Abstract
The present study examined the moderating role of health status (physical, mental, and social health) and the relationships between protective behavioral strategies utilized to reduce high-risk drinking (e.g., avoiding drinking games, setting consumption limits, or having a designated driver) and alcohol use and negative consequences in a sample of heavy drinking college students (N = 1,820). In this high risk sample, multiple regression analyses showed that stronger social health was related to increased drinking, while poorer physical, mental, and social health were related to increased alcohol negative consequences. Further, moderation effects revealed that increasing the use of protective behaviors was associated with significantly less drinking in those with stronger social health, as well as significantly lower numbers of negative consequences among participants with poorer physical and mental health. Implications for college counselors and medical personnel are discussed.
Despite considerable prevention efforts, excessive alcohol consumption and related consequences among college students remains a major area of concern for collegiate administrators and public health officials. Results from multiple national surveys estimate that roughly 70% of college students consume alcohol (Borsari, Murphy, & Barnett, 2007; O’Malley & Johnston, 2002) and between 40–50% of students engage in high risk or heavy episodic “binge” drinking (4+ drinks in one sitting for women and 5+ drinks in one sitting for men; O’Malley & Johnston, 2002; Wechsler & Nelson, 2008). The latest nationally representative data of college student drinking showed stabilized rates of overall heavy episodic drinking, but increases in frequent heavy episodic drinking (3 or more times in the past 2 weeks; Harvard School of Public Health College Alcohol Study [CAS]) (Wechsler, Lee, Kuo, Seibring, Nelson, & Lee, 2002; Wechsler & Nelson, 2008). Excessive drinking leads to several serious negative consequences, including academic and psychological impairment, risky sexual behavior, car accidents, violence, addiction, and even death. In CAS surveys, frequent heavy episodic drinkers were 21 times more likely than non-frequent heavy episodic drinkers to suffer more than four of 12 stated alcohol-related problems (Hingson, Heeren, Zakocs, Kopstein, & Wechsler, 2002). Moreover, proximate peers and surrounding communities often suffer secondary consequences through vandalism, noise disturbance, and verbal, physical, or sexual assault (Hingson et al., 2002; Wechsler, Moeyskens, Davenport, Castillo, & Hansen, 1995; Wechsler et al., 2002; Yu, 2001).
The relationship between alcohol and adverse health seems to exhibit a J-shaped curve, such that compared to abstainers, light to moderate drinking may actually confer beneficial physical, mental, and social effects while heavy drinking may pose detrimental health risks (Agarwal, 2002; Doll, Peto, Hall, Wheatley, & Gray, 1994). The negative effects associated with heavy drinking appear to be most pronounced for younger cohorts (i.e., adolescents and young adults) (Gronbaek, 2009). Given that college students represent the age group at greatest risk for alcohol-related problems and that heavy episodic drinking is most detrimental to health among this population (Murray, Connett, Tyas, Bond, Ekuma, Silversides, et al., 2002; Poikolainen, Paljarvi, & Makela, 2007), finding ways to intervene and reduce risk and harm is essential.
Student affairs personnel have attempted to intervene to reduce high rates of hazardous alcohol consumption on college campuses through a host of initiatives, ranging from zero-tolerance disciplinary sanctions to alcohol awareness education. One promising approach to health promotion may include the teaching of protective behavioral strategies (PBS), which have demonstrated efficacy in reducing overall consumption and related consequences among college students who employ them naturally (Araas & Adams, 2008; Haines, Barker, & Rice, 2006; Martens et al., 2005). These cognitive-behavioral strategies (e.g., avoiding drinking games, setting consumption limits, having a designated driver) are practiced during the active consumption of alcohol and appear well-suited to collegiate settings. As illustrated in a study of approximately 28,000 college students, three-quarters of respondents utilized at least one of 10 protective behaviors (Haines et al., 2006), thus indicating that PBS may impart an intuitive and easy to use approach by which college student drinkers may minimize alcohol-related harm. However, despite the overall success that protective behaviors have shown in promoting safer alcohol consumption, little is known of potential intervening variables or the subsets of students for whom these strategies may work best. By investigating the extent to which physical, mental, and social health status moderate the relationship between protective behaviors and risky alcohol consumption, the present study seeks to foster targeted and more efficient PBS-based interventions.
MENTAL HEALTH
Individuals with poorer mental health often consume alcohol to self-medicate or suppress negative affect, such as tension or depressed mood (Martin, Lynch, Pollock, & Clark, 2000; Ozegovic, Bikos, & Szymanski, 2001; Seeman & Seeman, 1992). Such coping-motivated drinkers fail to effectively resolve problems, and are especially vulnerable to harmful alcohol-related outcomes, including alcohol dependence (Carpenter & Hasin, 1999; Kuntsche, Knibbe, Gmel, & Engels, 2005). Interestingly, within collegiate populations, poor mental health, depressive symptoms, and psychological distress have consistently been linked to alcohol-related problems, but not alcohol intake itself (Nagoshi, 1999; Park & Grant, 2005; Weitzman, 2004). Martens and colleagues (2008) shed light on this inconsistency by finding that protective strategies mediated the relationship between depressive symptomatology and alcohol-related negative consequences in a sample of college students mandated to an alcohol intervention for violating campus alcohol policy. The authors postulated that students with depressive symptoms may lack the psychoemotional cognition and social networks needed to utilize PBS effectively. In support of this finding, higher levels of conscientiousness (e.g., possessing impulse control, goal-directedness, anticipating consequences), typically associated with higher mental health (Roberts, Walton, & Bogg, 2005), have been linked to greater PBS use and, in turn, less risky drinking (Martens, Karakashian, Fleming, Fowler, Hatchett, & Cimini, et al., 2009). Nevertheless, despite their lower likelihood to employ PBS, at-risk students of low mental health may actually have the most to gain from them. In a sample of 128 first-year college women, LaBrie and colleagues (2009) found that although mental health did not predict drinking or associated problems directly, it moderated the relationship between PBS and risky drinking such that protective behaviors were significantly associated with reduced alcohol consumption and related risks among participants reporting lower mental health. However, the findings of this smaller single-sex study cannot be generalized to wider college student populations. The current study, based on a large sample of male and female college students, is expected to demonstrate that among students with poorer mental health, those reporting increased implementation of PBS will report reduced alcohol risk.
Physical Health
Although extensive research has provided support for strong comorbidity between alcohol abuse and adverse physical health outcomes, such as cardiovascular, respiratory, and sleep disorders (Glenn, Parsons, & Stevens, 1989; Gossop, Neto, Radovanovic, Batra, Toteva, Musalek, et al., 2007), the few findings pertaining to college students have been conflicting. For example, symptoms of both poorer physical health (i.e., physical discomfort, fatigue, and lethargy) and stronger physical health (i.e., physical activity) have been associated with problematic drinking among college students (Carey, 1993; Vickers, Patten, Bronars, Lane, Stevens, Croghan, et al., 2004; Wright, 1983). In a representative longitudinal study of over 20,000 college undergraduates, increased drinking predicted decreased wellness behaviors, including exercise, nutrition, and illness prevention (Jensen, Peterson, Murphy, & Emmerling, 1992). Although no studies to date have correlated physical health with PBS utilization, those students with poorer physical health who may lack the volition to manage drinking responsibly are expected to reap distinct benefit from implementing explicit protective behaviors.
Social Health
Social health is particularly relevant to research of college student drinking behavior. Increased consumption rates during the college years have been attributed to environments comprised of same-aged young adults experiencing increased independence amid collegiate cultures that tend to revere social drinking. In these contexts, the more agreeable, extraverted, and open an individual, the more likely he or she has been found to adopt peers’ drinking behavior (Peterson, Morey, & Higgins, 2005) or drink excessively (Martsh & Miller, 1997). In contrast, social anxiety has been associated with decreased alcohol consumption (Rohsenow, 1982). Interestingly, first-year female students with higher social health have exhibited greater likelihood to utilize and benefit from PBS than peers with lower social health (LaBrie et al., 2009). Additional studies indicate that problems arising from elevated consumption may be attenuated for those students with high relational health as they may derive protective benefits from strong support networks and community integration (LaBrie, Thompson, Ferraiolo, Garcia, Huchting, & Shelesky, 2008; Vaux, 1988). In accordance with extant literature, in the current study, social health is expected to moderate the relationship between PBS and alcohol risk, such that students with stronger social health—who incidentally are expected to drink significantly more than those with poorer social health—are expected to benefit most from PBS, such that it will be associated with a greater reduction in drinking and associated consequences.
While it has previously been shown in a small sample of first-year college women that both mental and social health moderated the relationship between PBS and risky drinking (LaBrie et al., 2009), in the current study we seek to extend previous work by focusing on a large dual-site sample of male and female college students most at risk for heightened alcohol problems (i.e., heavy episodic drinkers) to determine how health status may influence the efficacy of PBS in mitigating risky drinking. Students engaging in heavy episodic drinking account for the strong majority of alcohol consequences on college campuses and hence represent the student population in greatest need of protective strategies to minimize alcohol risk. Consistent with prior research, use of protective behaviors is expected to be associated with lower alcohol use and decreased alcohol-related negative consequences. More specifically, those respondents reporting health status associated with higher alcohol risk (i.e., poorer mental health, poorer physical health, or stronger social health) should benefit most from the use of PBS, particularly with respect to reductions in negative consequences. Findings aim to inform student affairs and mental health professionals concerned with reducing risky drinking on college campuses, and propose ways in which such interventions may be tailored to target and protect subsets of at-risk students who may most benefit from PBS education.
METHOD
Sample
Participants were a subsample of a larger intervention study of students from two West Coast universities, a large public institution with approximately 30,000 undergraduates and a mid-sized private institution with approximately 5,500 undergraduates. The sample used in the current study (N = 1,820; 56.5% female) had a mean age of 19.92 (SD = 1.33). Racial composition was 76.0% Caucasian and 24.0% Asian, and class standing was as follows: 16.9% first-years, 24.6% sophomores, 26.9% juniors, and 31.5% seniors.
Design and Procedure
During the fall semester of 2008, a randomly selected group of 11,069 students across both campuses were invited via e-mail to participate in a confidential study regarding alcohol use and perceptions of drinking in college. The 4,984 (45.0% response rate) students who consented to participate in the study clicked on a designated link to access an online screening survey. Responses in the screening survey established eligibility for participation in a subsequent baseline survey and larger web-based social norms intervention study, which specifically aimed to examine race-based personalized normative feedback by restricting the sample to heavy drinking Caucasian and Asian students only. Asian-American students are of particular interest due to escalating rates of alcohol abuse and heavy episodic drinking in this population (see Grant, Dawson, Stinson, Chou, Dufour, & Pickering, 2004; Wechsler, Dowdall, Maenner, Gledhill-Hoyt, & Lee, 1998). As such, to screen into the baseline survey, participants had to be either Caucasian or Asian and have had at least one episode of heavy episodic drinking in the past month. All respondents signed a local IRB-approved consent form at the beginning of both the screening and baseline surveys and were paid a nominal stipend upon completion of each survey. Those 1,820 students who met the screening criteria and completed the baseline survey make up the current sample.
Measures
Measures appropriate to the current study include alcohol use, alcohol-related negative consequences, PBS, and health status.
Alcohol Consumption
Collegiate drinking was assessed using the Daily Drinking Questionnaire (DDQ; Collins, Parks, & Marlatt, 1985; Dimeff, Baer, Kivlahan, & Marlatt, 1999). Participants were instructed to consider a typical week in the past month before answering, “How many drinks did you typically consume on a Monday? Tuesday?” and so on. Students’ open-ended responses across these 7 days were summed to form a “total drinks per week” variable that was used in these analyses.
Negative Consequences
The 25-item Rutgers Alcohol Problem Index (RAPI; White & Labouvie, 1989) (α = .90) assessed alcohol-related consequences. Using a 0 (never) to 4 (more than 10 times) scale, participants indicated how many times in the past month the following things had happened to them because they were drinking or because of their alcohol use. The items included “Caused shame or embarrassment to someone,” “Passed out or fainted suddenly,” or “Felt that you had a problem with alcohol.” Items were summed to form the RAPI scale score used in the analyses.
Protective Behavioral Strategies
Participants completed Protective Behavioral Strategy Surveys (PBSS; Martens et al., 2005) (α = .82) to assess cognitive-behavioral strategies used to reduce risky drinking. The PBSS is the most rigorously tested and psychometrically validated measurement of alcohol-related protective behaviors (Benton, Schmidt, Newton, Shin, Benton, & Newton, 2004; Martens et al., 2005; Martens, Ferrier, & Cimini, 2007; Martens, Pedersen, LaBrie, Ferrier, & Cimini, 2007; Walters, Roudsari, Vader, & Harris, 2007). Using a scale ranging from 1 (never) to 5 (always), participants indicated the degree to which they engaged in the following behaviors when using alcohol or “partying.” The 15-item measure is comprised of statements including, “leave bar/party at a predetermined time,” “put extra ice in your drink,” “drink slowly, rather than gulp or chug,” “avoid drinking games,” and “use a designated driver.” The composite was constructed by averaging scores on these items.
Duke Health Profile
The Duke Health Profile (DUKE; Parkerson, Broadhead, & Tse, 1990), a self-report measure that has demonstrated good construct validity (Guillemin, Paul-Dauphin, Virion, Bouchet, & Briancon, 1997), was used to evaluate participants’ mental, social, and physical health. Mental health items included statements such as, “I like who I am” and “feeling depressed or sad”; social health items included “I am comfortable being around people” and “I am happy with my family relationships”; and physical health assessed the difficulty with which respondents performed conventional tasks like “walking up a flight of stairs” or “sleeping.” Each of these three health subscales was comprised of five items, to which participants indicated whether the statements described them 0 (not at all), 1 (somewhat), or 2 (exactly) or if they had experienced 0 (none), 1 (some), or 2 (a lot) of the given symptoms either “today” or “in the past week.” After reverse scoring necessary items, the raw score for each domain was computed and multiplied by 10. Accordingly, this resulted in physical, mental, and social health subscale scores ranging from 0 to 100, with higher scores representing better health.
RESULTS
Analytic Plan
Means scores for drinks per week, alcohol-related negative consequences, PBS, physical health, mental health, and social health were reported and their correlations were examined. Through two-step hierarchical multiple regressions models, we then assessed whether health status (physical, mental, and social) statistically moderated the effectiveness of alcohol protective strategies on the outcomes of drinks per week and alcohol-related negative consequences. The model predicting drinks per week was estimated as follows. The main effects of protective strategies, physical, mental, and social health were entered in Step 1. Step 2 included the interaction terms involving PBS with each physical, mental, and social health variable. The model predicting alcohol negative consequences was estimated in the same manner, in addition to controlling for drinks per week at Step 1. In both models, predictors were standardized prior to calculation of interaction terms to avoid statistical artifacts associated with multicollinearity, and statistically significant interactions were graphed at one standard deviation below (poor health) and above (strong health) the mean, according to established guidelines (Aiken & West, 1991).
Descriptives and Correlations
Mean scores were examined for drinks per week (M = 11.01, SD = 9.42), alcohol-related negative consequences (M = 4.24, SD = 5.65), and protective strategies (M = 4.27, SD = 0.96). Consistent with a sample of young adults attending college, the health status subscales of physical health (M = 75.60, SD = 17.84), mental health (M= 74.75, SD = 17.84), and social health (M= 80.71, SD = 17.68) appeared to be relatively strong. The correlation matrix is presented in Table 1. Among the notable findings, drinks per week correlated positively with alcohol negative consequences, but negatively with the implementation of PBS. Alcohol negative consequences correlated negatively with PBS and with physical, mental, and social health. Also as would be expected, all three health subscales (physical, mental, and social) were positively intercorrelated.
Table 1.
Correlation Matrix of Variables in Study
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Drinks per week | — | |||||
| 2. Alcohol negative consequences | .37*** | — | ||||
| 3. Protective Behavioral Strategies (PBS) | −.34*** | −.25*** | — | |||
| 4. Physical health | .05* | −.18*** | .00 | — | ||
| 5. Mental health | .01 | −.21*** | .09*** | .47*** | — | |
| 6. Social health | .11*** | −.10*** | .08*** | .22*** | .44*** | — |
p < .05.
p < .01.
p < .001.
Predicting Drinks Per Week
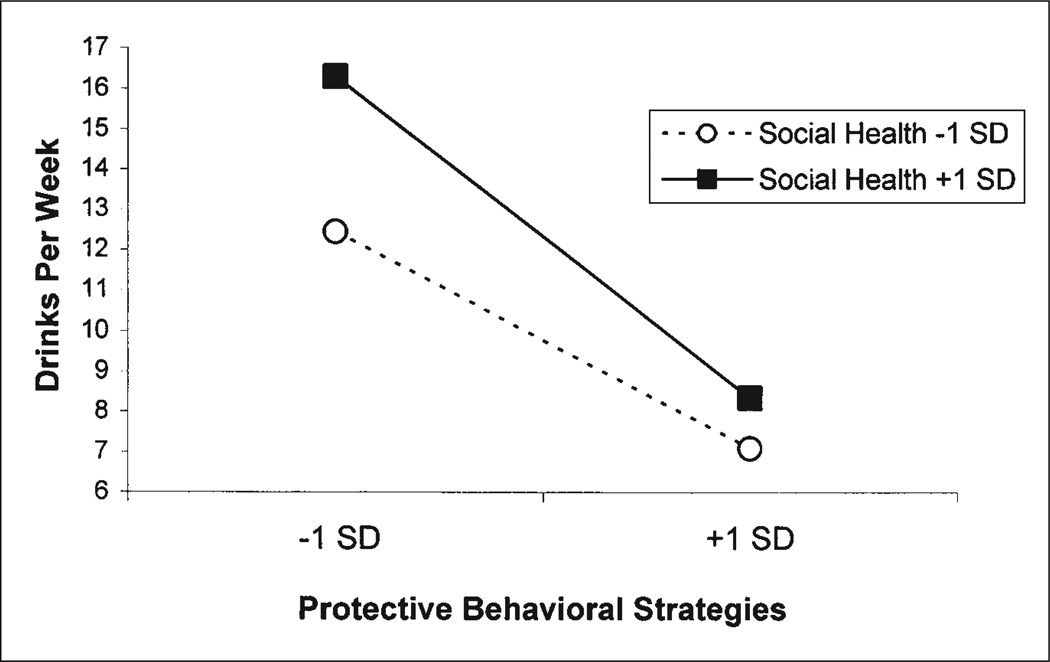
The regression model showed that the following predictors uniquely contributed to drinks per week (Table 2, top): lower protective strategies (β = −.35, p < .001), stronger social health (β = .15, p < .001), and PBS × social health (β = −.06, p < .05). As depicted in Figure 1, the significant moderation effect reveals that among students possessing stronger social health, increasing (from low to high) the use of PBS predicted a stronger corresponding decrease in drinks per week than those reporting poorer social health. Though simple slopes were found to be significant for both poorer (β = −.29, p < .001) and stronger (β = −.42, p < .001) social health, a steeper declining slope was evidenced among those with stronger social health.
Table 2.
Regression Models Predicting Drinks per Week and Negative Consequences
| ΔR2 | B | Final β | ||
|---|---|---|---|---|
| Drinks per week | ||||
| Step 1: | Main Effects | .13*** | ||
| PBS | −3.32 | −.35*** | ||
| Physical health | 0.30 | .03 | ||
| Mental health | −0.38 | −.04 | ||
| Social health | 1.37 | .15*** | ||
| Step 2: | Interactions | .01** | ||
| PBS × Physical health | −0.37 | −.04 | ||
| PBS × Mental health | −0.05 | −.01 | ||
| PBS × Social health | −0.54 | −.06* | ||
| Multipe R = .38 | ||||
| F(7, 1812) = 43.07*** | ||||
| Negative consequences | ||||
| Step 1: | Main Effects | .21*** | ||
| Drinks per week | 2.012 | .36*** | ||
| PBS | −0.61 | −.11*** | ||
| Physical health | −0.69 | −.12*** | ||
| Mental health | −0.67 | −.12*** | ||
| Social health | −0.26 | −.05* | ||
| Step 2: | Interactions | .02*** | ||
| PBS × Physical health | 0.63 | .12*** | ||
| PBS × Mental health | 0.27 | .05* | ||
| PBS × Social health | −0.17 | −.03 | ||
| Multipe R = .48 | ||||
| F(8, 1811) = 68.68*** | ||||
Note: PBS = Protective Behavioral Strategies
p < .05.
p < .01.
p < .001.
Figure 1.
Social health as moderator of the relationship between protective strategies and drinks per week.
Predicting Alcohol-Related Negative Consequences
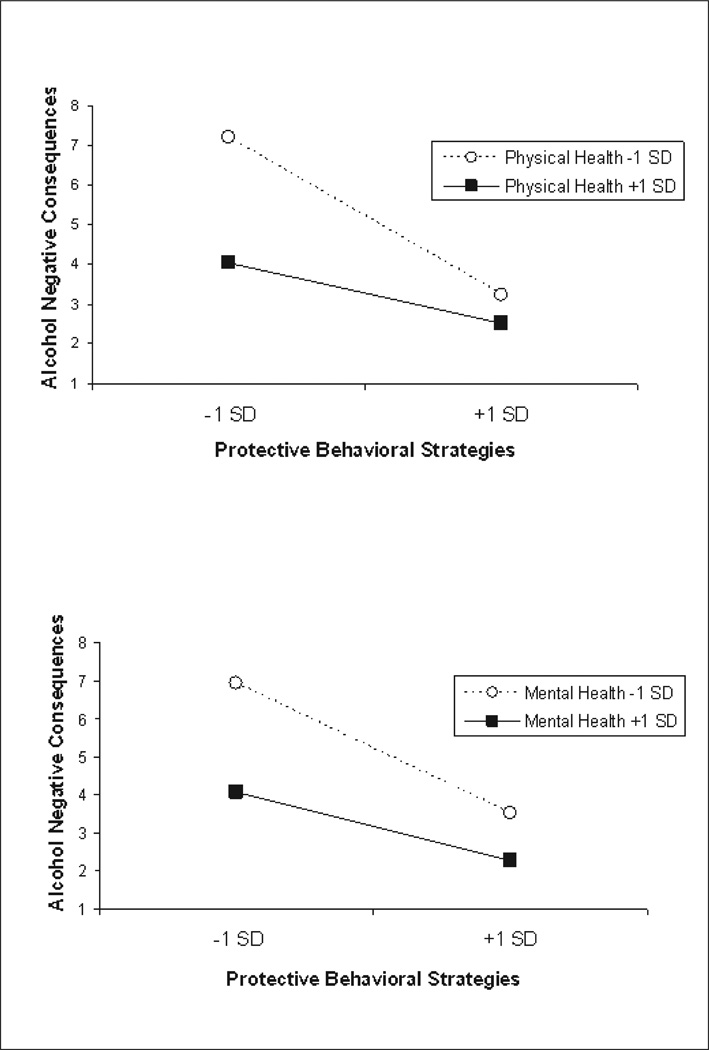
The following predictors uniquely contributed to the prediction of alcohol negative consequences (see Table 2, bottom): higher drinks per week (β = .36, p < .001), lower PBS (β = −.11, p < .001), poorer physical health (β = −.12, p < .001), poorer mental health (β = −.12, p < .001), poorer social health (β = −.05, p < .05), PBS × physical health (β = .12, p < .001), and PBS × mental health (β = .05, p < .05). Both significant moderation effects are illustrated in Figure 2. Shifting the use of PBS from low to high tended to be more successful in curtailing negative consequences among students with poorer, rather than stronger, physical health. Simple slope analyses were found to be significant for both poorer (β = −.35, p < .001) and stronger (β = −.14, p < .001) physical health, with a steeper slope for participants possessing poorer physical health. Similarly, students with poorer mental health with increased implementation of PBS experienced a greater reduction in negative consequences than those classified as stronger in mental health. Simple slope analyses were determined to be significant for both poorer (β = −.30, p < .001) and stronger (β = −.16, p < .001) mental health, with a steeper slope for participants possessing poorer mental health.
Figure 2.
Physical and mental health as moderators of the relationship between protective strategies and alcohol negative consequences.
DISCUSSION
The present investigation advances research that has found the implementation of PBS to be an effective and promising approach by which college students may reduce drinking and alcohol-related consequences. This was accomplished using a large sample of heavy drinking college students of varying levels of health to demonstrate that students’ inherent use of PBS appeared to attenuate alcohol risk (i.e., drinking and consequences). Particularly enlightening for collegiate harm reduction efforts are findings showing that, despite weak associations with alcohol consumption, poorer mental and physical health strongly correlated with negative consequences. Further, regression analyses showed that even though students who employed PBS drank less and experienced fewer negative consequences overall, increasing the use of PBS was linked to a stronger reduction in consequences among those students with poorer mental and physical health. Also, while students with stronger social health tended to consume greater amounts of alcohol, they too appeared to benefit from increasing PBS with respect to consumption, consuming fewer drinks than students with stronger social health who used PBS less often. By illustrating the efficacy of employing PBS within a high risk population of heavy episodic drinkers, and particularly among students reporting health statuses most susceptible to alcohol risk, the present study offers important insight for collegiate health and wellness personnel.
Among this sample of high risk collegiate student drinkers, physical, mental, and social health were independently associated with alcohol consequences, even after controlling for amount of alcohol consumed. This is the first study to document the link between college students’ physical health and alcohol consequences, over and above alcohol intake, thus drawing attention to poorer physical health as a potential risk factor in this population. Perhaps students with poorer mental health or poorer physical health lack the internal emotional regulation, volitional control, or social resources known to protect students against negative consequences associated with drinking. Although the current results assess the efficacy of naturally occurring protective strategies, implications point to the potential for initiatives aimed at teaching PBS, which are both easily taught and learned, to promote important reductions in drinking and consequences among at-risk students.
Student psychological and medical health centers may be ideal settings in which to intervene with those students of poorer mental or physical health most likely to benefit from PBS. Equipping counselors, practitioners, and affiliated personnel with the tools needed to teach and encourage students to use self-protective strategies may be valuable as students often engage the services of these centers due to mental or physical problems. Moreover, given the well-established comorbidity of mental and physical disorders, assessing the bodily health of students seeking psychological help and the emotional stability of students visiting medical health centers may help identify at-risk students. Further, it may be advantageous for campus psychological and medical centers to collaborate in screening for alcohol abuse and consequences. Ironically, although the majority of college health centers do not currently incorporate alcohol use assessment (Foote, Wilkens, & Vavagiakis, 2004), evidence shows above average rates of alcohol misuse among students visiting such centers; for example, in a sample of over 15,000 students seeking mental health treatment, 42% had engaged in heavy episodic drinking in just the past 2 weeks (Locke, Hayes, Crane, Schendel, Castonguay, Boswell, et al., 2009). This suggests that campus health centers may already be seeing high risk drinkers and should consider screening and intervening with their student clients. Developing both passive (through the use of flyers and posters) and interpersonal interventions that describe and teach PBS may be an effective way to reduce alcohol harm among these vulnerable students.
Considering both the increasing prevalence of emotional and physical problems observed in college populations (e.g., low self-esteem, anxiety disorders, depression, stress, sleeplessness) (Kitzrow, 2003; Lund, Reider, Whiting, & Prichard, 2009) and results illustrating the protective benefit of mental and physical well-being against drinking-related problems, wellness programming that seeks to alleviate stress and promote healthy behaviors may be beneficial to this population. For example, college orientations that address the protective benefits of cardiovascular health and proper sleep habits to overall well-being and collegiate success or train at-risk students (e.g., incoming first-years or judicially sanctioned) to better manage academic and social pressures may promote health and reduce risky drinking and adverse outcomes. In particular, non-punitive and non-coercive group motivational enhancement interventions conducted in the spirit of Motivational Interviewing (MI; Miller & Rollnick, 2002), which have demonstrated success in increasing college students’ motivation to alter their own behaviors, may present ideal settings for teaching and stressing the value of using protective strategies (Task Force of the National Advisory Council on Alcohol Abuse and Alcoholism, 2002).
This study also confirms previous research by finding that stronger social health appears to both promote increased drinking and protect students from alcohol-related consequences (LaBrie et al., 2008; Vaux, 1988). PBS utilization was found to be significantly associated with reduced drinking among participants, particularly those reporting stronger social health. These results differ slightly from prior findings in which PBS was linked to reduced drinking among first-year college women of stronger, but not poorer social health (LaBrie et al., 2009); in the current study, students with poorer social health who increased their use of PBS from low to high experienced reduced levels of drinking (though associations were not as dramatic as those with stronger social health). This suggests that, among high risk college drinkers, students reporting both stronger and poorer social health can benefit by employing PBS. Nevertheless, the paradoxical impact of social health status (promoting increased drinking while being associated with reduced consequences) suggests that college administration and student personnel recognize both sides of the equation. On one hand, student affairs personnel should assist in developing positive social health among students, perhaps by building socially integrated campus environments and providing those students lacking a sense of communal cohesiveness with opportunities to enhance social ties within the community. On the other hand, wellness programming may attempt to de-link social health and connectedness from heavy drinking. For example, campus interventions incorporating PBS education and targeted toward students judicially sanctioned for alcohol misuse or social groups typified by heavy drinking (e.g., fraternities/sororities and school/ intramural athletic teams) may help curtail heavier drinking while preserving the protective benefits associated with higher social health.
Results are tempered by several limitations. First, the sample includes only Caucasian and Asian college students. Forthcoming studies utilizing ethnically diverse representative samples will strengthen findings and offer insight into the usefulness of protective behaviors across race. Second, data rely on self-report measures, which may carry response bias. However, we made great efforts to ensure respondents that surveys were anonymous and confidential, thereby conforming to methods deemed valid and reliable in evaluating alcohol use and behavior (Maisto, Connors, & Allen, 1995). Third, data are cross-sectional. Research incorporating longitudinal designs may be used to better scrutinize the role of health to alcohol risk and the efficacy of protective strategies in attenuating that risk by assessing alcohol use prior or subsequent to PBS implementation. Specifically, PBS-based interventions that account for pre- and post-intervention assessment are warranted.
Nonetheless, the current study highlights the need for alcohol interventions with college students who have compromised mental or physical health, as these health statuses were related to increased negative consequences even when controlling for the amount of alcohol consumed. Future research should assess the efficacy of learned as compared to inherent protective behavioral usage in order to validate if PBS learned through training or pamphlets can reduce alcohol risk as effectively as naturally employed PBS. While the mental health-alcohol risk connection is widely acknowledged, the current findings draw attention to the understudied role that poorer physical health appears to play in the incidence of alcohol problems among high risk college students. Because students with poorer mental and physical health are most likely to utilize campus health services, health and counseling centers provide ideal loci for alcohol-related interventions. The key finding that utilizing PBS was associated with reduced consequences among students with poorer mental and physical health suggests that passive and direct interventions describing and teaching protective cognitive-behavioral strategies at these centers may be helpful in mitigating alcohol risk. However, because not all students with compromised health status seek campus health services, health professionals as well as other student affairs personnel are encouraged to develop outreach programming that teach and promote protective strategies. Moreover, the findings indicate that the adoption of PBS is beneficial in reducing consumption levels among students with stronger social health, who are inclined to drink heavily. Interventions that include PBS as a component may also be helpful with the broader student body, particularly those more socially connected (e.g., students in fraternities/sororities and student athletes). Thus, it appears that college counselors, medical professionals, and student affairs personnel should become familiar with PBS and encourage the adoption of these behaviors/strategies in order to reduce alcohol risk.
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism Grant R01AA12547 and the United States Department of Education Grant Q184H070017.
REFERENCES
- Agarwal DP. Cardioprotective effects of light-moderate consumption of alcohol: A review of putative mechanisms. Alcohol and Alcoholism. 2002;37(5):409–415. doi: 10.1093/alcalc/37.5.409. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- Araas TE, Adams TB. Protective behavioral strategies and negative alcohol-related consequences in college students. Journal of Drug Education. 2008;38(3):211–224. doi: 10.2190/DE.38.3.b. [DOI] [PubMed] [Google Scholar]
- Benton SL, Schmidt JL, Newton FB, Shin K, Benton SA, Newton DW. College student protective strategies and drinking consequences. Journal of Studies on Alcohol. 2004;65(1):115–121. doi: 10.15288/jsa.2004.65.115. [DOI] [PubMed] [Google Scholar]
- Borsari B, Murphy JG, Barnett NP. Predictors of alcohol use during the first year of college: Implications for prevention. Addictive Behaviors. 2007;32(10):2062–2086. doi: 10.1016/j.addbeh.2007.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB. Situational determinants of heavy drinking among college students. Journal of Counseling Psychology. 1993;40(2):217–220. [Google Scholar]
- Carpenter KM, Hasin DS. Drinking to cope with negative affect and DSM-IV alcohol use disorders: A test of three alternative explanations. Journal of Studies on Alcohol. 1999;60(5):694–704. doi: 10.15288/jsa.1999.60.694. [DOI] [PubMed] [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53(2):189–200. doi: 10.1037//0022-006x.53.2.189. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief Alcohol Screening and Intervention for College Students (BASICS): A harm reduction approach. New York: Guilford Press; 1999. [Google Scholar]
- Doll R, Peto R, Hall E, Wheatley K, Gray R. Mortality in relation of consumption of alcohol, 13 years’ observation on male British doctors. British Medical Journal. 1994;309(6959):911–917. doi: 10.1136/bmj.309.6959.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foote J, Wilkens C, Vavagiakis P. A national survey of alcohol screening and referral in college health centers. Journal of American College Health. 2004;52(4):149–157. [PubMed] [Google Scholar]
- Glenn SW, Parsons OA, Stevens L. Effects of alcohol abuse and familial alcoholism on physical health in men and women. Health Psychology. 1989;8(3):325–341. doi: 10.1037//0278-6133.8.3.325. [DOI] [PubMed] [Google Scholar]
- Gossop M, Neto D, Radovanovic M, Batra A, Toteva S, Musalek M, et al. Physical health problems among patients seeking treatment for alcohol use disorders: A study in six European cities. Addiction Biology. 2007;12(2):190–196. doi: 10.1111/j.1369-1600.2007.00066.x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug & Alcohol Dependence. 2004;74(3):223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Gronbaek M. The positive and negative health effects of alcohol and the public health implications. Journal of Internal Medicine. 2009;265:407–420. doi: 10.1111/j.1365-2796.2009.02082.x. [DOI] [PubMed] [Google Scholar]
- Guillemin F, Paul-Dauphin A, Virion JM, Bouchet C, Briancon S. Le profil de santé de DUKE: Un instrument de mesure generique de qualite de vie liee a la santé [The DUKE health profile: A generic instrument to measure the quality of life tied to health] Santa Publique. 1997;9(1):35–44. [PubMed] [Google Scholar]
- Haines MP, Barker G, Rice RM. The personal protective behaviors of college student drinkers: Evidence of indigenous protective norms. Journal of American College Health. 2006;55(2):69–76. doi: 10.3200/JACH.55.2.69-76. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Zakocs RC, Kopstein A, Wechsler H. Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18–24. Journal of Studies on Alcohol. 2002;63(2):136–144. doi: 10.15288/jsa.2002.63.136. [DOI] [PubMed] [Google Scholar]
- Jensen MA, Peterson TL, Murphy RJ, Emmerling DA. Relationship of health behaviors to alcohol and cigarette use by college students. Journal of College Student Development. 1992;33(2):163–170. [Google Scholar]
- Kitzrow MA. The mental health needs of today’s college students: Challenges and recommendations. NASPA Journal. 2003;41(1):167–181. [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clinical Psychology Review. 2005;25(7):841–861. doi: 10.1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Kenney SR, Lac A, Garcia JA, Ferraiolo P. Mental and social health impacts the use of protective behavioral strategies in reducing risky drinking and alcohol consequences. Journal of College Student Development. 2009;50(1):35–49. doi: 10.1353/csd.0.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Thompson AD, Ferraiolo P, Garcia JA, Huchting K, Shelesky K. The differential impact of relational health on alcohol consumption and consequences in first year college women. Addictive Behaviors. 2008;33(2):266–278. doi: 10.1016/j.addbeh.2007.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locke B, Hayes J, Crane A, Schendel C, Castonguay L, Boswell J, et al. Center for the Study of Collegiate Mental Health (CSCMH): 2009 pilot study. PA: CSCMH research team at the Pennsylvania State University, University Park; 2009. Unpublished manuscript. [Google Scholar]
- Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. Journal of Adolescent Health. 2009;46(2):124–132. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Connors GJ, Allen JP. Contrasting self-report screens for alcohol problems: A review. Alcoholism: Clinical and Experimental Research. 1995;19(6):1510–1516. doi: 10.1111/j.1530-0277.1995.tb01015.x. [DOI] [PubMed] [Google Scholar]
- Martens MP, Ferrier AG, Cimini MD. Do protective behavioral strategies mediate the relationship between drinking motives and alcohol use in college students? Journal of Studies on Alcohol & Drugs. 2007;68(1):106–114. doi: 10.15288/jsad.2007.68.106. [DOI] [PubMed] [Google Scholar]
- Martens MP, Ferrier AG, Sheehy MJ, Korbett K, Anderson DA, Simmons A. Development of the Protective Behavioral Strategies Survey. Journal of Studies on Alcohol. 2005;66(5):698–705. doi: 10.15288/jsa.2005.66.698. [DOI] [PubMed] [Google Scholar]
- Martens MP, Karakashian MA, Fleming KM, Fowler RM, Hatchett ES, Cimini DM. Conscientiousness, protective behavioral strategies, and alcohol use: Testing for mediating effects. Journal of Drug Education. 2009;39(3):273–287. doi: 10.2190/DE.39.3.d. [DOI] [PubMed] [Google Scholar]
- Martens MP, Martin JL, Hatchett ES, Fowler RM, Fleming KM, Karakashian MA, et al. Protective behavioral strategies and the relationship between depressive symptoms and alcohol-related negative consequences among college students. Journal of Counseling Psychology. 2008;55(4):535–541. doi: 10.1037/a0013588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Pedersen ER, LaBrie JW, Ferrier AG, Cimini MD, Ferrier AG. Measuring alcohol-related protective behavioral strategies among college students: Further examination of the Protective Behavioral Strategies Scale. Psychology of Addictive Behaviors. 2007;21:307–315. doi: 10.1037/0893-164X.21.3.307. [DOI] [PubMed] [Google Scholar]
- Martin CS, Lynch KG, Pollock NK, Clark DB. Gender differences and similarities in the personality correlates of adolescent alcohol problems. Psychology of Addictive Behaviors. 2000;14(2):121–133. doi: 10.1037//0893-164x.14.2.121. [DOI] [PubMed] [Google Scholar]
- Martsh CT, Miller WR. Extraversion predicts heavy drinking in college students. Personality and Individual Differences. 1997;23(1):153–155. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York: Guilford Press; 2002. [Google Scholar]
- Murray RP, Connett JE, Tyas SL, Bond R, Ekuma O, Silversides CK, et al. Alcohol volume, drinking pattern, and cardiovascular disease morbidity and mortality: Is there a u-shaped function? American Journal of Epidemiology. 2002;155(3):242–248. doi: 10.1093/aje/155.3.242. [DOI] [PubMed] [Google Scholar]
- Nagoshi CT. Perceived control of drinking and other predictors of alcohol use and problems in college. Addiction Research. 1999;7(4):291–306. [Google Scholar]
- O’Malley PM, Johnston LD. Epidemiology of alcohol and other drug use among American college students. Journal of Studies on Alcohol Supplement. 2002;63:23. doi: 10.15288/jsas.2002.s14.23. [DOI] [PubMed] [Google Scholar]
- Ozegovic JJ, Bikos LH, Szymanski DM. Trends and predictors of alcohol use among undergraduate female students. Journal of College Student Development. 2001;42(5):447–455. [Google Scholar]
- Park CL, Grant C. Determinants of positive and negative consequences of alcohol consumption in college students: Alcohol use, gender, and psychological characteristics. Addictive Behaviors. 2005;30(4):755–765. doi: 10.1016/j.addbeh.2004.08.021. [DOI] [PubMed] [Google Scholar]
- Parkerson GR, Broadhead WE, Tse CJ. The Duke Health Profile: A 17-item measure of health and dysfunction. Medical Care. 1990;28(11):1056–1072. doi: 10.1097/00005650-199011000-00007. [DOI] [PubMed] [Google Scholar]
- Peterson JB, Morey J, Higgins DM. You drink, I drink: Alcohol consumption, social context and personality. Individual Differences Research. 2005;3(1):50–58. [Google Scholar]
- Poikolainen K, Paljarvi T, Makela P. Alcohol and the preventive paradox: Serious harms and drinking patterns. Addiction. 2007;102(4):571–578. doi: 10.1111/j.1360-0443.2006.01740.x. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Walton KE, Bogg T. Conscientiousness and health across the life course. Review of General Psychology. 2005;9(2):156–168. [Google Scholar]
- Rohsenow DJ. Social anxiety, daily moods, and alcohol use over time among heavy social drinking men. Addictive Behaviors. 1982;7(3):311–315. doi: 10.1016/0306-4603(82)90062-4. [DOI] [PubMed] [Google Scholar]
- Seeman M, Seeman AZ. Life strains, alienation, and drinking behavior. Alcoholism: Clinical and Experimental Research. 1992;16(2):199–205. doi: 10.1111/j.1530-0277.1992.tb01364.x. [DOI] [PubMed] [Google Scholar]
- Task Force of the National Advisory Council on Alcohol Abuse and Alcoholism. A call to action: Changing the culture of drinking at U.S. colleges. Rockville, MD: National Institutes of Health, U.S. Department of Health and Human Services; 2002. [Google Scholar]
- Vaux A. Social support: Theory, research and intervention. Westport, CT: Praeger; 1988. [Google Scholar]
- Vickers KS, Patten CA, Bronars C, Lane K, Stevens SR, Croghan IT, et al. Binge drinking in female college students: The association of physical activity, weight concern, and depressive symptoms. Journal of American College Health. 2004;53(3):133–140. doi: 10.3200/JACH.53.3.133-140. [DOI] [PubMed] [Google Scholar]
- Walters ST, Roudsari BS, Vader AM, Harris TR. Correlates of protective behavior utilization among heavy-drinking college students. Addictive Behaviors. 2007;32:2633–2644. doi: 10.1016/j.addbeh.2007.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Dowdall GW, Maenner G, Gledhill-Hoyt J, Lee H. Changes in binge drinking and related problems among American college students between 1993 and 1997. Journal of American College Health. 1998;47(2):57–68. doi: 10.1080/07448489809595621. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Lee JE, Kuo M, Seibring M, Nelson TF, Lee H. Trends in college binge drinking during a period of increased prevention efforts. Journal of American College Health. 2002;50(5):203–217. doi: 10.1080/07448480209595713. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Moeyskens B, Davenport A, Castillo S, Hansen J. The adverse impact of heavy episodic drinkers on other college students. Journal of Studies on Alcohol. 1995;56(6):628–634. doi: 10.15288/jsa.1995.56.628. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Nelson TF. What we have learned from the Harvard School of Public Health College Alcohol Study: Focusing attention on college student alcohol consumption and the environmental conditions that promote it. Journal of Studies on Alcohol & Drugs. 2008;69(4):481–490. doi: 10.15288/jsad.2008.69.481. [DOI] [PubMed] [Google Scholar]
- Weitzman ER. Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. Journal of Nervous and Mental Disease. 2004;192(4):269–277. doi: 10.1097/01.nmd.0000120885.17362.94. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50(1):30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- Wright LS. Correlates of reported drinking problems among male and female college students. Journal of Alcohol and Drug Education. 1983;28(3):47–57. [Google Scholar]
- Yu J. Negative consequences of alcohol use among college students: Victims or victimizers? Journal of Drug Education. 2001;31(3):271–287. doi: 10.2190/HFAT-L1TN-G9G6-74KN. [DOI] [PubMed] [Google Scholar]