PubMed] [Google Scholar]
- 19.Sotiriou M, Ferguson SF, Davey M, Wolfson JM, Demokritou P, Lawrence J, et al. Measurement of particle concentrations in a dental office. Environ Monit Assess. 2008;137:351–61. doi: 10.1007/s10661-007-9770-7. [DOI] [PubMed] [Google Scholar]
- 20.Checchi L, Matarasso S, Pirro P, D’Achille C. Topographical analysis of the facial areas most susceptible to infection with transmissible diseases in dentists. Int J Periodontics Restorative Dent. 1991;11:164–72. [PubMed] [Google Scholar]
- 21.Szymanska J. Microbiological risk factors in dentistry. Current status of knowledge. Ann Agric Environ Med. 2005;12:157–63. [PubMed] [Google Scholar]
- 22.van Wijk PT, Meiberg AE, Bruers JJ, Groenewold MH, van Raalten AL, Dam BA, et al. The risk of blood exposure incidents in dental practices in the Netherlands. Community Dent Oral Epidemiol. 2012;40:567–73. doi: 10.1111/j.1600-0528.2012.00702.x. [DOI] [PubMed] [Google Scholar]
- 23.Cottone JA, Puttaiah R. Hepatitis B virus infection. Current status in dentistry. Dent Clin North Am. 1996;40:293–307. [PubMed] [Google Scholar]
- 24.Lewis MA. Herpes simplex virus: An occupational hazard in dentistry. Int Dent J. 2004;54:103–11. doi: 10.1111/j.1875-595x.2004.tb00263.x. [DOI] [PubMed] [Google Scholar]
- 25.Mandel ID. The functions of saliva. J Dent Res. 1987;66:623–27. doi: 10.1177/00220345870660S203. [DOI] [PubMed] [Google Scholar]
- 26.Leggat PA, Kedjarune U. Bacterial aerosols in the dental clinic: A review. Int Dent J. 2001;51:39–44. doi: 10.1002/j.1875-595x.2001.tb00816.x. [DOI] [PubMed] [Google Scholar]
- 27.Bennett AM, Fulford MR, Walker JT, Bradshaw DJ, Martin MV, Marsh PD. Microbial aerosols in general dental practice. Br Dent J. 2000;189:664–7. doi: 10.1038/sj.bdj.4800859. [DOI] [PubMed] [Google Scholar]
- 28.Szymanska J. Dental bioaerosol as an occupational hazard in a dentist's workplace. Ann Agric Environ Med. 2007;14:203–7. [PubMed] [Google Scholar]
- 29.Williams GH, 3rd, Pollok NL, 3rd, Shay DE, Barr CE. Laminar air purge of microorganisms in dental aerosols: Prophylactic procedures with the ultrasonic scaler. J Dent Res. 1970;49:1498–1504. doi: 10.1177/00220345700490065701. [DOI] [PubMed] [Google Scholar]
- 30.Prospero E, Savini S, Annino I. Microbial aerosol contamination of dental healthcare workers’ faces and other surfaces in dental practice. Infect Control Hosp Epidemiol. 2003;24:139–41. doi: 10.1086/502172. [DOI] [PubMed] [Google Scholar]
- 31.Harrel SK. Airborne spread of disease–The implications for dentistry. J Calif Dent Assoc. 2004;32:901–6. [PubMed] [Google Scholar]


