Abstract
Background and Objectives:
Preeclampsia is one of the main causes of maternal and fetal mortality. Despite numerous studies, its etiology is unknown. Recently there has been attention towards Folic acid. This study examined the association of Folic acid consumption and its serum levels with Preeclampsia.
Materials and Methods:
A case-control study conducted in Tabriz- Alzahra hospital. 52 preeclamptic women in 34-42 weeks and 52 normotensive pregnant women were studied from Jun to Nov 2009. Data was gathered through interview with the women and review of their medical records. Folic acid serum levels were measured by electrochemiluminescence method on Elecsys-2010 system using the Roche brand kit. Data were analyzed by t-test, chi-square, exact fisher and logistic regression.
Results:
46% of women in the case group and 71% in the control group regularly consumed Folic acid supplements before and during the first trimester of pregnancy. Frequency of correct pattern of Folic acid consumption in the case group were significantly lower than control group (P = 0.02). Findings about frequency of main food groups’ consumption containing folic acid indicated that the only mean difference between two groups was in relation to fruits (P = 0.002). The mean of Folic Acid serum levels in preeclamptic group was significantly lower than non- preeclamptic group [10.9 (3.9) vs. 13.6 (4.0) ng/ml, P = 0.001].
Conclusion:
it is recommended all health care providers educate clients especially high risk women about regular and timely consumption of supplements as well as food groups containing Folic acid specially fruits and its possible role in prevention of preeclampsia.
Keywords: Diet, Folic acid, Iran, preeclampsia, prenatal care
INTRODUCTION
Preeclampsia is one of the most important and common complications during pregnancy and is one of the main causes of maternal and fetal mortality[1] with variable prevalence in the world.[2,3] Studies performed in Iran reported that 1% to 8% of pregnant women suffer it.[4] Pregnancy-induced hypertension can result in damages on liver, brain and kidney in mothers and cause problems such as left ventricle insufficiency, reduced platelet, lyses of erythrocytes, cerebral hemorrhage and also early placenta abruption, preterm labor and increased fetal and neonatal mortality. Despite several decades of studies, it is not clear that which mechanism of pregnancy results in hypertension while blood pressure disorders are the most important unsolved problems in obstetrics.
Many factors such as genetic, nutritional and immunological factors and infections could be effective in leading to preeclampsia. Abnormal replacement of placenta, oxidative stress and abnormal function of endothelium in pathophysiology have been indicated, but its exact pathogenesis remains uncertain.[1,5]
During the last 10-20 years, there have been many changes in nutritional recommendations of pregnant women and the role of nutrition in controlling some problems of pregnancy such as blood pressure disorders have been studying by researchers.[6 Recently, there has been attention towards the role of Folic Acid.[7,8] Folic Acid with iron and Vitamin B12 play an important role in blood production and folate shortage can be the cause of many fatal disorders such as defects in neural tube defects like anencephaly and spina bifida.[9] Besides, Folic Acid has an important role on maintaining the tone of muscles of digestive system, improvement of neural system, skin, and hair and eyes health.[10] Liver and vegetables with dark green leaves like spinach, collard and broccoli are among the rich resources of Folic Acid.[11]
Folate deficiency can result from the more need of body for folate, insufficient intaking through dietary, more excretion by the body, metabolism disorders and also some medications that interfere with the body’s ability to use folate.[11,12] The recommended amount of Folic Acid consumption is 400 mg/day, but considering that this amount is not provided by the food,[11] it is recommended to prescribe supplement Folic Acid for all women who want to be pregnant.[13]
Folic acid may decrease the risk of preeclampsia from different ways: Folic acid supplementation reduces the plasma homocysteine that is in relation to severe preeclampsia. In addition, Folic acid supplementation improves the function of endothelial cells as one of the pathogen agents of preeclampsia.[14,15]
Although many studies have been performed about Folic Acid deficiency during pregnancy and increasing the risk of neural tube defects and it has been reported that 70% of these defects could be prevented through fortifying the foodstuff with folate besides the effect of daily consumption of Folic Acid in prevention from miscarriage, placenta abruption, improvement of fetus growth, reduction of lip and palate cleft risk have been documented,[16] however many contradictory results have been published about the role of Folic Acid in preeclampsia. Such that some studies have shown the positive effects of supplements in prevention from preeclampsia and some have rejected such effect.[17,19] Moreover, contradictory results have been shown regarding the relation between serum levels of Folic Acid and preeclampsia.[20,21]
Considering the high rate of preeclampsia and the importance of maternal, fetal and infancy complications resulting from it and also considering the importance of Folic Acid consumption during pregnancy and its probable role in prevention from preeclampsia, this study was carried out to determine the relation between consumption and serum levels of Folic Acid with preeclampsia among pregnant women.
MATERIALS AND METHODS
This was a case-control study which conducted in Al-Zahra educational hospital at 2009, the main center for complicated pregnancies, from June 2009 to November 2009 in Tabriz. Study setting included the High Risk ward, delivery room, clinic, and post partum ward of Al-Zahra educational hospital in Tabriz. This center was selected because it has been located at the center of the city and since it is a referral center for high risk pregnancies and an educational and treatment center which people from different social classes refer there. The study population included the normal pregnant women and preeclamptic women aged 18-35 years and pregnancy age of 34 to 42 weeks who had singleton pregnancy. The sample size was calculated 47 persons using the JAVA software and considering the SD1 = 3.1, SD2 = 5.1, mean difference = 2.6, power = 0.9 and α = 0.05 that by considering drop outs of 10% in sample size, it was regarded 52 persons.
52 preeclamptic women aged 18-35 in 34 to 42 weeks through available sampling and 52 normotensive pregnant women after matching according to age (the groups of 18-25, 26-29, and 30-35) number of pregnancies (first, second or third, fourth or more) and pregnancy age (34-36, 37-39 and 40-42 weeks) from clinic of Al-Zahra educational hospital in accordance with the aims were selected. Inclusion criteria for research in two groups were: intention in participation, mother age of 18-35, and lack of any illness in the following cases (cardiac, thorax, renal, neural, enteric, diabetes, addiction, mental disorder, organic disorder, depression, lack of genitourinary disorder) according to mother’s words and not using drugs because of any aforementioned illnesses, singleton pregnancy, pregnancy age of 34 to 42 weeks, lack of cigarette smoking or drug addiction, previous preeclampsia, preterm labor, mole hydatidifrom, records of stillbirth in the previous pregnancy. Both members must not have any placenta previa or fetal abnormality and or using aspirin, calcium or vitamin E (more than the content of multivitamin) in the recent pregnancy. The members of case group must have blood pressure higher than 140/90 mmhg and their proteinuria must be positive and the members of control group must be without any preeclamptic problems.
Measuring the blood pressure was carried out using the one mercuric set and proteinuria tests were done in the cases of not having any lab results and by sending the records of urine to be analyzed. The qualitative tests of protein according to the plus stripe test were carried out in all members of the group.
In order to determine the consumption pattern of folic acid supplements, correct pattern of consumption was used to women who were taking it before pregnancy or by the end of the first trimester and continued during the second trimester, Incorrect pattern or late started is used to women who started taking folic acid supplements during the second trimester and continuing at least the end of second trimester, Early stop is used to women who started taking folic acid supplements at any time but discontinued before the end of the second trimester, and not using is used to women who did not take folic acid supplements during the pregnancy.[17]
In order to measure the serum levels of folic acid, 2 cc blood was prepared from arm vessel in the tube and after separating the serum, the samples were sent to Danesh lab to measure the serum levels of folic acid in the same day using the electrochemilouminescense method on Elecsys-2010 (JPN, Swiss) system using the Roche brand kit. Not being afflicted by preeclampsia in the control group through asking questions from mother and controlling the pregnancy records and testing the blood pressure, and doing proteinuria tests was determined in sampling. The individuals participating in the study were controlled during delivery and 24 hours after delivery and if they lost the condition, they were excluded from the research. According to the similar studies and considering that it doesn’t take much time to control the patients from the 34th week until the delivery and in most cases treating the preeclampsia in the same time is termination of pregnancy, sampling was carried out from the 34th week to 42nd.
Data collection tools in the present study was a questionnaire prepared by the team, that through questioning the participants and studying the records of the patient in demographic field, the history of preeclampsia, the history of obstetric, blood pressure, proteinuria and taking the foods containing folic acid, and information concerning the neonate after birth, the questionnaires were filled out. In order to determine the mean and standard deviation of the frequency of using main food groups in both case and control group, first all food uses in day, week, month or year were changed to week and for each group the mean and standard deviation was calculated separately by using T test. In order to determine the validity of scientific tools the content validity method through asking the ideas of nutrition experts and midwives and obstetricians were used, to determine the reliability of the test methods in lab in the primary study, 2 separate sample were prepared from the 5 participants in two different name and without inserting the name of the group and the results were determined by Pearson Correlation Coefficient. The correlation rate of 0.93 was accepted. In order to determine the reliability of the questionnaire in relation to foods containing folic acid and supplements having it, test-retest was used. First the questionnaire was given to 10 participants then, after 10 days the questionnaire was filled out again by them, the results of the correlation tests were compared, and the correlation rate of 0.82 was accepted. The analyses of the data using t, chi-square and logistic regression tests through SPSS/ver.13 software were carried out. Before data collection, ethical satisfaction form was given to the study subjects and written consent also was received and voluntariness and confidentiality of the information were emphasized, and participants were informed that, the results could be given to them, either.
RESULTS
There was no statistical significant difference between the mean age of the both case and control groups [29.0 (4.5) VS. 28.3 (4.7), P = 0.5] also there was no statistical significant difference between Gravida and Para in both groups (P > 0.05). One third of the participants in each group had the experience of abortion and pregnancy in 75% of the case group and 81% of the control group was planned before. There was no significant difference between the body mass index of both groups (P > 0.05).
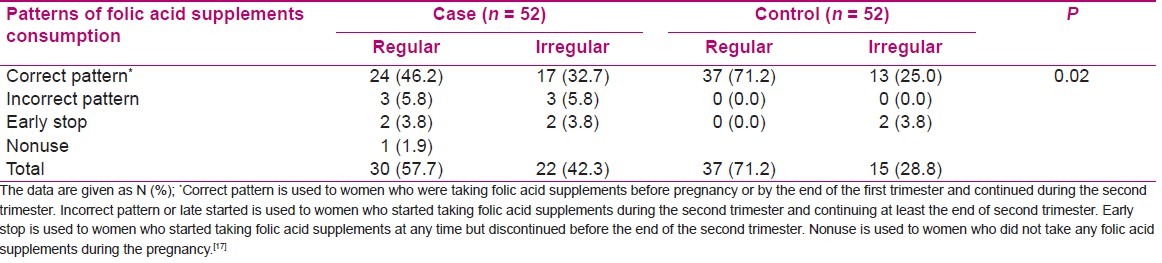
In order to determine the correlation between the consumption pattern of the folic acid supplements and preeclampsia considering the low number of samples in three groups, the late using, early stopping and non using, correct use (regular use before pregnancy or by the end of the first trimester) of the supplements in one group and irregular use, late use or early stopping or non using them in the other group was classified. The results showed that frequency of correct use of folic acid supplements in case group was significantly lower than control group (46% VS. 71%, P = 0.02)[Table 1].
Table 1.
Patterns of folic acid supplements consumption in case (preeclamptic women) and control (non-preeclamptic women) groups
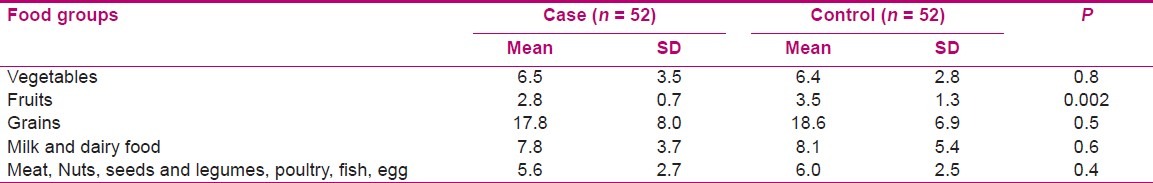
Comparing the mean frequency of main food groups consumption containing folic acid (vegetables, fruits, Grains, Milk and dairy foods, meat, Nuts, seeds and legumes, poultry, fish, egg) indicated that the only mean difference between two groups was in relation to fruits. The use of fruits in preeclampatic participants was significantly lower than control group (P = 0.002)[Table 2].
Table 2.
Frequency the consumption of main food groups containing folic acid in week in case and control groups
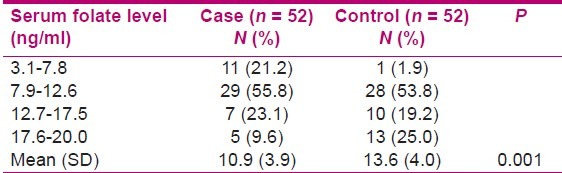
[Table 3] shows the serum levels of folic acid in preeclampatic and the non- preeclampatic women, the mean of folic acid serum levels in case group was significantly lower than non-preeclamptic group [10.9 (3.9) VS. 13.6 (4.0), P = 0.001].
Table 3.
Serum folate level in case and control groups
Using the analyses of logistic regression and controlling the interferer variables, blood group, the history of preeclampsia in the family and education level, there was a statistically significance relation between the serum levels of folic acid and preeclampsia. Increasing one unit of serum levels of folic acid, the risk of preeclampsia decreased significantly (OR = 0.88, CI 95%: 0.77-0.99). Also using the analyses of logistic regression by controlling the mentioned interferer variables and using fruits containing folic acid it was determined that among the persons who had experienced the irregular use of supplements, whether early or late, early stop and nonuse of supplements containing folic acid comparing participants who had used supplements correctly, the risk of afflicting by preeclampsia increased 2.2 times. Although this relation was not statistically significant (OR = 2.2, CI 95%: 0.9-5.6).
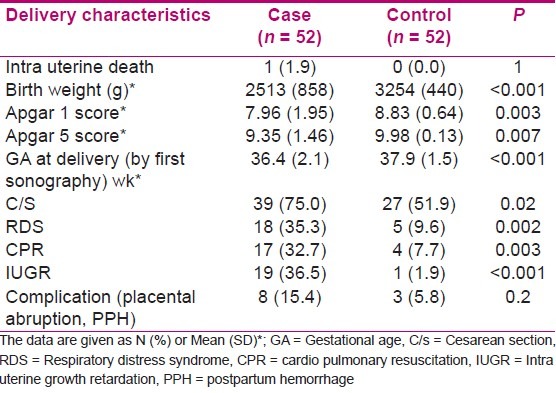
There were a significant difference between the following cases; birth weight (g), minute 1 Apgar score, minute 5 Apgar score, gestational age at delivery (according to the ultrasonography in the first weeks), type of delivery, respiratory distress syndrome, need for resuscitation in birth, and intra uterine growth retardation (IUGR) (P < 0.05)[Table 4]
Table 4.
Characteristics of the newborn in case and control groups
DISCUSSION
In the present study, 71 percent of the women in control group and 46 percent of the case group had started to use folic acid before and during the first trimester of the pregnancy. In the research of the Shahnazi et al only 20 percent of the pregnant women had used folic acid during the first trimester of the pregnancy.[23] This difference is related to the women’s evocation and increase in pregnant women’s cares and more recommendation in using the supplements with folic acid before or during the pregnancy in the form of incorporated cares of mothers’ health.
Moreover, the results showed that the frequency of correct and regular use of supplements containing folic acid in the case group was significantly lower than the control group. The studies of Hernandez et al in America and Canada[16] shows that the risk of preeclampsia among the individuals who had used folic acid early was 9.2% and it was 12.9% among the group who had not used supplements and using folic acid supplements reduced the risk of pregnancy induced hypertension (RR = 0.55, CI 95%,: 0.39-0.79).[17] In the research of Wen et al in Canada,[18] using folic acid supplements in the early second trimester of the pregnancy decreased the risk of preeclampsia. The rate of preeclampsia in folic acid supplement users was 2.2 percent and in non-users it was 5.1 percent that corresponds to the present results (OR = 0.37: CI 95%: 0.18-0.75).
The only mean difference in frequency of main food groups’ consumption between two groups was in relation to fruits. The use of fruits in preeclampatic participants in week was significantly lower than control group. There were not found any similar studies in this regard.
Food sources are not able to supply all the needs of the body to folic acid, since folic acid is readily destructed because of constant heat, unsuitable preparation and maintenance of the food. Considering that, all suppliers in the U.S are obliged to fortifying the food with folic acid and this FDA recommendation was applied by the aim of increasing the social health on some women which were not under the prenatal care or were unaware of the importance of using folic acid for preventing of congenital malformations, however, in adults it was along with the improvement in the condition of hyper homocysteinemia (hyper homocysteinemia is observed in the patients afflicted by preclampsia, eclampsia and placenta failure).[9,24] Then, fortification the food by folic acid could be used in the nutrition planning programs in society. Moreover, prescribing supplements containing at least 400-microgram folic acid daily for all women in reproductive years planning pregnancy is suggested in order to use its influence on preventing the preeclampsia, fetal malformation, preterm labor and low birth weight and to economize the budget of the country.
In the present research, there is a significant difference between the serum level of folic acid in both case and control group. Moreover, there was a reverse correlation between the serum level of the folic acid and frequency of the preeclampsia. Makedos et al.[20] in their study did not find any significant difference between the serum level of folic acid in case and control groups. Acilmis et al.[22] in their study showed that serum level of folic acid in case group is less than control group that confirm the results of the present study, Although this difference was not statistically significant. However, Kale et al.[21] and Mahmood et al.[25] illustrated in their studies that the serum level of folic acid in case group significantly is less than the control group that confirms the results of the present research. All the mentioned four studies are case -control study among which the sample size of Mahmood et al. (79 case and 113 control) and Kale et al (74 case and 100 control) are the most one. In the first two studies, the sample size was less than the present study.
Present study showed that mean of birth weight, 1 minute Apgar score, 5 minute Apgar score and gestational age at delivery in the case group is significantly less and frequency of caesarian section, respiratory distress syndrome in birth, need for resuscitation, and intra uterine growth retardation (IUGR) is significantly more than control group that confirms other results[20,21,26–29] and shows the undesirable neonate outcomes in preeclamptic mothers.
One of the restrictions of the present study is the low size of the samples and samplings in one center. Among the other restrictions, we could refer to not separating the preeclampsia severity in case group. Thus, it is suggested to carry out more studies by the aim of determining the relation of preeclampsia severity with using and level of folic acid serum in pregnant women in several centers and with large sample size. Moreover, the rate of folic acid in food of case and control groups can be studied and its relation with folic acid serum level be analyzed. If there is not any relation, thus, its reasons such as inactivity of folic acid during preparation process, and using food could be studied. The results of the present study could not be generalized to twin’s pregnancies, smoking ones and women with molehydatidform. Because of ethical considerations, conducting clinical research on effect of folic acid in pregnant women was impossible.
CONCLUSION
Considering the results of the present research for recognizing the probable factor related to preeclampsia, we could conclude that although folic acid is not the only element in preventing the preeclampsia, however, its serum level in case group is significantly less than control group. Therefore, on time start and regular continuous using of supplements containing folic acid notably reduces the risk of preeclampsia. it is recommended that all health care providers educate clients especially high risk women about the importance of Folic acid, regular and timely consumption of supplements as well as food groups containing Folic acid specially fruits and its posible role in prevention of preeclampsia during counseling. Considering that main percent of the case group did not have any correct consumption pattern of supplements containing folic acids, then health care providers using proper educational methods must encourage the women in reproductive years who planning pregnancy to use and follow the correct pattern of the supplements consumption.
Footnotes
Source of Support: None
Conflict of Interest: None.
REFERENCES
- 1.Cunningham F, Gant NF, Levenok J, Glistrap LC, Hauth JC, Wenstrom KD. Williams Obstetrics. New York: McGraw-hill publisher; 2005. pp. 5–7.pp. 883–936.pp. 1042 [Google Scholar]
- 2.Burrow GN, Duffy TP, Copel JA. Medical complication during pregnancy. Philadelphia: WB Saunders; 2004. pp. 43–54. [Google Scholar]
- 3.Szmidt-Adjde V, Vendittell F, David S, Bredent-Bangou J, Janky E. Calciuria and pre-eclampsia: A case-control study. Eur J Obstet Gynecol Repord Biol. 2006;88:130–5. doi: 10.1016/j.ejogrb.2005.06.029. [DOI] [PubMed] [Google Scholar]
- 4.Safari M, Yazdanpanah B. Prevalence and Maternal and prenatal complication in pre-eclamptic women referring to EMAM SAJJAD birth center of Yasouj. J Shahrekord Univ Med Sci. 2003;5:47–52. [Google Scholar]
- 5.Helal O, Defoort C, Robert S, Martin C, Lesavre N, Lopez-Miranda J. Increased levels of microparticles originating from endothelial cells, platelets and erythrocytes in subjects with metabolic syndrome: Relationship with oxidative stress. Nutr Metab Cardiovasc Dis. 2011;21(9):665–71. doi: 10.1016/j.numecd.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Dudek G. Nutrition Essential for Nursing Practice. Philadelphia: Lippincott Publisher; 2001. pp. 286–308.pp. 102–12. [Google Scholar]
- 7.Rabinson JM. In: Essential of Nutrition and Nutrition Therapy. Gorbani A, editor. Tehran: Shahrab Publisher; 2002. pp. 50–64. [Google Scholar]
- 8.Felicia D, Chikita Fredy F, Jayadi Iskandar W. Folic Acid Supplementation as Preeclampsia Prevention on Pregnant Women in Indonesia. JIMKI. 2010;1:1. [Google Scholar]
- 9.Katzung BG. In: Basic and Clinical Pharmacology. Sohrevardi SH, editor. 2006. pp. 656–9. [Google Scholar]
- 10.Murry R, Granner M, Rodwell A. In: Harper’s illustrated Biochemistry. Arianmehr S, editor. Tehran: Teymourzadeh; 2006. pp. 543–61. [Google Scholar]
- 11.Mahan KL, Stump ES. Krauses Food and Nutrition Therapy. Philadelphia: Saunders Elsevierh; 2008. pp. 90–92.pp. 177pp. 178pp. 183pp. 184pp. 823–827.pp. 1287 [Google Scholar]
- 12.Wikipedia, the free encyclopedia. Folate deficiency. 2011. [Last accessed on 2011]. Available from: http://en.wikipedia.org/wiki/Folate_deficiency .
- 13.Valafar SH, Emami Afshar N, Jafari N, Jalilvand P, Changizi N, Habibolahi A, et al. Maternal health care program in the Islamic Republic of Iran. The Ministry of Health and Medical Education. Department of Family Health and population, Office of Mothers Health. 2008:4–9. [Google Scholar]
- 14.Levine NH, Lyon Daniel K, Mulinare J. Folic Acid and preconceptional care. Prim Care Update Ob Gyns. 2001;8:78–81. doi: 10.1016/s1068-607x(00)00079-2. [DOI] [PubMed] [Google Scholar]
- 15.Tug N, Celik H, Cikim G, Ozcelik O, Ayar A. The correlation between plasma homocysteine and malondialdehyde levels in preeclampsia. Neuro Endocrinol Lett. 2003;24:445–8. [PubMed] [Google Scholar]
- 16.Hernandez-Diaz S, Werler MM, Louik C, Mitchell AA. Risk of gestational hypertension in relation to Folic acid supplementation during pregnancy. Am J Epidemiol. 2002;156:806–12. doi: 10.1093/aje/kwf129. [DOI] [PubMed] [Google Scholar]
- 17.Lindzon G, O’connor DL. Folate during reproduction: The Canadian experience with Folic acid fortification. Nut Res Pract. 2007;1:163–74. doi: 10.4162/nrp.2007.1.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wen SW, Chen XX, Rodger M, White RR, Yang Q, Smith GN, et al. Folic acid supplementation in early second trimester and risk of preeclampsia. Am J Obstet Gynecol. 2008;198:1–7. doi: 10.1016/j.ajog.2007.06.067. [DOI] [PubMed] [Google Scholar]
- 19.Wikipedia, the free encyclopedia. Levomefolic acid. 2011. [Last accessed on 2011]. Available from: http://www.en.wikipedia.org/wiki/Levomefolic_acid .
- 20.Makedos G, Papanicolaou A, Hitoglou A, Kalogiannidis I, Makedos A, Vrazioti V, et al. Homocysteine, folic acid and B12 serum levels in pregnancy complicated with preeclampsia. Arch Gynecol Obstet. 2007;275:121–4. doi: 10.1007/s00404-006-0223-2. [DOI] [PubMed] [Google Scholar]
- 21.Kale A, Kale E, Akdeniz N, Erdemuglu M, Yalinkaya A, Yayla M. Investigation of Folic acid, vitamin B12, vitamin B6 and Homocysteine levels in preeclamptic pregnancies. J Perinat Med. 2006;14:31–6. [Google Scholar]
- 22.Acilmis YG, Dikensoy E, Kutlar AI, Balat O, Cebesoy FB, Ozturk E, et al. Homocysteine, folic acid and vitamin B12 levels in maternal and umbilical cord plasma and homocysteine levels in placenta in pregnant women with pre-eclampsia. J Obstet Gynecol Res. 2011;37:45–50. doi: 10.1111/j.1447-0756.2010.01317.x. [DOI] [PubMed] [Google Scholar]
- 23.Shahnazi M, soltanzadeh M, gahvechi chai peyma A. Knowledge assessment about importance of folic acid consumption among pregnant women, Tabriz. Proceeding of nutrition congress of Tabriz University of Medical Sciences; research center publisher, Tabriz, Iran. 2006. p. 268. [Google Scholar]
- 24.Herrmann W, Hubner U, Koch I, Obeid R, Retzke U, Geisel J. Alteration of homocysteine catabolism in preeclampsia, HELLP syndrome and placental insufficiency. Clin Chem Lab Med. 2004;42:1109–16. doi: 10.1515/CCLM.2004.228. [DOI] [PubMed] [Google Scholar]
- 25.Mahmoud A, Elkattan E, Eldaly A, Omran E, Mandour I. A comparative study of folate and vitamin B12 serum levels in preeclamptic versus normotensive pregnant women in correlation with uterine and umbilical artery Doppler findings and pregnancy outcome. Turkish-German Gynecol Assoc J. 2009;10:152–7. [PMC free article] [PubMed] [Google Scholar]
- 26.Fathnejad-Kazemi A, Sehati F, Sattarzade N, Ebrahimi M. Predictive Value of Urinary Calcium to Creatinine Ratio, Roll-Over Test and BMI in Early Diagnosis of Pre-Eclampsia. Res J Biol Sci. 2010;5:183–6. [Google Scholar]
- 27.Abbade JF, Peracoli J, costo R, Calderon I, Borges V, Rudge M. Partial HEELP syndrome: maternal and perinatal outcome. Sao Paolo Med J. 2002;120:1123–30. doi: 10.1590/S1516-31802002000600005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ingec M, Borecki B, Kadanali S. Elevated plasma homocysteine concentration in sever preeclampsia. Tohoku J. 2005;206:225–31. doi: 10.1620/tjem.206.225. [DOI] [PubMed] [Google Scholar]


