Abstract
Purpose
To use direct observations of first prenatal visits to describe obstetric providers’ adherence to the evidence-based clinical practice guideline for smoking cessation counseling recommended by the American College of Obstetricians and Gynecologists, the 5 A's (Ask, Advice, Assess, Assist and Arrange).
Design
Observational study using audio-recordings of first obstetric visits.
Setting
An urban academic hospital-based clinic.
Participants
Obstetric care providers and pregnant women attending their first obstetric visit..
Methods
First obstetric visits were audio recorded. Visits were identified in which patients reported smoking, and discussions were analyzed for obstetric providers' use of the 5 A's in smoking cessation counseling.
Results
Obstetric providers asked about smoking in 98% of the 116 visits analyzed, but used 3 or more of the 5 A’s in only 21% (24) of visits. In no visits did providers use all 5 A's. In 54% of the visits, providers gave patients information about smoking; most commonly, about risks associated with perinatal smoking.
Conclusion
Few obstetric care providers performed the recommended 5 A's smoking cessation counseling with their pregnant smokers. Effective and innovative methods are needed to improve obstetric providers' use of the 5 A's.
Keywords: Communication, physician-patient relations, pregnancy, smoking, smoking cessation
Indexing Key Words: Manuscript format: Research, Research Purpose: descriptive, Study Design: Qualitative, Outcome Measure: behavioral, Setting: clinical/healthcare, Health Focus: smoking control, Strategy: skill building/behavior change, Target Population: adults, Target Population Circumstances: pregnant women
Purpose
Smoking during pregnancy is one of the most prevalent and preventable causes of maternal and infant morbidity and mortality in the United States.1–5 Despite this risk, 12 to 36% of women continue to smoke during pregnancy.6–9
Pregnancy can be a “teachable moment,” a time during which women are more receptive to behavior change.10–15 When obstetric care providers counsel pregnant smokers, they are more likely to quit smoking which improves pregnancy outcomes.16
The American College of Obstetricians and Gynecologists endorses use of the 5 A’s, an evidence-based, clinical practice guideline for smoking cessation.17–19 The 5 A's mnemonic reminds clinicians to: 1) Ask pregnant patients about smoking at every obstetric visit,20 2) Advise patients to stop smoking using clear, strong and personalized language, 3) Assess patients’ willingness to stop smoking and motivations to quit, 4) Assist patients to stop smoking by providing strategies and resources, and 5) Arrange specific follow-up to track patients’ progress.17, 18, 21–24 When clinicians use the 5 A’s in a variety of clinical settings including obstetrics, patients are more likely to quit smoking.24, 25
Prior studies examining provider adherence to these guidelines have all been self-reported data from surveys of obstetric care providers. These studies found rates as high as 100% of surveyed obstetric providers asked about smoking and advised smoking cessation and 30% reporting that they performed all 5 A's.26–28 However, multiple studies comparing physician self-report of recommended behaviors to other methods of assessment, such as chart audits, patient recall of provider behavior and direct observation, indicate that health provider self-report is very unreliable.29–31 No prior studies have directly observed obstetric care providers’ counseling patients about smoking. We examined audio recordings of first obstetric visits to describe providers’ adherence to the 5 A’s smoking cessation guidelines.
Design
Data from this analysis comes from two observational studies of 301 audio-recorded first obstetric visits. Fifty-one visits were from one study whose focus was patient-provider communication regarding behavioral risks (e.g., smoking, alcohol or drug use, mental health concerns, intimate partner violence, other forms of abuse/violence).32 The other 250 visits were from a study focusing on communication regarding intimate partner violence. Both studies were observational only; no interventions were tested.
Setting
The studies were conducted from January 2005 through April of 2009 in a hospital-based obstetrics and gynecologic outpatient clinic in an urban academic medical center in Pittsburgh, Pennsylvania. This first smaller study (N=51) began recruiting provider participants in January 2005 and patient subjects in May 2005 when more research staff was available to assist in recruitment. This first study recruited subjects using one part-time staff person until April 2006. The second study (N=250) began subject recruitment and data collection in October 2006 and finished in April 2009 and also relied on the efforts on one part-time staff person. The protocols for subject recruitment and data collection for both studies were the same and quality of recordings and other study data routinely checked and assured. Audio-recordings from the two studies were the same regarding study location, patient and provider populations, type of visit, recording equipment, sound quality, and study personnel.
Participants
Provider participants were eligible if they saw patients for first obstetric visits in the study setting. Patient participants were eligible if they spoke English, were 18 years of age or older, and did not have a third party with them (e.g., spouses, partners, family member) during their appointment. Provider and patient participants signed informed consent prior to participation. The projects were approved by the University of Pittsburgh Institutional Review Board (IRB # 0404143, 0602015). Patient participants provided socio-demographic information prior to audio recording the visits. Provider participants provided information on gender, race, training level and or years of practice.
Method
Audio recordings of first obstetric visits were examined to describe providers’ adherence to the 5 A’s smoking cessation guidelines. Digital voice recorders were placed in the clinic exam room at the beginning of the first obstetric visit and collected after the visit was completed. Two investigators reviewed and qualitatively coded all audio recordings to identify visits in which patients reported current tobacco use.
Recordings with patients who disclosed tobacco use were qualitatively coded for providers’ use of the 5A’s during the first obstetric visits. A codebook was developed based on the detailed descriptions of the 5 A's in the United States' Department of Health and Human Services' (DHHS) clinical guidelines "Treating Tobacco Use and Dependence: 2008 Update."19 Definitions and examples of each code are provided in Table 1. Each of the audio-recorded visits was reviewed for provider communication that correlated with use of any of the 5 A's. Frequencies were conducted on the number of visits in which each type of A was used, and the number of and type of A's used in each visit.
Table 1.
5A’s: Definitions and Examples
| Definition | Examples | |
|---|---|---|
| Ask | Physician asks the patient about current tobacco use status |
Do you currently use tobacco? Do you smoke? How would you describe your current smoking? |
| Advise | Physician provides the patient with clear, strong, and personalized advice to quit smoking |
Clear You need to stop smoking. It is important you quit smoking. Strong It is really important that you try to quit smoking. I think quitting smoking is critical for your health. Personalized … you need to quit for the health of your unborn child. … with small kids in the house, smoking is dangerous. |
| Assess | Physician verbally assesses patient’s readiness to quit |
Are you willing to give quitting a try? On a scale of 0 to 10 where 0 is not motivated at all and 10 is extremely motivated, how motivated are you to quit? |
| Assist | Physician provides brief counseling or self-help materials to help patient in their quit attempt. |
I am going to give the number to the quitline so you can use it. They have helped a lot of folks out and I think it would really be useful for you. What are some things you can do on your quit day to help you be successful? |
| Arrange | Physician arranges a follow-up visits or phone calls to review progress toward quitting. |
You come back in a month, but I would like to see you sooner to see how your quitting is going. Why don’t we schedule a follow-up visit to see how the quitting goes for you? |
Communication coded for any of the 5 A's was also analyzed for quality of the communication. The American Congress of Obstetricians and Gynecologists (ACOG) recommends the use of a multiple-choice question that increases rates of smoking disclosure, 18, 20 Thus, Ask communication was coded for whether the question was yes/no, open-ended or multiple-choice. The DHHS guidelines specify that Advice should be "clear, strong, and personalized." Advice met the criteria for being "clear" if it contained the pronoun "you" indicating advice directed to the patient herself and contained language that emphasized smoking cessation (e.g., "quit," "stop," "cut out") rather than reducing the amount of smoking. Advice was "strong" if it included language emphasizing the importance of smoking cessation (e.g. "very important," "crucial"). Advice was "personalized" when providers referred to something personally relevant to the patient's health, situation, past experiences or current circumstances to indicate how smoking cessation would impact them or their baby.
Instances of provider communication regarding smoking that did not fit within the definitions of any of the 5 A's were also noted. In all instances, this communication focused on giving the patient some form of smoking-related information. Thus, a code called "Giving Information" was created and applied it to these utterances. Visit time spent with the provider overall, on smoking communication, on each of the 5 A's and on "Giving Information" was also collected.
Two investigators (JC and CH) independently analyzed the audio recordings; over one-third of conversations (n = 43; 37%) were double-coded to assess inter-rater reliability. Disagreements were discussed and final decisions made by consensus. Inter-rater agreement was calculated using Cohen’s Kappa using Landis and Kock’s classification.33
Associations between each potential predictor and the outcomes of Advice, Assess, Assist, and use of 3 or more A’s were explored using the logistic model, with generalized estimating equations (GEE) employed to account for within-practice correlation. 34 The outcomes of Ask and Arrange could not be analyzed further because almost all physicians Asked, and almost none of the providers Arranged.
Results
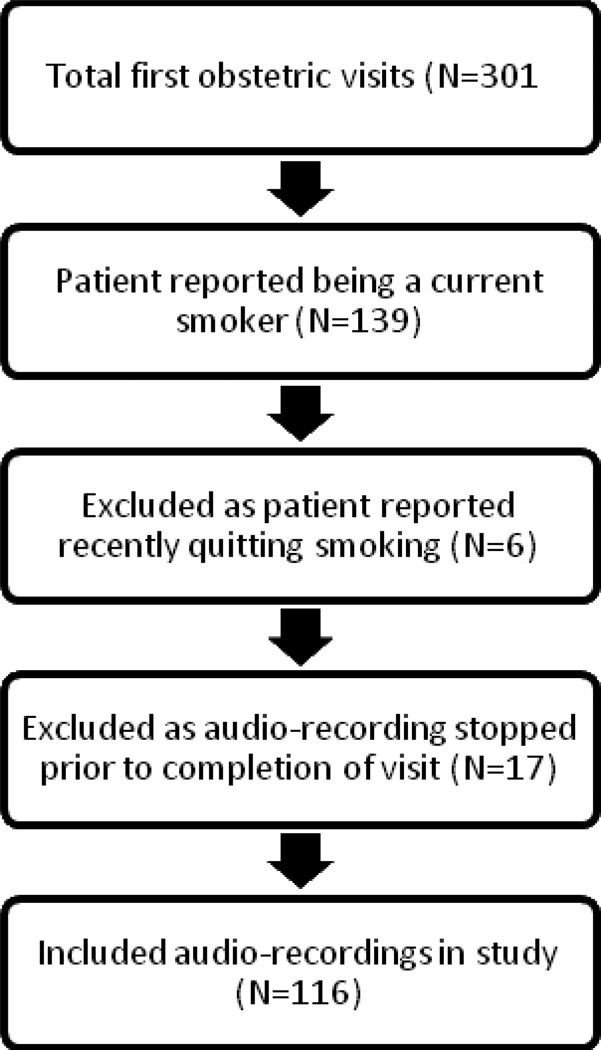
Of the 101 providers who were approached for the two studies, 71 (70%) consented. Of the 600 patients of these providers who were approached about participating in the studies, 301(50%) consented. The primary reason for refusal was patient desire to have their partner or another third party remain in the room during the visit. Of the 301 audio-recorded visits, in 139 visits the patient disclosed a history of smoking. We excluded 6 as the patient reported quitting prior to the visit. Another 17 visits were excluded from the analyses as the recording stopped prior to the end of the visit (e.g. during the physical exam); this left 116 audio-recorded visits in this analysis. (Figure 1).
Figure 1.
Study Flow Diagram
Most patients were single, White, and had completed high school. The mean age was 26 years old, and most had prior pregnancies. Of the 71 providers who consented, 48 providers had a visit audio recorded; almost all were women, and most were obstetrics and gynecology residents. Characteristics for both patient and provider participants are given in Tables 2 and 3, respectively.
Table 2.
Participant Characteristics
| Patient Characteristic | N(%) |
|---|---|
| Age (Mean Patient Age = 26 ± 5) | |
| <20 years | 7 (6) |
| 20–29 years | 84 (72.4) |
| 30–39 years | 24 (20.7) |
| 40 + years | 1 (0.9) |
| Marital Status | |
| Single | 96 (87.3) |
| Married | 8 (7.3) |
| Separated | 1 (0.9) |
| Divorced | 2 (1.8) |
| Widowed | 1 (0.9) |
| Living with same sex partner | 2 (1.8) |
| Ethnicity | |
| White | 66 (58.9) |
| African American | 42 (37.5) |
| Other | 4 (3.6) |
| Education | |
| Grade school | 5 (5.3) |
| High school or GED | 46 (48.4) |
| Some college | 30 (31.6) |
| Finished college | 9 (9.5) |
| Graduate school | 5 (5.3) |
| Type of provider who conducted visit | |
| Nurse midwife | 18 (15.5) |
| Nurse practitioner | 15 (12.9) |
| 1st year resident | 19 (16.4) |
| 2nd year resident | 16 (13.8) |
| 3rd year resident | 25 (21.6) |
| 4th year resident | 18 (15.5) |
| Physician Assistant | 5 (4.3) |
| Number of pregnancies | |
| First | 19 (16.7) |
| 2–4 pregnancies | 63 (55.3) |
| 5–7 pregnancies | 24 (21.1) |
| 8+ pregnancies | 8 (7.0) |
Table 3.
Provider Characteristics
| Provider Characteristic | N(%) |
|---|---|
| Age (Mean Provider Age = 31 ± 7) | |
| 20–29 years | 22 (62.9) |
| 30–39 years | 8 (22.9) |
| 40–49 years | 3 (8.6) |
| 50+ year | 2 (5.7) |
| Ethnicity | |
| White | 41 (91.1) |
| African American | 3 (6.7) |
| Other | 1 (2.2) |
| Gender | |
| Male | 3 (6.3) |
| Female | 45 (93.8) |
| Provider Type | |
| Nurse midwife | 8 (16.7) |
| Nurse practitioner | 4 (8.3) |
| 1st year resident | 10 (20.8) |
| 2nd year resident | 7 (14.6) |
| 3rd year resident | 9 (18.8) |
| 4th year resident | 9 (18.8) |
| Physician Assistant | 1 (2.1) |
All codes had substantial to near perfect agreement with kappas ranging from 92 to 99% agreement. In 98% of the audio-recorded first obstetric visits, an obstetric provider Asked about smoking. In the two visits in which the obstetric provider did not Ask, patients spontaneously disclosed current tobacco use prior to the provider asking. However, the providers in those visits did not ask any further details about the patient's smoking. When providers asked about smoking, all used a closed question generally intended to elicit a yes or no answer: "Do you smoke?" or "Any smoking this pregnancy?" No visits contained Ask communication that was either multiple-choice or open-ended.
In 36 visits (31%), providers Advised patients to quit smoking. In only 16 of these 36 (44%) visits was the Advice “clear.” An example of clear advice was, "We really want you to try to quit [smoking] altogether." An example of advice that was not clear was: "We don't recommend smoking, alcohol or drugs during pregnancy." In addition, in only 6/36 (17%) cases was the Advice “strong” with language emphasizing the importance (e.g. "very important," "crucial") of quitting smoking: "The best thing you can do for you and the baby is to quit smoking." More common examples of less strong advice included, "I’m sure you have heard this before, but we would recommend cutting back as much as possible and in a perfect world quitting smoking during pregnancy." However, many (23/36, 68%) personalized the advice to the patient, emphasizing how quitting smoking would benefit her pregnancy and baby: "Zero is better than three; every cigarette you don't smoke is good for the baby." In only 4/36 visits (11%) did providers give Advise in a clear, strong and personalized manner. For example: "It [quitting smoking] is the best that you can do for your health, and in this case, for the baby's health too. For you, just saying as a doctor, if you quit smoking--longevity-wise, your health--that is the best thing you can do for your health….So as much as I can, I encourage it."
In 26 visits (22%), providers Assessed patients' willingness or motivation to quit smoking. When providers Assessed, the conversation focused primarily on the patient's willingness to quit smoking, for example, "Are you interested in quitting?" No clinicians addressed factors that would motivate a patient to quit (e.g., “Tell me some reasons you think quitting smoking is a good idea.”). In 5 of the 26 instances of an Assess (19%), providers modified their assessments, changing the focus from quitting smoking to cutting down or reducing the number of cigarettes smoked. In two visits this modification occurred before the patient had the opportunity to describe her thoughts and feelings about quitting. For example, Provider: “So your plan is to quit or reduce---”Patient: “My plan is reduce to absolutely zero.”
In 35 visits (30%), providers Assisted. Instances of Assist primarily consisted of two different types: medication or referral to a smoking cessation program. Provision of medications to aid in quitting such as nicotine replacement or bupropion occurred in 11/35 visits (31%). The majority of Assists (27/35, 77%) consisted of a referral to a smoking cessation program: "We will give you a referral to our smoking cessation program." No providers Arranged a follow-up visit to discuss smoking.
Table 4 shows the number of A's used in the visits. Providers used only 1 or 2 of the 5 A's in most visits, with Ask being the most frequently used (98%) and in 39% visits, Ask was the only A conducted. Of those visits with 2 A's, providers were more likely to use Ask and Advise than any other combination. In only 24 (21%) of the visits did providers use 3 or more of the 5 A’s; no visits had all 5 A’s.
Table 4.
Number of 5A’s Used
| Number of 5A’s | Number of visits (%) |
|---|---|
| 0 A's | 1 (0.9%) |
| 1 A (all Ask) | 45 (39%) |
| 2 A's | 46 (40%) |
| Ask & Advise | 18 |
| Ask & Assess | 12 |
| Ask & Assist | 15 |
| Assess & Assist | 1 |
| 3 A's | 22 (19%) |
| Ask & Advise & Assess | 5 |
| Ask & Advise & Assist | 11 |
| Ask & Assess & Assist | 6 |
| 4 A's | 2 (2%) |
| 5 A's | 0 (0%) |
In over half of the visits (63/116, 54%), providers gave the patient some information about smoking. This information was either a description of the risks associated with smoking during pregnancy (25/63, 40%), information about smoking cessation aids such as the nicotine patch and bupropion (4/63, 6%), or a general description of smoking cessation resources available (e.g., "We have counselors available to help people stop smoking" (24/63, 38%). In one of the visits, the provider talked about possible barriers that exist for smokers to quit and another 7 (11%) focused on the benefits of reducing the number of cigarettes smoked.
The mean time spent for an entire first obstetric visit was 31 minutes, with visits ranging from 14 to 59 minutes. Table 5 shows the amount of time spent on smoking cessation counseling or use of any of the 5 A's and giving information. The mean amount of total time spent counseling was 47 seconds (range 0–170 seconds). When providers Assisted, the mean amount of time spent Assisting was 32 seconds (range 5–89 seconds). Mean time spent giving information was 34 seconds (range 8 to 131 seconds). In only three visits did the counseling last more than two minutes. In one of these visits--one in which the counseling was 127 seconds--the provider only Asked and spent 87 seconds giving information about the risks of smoking on pregnancies. In another of the visits with longer counseling (151 seconds), the provider Asked and Advised cessation but also spent the majority of time (79 seconds) giving information. In the visit in which the most time was spent on smoking cessation counseling (170 seconds), the provider performed 4 of the 5 A's (Ask, Advise, Assess and Assist) and spent the majority of the counseling on Assist (75 seconds).
Table 5.
Length of Time (in seconds) of 5A’s components
| Ask | Advise (combined if more than one advice) |
Assess | Assist (combined if more than one assist) |
Giving information (combined if more than one) |
Total | ||
|---|---|---|---|---|---|---|---|
| N | Valid | 112 | 35 | 24 | 34 | 64 | 116 |
| Missing | 4 | 81 | 92 | 82 | 52 | 0 | |
| Mean | 11.90 | 16.77 | 13.33 | 31.62 | 34.14 | 47.41 | |
| Std. Deviation | 9.800 | 16.765 | 9.300 | 23.233 | 23.895 | 36.508 | |
| Range | 73 | 92 | 34 | 84 | 123 | 170 | |
| Minimum | 2 | 4 | 3 | 5 | 8 | 0 | |
| Maximum | 75 | 96 | 37 | 89 | 131 | 170 | |
In the logistic regression analyses (with generalized estimating equations), obstetrician-gynecology resident physicians were more likely to Advise patients to quit smoking (p=0.03) and trended toward using 3 or more of the 5 A's (p=0.08) than nurse midwives, nurse practitioners and physician assistants. Patients who reported their race to be African American were more likely to receive smoking cessation advice than those who were white (p=0.02). No other provider or patient factors were significantly associated with the use of any of the 5 A's nor with the number of A's used. No differences were noted when comparing visits obtained from the first study to those obtained in the second study.
Conclusion
There are several important findings from this work. While most obstetric care providers asked their pregnant patients about smoking, none provided best practice smoking cessation counseling using all 5 A's. In this regard, obstetrics care providers are thus not providing the best quality of care to their pregnant patients who smoke. Repeatedly, studies have shown clinician advice and counseling to be effective in helping pregnant women quit. 16, 21–23, 25, 35, 36 Provider smoking cessation counseling using the 5 A's is essential to improving perinatal outcomes among pregnant smokers. Providers in our study relied on information giving rather than discussing patients' motivations, challenges and strategies for smoking cessation.
Our data suggests areas for improvement in smoking cessation counseling. First, few providers discussed patient willingness to quit or provided any resources or referrals. Given there is an on-site smoking cessation program, we expected more providers to Assist. One reason this rate is low could be that providers might have been worried that women were not ready to quit and did not want to hinder rapport. This may explain some of the instances of "giving information" when the providers described the smoking cessation resources but did not actively refer or coordinate the patient's access of these resources. One solution would be to spend more time assessing patient's interest and motivation to quit prior to giving information. This was never done.
Information giving, primarily a discussion of the adverse effects of smoking on pregnancy and infant outcomes, was a common provider behavior. This replicates other studies that found that a larger proportion of providers would give this information than perform the Assess, Assist or Arrange components of the 5 A's; in the study of Ohio obstetricians, 98% discussed the adverse effects.26 Providers seemed to view this information provision as a key component of their tobacco counseling, potentially believing that simple realization of smoking's harms would sufficiently motivate cessation. However, information giving is unlikely to lead to decreased smoking as knowledge alone is a poor predictor of behavior change. Most women know smoking harms the baby, yet they continue to smoke, in part, because they lack confidence and the skills to quit.37 A different way providers could convey this information and simultaneously explore patients' beliefs, attitudes and concerns regarding smoking would be to ask women what they know about the effects of smoking on the baby and their perception of the likelihood their baby would be affected.
Although our patient participants were primarily White, our providers were more likely to Advise African American patients to quit smoking. This is in direct contrast to findings from other studies.38, 39 Further research is needed to explore the possibility of racial differences in smoking cessation counseling and the reasons for any differences in counseling approaches. There may, for example, be geographical differences; our study was conducted among an urban setting in a Mid-Atlantic state while other studies were conducted in more rural areas in a Southern state.38, 39
The maximum amount of time spent addressing smoking was 170 seconds, which is below the recommended 3 minutes.19Studies have shown a dose effect with more time spent counseling associated with higher odds of quitting. Three minutes of smoking cessation counseling was the minimum amount of time needed to show an association with improved quit rates.19Even among the few visits during which providers spent more than two minutes counseling about smoking, most of that counseling was giving information rather than addressing patient motivation to quit. Providers need to spend more time using more effective counseling techniques in addressing smoking with their patients.
This study has several limitations. First, it is possible that additional discussions, information, and resources regarding smoking cessation may have occurred with other clinic staff (e.g., nurses, social workers) or during other prenatal visits. However, our chart reviews and observations of the clinical process suggested that this was unlikely. Additionally, this analyses does not take in consideration the possible co-existence of other medical or social issues or problems to which a provider may have preferentially shifted their time and attention. We will explore this possibility in future analyses.
Although they were blinded to the studies' foci, study participants were aware they were being audio recorded, which may then have altered their behavior and communication during the visit. However, when surveyed at the end of the recorded visit, 95% of our patient participants and 87% of our provider participants indicated that study participation did not change their behavior. Even if not true, this study would represent the best these clinicians do providing smoking cessation counseling and probably overestimates routine behavior.
Although 116 visits represent a relatively large sample of audio-recorded visit data, the relatively small number of obstetric provider participants (48 providers) and the use of a single clinic site limits the generalizability of our findings. The size of our study also limited our ability to look for associations between provider characteristics and communication styles.
Additionally, the majority of our providers were also resident obstetrician-gynecologists. It may be the case that these providers differ from practicing clinicians in that the residents may lack training and experience in smoking cessation counseling. Our residency training program's training on the smoking cessation guidelines tends to be spotty without any focus on the communication skills used in such counseling. However, the resident physicians in our study were the providers more likely to Advise smoking cessation and use a larger number of the A's. Additional studies are needed to explore how practicing obstetric care providers are addressing smoking cessation with their pregnant smokers and whether they are more adherent to the 5 A's counseling approach.
Characteristics of our patient population may also limit generalizability. The smoking rate among our study participants (46%) is very high compared to national averages.3, 4, 6 Indeed, one national study found Pittsburgh ranked as the worst of 50 cities for perinatal smoking.40 Additionally, our patient participants were mostly single with other children. Providers may have de-prioritized smoking cessation in the face of other perceived psycho-social stressors or behavioral risks.
As the data for this analysis came from two studies whose original focus had not been smoking cessation discussion, no contextual information was available to understand better the decisions and behaviors of our obstetric care providers. For example, provider surveys of self-rated use of 5 A’s would have enriched the analyses.
SO WHAT?
What is already known on this topic?
Previous obstetric provider survey studies described relatively high adherence rates to the 5 A's smoking cessation guidelines.26–28 Self-report studies are prone to social desirability and over-estimation; clinicians, in particular, are poor at self-assessment.31
What does this article add?
We found lower use of the 5A’s and noted most smoking discussions focused on giving information. Our data suggest that while obstetric providers believe they are performing best practice smoking cessation counseling, most could do better.
What are the implications for health promotion practice or research?
Our study illustrates that obstetric providers are not adequately addressing tobacco use during pregnancy. Given the known harms of perinatal smoking,1–5there is a imperative need for obstetric care providers to improve their smoking cessation counseling skills. ACOG proposed increasing the number of obstetric care providers trained in evidence-based smoking cessation counseling in the Healthy People 2020 Objectives.41 More work is needed to develop and disseminate effective methods of teaching obstetric providers counseling skills such as the 5 A's.
Acknowledgments
Funding
Funding was provided by the Scaife Family Foundation, an American Professors of Gynecology and Obstetrics/Abbott Medical Education Foundation award, the Building Interdisciplinary Research Careers in Women's Health (BIRCWH) Award (NIH/NICHD 5 K12HD43441-04 PI Roberts; Scholar Chang), and the Agency for Healthcare Research and Quality (1 K08 HS13913-01A1, PI Chang). Dr. Landsittel's effort was covered by Grant Number 5UL1 RR024153-05 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. None of these funding organizations provided any direction, input or influence in the conduct of this study, data analysis, interpretation of results or writing of this manuscript.
Footnotes
Disclosure: No financial disclosures or conflicts of interest were reported by the authors of this paper.
Contributor Information
Judy C. Chang, Department of Obstetrics, Gynecology and Reproductive Sciences and General Internal Medicine, Magee-Womens Research Institute, and Center for Research in Health Care, University of Pittsburgh School of Medicine, 300 Halket St., Pittsburgh, PA 15213, Phone: 412-641-1441, Fax: 412-641-1133, jchang@mail.magee.edu.
Stewart C. Alexander, Department of Medicine and Center for Palliative Care, Duke University School of Medicine; Center for Health Services Research in Primary Care, VA Medical Center, 2424 Erwin Rd. Suite 602, Durham, NC 27705, Phone: 919-668-7220, Fax: 919-668-1300, alexa045@mc.duke.edu.
Cynthia L. Holland, Magee-Womens Hospital, Department of Obstetrics, Gynecology and Reproductive Sciences, 300 Halket St., Pittsburgh PA 15213, Phone: 412-641-4597, Fax: 412-624-6241, hollandcl2@upmc.edu.
Robert M. Arnold, Professor of Medicine, Chief, Section of Palliative Care and Medical Ethics, Assistant Director, Institute to Enhance Palliative Care, Director, Institute for Doctor-Patient Communication, UPMC Montefiore Hospital, Suite 932W, 200 Lothrop St., Pittsburgh PA, 15213, Phone: 412-692-4810, Fax: 412-656-7431, rabob@pitt.edu.
Douglas Landsittel, Center for Research on Health Care Data Center, Institute for Clinical Research Education, University of Pittsburgh, 200 Meyran Ave., Suite 300, Pittsburgh PA, 15213, Phone: 412-864-3019, Fax: 412-586-9672, landsitteldp@upmc.ed.
James A. Tulsky, Department of Medicine and Center for Palliative Care, Duke University School of Medicine; Center for Health Services Research in Primary Care, VA Medical Center; Cancer Prevention, Detection, and Control Research Program, Duke Comprehensive Cancer Center, 2424 Erwin Rd., Hock Plaza, Suite 1105, Durham, NC 27705, Phone: 919-668-7215, Fax: 919-668-1300, jtulsky@duke.edu.
Kathryn I. Pollak, Community and Family Medicine, Duke University Medical Center; Cancer Prevention, Detection, and Control Research Program, Duke Comprehensive Cancer Center, 2424 Erwin Rd. Suite 602, Durham, NC 27705, Phone: 919-681-4757, Fax: 919-681-4785, polla007@mc.duke.edu.
References
- 1.Roelands J, Jamison MLAD, James A. Consequences of smoking during pregnancy on maternal health. Journal of Women's Health. 2009;18(6):867–872. doi: 10.1089/jwh.2008.1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pollack HA. Sudden infant death syndrome, maternal smoking during pregnancy, and the cost-effectiveness of smoking cessation intervention. American Journal of Public Health. 2001;91(3):432–436. doi: 10.2105/ajph.91.3.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.United States Department of Health and Human Services. Women and Smoking: A Report of the Surgeon General. Rockville, MD: United States Department of Health and Human Services; 2001. [Google Scholar]
- 4.DiFranza JR, Aligne CA, Weitzman M. Prenatal and postnatal environmental tobacco smoke exposure and children's health. Pediatrics. 2004;113(4 Suppl):1007–1015. [PubMed] [Google Scholar]
- 5.Dietz P, England L, Shapiro-Mendoza C, Tong V, Farr S, Callaghan W. Infant morbidity and mortality attributable to prenatal smoking in the US. Am J Prev Med. 2010;39(1):45–52. doi: 10.1016/j.amepre.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 6.Tong VT, Jones JR, Dietz PM, D'Angelo D, Bombard JM Centers for Disease Control and Prevention. Trends in smoking before, during, and after pregnancy - Pregnancy Risk Assessment Monitoring System (PRAMS), United States, 31 sites, 2000–2005. Morbidity & Mortality Weekly Report. Surveillance Summaries. 2009;58(4):1–29. [PubMed] [Google Scholar]
- 7.Colman GJ, Joyce T. Trends in smoking before, during, and after pregnancy in ten states. American Journal of Preventive Medicine. 2003;24(1):29–35. doi: 10.1016/s0749-3797(02)00574-3. [DOI] [PubMed] [Google Scholar]
- 8.Kahn RS, Certain L, Whitaker RC. A reexamination of smoking before, during, and after pregnancy. American Journal of Public Health. 2002;92(11):1801–1808. doi: 10.2105/ajph.92.11.1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Substance Abuse and Mental Health Services Administration Office of Applied Studies. Results from the 2004 National Survey on Drug Use and Health: National Findings, Tobacco Use. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2005. [Google Scholar]
- 10.McBride C, Puleo E, Pollak K, Clipp EWS, Emmons K. Understanding the role of cancer worry in creating a "teachable moment" for multiple risk factor reduction. Social Science and Medicine. 2008;66(3):790–800. doi: 10.1016/j.socscimed.2007.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McBride C, Emmons K, Lipkus I. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18:156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 12.McBride C. Tobacco cessation programs for pregnant women and mothers of young children. In: Tremblay R, Barr R, Peters R, editors. Encyclopedia on Early Childhood Development. Montreal, Quebec: Centre of Excellence for Childhood Development; 2003. [Google Scholar]
- 13.Stotts AL, DiClemente CC, Carbonari JP, Mullen PD. Postpartum return to smoking: staging a "suspended" behavior. Health Psychology. 2000;19(4):324–332. doi: 10.1037//0278-6133.19.4.324. [DOI] [PubMed] [Google Scholar]
- 14.Curry SJ, McBride C, Grothaus L, Lando H, Pirie P. Motivation for smoking cessation among pregnant women. Psychology of Addictive Behaviors. 2001;15(2):126–132. doi: 10.1037//0893-164x.15.2.126. [DOI] [PubMed] [Google Scholar]
- 15.O'Campo P, Faden RR, Brown H, Gielen AC. The impact of pregnancy on women's prenatal and postpartum smoking behavior. Am J Prev Med. 1992;8(1):8–13. [PubMed] [Google Scholar]
- 16.Lumley J, Oliver SS, Chamberlain C, Oakley L. Interventions for promoting smoking cessation during pregnancy.[update of Cochrane Database Syst Rev. 2000;(2):CD001055; PMID: 10796228] Cochrane Database of Systematic Reviews. 2004;18(4) doi: 10.1002/14651858.CD001055.pub2. CD001055. [DOI] [PubMed] [Google Scholar]
- 17.American College of Obstetricians and Gynecologists. Smoking Cessation. [Accessed January 28, 2008];American College of Obstetricians and Gynecologists. Available at: http://www.acog.org/departments/dept_web.cfm?recno=13.
- 18.American Academy of Pediatrics, American College of Obstetricians and Gynecologists. Guidelines for Perinatal Care. 6 ed. Washington D.C: American Academy of Pediatrics and the American College of Obstetricians and Gynecologists; 2007. [Google Scholar]
- 19.Agency for Health Care Policy and Research (AHCPR) Treating tobacco use and dependence: 2008 update. AHCPR Supported Clinical Practice Guildelines. 2008 [Google Scholar]
- 20.Mullen PD, Carbonari JP, Tabak ER, Glenday MC. Improving disclosure of smoking by pregnant women. American Journal of Obstetrics & Gynecology. 1991;165(2):409–413. doi: 10.1016/0002-9378(91)90105-z. [DOI] [PubMed] [Google Scholar]
- 21.Melvin C, Gaffney C. Treating nicotine use and dependence of pregnant and parenting smokers: an update. Nicotine & Tobacco Research. 2004;6(Suppl 2):S107–S124. doi: 10.1080/14622200410001669231. [DOI] [PubMed] [Google Scholar]
- 22.Melvin C. Treating tobacco use among pregnant and parenting smokers. In: Tremblay R, Barr R, Peters R, editors. Encyclopedia on Early Childhood Development. Montreal, Quebec: Centre of Excellence for Childhood Development; 2003. [Google Scholar]
- 23.Melvin C, Dolan-Mullen P, Windsor R, Whiteside H, Jr, Goldenberg R. Recommended cessation counselling for pregnant women who smoke: a review of the evidence. Tobacco Control. 2000;9(Suppl-III) doi: 10.1136/tc.9.suppl_3.iii80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fiore MC, Bailey WC, Cohen SJ, et al. Treating Tobacco Use and Dependence. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; 2000. Jun, [Google Scholar]
- 25.Richmond R. Physicians can make a difference with smokers: evidence-based clinical appoaches. Int J Tuberculosis Lung Dis. 1999;3:100–112. [PubMed] [Google Scholar]
- 26.Chapin J, Root W. Improving obstetrician-gynecologist implementation of smoking cessation guidelines for pregnant women: An interim report of the American College of Obstetricians and Gynecologists. Nicotine & Tobacco Research. 2004;6(2):S253–S257. doi: 10.1080/14622200410001669123. [DOI] [PubMed] [Google Scholar]
- 27.Grimely D, Bellis J, Raczynski J, Henning K. Smoking cessation counseling practices: A survey of Alabama obstetrician-gynecologists. Southern Medical Journal. 2001;94(3):297–303. [PubMed] [Google Scholar]
- 28.Hartmann K, Wechter M, Payne P, Salisbury K, Jackson R, Melvin C. Best practice smoking cessation intervention and resource needs of prenatal care providers. Obstet Gynecol. 2007;110(4):765–770. doi: 10.1097/01.AOG.0000280572.18234.96. [DOI] [PubMed] [Google Scholar]
- 29.Bastani R, Glenn B, Maxwell A, Ganz P, Mojica C, Chang C. Validation of self-reported colorectal cancer (CRC) screening in a study of ethnically diverse first-degree relatives of CRC cases. Cancer Epidemiol Biomarkers Prev. 2008;17:791–798. doi: 10.1158/1055-9965.EPI-07-2625. [DOI] [PubMed] [Google Scholar]
- 30.Montano D, Phillips W. Cancer screening by primary care physicians: a comparison of rates obtained from physician self-report, patient survey and chart audit. American Journal of Public Health. 1995;85(6) doi: 10.2105/ajph.85.6.795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L. Accuracy of Physician Self-assessment Compared With Observed Measures of Competence: A Systematic Review. JAMA. 2006;296(9):1094–1102. doi: 10.1001/jama.296.9.1094. [DOI] [PubMed] [Google Scholar]
- 32.Chang JC, Dado D, Frankel RM, et al. When pregnant patients disclose substance use: missed opportunities for behavioral change counseling. Patient Education & Counseling. 2008;72(3):394–401. doi: 10.1016/j.pec.2008.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Landis J, Koch G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 34.Hayes AF. Beyond Baron and Kenny: Statistical Mediation Analysis in the New Millennium. Communication Monographs. 2009;76(4):408–420. [Google Scholar]
- 35.Lumley J, Oliver S, Waters E. Interventions for promoting smoking cessation during pregnancy.[update in Cochrane Database Syst Rev. 2004;(4):CD001055; PMID: 15495004] Cochrane Database of Systematic Reviews. 2000;(2) doi: 10.1002/14651858.CD001055. CD001055. [DOI] [PubMed] [Google Scholar]
- 36.Maciosek MV, Coffield AB, Edwards NM, Flottemesch TJ, Goodman MJ, Solberg LI. Priorities Among Effective Clinical Preventive Services: Results of a Systematic Review and Analysis. American Journal of Preventive Medicine. 2006;31(1):52–61. doi: 10.1016/j.amepre.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 37.Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall, Inc; 1986. [Google Scholar]
- 38.Pollak K, Yarnall K, Rimer B, Lipkus I, Lyna P. Factors associated with patient-recalled smoking cessation advice in a low-income clinic. Journal of the National Medical Association. 2002;94(5):354–363. [PMC free article] [PubMed] [Google Scholar]
- 39.Pollak K, Arredondo E, Yarnall K, et al. How do residents prioritize smoking cessation for young "high-risk" women? Factors associated with addressing smoking cessation. Preventive Medicine. 2001;33(4):292–299. doi: 10.1006/pmed.2001.0884. [DOI] [PubMed] [Google Scholar]
- 40.Annie E Casey Foundation. The Right Start. City Trends: Conditions of Babies and Their Families in America's Largest Cities (1990–1998) Baltimore, MD: Annie E. Casey Foundation; 1999. [Google Scholar]
- 41.Department of Health and Human Services (DHHS) Proposed Healthy People 2010 Objectives. [Accessed August 30, 2010, 2010];Department of Health and Human Services (DHHS) 2009 Oct 30; Available at: http://www.healthypeople.gov/hp2020/Objectives/ViewObjective.aspx?Id=528&TopicArea=Tobacco+Use&Objective=TU+HP2020%e2%80%931&TopicAreaId=47.