Abstract
Objectives
Investigate if asthma coaching reduces emergency department (ED) visits and hospitalizations and increases outpatient asthma monitoring (AM) visits.
Design
Randomized controlled trial
Setting
Urban tertiary-care children’s hospital
Participants
Primary caregivers (“parents”) of children age 2–10 years with asthma, Medicaid-insurance, and urban residence who were attending the ED for acute asthma care.
Intervention
18 months of coaching focused on asthma home management, completing periodic outpatient AM visits, and developing collaborative relationship with primary care provider (PCP); or usual care (control group).
Outcome Measures
Primary = ED visits. Secondary = hospitalizations and AM visits (non-acute visits focused on asthma care). Outcomes were measured during year before and 2 years after enrollment.
Results
We included 120 intervention and 121 control parents. More children of coached parents had ≥ 1 AM visit after enrollment (relative risk [RR], 1.21; 95% confidence interval [CI], 1.04–1.41), but proportions with ≥ 4 AM visits over 2 years were low (intervention=20%; control=10%). Similar proportions of children per study group had ≥ 1 ED visit (71/120 versus 76/121; RR, 0.94; 95% CI, 0.77–1.15) and ≥ 1 hospitalization (29/120 versus 32/121; RR, 0.91; 95% CI 0.59–1.41) after enrollment. An ED visit after enrollment was more likely if one occurred before enrollment (RR, 1.46; 95% CI 1.16–1.86; adjusted for study group), but risk was similar per study group when adjusted for previous ED visits (RR, 1.02; 95% CI, 0.82–1.27).
Conclusions
This parental asthma coaching intervention increased outpatient asthma monitoring visits, although these visits were infrequent, but did not reduce ED visits.
INTRODUCTION
Morbidity from asthma is high and disproportionately affects urban children of lower socioeconomic status.1–9 While national asthma guidelines recommend regular primary care provider (PCP) visits to monitor control, adjust medications, and provide education and guidance,10 these visits occur infrequently, especially among children with Medicaid insurance.11–16 Thus, there are few opportunities for parents and PCPs to foster collaborative relationships important for effective chronic care.17
There have been numerous approaches to improving pediatric asthma management. Some have targeted medical providers with programs to enhance therapeutic and communication skills, including providing specific toolkits with resources for parents.18–22 Other interventions have focused on parents and children with educational and support programs to increase follow-up and medication adherence.23 While some programs have had modest success, those targeting underprivileged, Medicaid-insured patients have noted outcomes limited by low adherence to medications and follow-up and poor receptiveness to behavioral and environmental modifications.22
In previous studies we investigated peer coaching to influence multiple behaviors associated with asthma care targeting parents of Medicaid-insured children in St. Louis, Missouri. We found that coaching after emergency department (ED) visits increased PCP follow-up but did not reduce ED visits, and coaching after hospitalizations reduced re-hospitalization but not ED visits.16,17,24 In our experience, lay coaches were effective in engaging parents in meaningful discussions of asthma care, and parents preferred telephone instead of in-person contacts.25 Building on these prior studies, we evaluated long-term coaching to reduce ED visits. This intervention focused on key behaviors (asthma management strategies) including daily management using an asthma action plan, attending asthma monitoring visits at the PCP, and parent-PCP partnership. We hypothesized that 18 months of coaching would increase asthma self-management, asthma monitoring visits and thereby reduce ED visits and hospitalizations.
METHODS
Study Design
This was a randomized controlled trial (RCT) conducted through St. Louis Children’s Hospital, a university-affiliated tertiary-care hospital. Each subject (“parent”) was enrolled for 24 months (18 month intervention period and 6 months of continued chart auditing). The Human Research Protection Office approved study procedures, and all subjects provided informed consent.
Participants, Recruitment, and Study Group Allocation
From 9/1/03 to 5/15/05, during ED visits, we enrolled a convenience sample of “parents” (caregivers serving in the parent role, usually mothers) of eligible children treated for asthma exacerbations in our ED, who spoke English, had working telephones, and agreed to study procedures. Eligible children were age 2–10 years; had, by parent report, an asthma diagnosis and ≥ 1 other visit to the PCP or an ED for acute asthma during the preceding 15 months; resided in local urban zip codes; had Medicaid insurance; and received ≥ 1 albuterol dose during the enrollment visit. We estimate that 10% of approached parents declined to participate. Participation was limited to one parent-child dyad per household. ED clinicians independently directed treatment and determined disposition.
Before completing baseline questionnaires, parents were randomly allocated by a computerized formal probability model masking enrollers, parents, and ED staff to group assignment. Randomization was blocked and stratified by PCP practice (20 strata) to reduce selection bias and adjust for differences between practices. Within each practice, study group allocation was balanced. PCPs were aware the study was ongoing, but not alerted after enrollment occurred.
Asthma Coach Intervention
The intervention was modeled after the coaching process described by Fisher and colleagues24 and based on the Transtheoretical Model of Behavior Change (TTM).26 The targeted asthma management strategies were: have and utilize an updated asthma action plan, complete asthma monitoring (AM) visits at the PCP every 3–4 months, develop collaborative partnership with the PCP (parent feels empowered to co-manage asthma and dialogue regarding asthma care), use controller medication as prescribed and avoid environmental triggers.
Two female lay coaches (both with personal experience in asthma care) were involved throughout the study, and each intervention-group parent was assigned to one coach. Coaches were taught asthma pathophysiology, symptoms, and management principles, and how to communicate effectively, provide psycho-social support to parents during times of stress, assess parents’ readiness to engage (stage-of-change) in targeted management strategies, and promote behavior change using non-directive, non-threatening methods appropriate for the assessed stage-of-change. The coach would assess the parent’s understanding of the management strategies and willingness and confidence to initiate or continue them, including motivators, barriers, and possible solutions to barriers. The coaches were encouraged to use a consistent approach and delivery, including a checklist of management strategies; no specific script was used.
Stage-of-change was categorized according to the standard TTM stages.26 Parents doing the asthma management strategy for > 6 months were categorized as “I still am” (maintenance); if < 6 months, “I am” (action). If a parent was not yet doing the strategy but had a strong motivator, knew barriers and could discuss solutions, “I will” (preparation); if there was no strong motivator, barriers not known or lacked solutions, “I may” (contemplation); if the parent seemed overwhelmed stating many reasons why the strategy could not be done, “I can’t” (precontemplation); if reluctant to even discuss the strategy, “I won’t” (precontemplation).
During each contact, the coach discussed as many management strategies as possible based on her assessment of the parent’s readiness and willingness. It was expected that the parent would likely be in different stages for each strategy so the coach began with the strategy for which the parent seemed most ready, then shifted to those for which there was less confidence. The coaches sought to empower parents to identify motivators, understand barriers, and seek solutions to barriers while being active managers of their children’s asthma.
The intervention was implemented in a flexible manner without a strict schedule of contacts, allowing the coaches to tailor to the parents’ needs.27,28 The goals were to complete initial in-person visits or phone calls during the two weeks after enrollment and ≥ 1 contact (telephone or in-person) per month, or more frequently based on need perceived by the coach or communicated by the parent. Based on our experience, we anticipated contact frequency would decrease as the intervention proceeded towards completion.24 We expected that some parents would be difficult to consistently contact due to their busy schedules, some would be less willing to engage, and some would become more empowered and self-sufficient needing less coaching. For all parents the intervention continued for 18 months regardless of number of contacts or stage achieved.
The coaches maintained computerized records of contacts and recorded their assessments of parents’ stages-of-change for each management strategy discussed. For quality improvement, the coaches met weekly with their supervisor to discuss intervention delivery (e.g. experiences with parents and how they handled challenging situations). This process sharpened the coaches’ skills and ensured similar and consistent approaches.
Coached parents were also telephoned two and six months after enrollment by a pediatric nurse experienced in telephone management of acute asthma to assess understanding of acute symptoms and utility of asthma action plans and answer questions regarding asthma care; information obtained was shared with the coaches.
Usual Care
As per routine, patients discharged from the ED received an instruction sheet29 functioning as a short-term asthma action plan. Patients hospitalized were evaluated by specialized nurses and given discharge instructions emphasizing controller medication use and PCP follow-up.30
Outcomes
The primary outcome was proportion of children per group with ≥ 1 asthma-related ED visit during the 24 months after enrollment. Secondary outcomes were proportions with ≥ 1 asthma-related hospitalization, ≥ 1 asthma monitoring (AM) visit, and ≥ 1 PCP visit for acute asthma. These outcomes were measured by chart review.
Trained research assistants (RAs), masked to study group assignment, audited PCP and study hospital records for each participating child and they abstracted data for office visits, ED visits and hospitalizations that occurred during the 12 months preceding and 24 months following enrollment. ED visits ending in hospitalizations were counted as ED visits in determining the primary outcome. PCP asthma-related visits were subcategorized by presence of acute asthma symptoms and treatment administered/prescribed. AM visits were non-acute visits focused on asthma care, including well-child visits with asthma documented. Routine visits to the hospital asthma clinic were included in outpatient AM visit counts. The RAs also recorded when controller medications (inhaled corticosteroid (ICS) or leukotriene modifiers) and asthma action plans were documented during PCP visits. We did not measure prescription dispersal, filling, or adherence. After study completion investigators, masked to RA’s assessments, verified visit categorizations.
Analysis
SAS 9.1.3 software (Cary, North Carolina) was used for analysis. We estimated a sample size of 210 to detect a 20% difference in the primary outcome (proportion with ≥ 1 ED visit over 2 years) between groups with alpha = 0.05 and power of 0.8. We overenrolled assuming a potential 15% dropout rate.
Relative risk of ED visits, hospitalizations, and outpatient visits were compared between groups using Cochran-Mantel-Haenszel methods. We analyzed rates of ED visits according to intention-to-treat (ITT), including all enrolled subjects, as well as per-protocol, including all eligible enrolled subjects. Comparison of asthma-related ED visits was adjusted for practice strata and for having a prior year asthma-related ED visit (not including enrollment visit). Effect of number of coach contacts on asthma-related ED visits was estimated using logistic regression. Effect of coaching on asthma-related hospitalizations and on AM visits was adjusted for similar prior year events (not including hospitalization at enrollment visits). Effect of number of coaching contacts on AM visits was examined using logistic regression.
RESULTS
Characteristics of Participants
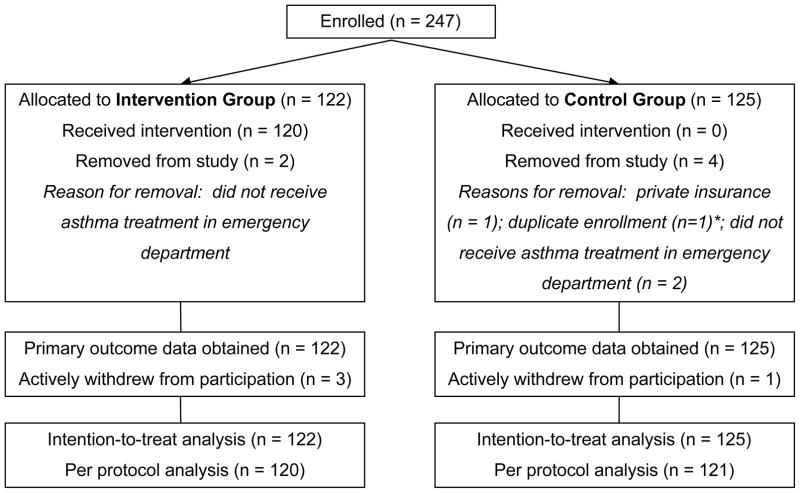
We enrolled 247 parents; 122 allocated to Asthma Coach (AC) and 125 to Usual Care (UC). We withdrew six for ineligibility. (Figure 2) Per-protocol analysis included the remaining 241 parents and children. Baseline characteristics are reported in Tables 1 and 2. Four parents withdrew from ongoing contact; three were in the AC group. Chart audits were completed for all children, except one whose parent also withdrew consent to obtain further outcomes.
Table 1.
Baseline Characteristics of Parents
| Asthma Coach | Usual Care | |
|---|---|---|
| n=120 | n=121 | |
| Gender, female | 116 (97%) | 117 (97%) |
| Age in years | 29.6 (7.6) | 29.3 (7.3) |
| Race | ||
| Black or African American | 113 (94%) | 114 (94%) |
| White | 5 (4%) | 7 (6%) |
| American Indian and African American | 1 (1%) | 0 |
| Other | 1 (1%) | 0 |
| Relationship to child | ||
| Mother | 112 (93%) | 113 (93%) |
| Father | 4 (3%) | 4 (3%) |
| Grandparent | 4 (3%) | 3 (2%) |
| Aunt | 0 | 1 (1%) |
| Number of children in home | 3 (1.5; 1–8) | 3 (2; 1–7) |
| Number of adults in home | 1 (1; 1–5) | 1 (1; 1–4) |
| Highest education level completed | ||
| Did not complete high school | 30 (25%) | 29 (24%) |
| High school graduate, no college | 39 (32%) | 45 (37%) |
| Some college or technical school | 47 (39%) | 36 (30%) |
| College graduate | 4 (3%) | 11 (9%) |
| Work status * | ||
| Employed full-time | 48 (40%) | 59 (49%) |
| Employed part-time | 24 (20%) | 14 (12%) |
| Self-employed | 4 (3%) | 5 (4%) |
| Homemaker | 12 (10%) | 11 (9%) |
| Student | 15 (12%) | 8 (7%) |
| Retired | 1 (1%) | 0 |
| Unable to work | 1 (1%) | 3 (2%) |
| Out of work | 19 (16%) | 25 (21%) |
| Social Isolation ** | 56 (47%) | 50 (41%) |
| Percent Below Federal Poverty Level *** | 28% (22%; 1%–78%) | 28% (21%; 1%–57%) |
Categorical data reported as number (%), continuous data as mean (standard deviation) or median (interquartile range, range).
Multiple responses per subject possible.
Social Isolation was measured using a non-validated tool. Parents were asked how many friends or relatives they can “talk with” or “ask a favor”. Data reflect number of subjects reporting < 7 (median).
Based on parents’ addresses at enrollment and 2000 United States Census Block Group data.
Table 2.
Baseline Characteristics of Children
| Asthma Coach | Usual Care | |
|---|---|---|
| n=120 | n=121 | |
| Gender, male | 77 (64%) | 69 (57%) |
| Age, years | 5.1 (2.5) | 5.2 (2.6) |
| Race | ||
| Black or African American | 113 (94%) | 115 (95%) |
| White | 2 (2%) | 2 (2%) |
| African American and White | 2 (2%) | 4 (3%) |
| American Indian or Alaska Native | 1 (1%) | 0 |
| Other | 2 (2%) | 0 |
| Asthma Symptom Score * | 5 (6; 0–19) | 5 (6; 0–18) |
| Emergency department visits during preceding year | 0 (1; 0–5) | 1 (1; 0–6) |
| Hospitalizations during preceding year | 0 (1; 0–3) | 0 (1; 0–3) |
| Primary Care Provider visits during preceding year | ||
| For Acute Asthma Symptoms | 0 (0; 0–3) | 0 (0; 0–3) |
| For Asthma Monitoring ** | 0 (1; 0–8) | 0 (1; 0–5) |
| Hospitalized at enrollment emergency department visit | 29 (24%) | 25 (21%) |
Categorical data reported as number (%), continuous data reported as mean (standard deviation) or median (interquartile range, range).
Parents were asked 3 questions regarding # of days with symptoms [a) at any point, b) awakening from sleep, and c) interfering with play] within week preceding current exacerbation; maximum score = 21. Although not validated, these questions are based on constructs assessing asthma impairment and severity in the National Asthma Education and Prevention Program. [J Allergy Clin Immunol. 2007;120:S94–138]
Asthma Monitoring visits were non-acute visits focused on asthma care.
Intervention Implementation: Coaching Contacts and Stage-of-Change Movement
The coaches completed initial contacts with 67% of parents within 2 weeks of enrollment, 84% within 4 weeks, and all parents by 127 days [median time = 8 days (25th and 75th percentiles = 3 and 19.5 days)]. During the 18-month intervention, 90% of contacts were phone calls, mean number of contacts/parent was 7.3 ± 4.0 (standard deviation), and mean number of attempts/contact was 8.1 +/− 8.0 (standard deviation). Contact frequency decreased over time as anticipated (Table 3). We examined three specific management strategies and found that coaches were able to engage parents more often in discussing asthma action plan use, less often for asthma monitoring visits and least often for partnership with PCP. (Table 4)
Table 3.
Percentage of Intervention Group Parents with ≥ 1 Coach Contact by Quarter during Intervention Period
| Quarter | Percentage contacted |
|---|---|
| 1 | 98.3 |
| 2 | 75.8 |
| 3 | 61.7 |
| 4 | 45.8 |
| 5 | 49.2 |
| 6 | 41.7 |
For all coached parents the intervention continued for 18 months regardless of number of contacts or stage-of-change achieved.
Table 4.
Frequency of Stage-of-Change Assessment and Progress during Intervention by Three Asthma Management Strategies for Intervention Group Parents (n=120)
| Asthma Action Plan Use | Completing Asthma Monitoring Visit | Partnership between Parent and Primary Care Provider | |
|---|---|---|---|
| Staged at least once for management strategy | 97% | 92% | 85% |
| Mean number of staging episodes per parent | 5.3 | 3.5 | 2.9 |
| Median months to forward movement ≥ 1 stage * | 3 | 14 | 17 |
| Began in action or maintenance stages * | 10% | 26% | 8% |
| Ended in action or maintenance stages * | 54% | 46% | 18% |
Asthma coaches recorded stage-of-change for each management strategy discussed based on their perceptions of the parents.
Stage-of-change categorized along spectrum: I won’t (pre-contemplation) or I can’t (pre-contemplation); I may (contemplation); I will (preparation); I am (action); I still am (maintenance).
Asthma Monitoring visit = non-acute visit focused on asthma care.
Partnership = collaborative relationship between parent and primary care provider.
Effect of Coaching on Outpatient Visits
Coaching increased asthma monitoring (AM) visits and non-asthma PCP visits. (Table 5) AC children were more likely than UC children to have ≥ 1 AM visit (RR, 1.21; 95% CI, 1.04–1.41) during the 2 years after enrollment, and to have ≥ 4 AM visits (RR, 2.02; 95% CI 1.06–3.84), although these proportions were low with the number needed to treat regarding ≥ 4 AM visits of 9.9. Among AC children, the probability of an AM visit increased with each additional coach contact (odds ratio,1.27; 95% CI 1.08–1.50). Having an AM visit after enrollment was more likely if an AM visit occurred before enrollment (RR, 1.33; 95% CI 1.14–1.54; adjusted for study group). After adjusting for having prior year AM visits, children of coached parents were more likely to have AM visits after enrollment (RR, 1.20; 95% CI 1.04–1.39). While AC children were more likely to have ≥ 1 AM visit with documented controller medication, this percentage was still low (58%); median number of such visits over the 2-year follow-up = 1. Asthma action plan documentation in PCP records was similar between groups and too infrequent for further analysis.
Table 5.
Health Care Visits by Study Group
| Asthma Coach n=120 | Usual Care n=121 | Relative Risk (95% CI) | |
|---|---|---|---|
| ED Visit for Asthma | |||
| Children with ≥ 1 visit, number (%) | 71 (59%) | 76 (63%) | 0.94 (0.77–1.15) |
| Total number of visits, median (range) | 1 (0–11) | 1 (0–9) | |
| Time until first visit, mean months | 4.4 (0.13–22.0) | 5.9 (0.03–21.8) | |
| ED visit for Any Reason | |||
| Children with ≥ 1 visit, number (%) | 92 (77%) | 95 (79%) | 0.98 (0.85–1.12) |
| Total number of visits, median (range) | 2 (0–24) | 2 (0–14) | |
| Hospitalization for Asthma | |||
| Children with ≥ 1 hospitalization, number (%) | 29 (24%) | 32 (26%) | 0.91 (0.59–1.41) |
| Total number of hospitalizations, median (range) | 0 (0–6) | 0 (0–4) | |
| Time until first hospitalization, mean months | 6.0 (0.79–22.1) | 7.9 (0.16–23.4) | |
| Asthma Monitoring (AM) Visit * | |||
| Children with ≥ 1 visit, number (%) | 97 (81%) | 81 (67%) | 1.21 (1.04–1.41) |
| Children with ≥ 4 visits, number (%) | 24 (20%) | 12 (10%) | 2.02 (1.06–3.84) |
| Total number of visits, median (range) | 2 (0–10) | 1 (0–11) | |
| AM Visit with Controller Medication Documentation | |||
| Children with ≥ 1 visit, number (%) | 70 (58%) | 52 (43%) | 1.36 (1.05–1.75) |
| Total number of visits, median (range) | 1 (0–5) | 0 (0–4) | |
| PCP Visit with Asthma Action Plan Documentation | |||
| Children with ≥ 1 visit, number (%) | 12 (10%) | 13 (11%) | 0.93 (0.44–1.96) |
| Total number of visits, median (range) | 0 (0–3) | 0 (0–2) | |
| PCP Visit for Acute Asthma Symptoms | |||
| Treatment Documented | |||
| Children with ≥ 1 visit, number (%) | 27 (23%) | 17 (14%) | 1.60 (0.92–2.78) |
| Total number of visits, median (range) | 0 (0–7) | 0 (0–3) | |
| No Treatment Documented | |||
| Children with ≥ 1 visit, number (%) | 39 (32%) | 28 (23%) | 1.40 (0.93–2.13) |
| Total number of visits, median (range) | 0 (0–10) | 0 (0–4) | |
| PCP Well-Child Visit without Asthma Documentation | |||
| Children with ≥ 1 visit, number (%) | 16 (13%) | 14 (12%) | 1.15 (0.59–2.26) |
| Total number of visits, median (range) | 0 (0–2) | 0 (0–2) | |
| PCP Non-Asthma Visit | |||
| Children with ≥ 1 visit, number (%) | 51 (43%) | 35 (29%) | 1.47 (1.04–2.08) |
| Total number of visits, median (range) | 0 (0–5) | 0 (0–7) |
Data represent visits occurring during the two years following enrollment; n=241; per protocol analysis
ED = emergency department, PCP = primary care provider.
Medians compared using Wilcoxon rank sum test.
Asthma Monitoring visit = non-acute visit focused on asthma care; included PCP well-child visits with asthma documented and hospital asthma clinic visits. [similar proportions per group with ≥ 1 asthma clinic visit; Asthma Coach= 22%, Usual Care=15%, p=0.19, Jonckheere-Terpstra test].
Effect of Coaching on Emergency Department Visits
Similar proportions of children per group had ≥ 1 asthma-related ED visit during the 2 years after enrollment (ITT analysis; AC=69/122, UC=67/125). Having an ED visit after enrollment was more likely if an ED visit occurred before enrollment (RR, 1.46; 95% CI 1.16–1.86; adjusted for study group), but risk was similar per group when adjusted for previous ED visits (RR, 1.02; 95% CI, 0.82–1.27). Indicators of more severe disease at enrollment (symptom score > median or hospitalization) did not change the effect of coaching on ED visits. Among coached parents, the number of ED visits did not vary with number of coach contacts. Total numbers of asthma-related ED visits and ED visits for any reason were similar between groups (Table 5).
Effect of Coaching on Hospitalizations
Proportions of children with ≥ 1 asthma-related hospitalization after enrollment were similar between groups. (Table 5) Having a hospitalization after enrollment was more likely if a hospitalization occurred before enrollment (RR, 2.45; 95% CI 1.59–3.77; adjusted for study group), but risk of a hospitalization after enrollment was similar by study group when adjusted for having a hospitalization before enrollment (RR, 0.86; 95% CI, 0.56–1.30).
Effect of Coaching and Asthma Monitoring Visits on Emergency Department Visits
Controlling for study group and prior year ED visits, neither having an AM visit nor an AM visit with documented controller medication decreased the likelihood of ≥ 1 asthma-related ED visit (RR, 1.18; 95% CI, 0.92–1.52; and; RR, 1.29; 95% CI, 1.05–1.58, respectively). Only 13% of ED visits were preceded by PCP visits within 2 weeks, and this interval was > 4 weeks for 73% of ED visits with no difference by study group
COMMENT
We investigated parental asthma coaching to improve important aspects of care and reduce morbidity in a high risk population. While coaching increased self-reported use of action plans and chart audit-confirmed asthma monitoring visits including those with documented controller medications, these changes were not associated with fewer ED visits. Others have shown that continuity of care can reduce ED visits31 and that collaborative patient-PCP partnership is important for high-quality chronic care.17 It appears that the monitoring visits that we achieved were too infrequent to affect these outcomes. How to foster effective collaborative patient-PCP partnerships remains challenging.
Reducing ED visits is an important but elusive goal of asthma management.10 A recent Cochrane Collaboration© review reported that “educational interventions” for children (and caregivers) treated in the ED for asthma lowers risk for ED visits and hospitalizations, but noted “significant heterogeneity” among interventions and populations studied.23 Of the RCTs that enrolled low-income, urban, disadvantaged families and measured ED visits as the primary outcome, only two reported benefit.23,32,33 Both of them measured ED visits by parent report,32,33 and one reported outcomes for only 6 months.32 We measured visits for two-years after enrollment using medical record review rather than relying on parent-report – important differences in design that may explain the variation in findings.
The factor most associated with an ED visit after enrollment was a prior ED visit. What drives this phenomenon is unclear. Others have reported that many urban parents of children with asthma prefer the ED “because they perceived it provides the best quality care.”34,35 In our study, PCP visits for acute asthma were rarer than ED visits, few ED visits were preceded by a PCP visit, and 28% of children had a PCP visit with acute symptoms but no documented treatment. If over-reliance on the ED is due to lack of an alternative source of effective acute management guidance, one solution may be a nurse-staffed call center that utilizes an asthma management protocol.36
Like similar studies, we experienced challenges delivering this intervention. By design it was implemented flexibly without a strict schedule or mandatory number of contacts. Yet, maintaining consistent contact was challenging due in part to parents’ frequent phone disconnections. It is possible that more frequent coach contacts may improve sustainability and effectiveness of the program.
Our study has limitations not yet discussed. We enrolled a convenience sample and did not collect data on those not enrolled. However, in another coaching study in this ED using a similar recruitment strategy,16 we carefully characterized the potential for selection bias and found no evidence.37 For ED visits and hospitalizations, only records from this hospital were reviewed, and St. Louis has another children’s hospital with an ED. However, according to a recent study, our hospital accounted for 70% of asthma-related hospitalizations among children ≥ 14 years-old in these zip codes, and only 5% were subsequently admitted at the other hospital.9 It is unlikely that underestimation of visits by this small amount biased results. We did not measure PCP care beyond chart review and acknowledge inherent limitations in such data. Consequently, we may have underestimated provision of controller medications, provision of acute treatment, and provision of action plans, but any measurement error is unlikely to have differed by study group.
Conclusion
In conclusion, this parental coaching intervention increased asthma monitoring visits although such visits remained infrequent, and did not reduce ED visits or hospitalizations. Future interventions to reduce morbidity for this patient population should include strategies targeting both the parent and the PCP to accomplish the goals of a collaborative model of chronic disease management as described by Wagner et al.17 Lay asthma coaches were well accepted by this high risk population and could be included in such a system of care delivery.
Figure 1. Participant Flow Chart.
* Duplicate enrollment involved a parent enrolled again during a subsequent ED visit with a different child; she was allocated to UC each time and continued with data collection only for the first child.
Acknowledgments
This study was funded by a grant from the National Heart Lung Blood Institute (HL 072919).
The authors acknowledge the efforts, expertise and guidance from Drs. David M. Jaffe and Ellen F. Crain as the data-safety monitors, and thank Drs. Gordon R. Bloomberg and James P. Keating for their helpful advice.
Footnotes
Dr. Trinkaus had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Akinbami L Centers for Disease Control and Prevention National Center for Health Statistics. The state of childhood asthma, United States, 1980–2005. Adv Data. 2006;381:1–24. [PubMed] [Google Scholar]
- 2.Moorman JE, Rudd RA, Johnson CA, et al. Centers for Disease Control and Prevention (CDC) National surveillance for asthma – United States, 1980–2004. MMWR Surveill Summ. 2007;56:1–54. [PubMed] [Google Scholar]
- 3.Akinbami LJ, Schoendorf KC. Trends in childhood asthma: prevalence, health care utilization and mortality. Pediatrics. 2002;110:315–322. doi: 10.1542/peds.110.2.315. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Asthma prevalence and control characteristics by race/ethnicity – United States, 2002. MMWR Morb Mortal Wkly Rep. 2004;53:145–148. [PubMed] [Google Scholar]
- 5.Miller JE. The effects of race/ethnicity and income on early childhood asthma prevalence and health care use. Am J Public Health. 2000;90:428–430. doi: 10.2105/ajph.90.3.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Halfon N, Newacheck PW. Childhood asthma and poverty: differential impacts and utilization of health services. Pediatrics. 1993;91:56–61. [PubMed] [Google Scholar]
- 7.Simon PA, Zeng Z, Wold CM, Haddock W, Fielding JE. Prevalence of childhood asthma and associated morbidity in Los Angeles County: Impacts of race/ethnicity and income. J Asthma. 2003;40:535–543. doi: 10.1081/jas-120018788. [DOI] [PubMed] [Google Scholar]
- 8.Gold DR, Wright R. Population disparities in asthma. Annu Rev Public Health. 2005;26:89–113. doi: 10.1146/annurev.publhealth.26.021304.144528. [DOI] [PubMed] [Google Scholar]
- 9.Bloomberg GR, Trinkaus KM, Fisher EB, Jr, Musick JR, Strunk RC. Hospital readmissions for childhood asthma: a 10-year metropolitan study. Am J Respir Crit Care Med. 2003;167:1068–1076. doi: 10.1164/rccm.2201015. [DOI] [PubMed] [Google Scholar]
- 10.National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the diagnosis and management of asthma - summary report 2007. J Allergy Clin Immunol. 2007;120:S94–138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 11.Reeves MJ, Bohm SR, Korzeniewski SJ, Brown MD. Asthma care and management before an emergency department visit in children in western Michigan: how well does care adhere to guidelines? Pediatrics. 2006;117:S118–126. doi: 10.1542/peds.2005-2000I. [DOI] [PubMed] [Google Scholar]
- 12.Smith SR, Wakefield DB, Cloutier MM. Relationship between pediatric primary provider visits and acute asthma ED visits. Pediatr Pulmonol. 2007;42:1041–1047. doi: 10.1002/ppul.20694. [DOI] [PubMed] [Google Scholar]
- 13.Cabana MD, Bruckman D, Bratton SL, Kemper AR, Clark NM. Association between outpatient follow-up and pediatric emergency department asthma visits. J Asthma. 2003;40:741–749. doi: 10.1081/jas-120023499. [DOI] [PubMed] [Google Scholar]
- 14.Zorc JJ, Scarfone RJ, Li Y, et al. Scheduled follow-up after a pediatric emergency department visit for asthma: a randomized trial. Pediatrics. 2003;111:495–502. doi: 10.1542/peds.111.3.495. [DOI] [PubMed] [Google Scholar]
- 15.Smith SR, Jaffe DM, Fisher EB, Trinkaus KM, Highstein G, Strunk RC. Improving follow-up for children with asthma after an acute emergency department visit. J Pediatr. 2004;145:772–777. doi: 10.1016/j.jpeds.2004.08.029. [DOI] [PubMed] [Google Scholar]
- 16.Smith SR, Jaffe DM, Highstein G, Fisher EB, Trinkaus KM, Strunk RC. Asthma coaching in the pediatric emergency department. Acad Emerg Med. 2006;13:835–839. doi: 10.1197/j.aem.2006.03.565. [DOI] [PubMed] [Google Scholar]
- 17.Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: Translating evidence into action. Health Affairs. 2001;20:64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 18.Cloutier MM, Hall CB, Wakefield DB, Bailit H. Use of asthma guidelines by primary care providers to reduce hospitalizations and emergency department visits in poor, minority, urban children. J Pediatr. 2005;146(5):591–597. doi: 10.1016/j.jpeds.2004.12.017. [DOI] [PubMed] [Google Scholar]
- 19.Cloutier MM, Wakefield DB, Sangeloty-Higgins P, Delaronde S, Hall CB. Asthma guideline use by pediatricians in private practices and asthma morbidity. Pediatrics. 2006;118(5):1880–1887. doi: 10.1542/peds.2006-1019. [DOI] [PubMed] [Google Scholar]
- 20.Halterman JS, Fisher S, Conn KM, Fagnano M, Lynch K, Marky A, Szilagyi PG. Improved preventive care for asthma: a randomized trial of clinician prompting in pediatric offices. Arch Pediatr Adol Med. 2006;160(10):1018–1025. doi: 10.1001/archpedi.160.10.1018. [DOI] [PubMed] [Google Scholar]
- 21.Cabana MD, Slish KK, Evans D, Mellins RB, Brown RW, Lin X, Kaciroti N, Clark NM. Impact of physician asthma care education on patient outcomes. Pediatrics. 2006;117(6):2149–2157. doi: 10.1542/peds.2005-1055. [DOI] [PubMed] [Google Scholar]
- 22.Bratton SL, Cabana MD, Bron RW, et al. Asthma educational seminar targeting Medicaid providers. Repir Care. 2006;51:49–55. [PubMed] [Google Scholar]
- 23.Boyd M, Lasserson TJ, McKean MC, Gibson PG, Ducharme FM, Haby M. Interventions for educating children who are at risk of asthma-related emergency department attendance. Cochrane Database Syst Rev. 2009:CD001290. doi: 10.1002/14651858.CD001290.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fisher EB, Strunk RC, Highstein GR, et al. Randomized controlled evaluation of the effect of community health workers on hospitalization for asthma: the asthma coach. Arch Pediatr Adol Med. 2009;163:225–232. doi: 10.1001/archpediatrics.2008.577. [DOI] [PubMed] [Google Scholar]
- 25.Garbutt JM, Banister C, Highstein G, et al. Telephone coaching for parents of children with asthma: impact and lessons learned. Arch Pediatr Adolesc Med. 2010;164:625–630. doi: 10.1001/archpediatrics.2010.91. [DOI] [PubMed] [Google Scholar]
- 26.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: Toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 27.Prochaska JO, DiClemente CC, Velicer WF, Rossi JS. Standardized, individualized, interactive and personalized self-help programs for smoking cessation. Health Psychol. 1993;12:399–405. doi: 10.1037//0278-6133.12.5.399. [DOI] [PubMed] [Google Scholar]
- 28.Skinner BF. Science and Human Behavior. New York, NY: Macmillan; 1953. [Google Scholar]
- 29.Petersen DL, Murphy DE, Jaffe DM, et al. A tool to organize instructions at discharge after treatment of asthmatic children in an emergency department. J Asthma. 1999;36:597–603. doi: 10.3109/02770909909087297. [DOI] [PubMed] [Google Scholar]
- 30.Borgmeyer A, Gyr PM, Jamerson PA, Henry LD. Evaluation of the role of the pediatric nurse practitioner in an inpatient asthma program. J Pediatr Health Care. 2008 Sep-Oct;22(5):273–81. doi: 10.1016/j.pedhc.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 31.Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics. 2001;107:514–529. doi: 10.1542/peds.107.3.524. [DOI] [PubMed] [Google Scholar]
- 32.Teach SJ, Crain EF, Quint DM, Hylan ML, Joseph JG. Improved asthma outcomes in a high-morbidity pediatric population: results of an emergency department-based randomized clinical trial. Arch Pediatr Adolesc Med. 2006;160:535–541. doi: 10.1001/archpedi.160.5.535. [DOI] [PubMed] [Google Scholar]
- 33.Butz AM, Tsoukleris MG, Donithan M, et al. Effectiveness of nebulizer use-targeted asthma education on underserved children with asthma. Arch Pediatr Adolesc Med. 2006;160:622.628. doi: 10.1001/archpedi.160.6.622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Valerio M, Cabana MD, White DF, Heidmann DM, Brown RW, Bratton SL. Understanding of asthma management: Medicaid parents’ perspectives. Chest. 2006;129:594–601. doi: 10.1378/chest.129.3.594. [DOI] [PubMed] [Google Scholar]
- 35.Mansour ME, Lanphear BP, DeWitt TG. Barriers to asthma care in urban children: parent perspective. Pediatrics. 2000;106:512–519. doi: 10.1542/peds.106.3.512. [DOI] [PubMed] [Google Scholar]
- 36.Nelson KA, Freiner D, Garbutt J, et al. Acute asthma management by a pediatric after-hours call center. Telemed J E Health. 2009;15:538–545. doi: 10.1089/tmj.2009.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smith SR, Jaffe DM, Petty M, Worthy V, Banks P, Strunk RC. Recruitment into a long-term pediatric asthma study during emergency department visits. J Asthma. 2004;41:477–484. doi: 10.1081/jas-120033991. [DOI] [PubMed] [Google Scholar]