Abstract
Context:
Sleep is an effective factor in the process recovery from diseases. Many variables affect the sleep quality of hospitalized older patients.
Aim:
This study was conducted to evaluate the quality of sleep and its related risk factors in hospitalized older patients in Kashan’s hospitals, Iran 2009. Settings and design: a cross-sectional study was carried out on a sample of 400 hospitalized older adults in the hospital of Kashan, Iran.
Materials and Methods:
The Farsi Pittsburgh Sleep Quality Index (FPSQI) was used for gathering data. A global sum of 6 or greater indicates a poor quality of sleep. Statistical analysis used: data were analyzed using the Chi-square test, t-test, ANOVA, and binary logistic regression at the multivariate model.
Results:
The overall quality of sleep of the patients in this study was poor. In the final regression model, sex (OR = 0.342), level of education (OR = 0.470), type of ward (OR = 0.592), previous hospitalization experience (OR = 2.336), and use of hypnotics in hospital (OR = 3.633) were the most important predictors of sleep quality. The most prevalent sleep disturbing factors were worries and anxiety, environmental noises and pain. However, the most negative effects on the PSQI mean score were reported to be from dyspnea, environmental lights, and changes in the sleep habits. Quality of sleep also had significant relationship with sleep latency (P = 0.001) and having a respiratory disorder.
Conclusions:
The knowledge of sleep disturbing factors in hospitalized older adults might help in planning preventive strategies to improve quality of sleep.
Keywords: Aged, hospitalization, insomnia, risk factors
INTRODUCTION
Aging is associated with serious changes in the pattern and quality of sleep.[1] Some researchers have argued that sleep disturbances experienced with the increase of age can be linked to the other changes, including the significant increase of medical and mental health problems and lifestyle alterations.[2,3] It is estimated that 30-45% of the world’s population complaint from sleep disorders[4–9] and its prevalence increases with age. It is predicted that the population of elderly reaches to 10 millions in Iran by the year 2019.[10] It has shown that poor quality sleep is the third most common health problem of older adults, ranking behind headaches and gastrointestinal disorders.[6] A large study has suggested that 42% of older adults with age more than 65 year had difficulty initiating and maintaining sleep with an annual incidence rate of approximately 5%.[11] Insomnia is the most prevalent consequence of physical disorders that is commonly associated with sleep latency (more than 30 min), difficulty with sleep maintenance, or early awakening.[12]
Sleep quality is important for two reasons. Firstly, complaints related to sleep quality are common. Bedtime and sleeping difficulties are the major factors affecting sleep quality and account for 15-35% of these difficulties and secondly, low sleep quality is an indicator of many illnesses.[13] Poor sleep quality can decrease the person’s feelings, thoughts, and motivation. Physical and cognitive symptoms of people with poor sleep quality are tiredness, loss of concentration, weariness, low threshold for pain, anxiety and nervousness, irrational thoughts, hallucinations, loss of appetite, constipation, and being more accident prone.[3,14] It is also well known that sleeping problems cause tension, delay in wound healing, increase of pain, and difficulties in performing daily activities.[15]
Older adults are hospitalize three times more than persons lower than 65 year of age and their long of stay is also more.[16] Hospitalization causes sleep pattern disturbances and insomnia.[17,18] Although patients may appear to sleep in hospital, it may not be refreshing or restorative.[17,19] Several reports can be found in relation to the prevalence of sleep disturbances in older adults; however, the quality of sleep in hospitalized older adults have not been studied so much in recent years.[20] Because the trend of the aging of population and due to the effects of sleep on the elderly’s health and quality of life, the lack of an up-to-date study on the quality of sleep in elderly patients with physical disorders and specially the hospitalized elderly patients, specially from Iran and the middle-east region and the responsibility of nurses to have adequate information about the sleeping patterns and sleep problems of their clients. This study was conducted to evaluate the quality of sleep and its related risk factors in hospitalized older patients in Kashan’s hospitals, Iran 2009.
MATERIALS AND METHODS
Research design and context
A cross-sectional study was conducted on a sequential sample of 400 hospitalized older patients in the university hospitals in Kashan, Iran. This study received ethical approval from the ethics committee of Kashan University of Medical Sciences (KAUMS). All subjects provided written consent before participation. This study consecutively recruited patients aged 65 and older admitted to surgical and medical wards of the University teaching Hospital between June 1, 2009 and October 31, 2009.
The inclusion criteria were: age 65 or above, able to communicate either by speaking or writing and not being in an elderly hospice before the study. Exclusion criteria were: patients unable of answering questionnaires because of severe speech disorders (aphasia, dysarthria) or severe hearing loss; length of stay (LOS) in hospital less than 7 days and patients suffering from cognitive impairment according to the short portable mental status questionnaire (SPMSQ). The SPMSQ is a 10-question, reliable and easy to use test to evaluate the cognitive function in older adults.[21,22] In our study, reliability was calculated using the test retest (0.79). The sample size was calculated based on the previous report which estimated that 47% of hospitalized older patients have some form of sleep disorders.[23]
Instruments
Tow questionnaires were used to collect data from the participants. 1) Personal information form and 2) The Farsi Pittsburgh Sleep Quality Index (FPSQI). The personal information form included the following information: demographic information such as age, gender, education level, and marital status and ten questions related to type of ward in which the patient was hospitalized (medical and surgical), daytime napping, LOS, using hypnotics at hospital, previous hospitalization experience, medical disorder, type of sleep disorders and sociopersonal, physical, and environmental factors.
The PSQI is a self-rated instrument that frequently was used to measure the quality and patterns of sleep in older adults. The questionnaire is simple, easily completed, and all of the self-rated items are grouped into seven individual components of subjective sleep quality, sleep latency, length of sleep, sleeping habit, sleep disorders, use of sleeping medication, and daytime dysfunction over the last week. Each component scores between 0 and 3 points. The total index score will be between 0 and 21. A global sum of 6 or greater indicates a “poor” quality of sleep.[24] The original English version of the PSQI was initially translated into Farsi. Subsequently, a faculty member with a good knowledge of English performed a retrograde translation into English. The two English versions (original and retrograde translated) were compared. No specific item needed to be replaced. Reliability was calculated using the Cronbach’s alpha internal consistency coefficient (α = 0.82). The questionnaires were completed by the patients if they were educated. Otherwise, a registered nurse asked questions to gather information.
Statistical analysis
Statistical analysis was performed using SPSS version 14. The first step was to determine the relationship between the dependent variable (sleep quality) with independent variables using univariate analysis included chi-square or Fisher exact tests for qualitative variables and t-test and ANOVA for quantitative variables. In order to remove the distorting effect of the variables was carried out binary logistic regression at the multivariate model.
In multiple analyses, the variables which had a significant relationship (P < 0.05) or close to significant level (P < 0.2) with the dependent variable (sleep quality) were entered into the model with the enter method. For explicating the intensity of correlation in the final model, the Odds ratio (OR) was utilized and the significance level was considered as 0.1. Fitness of model was confirmed with the Hosmer and Lemeshow test.
RESULTS
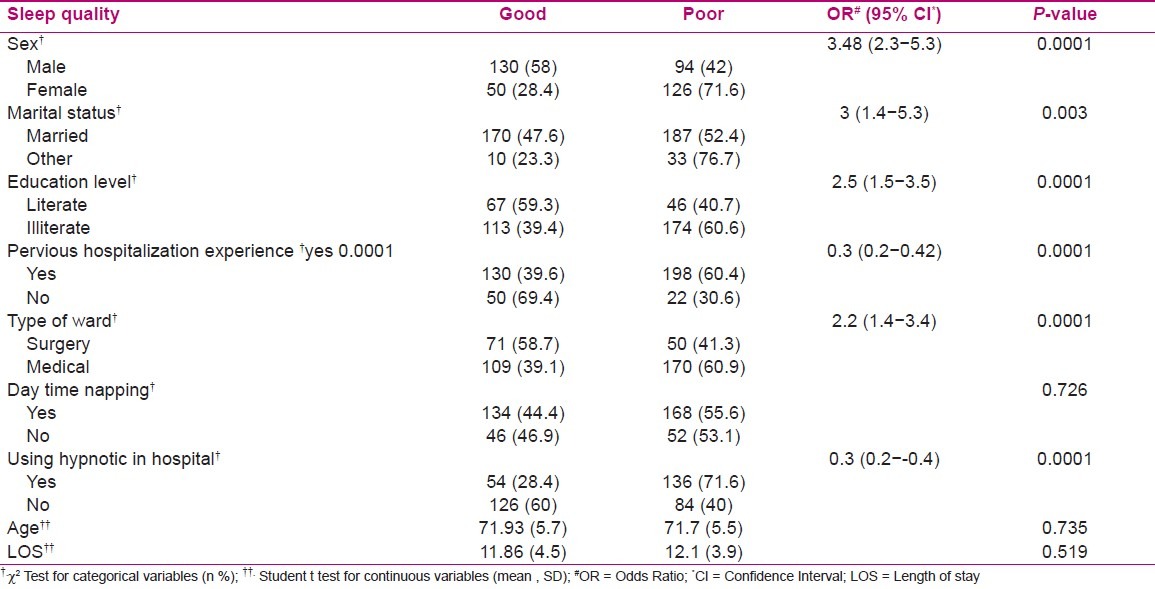
Four hundred hospitalized older patients with an average age of 71.8 (5.6) participated in this study. The average of total score of sleep quality of the patients was 7.3 (4.8) and 220 subjects (55%) had a poor sleep quality. The mean score of sleep quality was 10.9 (3.5) in the subjects with poor sleep and 2.9 (1.3) in group with good sleep quality. The demographic and clinical characteristic of patients is stated in [Table 1] according to sleep quality. In univariate analysis, significant difference was observed among sleep quality and gender (P < 0001), marital status (P < 003), literacy level (P < 0001), previous hospitalization experience (P < 0001), type of ward (P < 0001), and the using hypnotic in hospital (P < 0001). However, gender, LOS and day time napping did not have significant relationship with sleep quality.
Table 1.
Characteristics of the 400 hospitalized older adult patients in the study according to sleep quality
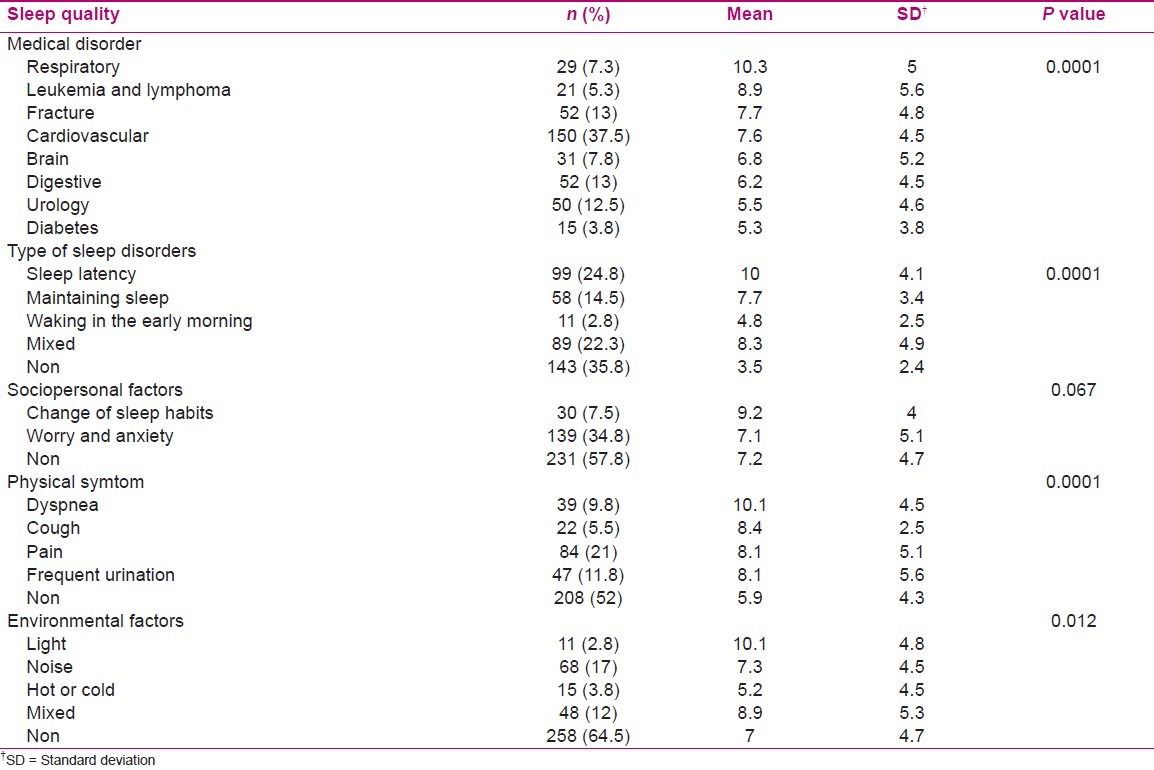
The mean score of sleep quality did have a significant relationship with the medical disorder (P < 0001). The most important diseases that had negative effect on sleep quality were the respiratory complications. The mean score of sleep quality had a significant relationship with the type of sleep disturbance (P < 0001); those individuals who had delay in sleeping had a poor sleep quality. The mean score of sleep quality had statistically significant relationship with physical (P < 0001), and environmental factors (P < 012) but did not have a significant relationship with sociopersonal factors [Table 2]. The highest mean score of sleep quality in the sociopersonal dimension was sleep habits change, in the physical dimension was dyspnea and at environmental dimension was light.
Table 2.
The quality of sleep scores (mean ± SD) of hospitalized older adults according to medical disorder, type of sleep disorders and sociopersonal, physical, and environmental factors
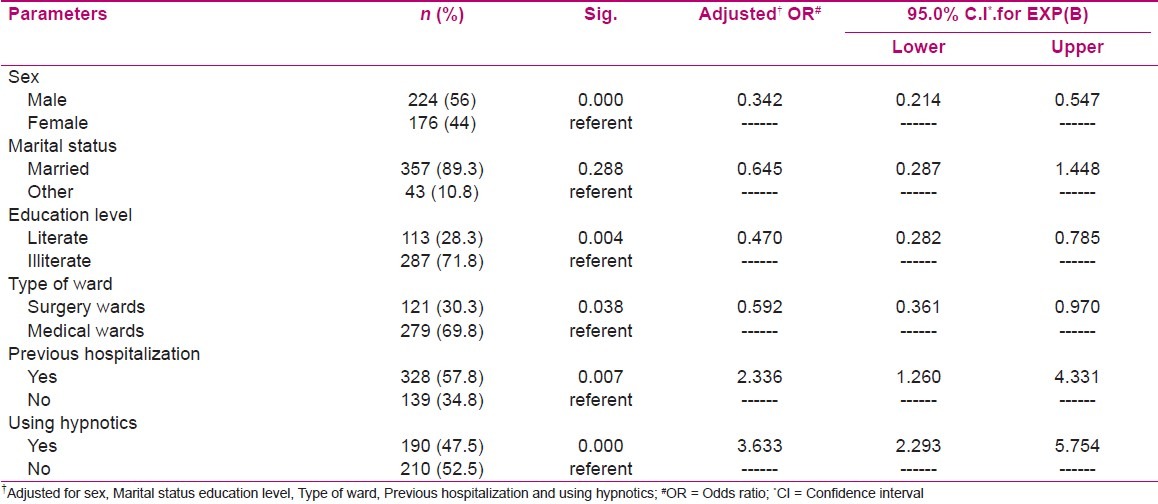
In multivariate analysis, the variables of gender (OR = 0.342), literacy level (OR = 0.470), type of ward (OR = 0.592), previous hospitalization experience (OR = 2.336), using hypnotic in hospital (OR = 3.633) stayed in the model that had a statistical relationship with the sleep quality [Table 3.]
Table 3.
Multiple logistic regression model for determining the predictors of sleep quality in hospitalized older adult patients
DISCUSSION
This study was conducted to evaluate the quality of sleep in the hospitalized elderly. The results showed that more than half of the hospitalized older adults had poor sleep quality. Previous studies have shown that aging is accompanied with changes in the circadian rhythm, sleep structure and its quality.[5] These changes are intensified with hospitalization.[5] In addition, the hospitalized patients spend a long time in bed, during the day, which interferes with their circadian rhythm and night sleep.[25] However; some researchers argue that this is not a result of the aging process per se. The sleep disturbances experienced with the increase of age can be linked to the increase of medical problems and life style changes. [2] This may specially be true for the hospitalized older adults.[26] According to Dogan et al., hospitalized older adults had a lower sleep quality than nonhospitalized controls.[19] The results of Lei et al. was almost similar to this study.[2] It is also generally known that the hospital environment could negatively affect the sleep quality. Several factors have contributed to this negative effect such as changes in the patients’ normal environment, temperature, noise produced by machines and staff, anxieties and worries in relation to illnesses and not carrying out their home responsibilities, pain, breathing problems, pre- and postsurgical problems and lack of physical activity.[3,19,27,28]
Gender was one of the significant factors in sleep quality. We found that the chance of having a good sleep quality was more in men than women. This finding was consistent with the results of Kiejna et al. who reported that gender was one of the four factors related to sleep disorder.[29] Researchers have also shown that hormonal changes have an important role in structural changes of sleep among older women.[30,31]
This study found that sleep quality of married older adults was better than divorced or widowed persons and individuals who were living alone. Kiejna et al. have also found that being divorced results in sleep disorders in the population over 65 years of age.[29] Also widowhood increases the risk of insomnia in the older people.[32] Ohayon et al. have also reported that being divorced and widowed or being single are important risk factors for sleep problems.[33] Adib-Hajbaghery and Akbari have also reported that amount and quality of social support significantly affect the old peoples’ health and disability.[34] Thus, the single older adults with lack of social relations may be more susceptible to decline than others. Therefore, we may conclude that the lack of familial and social support can negatively affect the sleep quality of the older patients.
Our study found that poor sleep quality was associated with the low education level. The highest mean PSQI score was for illiterate individuals. Several previous researchers have also reported that socioeconomic factors such as education level, occupation, and income have significant relationship with sleep quality.[19,35–38] It seems that illiterate persons are less familiar with problem solving methods. Also the economical situation of these individuals is inappropriate and hospitalization exerts an additional load on the household’s economy that results in more stresses and sleep disturbance.
This study a significant relationship was observed between sleep quality and the type of ward. Patient in surgical wards had a better sleep quality than patients in medical wards. This finding was in contrast to the findings of some of previous studies, that the sleep quality of patients in medical units was better than that of patients in surgical units.[20,30,39,40] Although fear of being in a strange environment, anxieties related to the illness, and pre- or postsurgical periods may negatively affect the sleep quality, our patients in medical units were frequently suffering of problems such as dyspnea, cough, and nocturia that cannot be easily eradicated and therefore have negatively affected their sleep quality.[41] On the other hand, the most popular problem in surgical units was pain that perhaps was treated with analgesics. Therefore, the patients in surgical units had a better sleep quality than the ones in medical units.
Sleep quality of the older patients who had previous hospitalization experience had been reduced 2.33 times that is congruent with the results of other studies.[21,42] The reason for this issue might be the sense of hopelessness due to treatment of chronic illness in the older patients. It seems that the effect of prior hospitalization on sleep quality ought to be examined more.
This study showed that the sleep quality of older patients who took hypnotic had been reduced 3.63 times. Using hypnotic for a long time had a reversal effect on sleep quality.[25,43] Nurses should also assess the elderly patients’ sleep habits and provide them before the prescription of hypnotics or sedative drugs.[26] On the other hand, medications with limited said effects and a low dosage should be used for the elderly people.[44]
Results of this study, same as other studies, did not show any relationship between the duration of stay and the sleep quality.[19,26] However, in Cara et al. and Frighetto et al. studies, the LOS had a negative effect on sleep quality.[41,43] The reason for this difference might be due to different abilities of adaptation among the older individuals in different regions of the world or it might be due the difference in design of studies.
No significant relationship was found between sleep quality and daytime napping that is congruent with Lai’s study.[42] Daytime napping would increase with age because the older adults have an increased opportunity to nap.[11]
We observed a significant relationship between quality of sleep and type of sleep disorder. Patients with sleep latency had the highest mean of the PSQI score. Previous studies have also shown that difficulty in falling asleep or in maintaining sleep is common among the older adults and may result in poor sleep quality, increased probability of falls, decreased concentration and memory, and overall decrease in quality of life.[32,45,46]
In this research, the sleep quality was worse among the patients who suffered from respiratory diseases compared with the other diseases. In addition, considering the physical symptoms, the lowest sleep quality was related to the patients with dyspnea. It seems that respiratory diseases create more persistent symptoms such as cough and dyspnea that not only require frequent interventions by the nursing staff, but also interfere with the onset or maintenance of sleep.[11]
We also observed a significant relationship between environmental factors with the sleep quality. Environmental noises were the most frequent sleep disturbing factors. However, environmental lights had the most negative effects on the PSQI mean scores. This finding was consistent with the report of Wooten who conducted a study on management of sleep disorders in the elderly.[47] Isaia et al. have also reported that the noises produced by other patients or their visiting relatives, environmental light, changes in sleep habits and nursing cares performed at night were among the most sleep disturbing factors for hospitalized elderly.[26]
CONCLUSION
Numerous factors may affect the sleep quality among the hospitalized older adults. This study showed that using hypnotics at hospitals, previous hospitalization experience, type of ward, literacy level, and gender were the most important factors affecting the sleep quality in the hospitalized elderly. Knowing these factors can assist nurses in proper planning and for preventing sleep disturbance of the older adults.
Some limitations of this study must be discussed. We did not have the information about the patients’ sleep before the elderliness and we did not examine the patients regarding the primary sleep disorders either.
ACKNOWLEDGMENT
This work was granted and approved by Kashan University of Medical Sciences. Therefore the authors would like to acknowledge of Kashan University of Medical Science for supporting this research. We also would like to thank of Masoomeh Salimiyn for her kind co-operations in collecting data.
Footnotes
Source of Support: Kashan University of Medical Sciences
Conflict of Interest: None
REFERENCES
- 1.Campbell SS, Stanchina MD, Schlang JR, Murphy PJ. Effects of a Month-Long Napping Regimen in Older Individuals. J Am Geriatr Soc. 2011;59:224–32. doi: 10.1111/j.1532-5415.2010.03264.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Foley D, Ancoli-Israel S, Britz P, Walsh J. Sleep disturbances and chronic disease in older adults: Results of the 2003 National Sleep Foundation Sleep in America Survey. J Psychosom Res. 2004;56:497–502. doi: 10.1016/j.jpsychores.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 3.Richards KC, Sullivan SC, Phillips RL, Beck CK, Overton-McCoy AL. The effect of individualized activities on the sleep of nursing home residents who are cognitively impaired: A pilot study. J Gerontol Nurs. 2001;27:30–7. doi: 10.3928/0098-9134-20010901-07. [DOI] [PubMed] [Google Scholar]
- 4.Reynolds CF, III, Regestein Q, Nowell PD. In: Clinical Geriatric Psychopharmacology. 3rd ed. Salzman C, editor. Baltimore, MD: Williams and Wilkins; 1998. p. 395.p. 416. [Google Scholar]
- 5.Reid KJ, Martinovich Z, Finkel S, Statsinger J, Golden R, Harter K, et al. Sleep: A marker of physical and mental health in the elderly. Am J Geriatr Psychiatry. 2006;14:860–6. doi: 10.1097/01.JGP.0000206164.56404.ba. [DOI] [PubMed] [Google Scholar]
- 6.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 7.Cotroneo A, Gareri P, Lacava R, Cabodi S. Use of zolpidem in over 75-year-old patients with sleep disorders and comorbidities. Arch Gerontol Geriatr Suppl. 2004;9:93–6. doi: 10.1016/j.archger.2004.04.015. [DOI] [PubMed] [Google Scholar]
- 8.Léger D, Poursain B, Neubauer D, Uchiyama M. An international survey of sleeping problems in the general population. Curr Med Res Opin. 2008;24:307–17. doi: 10.1185/030079907x253771. [DOI] [PubMed] [Google Scholar]
- 9.Ohayon MM, Zulley J, Guilleminault C, Smirne S, Priest RG. How age and daytime activities are related to insomnia in the general population: Consequences of older people. J Am Geriatr Soc. 2001;49:360–6. doi: 10.1046/j.1532-5415.2001.49077.x. [DOI] [PubMed] [Google Scholar]
- 10.Ravanipour M, Salehi S, Taleghani F, Abedi HA. Elderly self-management: A qualitative study. Iran J Nurs Midwifery Res. 2010;15:60–5. [PMC free article] [PubMed] [Google Scholar]
- 11.Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: An epidemiologic study of three communities. Sleep. 1995;18:425–32. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- 12.Fiorentino L, Ancoli-Israel S. Insomnia and its treatment in women with breast cancer. Sleep Med Rev. 2006;10:419–29. doi: 10.1016/j.smrv.2006.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aðargün MY, Kara H, Anlar Ö. The validity and reliability of Pittsburgh Sleep Quality Index [in Turkish] Turk Psikiyatri Derg. 1996;7:107–15. [Google Scholar]
- 14.Weinger MB, Ancoli-Israel S. Sleep deprivation and clinical performance. JAMA. 2002;287:955–7. doi: 10.1001/jama.287.8.955. [DOI] [PubMed] [Google Scholar]
- 15.Doraciak Y. Aspects of sleep. Nurs Times. 1990;287:38–40. [Google Scholar]
- 16.Smeltzer S, Bare B. Brunner and suddarth’s text book of medical- surgical nursing. 10th ed. Philadelphia: Lippincott Willams and Wilkins Co; 2004. p. 195. [Google Scholar]
- 17.Raymond I, Nielsen TA, Lavigne G, Manzini C, Choinière M. Quality of sleep and its daily relationship to pain intensity in hospitalized adult burn patients. Pain. 2001;92:381–8. doi: 10.1016/S0304-3959(01)00282-2. [DOI] [PubMed] [Google Scholar]
- 18.Lauri S, Lepistö M, Käppeli S. Patients’ needs in hospital: Nurses’ patients’ views. J Adv Nurs. 1997;25:339–46. doi: 10.1046/j.1365-2648.1997.1997025339.x. [DOI] [PubMed] [Google Scholar]
- 19.Dogan O, Ertekin S, Dogan S. Sleep quality in hospitalized patients. J Clin Nurs. 2005;14:107–13. doi: 10.1111/j.1365-2702.2004.01011.x. [DOI] [PubMed] [Google Scholar]
- 20.Potter PA, Perry AG. Fundamentals of Nursing. Philadelphia, PA: Mosby Year Book; 1993. p. 185. [Google Scholar]
- 21.Pfeiffer E. Short portable mental status evaluation questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–41. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 22.Roccaforte WH, Burke WJ, Bayer BL, Wengel SP. Reliability and validity of the Short Portable Mental Status Questionnaire administered by telephone. J Geriatr Psychiatry Neurol. 1994;7:33–8. [PubMed] [Google Scholar]
- 23.Meissner HH, Riemer A, Santiago SM, Goldman MD, Williams AJ. Failure of physician documentation of sleep complaints in hospitalized patients. West J Med. 1998;169:146–9. [PMC free article] [PubMed] [Google Scholar]
- 24.Gentili A, Weiner DK, Kuchibhatla M, Edinger JD. Test-re-test nursing home residents. J Am Geriatr Soc. 1995;43:1317–8. doi: 10.1111/j.1532-5415.1995.tb07415.x. [DOI] [PubMed] [Google Scholar]
- 25.Koch S, Haesler E, Tiziani A, Wilson J. Effectiveness of sleep management strategies for residents of aged care facilities: Findings of a systematic review. J Clin Nurs. 2006;15:1267–75. doi: 10.1111/j.1365-2702.2006.01385.x. [DOI] [PubMed] [Google Scholar]
- 26.Isaia G, Corsinovi L, Bo M, Santos-Pereira P, Michelis G, Aimonino N, et al. Insomnia among hospitalized elderly patients: Prevalence, clinical characteristics and risk factors. Arch Gerontol Geriatr. 2011;52:133–7. doi: 10.1016/j.archger.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 27.Hodgson LA. Why do we need sleep. Relating theory to nursing practice? J Adv Nurs. 1991;16:1503–10. doi: 10.1111/j.1365-2648.1991.tb01599.x. [DOI] [PubMed] [Google Scholar]
- 28.Southwell MT, Wistow G. Sleep in hospitals at night: Are patients’ needs being met? J Adv Nurs. 1995;21:1101–9. doi: 10.1046/j.1365-2648.1995.21061101.x. [DOI] [PubMed] [Google Scholar]
- 29.Kiejna A, Rymaszewska J, Wojtyniak B, Stokwiszewski J. Characteristics of sleep disturbances in Poland-results of the National Health Interview Survey. Acta Neuropsychiatrica. 2004;16:124–9. doi: 10.1111/j.0924-2708.2004.00063.x. [DOI] [PubMed] [Google Scholar]
- 30.Van den Berg JF, Miedema HM, Tulen JH, Hofman A, Neven AK, Tiemeier H. Sex Differences in Subjective and Actigraphic Sleep Measures: A Population- Based Study of Elderly Persons. Sleep. 2009;32:1367–75. doi: 10.1093/sleep/32.10.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kalleinen N, Polo O, Himanen SL, Joutsen A, Urrila AS, Polo-Kantola P. Sleep deprivation and hormone therapy in post menopausal women. Sleep Med. 2006;7:436–47. doi: 10.1016/j.sleep.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 32.Foley DJ, Monjan A, Simonsick EM, Wallace RB, Blazer DG. Incidence and remission -of insomnia among elderly adults. An epidemiologic study of 6,800 persons over three years. Sleep. 1999;22(Suppl 2):S366–72. [PubMed] [Google Scholar]
- 33.Ohayon MM, Caulet M, Priest RG, Guilleminault C. DSM-IV and ICSD-90 insomnia symptoms and sleep dissatisfaction. Br J Psychiatry. 1997;171:382–8. doi: 10.1192/bjp.171.4.382. [DOI] [PubMed] [Google Scholar]
- 34.Adib-Hajbaghery M, Akbari H. The severity of old age disability and its related factors. Feyz. 2009;13:225–34. [Google Scholar]
- 35.Adams J. Socioeconomic position and sleep quantity in UK adults. J Epidemiol Community Health. 2006;60:267–9. doi: 10.1136/jech.2005.039552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Friedman EM, Love GD, Rosenkranz MA, Urry HL, Davidson RJ, Singer BH, et al. Sioeconomic Status Predicts Objective and Subjective Sleep Quality in Aging Women. Psychosom Med. 2007;69:682–91. doi: 10.1097/PSY.0b013e31814ceada. [DOI] [PubMed] [Google Scholar]
- 37.Moore PJ, Adler NE, Williams DR, Jackson JS. Socioeconomic status and health: The role of sleep. Psychosom Med. 2002;64:337–44. doi: 10.1097/00006842-200203000-00018. [DOI] [PubMed] [Google Scholar]
- 38.Sekine M, Chandola T, Martikainen P, McGeoghegan D, Marmot M, Kagamimori S. Explaining social inequalities in health by sleep: The Japanese civil servants study. J Public Health (Oxf) 2006;28:63–70. doi: 10.1093/pubmed/fdi067. [DOI] [PubMed] [Google Scholar]
- 39.Tranmer JE, Minard J, Fox LA, Rebelo L. The sleep experience of medical and surgical patients. Clin Nurs Res. 2003;12:159–73. doi: 10.1177/1054773803012002004. [DOI] [PubMed] [Google Scholar]
- 40.Lei Z, Qiongjing Y, Qiuli W, Sabrina K, Xiaojing L, Changli W. Sleep quality and sleep disturbing factors of inpatients in a Chinese general hospital. J Clin Nurs. 2009;18:2521–9. doi: 10.1111/j.1365-2702.2009.02846.x. [DOI] [PubMed] [Google Scholar]
- 41.Þendir M, Acaroðlu R. Evaluation of night-time pain characteristics and quality of sleep in postoperative turkish orthopedic patients. Clin Nurs Res. 2011;20:326–42. doi: 10.1177/1054773811406110. [DOI] [PubMed] [Google Scholar]
- 42.Lai HL. Self-reported napping and nocturnal sleep in Taiwanese elderly insomniacs. Public Health Nurs. 2005;22:240–7. doi: 10.1111/j.0737-1209.2005.220307.x. [DOI] [PubMed] [Google Scholar]
- 43.Frighetto L, Marra C, Bandali S, Wilbur K, Naumann T, Jewesson P. An assessment of quality of sleep and the use of drugs with sedating properties in hospitalized adult patients. Health Qual Life Outcomes. 2004;2:17. doi: 10.1186/1477-7525-2-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Neubauer DN. Sleep problems in the elderly. Am Fam Physician. 1999;59:2551–7. 2559–60. [PubMed] [Google Scholar]
- 45.Bachman DL. Sleep disorders with aging: Evaluation and treatment. Geriatrics. 1992;47:53–6. 59–61. [PubMed] [Google Scholar]
- 46.Ancoli-Israel S, Ayalon L, Salzman C. Sleep in the elderly: Normal variations and common sleep disorders. Harv Rev Psychiatry. 2008;16:279–86. doi: 10.1080/10673220802432210. [DOI] [PubMed] [Google Scholar]
- 47.Wooten V. Evaluation and management of sleep disorders in the elderly. Psychiatr Ann. 1990;28:466–73. [Google Scholar]


