Abstract
The bacterial pathogen Helicobacter pylori has co-evolved with humans and colonizes roughly one half of the human population, but only causes overt gastric disease in a subset of infected hosts. In this Review, we discuss the pathogenesis of this bacterium and the mechanisms it uses to promote persistent colonization of the gastric mucosa, with a focus on recent insights into the role of the virulence factors VacA, CagA and CagL. We also describe the immunobiology of H. pylori infection and highlight how this bacterium manipulates the innate and adaptive immune systems of the host to promote its own persistence.
Helicobacter pylori is a highly successful human pathogen that colonizes roughly one half of the world's population. It is typically transmitted orally within families during early childhood and can persist for decades in its preferred niche, the gastric mucosa, despite triggering vigorous innate and adaptive immune responses. H. pylori infection causes chronic gastritis, which is asymptomatic in the majority of carriers but is considered a major risk factor for the development of gastric and duodenal ulcers and the two gastric malignancies, mucosa-associated lymphoid tissue lymphoma and gastric adenocarcinoma1. In addition to its tight association with cancer, H. pylori stands out among other Gram-negative bacterial pathogens in its ability to persist and establish chronic infection.
Contrary to long-held dogma, the stomach is not a sterile organ and is estimated to support a community composed of up to 200 different species2. However, when H. pylori is present it tends to be numerically dominant and readily visible in gastric biopsy tissue sections as helical rod-shaped organisms covering the gastric epithelial cells and surrounding mucus. Initial colonization depends on bacterial urease activity and cell-shape modulation to penetrate the gastric mucus. Constitutive DNA and protein repair pathways, combined with bacterial genome diversification and attenuation of host cell chemical radical production are now recogized as essential for persistence of the bacterium in this niche. The two known H. pylori toxins, VacA and CagA, have been the focus of much work aimed at understanding H. pylori virulence. While work on VacA has been reviewed recently3, we highlight new insights on functional interactions between VacA and CagA and the modulation of immune responses by VacA and another secreted virulence factor, the γ-glutamyl transpeptidase (GGT).
Besides its aresenal of virulence factors, persistence of H. pylori is strongly influenced by the ability of the bacterium to evade, subvert and manipulate the host's immune system. This bacterium can evade detection by several innate immune receptors through target modification and it can also subvert other innate recognition pathways through the suppression of downstream signal transduction, while evasion of adaptive immunity is achieved by the modulation of T-cell effector functions.
In this review we discuss the remarkable ability of H. pylori to colonize and persist in the hostile environment of the human stomach, through the interplay of several secreted virulence factors and sophisticated manipulation of innate and adaptive immune responses. We also highlight progress on understanding the consequences of persistence for both the bacterium and the host.
Colonization of the gastric mucosa
Escape from the acidic lumen
The stomach is a particularly challenging niche for bacterial habitation. In the lower bowel, which has a neutral or slightly alkaline pH, bacterial density is highest in the lumen; by contrast, the production of gastric acid in the stomach, which results in a pH of 1-2, severely limits luminal colonization. Indeed, H. pylori can only survive for minutes in the stomach lumen and must quickly migrate to the gastric epithelial surface4. Similar to the intestine, the mucus layer in the stomach forms a physical barrier to bacterial penetration and likely a scaffold for the binding of antimicrobial compounds of the host5. Bacterial urease production is required for acid resistance through the localized production of ammonium ions, and flagellar-based motility allows penetration of the mucus (Figure 1)6. Furthermore, urease activity facilitates flagellar motility through the mucus layer by changing the viscoelasticity properties of gastric mucins. At low pH, gastric mucins form a gel that effectively traps the bacteria, but urease-catalyzed production of ammonium ions raises the pH to near neutral and the mucus gel transitions to a viscoelastic solution through which H. pylori can swim7, 8. Regulators of motility, including chemotaxis9-12 and cell shape13-15 have been probed to discover additional colonization factors and to better define H. pylori's optimal niche. Helical cell shape is thought to enhance motility through viscous media by a corkscrew mechanism and cell shape mutants that have lost helical twist and/or curvature show attenuated colonization13-15. Mutants in several chemotaxis components show altered localization including lower numbers of bacteria in close association with gastric epithelial cells16 or deeply penetrating the gastric glands9. In addition to promoting clearance, the altered localization of chemotaxis mutants correlates with lower inflammation, impaired recruitment of CD4+ T-cells and the absence of a T-helper 17 response10, 16. Thus, the intimate association with the gastric epithelium promotes stable infection while simultaneously provoking more inflammation. Higher inflammation correlates with lower bacterial loads17, which suggests that H. pylori must actively manage its interaction with the host epithelium to avoid clearance and persist at this site (Figure 1).
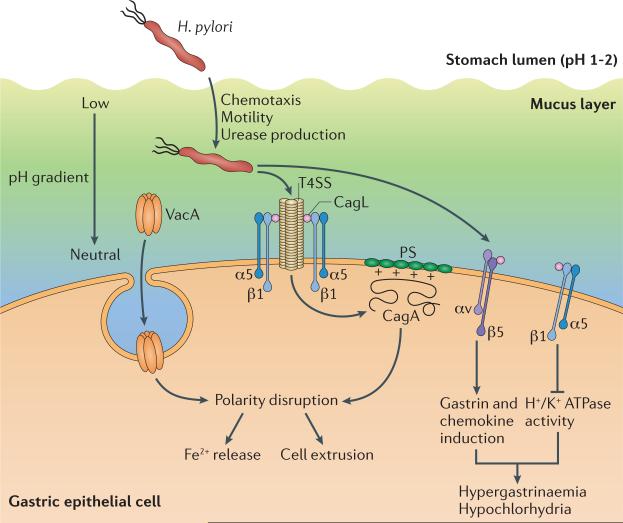
Figure 1. H. pylori colonization and persistence factors.
During initial infection of the stomach lumen, urease-dependent ammonia production locally raises the pH, which promotes bacterial survival and solubilizes the mucus gel to facilitate bacterial motility. Chemotaxis(driven by pH and possibly other gradients) and helical rod shape promote flagellar-based motility away from the acidic lumen to H. pylori's preferred niche, on and adjacent to gastric epithelial cells. SabA, BabA and other variably expressed adhesins may shift the balance to cell-associated bacteria. Inset: cell-associated bacteria alter gastric epithelial cell behavior through VacA, CagA and CagL which all have multiple cellular targets. This includes CagA and VacA dependent disruption of cell polarity that can promote iron acquisition or cell extrusion, CagA and CagL dependent induction of chemokines and/or the gastric hormone gastrin, CagL dependent inhibition of acid secretion by the H+/K+ ATPase, and affects on proliferation, apoptosis and differentiation mediated by all three effectors. As noted in the main text, in addition to CagL (depicted), CagA and CagY have also been shown to bind α5β1 integrins although the precise interaction surface remains to be determined. fla, flagella; che, chemotaxis; ure, urease; T4SS, Cag Type IV secretion system; PS, phosphatidylserine; α5β1 and αvβ5, indicated integrin subunits.
Persistent colonization of the gastric mucosa
H. pylori uses diverse strategies to promote its survival in the face of robust immune responses. All H. pylori strains encode proteins important for detoxifying reactive oxygen species (for example, catalase and superoxide dismutase) and H. pylori arginase limits NO production by macrophage-, neutrophil- and epithelial cell-derived nitric oxide synthase18, 19. Moreover, multiple DNA repair pathways contribute to efficient colonization20 even while the surrounding host tissue accumulates DNA lesions21, 22. Recent work has shown that H. pylori strains constitutively express DNA repair proteins such as RecA and thus lack a classic SOS response to DNA damage23, 24. Upon DNA damage, H. pylori instead upregulates natural competence which promotes chronic persistence, likely through enhanced genetic diversification23, 25.
The H. pylori genome contains multiple intragenic and extragenic repeat sequences26. CagY, which is expressed on the cell surface and is required for the T4SS-mediated translocation of the effector CagA (see below), can undergo recombination between internal repeat motifs that generally preserve the reading frame27. During experimental infection of mice and rhesus macaques, CagY variants accumulate that have gained or lost T4SS activity. These results suggest that CagA translocation and the associated biological responses, including inflammation, may have both beneficial and detrimental effects on bacterial persistence leading to selection for both retention and loss of T4SS activity28.
Among the 60 predicted outer membrane proteins (OMPs), the HOP family shares highly similar or identical sequences at their amino and carboxy termini and includes sevearl known or predicted H. pylori adhesins that promote binding to the gastric epithelium29. These shared sequences could promote intra- or intergenomic recombination. Sequencing of H. pylori HOP loci from human clinical strain collections has revealed likely gene conversion of the Lewis B binding adhesin gene babA with babB or babC30-33 and of sabB with the sialyl-Lewis binding adhesin sabA or omp2734-36. During experimental rhesus macaque or mouse infection, replacement of babA with babB results in strains that have lost the ability to bind immobilized Lewis B antigens32, 37. Additionally, replacement of sabA with sabB leads to strains expressing two copies of sabA, which results in increased binding to sialyl-Lewis antigens on murine gastric tissues36. Some alleles of babA and sabA can undergo phase variation by slipped strand mispairing at dinucleotide sequences in the coding sequences or homopolymeric tracts in their promoters, again leading to either loss or elevated gene expression38-40. The carbohydrate antigens bound by these adhesins can be expressed on the cell surface and/or on secreted glycoproteins such as mucin. Furthermore some of these antigens, such as sialyl-Lewis antigens, are induced during inflammation. Phase variation by gene conversion and slipped strand mispairing allows for development of subpopulations with variable adherence properties that could allow the pathogen to evade immune responses or resist shedding. This ability to generate diverse subpopulations may also impact transmission to new hosts.
Secreted toxins of H. pylori
VacA and CagA effectors
H. pylori strains actively manipulate host tissues and promote their own persistence through the activity of a number of secreted toxins, some of which are discussed below. Vacuolating cytotoxin A (VacA), which was recently reviewed3, is a pore-forming toxin that disrupts cell polarity, promotes apoptosis of epithelial cells and inhibits T-cell proliferation and effector functions3. The vacA gene is carried by all H. pylori strains, and sequence variation in several domains of this protein is linked to varying expression levels and cell type specific toxicity, as well as disease severity3. Another important toxin is cytotoxin-associated gene A (CagA). Originally characterized as an immunodominant antigen from patients infected with highly virulent vacA alleles41, 42, CagA is translocated into host cells by the Cag type IV secretion system (T4SS) encoded on the cag pathogenicity island (PAI)1, 43. Strains expressing CagA are associated with an increased cancer risk and transgenic expression of CagA in mice induces gastric carcinoma and other malignancies, which has lead to its designation as a bacterial oncoprotein44.
CagA-VacA interactions
To act as an oncoprotein, CagA must persist in cells or act in a hit and run manner. CagA has not been readily detected in gastric cancer tissues45 and thus was suggested to have an early causative role in cancer progression. It has now been elegantly shown that translocated CagA is degraded by autophagy during infection by H. pylori strains carrying the m1 allele of VacA via the ability of this VacA isoform to bind the cell surface receptor low-density lipoprotein receptor-related protein-1 (LRP1)46. VacA binding of LPR1 leads to loss of reduced glutathione (GSH) in the cell and increased production of reactive oxygen species (ROS). This in turn activates Akt kinase-dependent degradation of the tumour suppressor p53 and induction of autophagy that degrades CagA. Interestingly, autophagy is not activated in cells expressing a variant form of the CD44 adhesion molecule46. These cells have increased intracellular levels of GSH due to activation of xCT, a glutamate-cysteine transporter47 and therefore do not induce ROS or autophagy upon VacA binding. CD44 is a cell surface marker associated with epithelial cancer stem cells and CagA could be detected in variant-CD44 expressing cells from gastric cancer patients46. Paradoxically, tissue changes associated with H. pylori-induced gastric carcinogenesis, including development of intestinal metaplasia, were thought to render the stomach less hospitable for H. pylori colonization leading to lower colonization loads. However, H. pylori was shown to intimately interact with gastric progenitor cells in a mouse infection model48. The ability of H. pylori to colonize cells having stem cell-like properties and persistance of CagA protein in these cells due to the activiation of xCT and thus impaired autophagy dependent CagA degradation could provide a mechanism for a sustained role of H. pylori colonization and CagA in oncogenesis.
Once translocated into host cells, CagA can be tyrosine phosphorylated on EPIYA motifs49 by Src- and Abl family kinases. These two types of kinases are activated sequentially and in a tightly regulated manner, with Src kinases mediating the initial, preferential phosphorylation of EPIYA-C (and –D) motifs and Abl kinases phosphorylating any EPIYA motif at later time points post-infection50. Phosphorylated CagA interacts with SHP-2 tyrosine phosphatase and Csk kinase while unphosphorylated CagA is known to interact with Crk adaptor, c-Met, Grb2, PAR1/MARK and E-cadherin43. Collectively, these interactions lead to altered cell signalling and changes in cell polarity, extrusion, motility, proliferation and pro-inflammatory cytokine secretion1, 43 As discussed below, many of these phenotypes have now been linked to acquistion of nutrients by the bacterium to promote persistance and/or host pathology.
Under standard conditions, CagA expression is not required for stomach colonization, but promotes inflammation in the Mongolian gerbil model51. Cag T4SS activity is often lost during murine infection, which complicates efforts to elucidate the pathophysiological roles of CagA during chronic H. pylori infection28, 52, 53. However, in a polarized cell culture model, CagA promotes increased basolateral uptake and transcytosis of transferrin while VacA drives mislocalization of the transferrin receptor to sites of bacterial attachment to facilitate iron acquisition by the bacterium54. In cagA mutants, the formation of microcolonies on the apical surface of the cell requires iron supplementation, whereas this is not a requirement for wild-type bacteria, suggesting that CagA- and VacA-dependent cell polarity perturbations confer a nutritional benefit. Consistent with this hypothesis, CagA is required for efficient colonization of Mongolian gerbils under iron-limiting conditions54. Thus CagA and VacA collaborate to promote efficient colonization in the iron-limited environment of the stomach and to moderate pathologic effects of CagA.
Ultrastructural insights into CagA secretion
Given the importance of CagA in persistance and pathology, there has been much interest in the mechanisms governing CagA delivery into host cells. Translocation of CagA from the bacterium to the host cell cytosol is mediated by the Cag T4SS. This is a contact-dependent secretion system that forms a large complex spanning the inner and outer membrane, containing a pilus and several ATPases that promote T4SS assembly, pilus formation and/or CagA translocation55. The H. pylori cag PAI encodes homologues or paralogues of the prototypical Agrobacterium tumefaciens Vir T4SS56, including the putative VirB7 (CagT), B9 (CagX) and B10 (CagY) inner and outer membrane spanning channel subunits57, the major (VirB2, CagC) and minor (VirB5, CagL) pilus subunits and several additional H. pylori specific cag proteins that are required for CagA translocation (for example, CagH and CagI)58, 59. Many Cag T4SS components have distinct domain structures from their Vir counterparts. For example, the VirB10 homologue, CagY, is considerably larger (~220 kDa) and contains additional domains composed of repeat regions27. Additionally, the three core cell envelope spanning channel subunit homologues, CagY, CagT and CagX, have been suggested to localize to the pilus surface or to the base of the pilus using transmission electron microscopy (TEM)60, 61. A later study localized CagL and CagA to the tip of the pilus62. CagL was suggested to act as a tip adhesin which binds to α5β1 integrin (the host cell receptor for CagL) through an RGD motif and neighbouring sequences (see insert Figure 1)62, 63. CagL binding and α5β1 integrin signalling were found to be required for both pilus extension and CagA translocation. Soluble RGD peptide could partially rescue the CagA translocation defect of a cagLRGA mutant, but not a ΔcagL deletion strain suggesting a two-step model, where surface exposed CagL binds and activates α5β1 integrin, partially activating focal adhesion kinase (Fak) and Src kinase, promoting pilus extension. In a second step, pilus associated CagL further stimulates α5β1 integrin, in addition to stimulating the activities of Fak and Src, thereby inducing CagA translocation and ensuring its rapid tyrosine phosphorylation by Src.
The relationship between pilus formation and CagA secretion was further explored by field emission scanning EM (FESEM), which readily detects Cag T4SS dependent pili64. This technique confirmed the requirement of CagL for pilus formation and also revealed a hyperpiliated phenotype for cagH mutants which, like cagL mutants, fail to translocate CagA64. A ΔcagY mutant produces pili28, which is surprising because CagL was found to be unstable in a ΔcagY mutant in another study59. At present, the mechanism by which CagL (or CagA, T, X and Y) becomes surface exposed or incorporated into pili has not been explored. Collectively these data suggest that pilus formation is not sufficient for CagA translocation, that pilus formation can proceed in the absence of at least one core T4SS component, and that there may be CagL-independent mechanisms of integrin activation, of pilus assembly and CagA translocation in some strains. In fact, CagA, CagI and CagY were shown to bind α5β1 integrin in vitro and using yeast two hybrid studies65. CagA, in particular, shows much higher integrin binding affinity in vitro than CagL; CagA binding is not inhibited by the Yersinia entercolitica RGD-containing invasin whereas CagL binding is inhibited, which would indicate that CagA and CagL use different integrin interaction surfaces. Antibodies that prevent integrin switching between a bent and open configuration block CagA translocation65 and the α5β1 integrin interaction domain of CagA was shown to inhibit CagA translocation when provided as a soluble peptide66 indicating a complex series of molecular interactions are required for integrin activation and CagA secretion. Further insights into the precise nature of the interactions between CagA, CagL and host interaction partners are beggining to be revealed by structural and molecular evolution studies (see text box 1). .
CagL effector functions
While the CagA translocation defect of cagL mutants suggested that CagL has a structural role as part of the T4SS, a number of studies suggest additional functions67-70. Studies with purified recombinant CagL revealed that the protein can induce cell spreading and focal adhesion formation in a similar manner to the host extracellular matrix RGD-containing protein fibronectin69. CagL activates epidermal growth factor receptor (EGFR) more efficiently than fibronectin, and this was shown to result from RGD-dependent displacement of ADAM17 (a disintegrin and metalloprotease) from α5β1 integrin, activating ADAM17 protease activity68. ADAM17 cleaves and releases surface bound heparin-binding EGF-like growth factor. The resulting activation of EGFR in gastric epithelial cells represses H,K-ATPase activity (and thus diminshes acid secretion) via a repressive NF-κB binding site in the H,K-ATPase promoter. CagL can also bind αvβ5 integrin independently of its RGD motif, which mediates the induction of gastrin70. Gastrin is a potent inducer of acid secretion, thus, simultaneous activation of gastrin and repression of the H,K-ATPase could explain the observed hypergastrinaemia and hypochlorhydria during chronic H. pylori infection. Finally, CagL RGD-dependent activation of α5β1 integrin activates the pro-inflammatory cytokine interleukin-8 (IL-8) independently of CagA translocation and Nod1 signalling67, indicating that CagL induces inflammation. Increased risk cancer and ulcer which is associated with the carriage of the Cag PAI, has largely been attributed to CagA but these studies indicate that CagL may be an equally important effector. Furthermore, studies on the evolution of the Cag PAI suggest that additional Cag proteins may directly interact with host proteins via exposure on the cell surface or as novel effectors (see text box 1).
Evasion of innate immune recognition
In addition to the multiple virulence factors that H. pylori uses to manipulate the host and ensure its persistence, the pathogen has evolved elaborate strategies to evade and subvert host immune defences, which are key to the success of this pathogen. The first defence barrier against H. pylori is formed by mucus-producing epithelial cells lining the gastric mucosa and by innate immune cells that either reside in the gastric lamina propria under steady state conditions or are recruited there during infection. The detection of conserved pathogen-derived molecular structures (pathogen-associated molecular patterns, PAMPs) by epithelial cells and innate immune cells occurs via four distinct classes of innate immune receptors (so-called pattern recognition receptors, PRRs) that differ in their subcellular localization, coupling to downstream signalling pathways and specificity. H. pylori has evolved to avoid detection by several types of PRRs that are crucial for the recognition of other Gram-negative enteropathogens.
Evasion and manipulation of TLR and RLR recognition
The best-defined among the four classes of PRRs are the Toll-like receptors (TLRs). TLRs are either surface-exposed on the plasma membrane or localize to endosomes and bind diverse classes of microbially derived PAMPs. Among these are the ligands for TLR4 (LPS), TLR2 (lipoteichoic acid and lipoproteins), TLR3 (dsRNA and polyinosinic:polycytidylic acid), TLR5 (flagellin) and TLR9 (unmethylated CpG). H. pylori largely avoids recognition by TLRs, with evasion of TLR4 detection of LPS being the best understood example. H. pylori LPS is predominantly tetra-acylated and is 1000-fold less bioactive than the hexa-acylated LPS of E. coli 71. Furthermore, the relative inactivity of H. pylori LPS was recently shown to result from the removal of phosphate groups from the 1'- and 4'- positions of the lipid A backbone, which generates LPS that exhibits less negative charge, resists binding by antimicrobial peptides such as polymyxin B and escapes detection by TLRs72. The phosphatases responsible for lipid A modification in H. pylori have been identified and the respective gene deletion mutants indeed fail to colonize experimentally infected mice72. The TLR(s) involved in the residual detection of H. pylori LPS remain a matter of debate; whereas several studies utilizing purified LPS have implicated the classical LPS sensor TLR473, 74, others suggest that TLR2 is the main sensor of H. pylori LPS75, 76 (Figure 2). A clear interpretation of the published studies is complicated by the fact that they rely on models in which the respective TLR is ectopically expressed, often in the absence of its co-receptor, and the fact that both TLR4 and TLR2 participate in the detection of other, non-LPS-related PAMPs of H. pylori77, 78, which may contaminate LPS preparations.
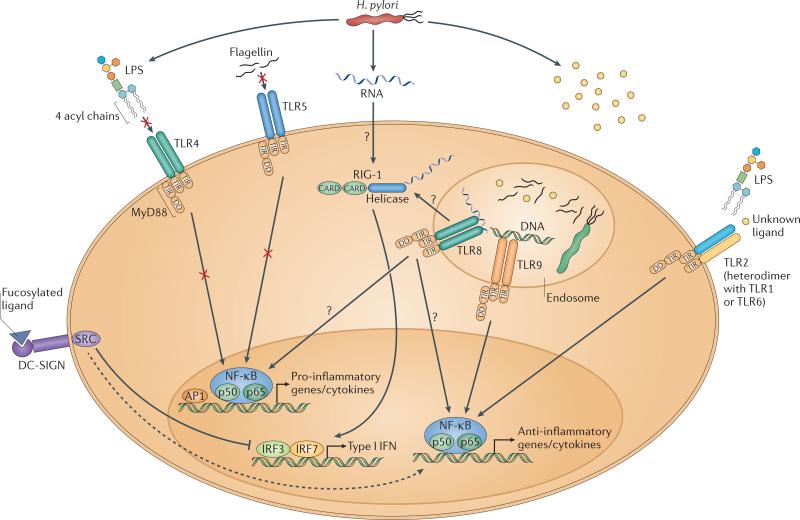
Figure 2. H. pylori subversion of innate immune recognition.
H. pylori harbors PAMPs that have evolved to evade detection by pro-inflammatory TLRs. H. pylori expresses tetra-acylated LPS, which is less bioactive than the hexa-acylated form typical of other Gram-negative pathogens due to specific lipid A modifications that prevent detection by TLR4. H. pylori flagella are not detected by TLR5 due to mutations in the TLR5 binding site of flagellin. The bacterium's DNA, as well as an as yet uncharacterized PAMP (and possibly H. pylori LPS) are detected by TLRs 9 and 2, respectively; these TLRS predominantly activate anti-inflammatory signalling pathways and anti-inflammatory IL-10 expression. 5‘ triphosphorylated RNA is detected by the RLR RIG-I, which activates the transcription factors IRF3 and IRF7 to induce type I IFN expression, and is potentially detected also by TLR8 in endosomes. H. pylori's fucosylated DC-SIGN ligands suppress activation of the signalling pathways downstream of this CLR and activate anti-inflammatory genes. Please note that not all depicted TLRs, RLRs and CLRs are necessarily expressed by the same cell type; only one generic cell type is shown here for simplicity. DD, death domain; TIR, Toll/Interleukin-1 receptor domain; CARD, caspase activation and recruitment domain; MyD88, myeloid differentiation primary response gene 88; DC-SIGN, dendritic cell-specific intercellular adhesion molecule-3 grabbing non-integrin; SRC, steroid receptor coactivator.
Another putative H. pylori PAMP, flagellin, escapes recognition by TLR5 due to modifications in the N-terminal TLR5 recognition domain79 (Figure 2). Mutating residues 89-96 of Salmonella flagellin to the corresponding flaA sequence of H. pylori abolishes its recognition by TLR580. Experiments using dendritic cells (DCs) lacking TLRs 2, 4, 7 and 9, or combinations thereof, revealed that the innate immune system recognizes H. pylori nucleic acids77. Intracellular delivery of H. pylori DNA to DCs by lipofection efficiently activates endosomally localized TLR977, however the net effect of this activation is anti- rather than pro-inflammatory81-83 (Figure 2). TLR9 signalling has anti-inflammatory consequences in the early stages of infection in a mouse model81 and H. pylori DNA can even be used therapeutically to treat experimentally induced inflammatory bowel disease in mice82, 83. The bioactivity of H. pylori DNA may account for the inverse correlation between H. pylori colonization and the risk of developing inflammatory bowel diseases84, which has been attributed to a specific “immuno-regulatory“ sequence (TTTAGGG) that appears to be unique to the H. pylori genome82, 83. H. pylori RNA sensing by DCs has been suggested to be mediated by endosomally localized TLR877, as well as a cytoplasmic nucleic acid sensor belonging to the RIG-like helicase receptor family (RLRs), RIG-I. RIG-I appears to be required for the detection of 5‘ triphosphorylated H. pylori RNA and the ensuing IRF3/7-dependent induction of type I interferons (IFNs) by DCs77 (Figure 2). Whether the activation of RIG-I and the H. pylori-induced production of type I IFNs has predominantly pro- or anti-inflammatory effects remains to be determined.
The detection of H. pylori non-LPS ligands by TLR2 represents another example of how H. pylori exploits the immune system for the induction of anti-inflammatory responses. Activation of TLR2 triggers the MyD88-dependent expression of a number of anti-inflammatory genes, most notably interleukin-1077 (Figure 2). Furthermore, TLR2−/− mice infected with Helicobacter felis, a close relative of H. pylori, control experimental infections better than wild type mice and develop stronger T-cell responses and T-cell-driven immunopathology78. The effects of TLR2 gene deletion are phenocopied by MyD88−/− mice, indicating that the absence of anti-inflammatory signals induced by Helicobacter is phenotypically dominant over the simultaneous lack of MyD88-dependent pro-inflammatory signals induced by other TLRs78.
Suppression of CLR-mediated signalling
In addition to its TLR and RLR ligands, H. pylori also harbors ligands for a third class of PRRs, the C-type lectin receptors (CLRs). The best characterized of these are fucosylated ligands that bind to the CLR family member DC-SIGN85. In contrast to pathogens such as M. tuberculosis and HIV, which express mannosylated DC-SIGN ligands and activate pro-inflammatory downstream signalling pathways, the fucose residues of H. pylori's DC-SIGN ligands actively dissociate the signalling complex downstream of DC-SIGN (consisting of the scaffold proteins LSP1, KSR1 and CNK and the kinase Raf-1) and suppress pro-inflammatory signalling85 (Figure 2). The differential biological effects of mannosylated and fucosylated DC-SIGN ligands are in line with the proposed role of this PRR in tailoring and fine-tuning adaptive immunity to specific pathogens via the DC-SIGN/Raf-1-mediated acetylation of TLR-activated nuclear NF-κB86. Acetylation of the NF-κB subunit p65both prolongs and increases IL-10 transcription to enhance anti-inflammatory cytokine responses86.
In summary, most of the available data support the conclusion that H. pylori avoids the induction of a strong pro-inflammatory response, as well as subsequent adaptive immunity and clearance, through two main mechanisms: the evasion of innate immune detection by pro-inflammatory TLRs and the preferential activation and manipulation of anti-inflammatory TLRs and CLRs. Together, these strategies promote persistence of the organism.
Activation of NLRs and the inflammasome
The heterogeneous cytoplasmic family of Nod-like receptors (NLRs) comprise the fourth and final family of PRRs. NLRs detect a wide range of PAMPs and are also essential for sensing host-derived, damage-associated molecular patterns (DAMPs) that are released upon perturbations of tissue homeostasis87. Broadly speaking, NLRs fall into two categories: Nod1 and Nod2 recognize peptidoglycan metabolites and activate the transcription factor NF-κB to induce innate and adaptive immune response genes88, while most other NLRs promote the assembly of multiprotein complexes called inflammasomes, which activate the cysteine protease caspase-189.
Detection of H. pylori peptidoglycan by Nod1
Nod1-mediated detection of H. pylori peptidoglycan was one of the first PRR-mediated innate immune pathways found to become activated upon H. pylori infection90. Although initial work indicated that only T4SS-proficient H. pylori strains (harboring a functional Cag T4SS) could deliver peptidoglycan and its active metabolite (meso-diaminopimelate-containing N-acetylglucosamine-N-acetylmuramic acid) into the cytoplasm of host epithelial cells90, it is now clear that outer membrane vesicles (OMVs) from Cag PAI-negative strains of H. pylori can also target peptidoglycan to Nod191 (Figure 3). Intragastric delivery of OMVs in mice induces innate and adaptive immune responses through a NOD1-dependent but TLR-independent mechanism91. The delivery of peptidoglycan by both OMVs and the T4SS occurs at cholesterol-rich lipid rafts91, 92 (Figure 3). In addition to the initially reported Nod1 signalling pathway resulting in NF-κB translocation to the nucleus90, Nod1 also activates the transcription factor AP-1 via the ERK and p38-dependent pathways93. A direct consequence of Nod1 signalling is efficient killing of H. pylori by beta-defensin 2, an antimicrobial peptide produced by Nod1-activated gastric epithelial cells94. The idea that H. pylori-induced activation of NF-κB depends on Nod1 has recently been challenged by a report showing that introduction of an siRNA specific for Nod1 does not alter the nuclear translocation of the NF-κB subunit p6595. This study rather provides evidence for an alternative Nod1-dependent signalling pathway, which activates the IRF3/7 transcription factor to induce the production of type I IFNs that are required for H. pylori-specific cytokine and chemokine responses and infection control95 (Figure 3).
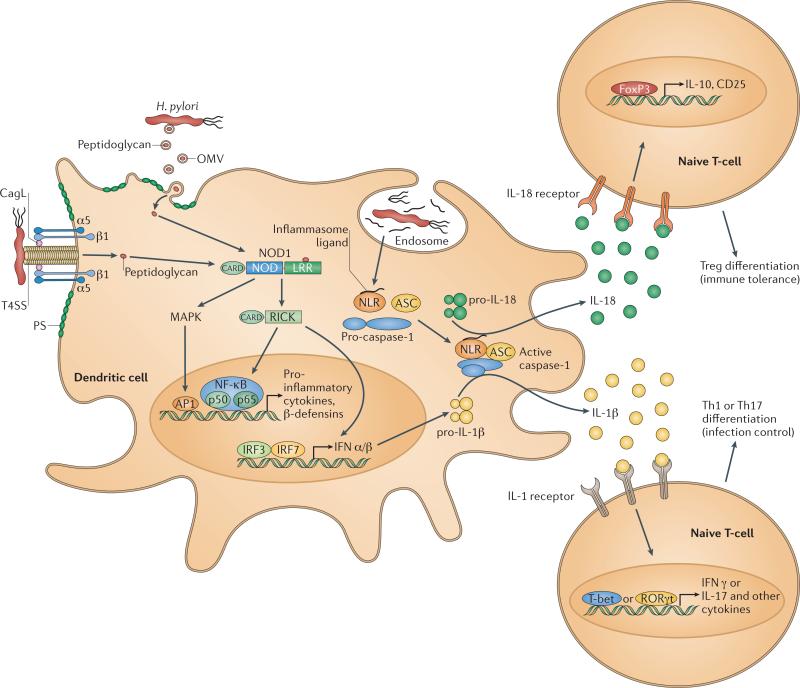
Figure 3. H. pylori activation of NLRs, NF-κB signalling and caspase-1.
H. pylori peptidoglycan is delivered to the cytoplasmic NLR Nod1 through either the type IV secretion system (T4SS; via its interaction with α5β1 integrin at cholesterol-rich lipid rafts) or via outer membrane vesicles. Activated Nod1 induces the AP1/NF-κB-dependent expression of pro-inflammatory cytokines and defensins, and the IRF3/7-dependent expression of type I IFNs. Additional unidentified H. pylori NLR ligands activate the inflammasome to induce autoproteolytic pro-caspase-1 cleavage and the subsequent processing and release of mature IL-1β and IL-18. IL-18 binds to its receptor on naive T-cells and promotes FoxP3-dependent Treg differentiation and immune tolerance, which in turn prevents clearance and ensures persistent colonization of H. pylori. In contrast,IL-1β binding to its receptor induces T-bet- and RORγT-dependent Th1 and Th17 differentiation and the expression of the respective signature cytokines IFN-γ and IL-17. Please note that the pictured innate immune cell is a dendritic cell, whereas peptidoglycan-induced Nod1 signalling has been demonstrated in gastric epithelial cells. OMVs, outer membrane vesicles; ASC, apoptosis-associated speck-like protein containing a carboxy-terminal CARD domain; NOD, nucleotide-binding oligomerization domain; LRR, leucine-rich repeat domain; RICK, receptor-interacting serine/threonine kinase; MAPK, MAP kinase.
Inflammasome activation by H. pylori
H. pylori harbors one or more ligands that trigger activation of the inflammasome and of caspase-1, a cysteine protease that controls the processing and secretion of two cytokine precursors, pro-IL-1β and pro-IL-1887. Like other caspases, caspase-1 is synthesized as an inactive precursor, which becomes auto-proteolytically activated only upon inflammasome assembly. Inflammasome assembly in turn is regulated by ligand binding and subsequent hetero-oligomerization of inflammasome sensors in conjunction with an adaptor molecule (apoptosis-associated speck-like protein containing a CARD, ASC) and pro-caspase-187, 89. Whereas the inflammasome ligands and NLR sensors involved in H. pylori detection remain obscure, in vitro and in vivo studies have demonstrated that caspase-1 becomes activated in DCs upon co-culture with H. pylori and that IL-18 and IL1-β are processed and released into the infected gastric mucosa96, 97 (Figure 3).
There is no evidence to suggest that H. pylori actively avoids inflammasome or caspase-1 activation. In fact, mice lacking caspase-1 due to targeted deletion of the corresponding gene clear an experimental infection with Helicobacter felis or H. pylori more efficiently than wild-type animals, and exhibit more pronounced pathogen-specific T-cell responses and T-cell-driven immunopathology96. The explanation for this unexpected observation was provided by mouse strains lacking either IL-18 or its receptor, IL-18R: these mice phenocopy the effects of caspase-1 gene deletion, i.e. they clear the infection better than wild-type mice due to enhanced T-cell responses, and as a consequence, develop more severe immunopathology.96, 98 Further analysis revealed that IL-18 is crucial for inducing regulatory T-cell (Treg) responses to H. pylori (Figure 3), which in turn restrict excessive effector T-cell activation and promote persistence98. Interestingly, IL-1β (the other caspase-1 cytokine substrate) apparently opposes IL-18 function. IL-1R−/− animals lacking the receptor for IL-1β fail to launch H. pylori-specific Th1 and Th17 responses, and cannot control an experimental infection (even when vaccinated against H. pylori before challenge) and, as a consequence, are protected against even the mildest forms of infection-associated immunopathology96. These data corroborate an earlier report showing that stomach-specific expression of human IL-1β is sufficient to induce gastric inflammation and gastric cancer in transgenic mice99, and also explain why promoter polymorphisms associated with increased steady-state levels of IL-1β predispose carriers to a high gastric cancer risk100. Furthermore, the effects of IL-1R gene deletion appear to be phenocopied by H. pylori-infected mice lacking the inflammasome adaptor ASC101. In conclusion, detection of H. pylori via NLRs and subsequent activation of the inflammasome and downstream signalling pathways is crucial for efficient infection control (in the case of Nod1 signalling and inflammasome-mediated IL-1β secretion) and at the same time ensures the restriction of excessive T-cell responses and immunopathological tissue damage (via inflammasome-mediated IL-18 secretion).
Modulation of T-effector cell responses
Suppression of Th1- and Th17-mediated immunity
Experimental infection studies have shed light on the elements of the innate and adaptive immune system required for control of H. pylori infections, and in particular for the generation of vaccine-induced protective immunity17, 102-107. Whereas B-cells and antibodies are dispensible for H. pylori control103, 104, 107 (at least for the sub-optimal, non-sterilizing reduction in colonization by 1-2 orders of magnitude that is considered the gold standard in the H. pylori vaccinology field, see text box 2), it is now clear that CD4+ effector T-cells (not to be confused with the CD4+ Tregs mentioned above), and in particular Th1 and Th17-polarized T-effector cell subsets and their signature cytokines, are critical for proper control of this infection17, 102, 106. The same T-cell subtypes have been implicated in promoting the immunopathological changes of the chronically infected gastric mucosa that manifest histologically as atrophic gastritis, compensatory epithelial hyperplasia and intestinal metaplasia in experimentally infected animals and symptomatic human carriers108, 109.
Two virulence factors have been specifically implicated in the manipulation and inhibition of human T-cells (Figure 4). VacA inhibits T-cell proliferation by interfering with the T-cell receptor/interleukin-2 signalling pathway at the level of the Ca2+/calmodulin-dependent phosphatase calcineurin110, 111. VacA prevents nuclear translocation of the T-cell transcription factor NF-AT and its subsequent transactivation of T-cell-specific immune response genes110, 111 (Figure 4). Follow up studies have since identified β2 integrin (CD18) as the receptor for VacA on human T-cells112; β2 integrin associates with CD11a on T-cells to form the heterodimeric transmembrane receptor LFA-1 (lymphocyte function-associated antigen-1). H. pylori exploits the recycling of LFA-1 to facilitate VacA uptake112 in a manner that depends on protein kinase C-mediated serine/threonine phosphorylation of the β2 integrin cytoplasmic tail113. The other H. pylori virulence determinant implicated in T-cell inhibition is γ-glutamyl-transpeptidase GGT114, 115. Similar to VacA, GGT is a secreted factor that blocks proliferation of T-cells through a mechanism that involves the inhibition of cyclin-dependent kinase activity in the G1 phase of the cell cycle by the disruption of the Ras signalling pathway114, 115 (Figure 4).
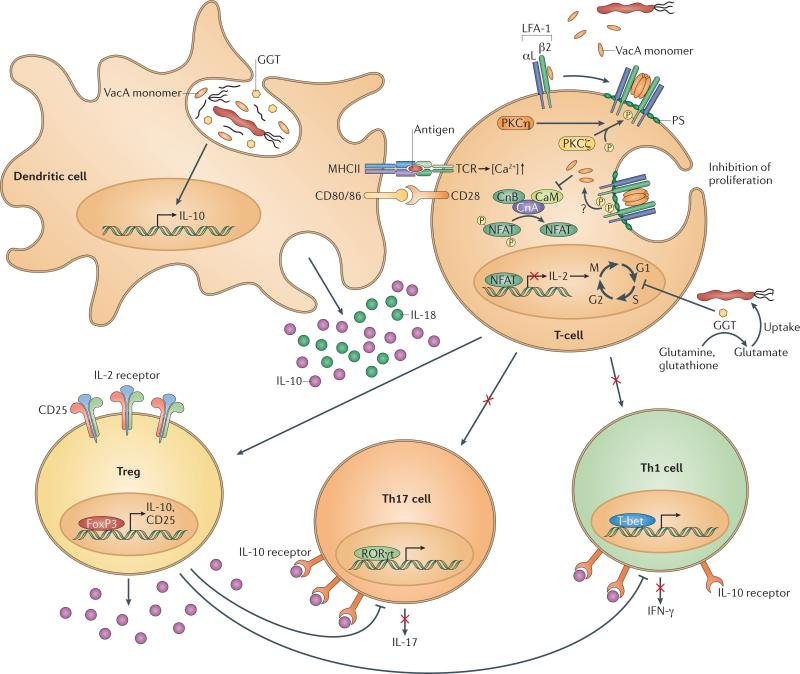
Figure 4. H. pylori impairs T-cell-mediated immunity via direct and indirect mechanisms.
All strains of H. pylori express the secreted virulence factors VacA and GGT to directly inhibit T-cell activation, proliferation and effector functions. Hexameric VacA binds to the β2 integrin subunit of the heterodimeric transmembrane receptor LFA-1; the receptor complex is internalized upon protein kinase C-mediated serine/threonine phosphorylation of the β2 integrin cytoplasmic tail. Cytoplasmic VacA prevents nuclear translocation of NF-AT by inhibiting its dephosphorylation by the Ca2+/calmodulin-dependent phosphatase calcineurin, and thereby blocks IL-2 production and subsequent T-cell activation and proliferation. GGT arrests T-cells in the G1 phase of the cell cycle and thus prevents their proliferation. Both VacA and GGT also indirectly prevent T-cell immunity via re-programming of DCs; VacA/GGT-exposed DCs produce IL-10, and induce the FoxP3- and contact-dependent differentiation of T-cells into regulatory T-cells while at the same time preventing Th1 and Th17 differentiation. Depicted interactions at the T-cell/DC synapse include MHCII binding to the T-cell receptor and binding of costimulatory molecules CD80/CD86 to CD28. DC-derived and/or Treg-derived IL-10 further suppresses Th1 and Th17 effector functions. Note that the direct effects of VacA on T-cells appear to be human-specific, whereas indirect effects of VacA and GGT on T-cells via DCs have only been documented in the murine system. LFA-1, lymphocyte function-associated antigen-1; NF-AT- nuclear factor of activated T-cells; GGT, γ-glutamyl-transpeptidase; CnA,B, calcineurin A and B subunits; CaM, calmodulin; RORγT, retinoid-related orphan receptor γT; T-bet, T-box transcription factor.
Skewing of T-cell responses
Both VacA and GGT also affect T-cell activity in an indirect manner, by promoting the preferential differentiation of naive T-cells into Tregs116. Treg differentiation in response to H. pylori infection requires the direct interaction of naive T-cellswith ‘tolerogenic‘ DCs that have been exposed to H. pylori, either in the gastric mucosa or in the stomach-draining (gastric or mesenteric) lymph nodes98, 117, 118H. pylori-exposed DCs fail to induce effector T-cell responses of the Th1 and Th17 type in vitro and in vivo; instead, such DCs preferentially induce the expression of the Treg-specific transcription factor FoxP3, the surface marker CD25 and the anti-inflammatory cytokine IL-10 in naive T-cells 98, 107, 117 (Figure 4). Such peripherally induced Tregs affect the control of H. pylori profoundly, as shown in chronically infected patients119-123 and by animal experiments in which Tregs were systemically depleted in infected hosts52, 107. Tregs accumulate in the H. pylori-infected human gastric mucosa119, 121, especially in children123 and in asymptomatic carriers122, and effectively suppress H. pylori-specific memory T-cell responses120.
Experimental depletion of Tregs facilitates clearance of H. pylori in infected animals52 and enhances vaccine-induced protective immunity in vaccinated mice107. The Treg-facilitated persistence of H. pylori requires T-cell-specific expression of IL-10; in fact, IL-10−/− mice and a strain lacking IL-10 expression in the CD4+ T-cell compartment are capable of spontaneously controlling experimental infections52, 78, 124. The efficient control or even clearance of H. pylori in animals invariably comes at the price of enhanced gastric immunopathology (gastritis and epithelial changes such as atrophy and intestinal metaplasia). Interestingly, an analogous observation has been reported for human carriers, which either accumulate large numbers of IL-10-producing, H. pylori-specific Tregs and are colonized heavily (asymptomatic carriers), or develop gastric ulcers because their Treg response is inadequate122. The H. pylori-specific ‘tolerization‘ of DCs, which appears to be a prerequisite for the skewing of T-cell responses (at least in experimental models98, 117), requires the activity of both VacA and GGT 116 (Figure 4). While the exact mechanism of VacA- and GGT-specific DC tolerization remains to be elucidated, the newly assigned function of both factors in Treg induction and persistence is consistent with previous reports showing that gene deletion mutants lacking VacA or GGT have colonization defects relative to their parental, VacA/GGT-proficient wild-type isolates125, 126.
Systemic consequences of immunosuppression
The active inhibition and manipulation of adaptive, T-cell-driven immune responses by H. pylori has a variety of consequences for the host. The persistence mechanisms of H. pylori are dominant enough to override the protective effects conferred by H. pylori-specific vaccination; a challenge infection can only be cleared (or at least strongly reduced) by vaccinated mice if Tregs or DCs are depleted107. These observations may partly explain the difficulties and obstacles faced in H. pylori vaccine development (see text box 2). An interesting side effect of H. pylori-specific immunomodulation and manipulation is evident in Western societes from which H. pylori is gradually disappearing due to reduced transmission rates, the frequent use of antibiotics in childhood and generally improved sanitation conditions127. In these populations, the incidence of allergic asthma, other allergic disease manifestations and chronic inflammatory diseases is steadily increasing and an inverse association with H. pylori colonization has been documented for allergic asthma128-132 and inflammatory bowel diseases84 (see text box 3). While the exact mechanisms underlying this inverse association remain to be elucidated, the idea that H. pylori-induced immune regulation and manipulation are causally linked to protection from such immune disorders is compelling (see text box 3). The fact that Tregs isolated from H. pylori-infected mice are sufficient to protect naive recipients against allergen-induced asthma in adoptive transfer models argues in favor of Treg-mediated cross-protection against allergen-specific immune responses98, 133. Further work in this area is urgently needed to shed more light on the intricate interactions of this extraordinarily well-adapted, persistent pathogen with the host adaptive immune system.
Conclusions and future perspectives
The work summarized in this Review outlines how H. pylori uses a combination of virulence factors and immune subversion and manipulation mechanisms to colonize and persist in the challenging environment of the gastric mucosa. Experimental work in recent years has elucidated exciting details on the structure and function of the type IV secretion system, the pleiotropic effects of CagA delivery, the CagA-independent effects of the secretion system and the newly discovered function of the extracellular effector CagL. The role of cell shape and chemotaxis in persistent colonization is now well documented with respect to the genes involved. Progress in other areas, in particular H. pylori-specific vaccine development, has suffered from setbacks in phase I clinical trials and the lack of continuous industry support. The necessity of overriding the bacteria's persistence strategies has been identified as a major challenge in H. pylori-specific vaccine development. More and more interest in the field has shifted to gaining a better understanding of the benefits, suggested from epidemiological studies, that the infection may bestow on the large majority of asymptomatic carriers, and experimental evidence has been forthcoming to support such claims. In particular, it is now becoming increasingly clear that the virulence factors deployed by H. pylori and the mechanisms that are exploited to override T-cell-driven immunity and to ensure persistent infection have systemic immunomodulatory effects that likely explain the benefits of the infection to asymptomatic carriers. The molecular mechanisms allowing H. pylori to suppress T-cell activation via production of VacA and GGT, and to skew T-cell responses towards regulatory T-cells, are increasingly well understood.
Other aspects of the Helicobacter-host interaction have received surprisingly little, if any, attention; these include the specifics of inflammasome activation by H. pylori and of innate immune activation by H. pylori in general, the molecular basis of its host species specificity, and the relative (or perhaps additive) contributions of its direct and indirect (inflammation-mediated) carcinogenic properties to gastric cancer development. Another important aspect of H. pylori biology that has been largely ignored relates to its transmission. While several independent, mostly older, studies indicate that mothers serve as the predominant source of their children's H. pylori infection, the transmission route remains unclear. Also, very little is currently known about the vast differences in gastric cancer risk of (often closely related, and physically close) human populations, which is likely to be influenced by human genetic predisposition, population ecology and behaviour. In summary, many of the peculiarities that set H. pylori apart from other Gram-negative enteropathogens remain underexplored and deserve further work.
Text box 1: Structural and evolutionary insights on Cag proteins.
A combination of NMR, X-ray crystallographic, biochemical and localization studies have revealed that CagA, which can form a dimer, has a novel elongated structure that directly facilitates its interactions with α5β1 integrin, phosphatidyl serine (PS) in the cell membrane and the Par1 kinase, as well as inter- and intramolecular interactions with itself134 (see insert of Figure 1). The ordered N-terminal 70% of the protein contains three domains. In addition to the integrin interacting sub-domain (D2’), Domain II contains a basic patch that includes a previously defined PS interaction surface135, which causes external accumulation of PS at sites of bacterial attachment and is necessary for CagA translocation. After translocation, this same patch is required for CagA membrane tethering in polarized cells (as shown by transfection studies) and Par1-mediated disruption of polarity135. Domain III can form an intramoecular interaction with the intrinsically disordered C-terminal 30% of the protein that includes the Src Homology 2-binding EPIYA motifs and the Par1 interacting Cag multimerization (CM) motif. Interestingly, this intramolecular interaction appears to restrain this domain in a lariat structure that apparently stabilizes interactions with Par1 through reduced turnover, enhancing CagA-dependent induction of cell motility134. Mutational studies are beginning to define the specific molecular interactions predicted from these structural studies.
Additional insights into the precise residues that may be important for interactions between CagA and other potential effectors and their host targets comes from molecular evolution and disease association studies. Evaluation of the functional consequences of transient and fixed mutations indicates continuous selection for maintenance of Cag PAI function in spite of frequent loss or inactivation in many H. pylori strain populations, suggesting a mixture of positive and negative selection pressures on this virulence determinant136. European origin of strains correlates with increased risk of gastric cancer, higher inflammation and accumulation of host DNA damage found in the mountain region (high risk) compared to coastal region (low risk) in Columbia137. One study found an association between two linked nonsynonymous SNPs near the RGD motif of CagL and gastric cancer, and higher α5β1 integrin expression in the corpus region of the stomach in a Taiwanese population138. Another study found an association between two synonymous SNPs in the CagE ATPase and gastric cancer in a population from Venezuela and Columbia139. Analysis of positive selection, which indicates an accumulation of diversifying mutations, revealed strong signals for the known effector proteins CagA and CagL, the surface exposed protein CagY and an uncharacterized protein CagQ136. This elevated rate of diversification could result from immune pressure or interaction with host proteins that are polymorphic in different hosts. Further analyses of these variants in view of the recent stuctural data combined with functional studies and replicate associations in other populations will further expand our understanding of H. pylori pathogenesis and strain dependent disease risk.
Text box 2: Progress and obstacles in H. pylori-specific vaccine development.
Efforts to develop a H. pylori-specific vaccine began in the early 1990's with the recognition that infection with this bacterium is the most important cause of peptic ulcer disease and a strong risk factor for gastric cancer. Prophylactic immunization, especially during infancy or early childhood, was projected as recently as 2009 to be cost-effective in the U.S. (with respect to dollars spent per quality-adjusted life years140), despite the documented gradual loss of H. pylori from Western populations127. However, the results of H. pylori vaccine development efforts, both preclinical and early clinical, have been disappointing to date. Sterilizing immunity is rarely achieved, even in animal models, and there is no consensus on the delivery route, adjuvants and choice of antigens. The most promising preclinical results have generally been obtained with vaccination strategies aimed at inducing protective T-cell-mediated rather than humoral immunity, with local gastric Th1 and Th17 responses representing reasonably good correlates of, and prerequisites for, protection (reviewed recently in 141).
H. pylori antigens ectopically expressed in Salmonella enterica vaccine strains, whole cell H. pylori extracts, and multi-component, parenterally or mucosally delivered recombinant vaccines have all been used successfully in mice (for recent comprehensive review articles see141, 142). H. pylori antigens with documented immunogenicity in rodents include the urease enzyme, CagA, VacA, catalase, neutrophil-activating protein (NAP) and heat shock proteins; these can be delivered by various mucosal routes such as orogastric, intranasal, sublingual and rectal141, 142. Despite the strict limitation of H. pylori to its gastric niche, systemic immunization via the intraperitoneal or subcutaneous routes can be as effective as mucosal vaccination141, 142. In contrast to most other vaccines, H. pylori-specific immunization generates prophylactic as well as therapeutic immunity in rodent models. Persistence mechanisms employed by H. pylori to overcome and subvert adaptive immunity have been identified as crucial obstacles precluding sterilizing immunity107; vaccination strategies may therefore need to be designed to bypass or override the host immunoregulatory response.
Two recently conducted phase I clinical trials in human volunteers showed antigen-specific humoral and cellular responses143, 144, but did not confer satisfactory protection against challenge infection143. In one trial, intramuscular immunization with three recombinant antigens (CagA, VacA and neutrophil-activating protein- NAP) adjuvanted with alum induced responses to some or all antigens in the majority of volunteers irrespective of the exact doses and immunization schedules; T-cell responses were observed only against CagA and VacA, but were detectable as late as 24 months post primary vaccination and thus indicative of T-cell memory144. Oral immunization with live Salmonella enterica serovar Typhi Ty21a expressing H. pylori urease or HP0231 provided evidence that the clearance or reduction of a challenge infection requires T-cell mediated immunity, yet the study failed to demonstrate improved infection control in the vaccinated group relative to the non-immunized (but challenged) volunteers143. In conclusion, whereas rodent models of H. pylori-specific vaccination have revealed useful antigens, adjuvants and delivery routes, the ultimate proof of immunogenicity and protective immunity in humans remains elusive. The continued support from private sector initiatives is widely viewed as being essential to promoting H. pylori vaccine development also in the future142.
Text box 3 H. pylori-mediated protection against allergic and chronic inflammatory disorders.
H. pylori is an ancient member of the human indigenous microbiota145, but began to disappear from individuals in developed countries in the twentieth century127. This has led to diminishing rates of peptic ulcer disease and gastric cancer146. Coincident with the decline in H. pylori colonization rates, especially during the second half of the last century, the incidence of allergic asthma and other allergic disease manifestations has reached epidemic proportions in large parts of the developed world. Cross-sectional studies have documented that the two phenomena are inversely correlated, with H. pylori carriers exhibiting a decreased risk of developing childhood- or early-onset allergic asthma, rhinitis and atopic dermatitis than the non-infected population129, 130, 131, 147. A large meta-analysis documented a similar inverse relationship between H. pylori status and the risk of developing either of two inflammatory bowel diseases, Crohn's disease and ulcerative colitis84.
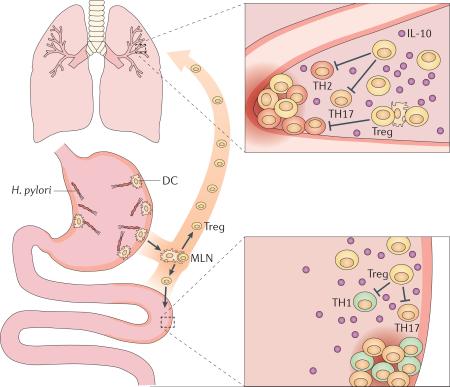
A limited amount of experimental evidence from animal studies is now available to support both of these observations (summarized in the figure). In a model of acute Salmonella typhimurium-induced intestinal inflammation, experimental co-infection with H. pylori suppresses Salmonella-specific Th17 responses as well as cecal Salmonella-induced inflammation, likely via increased production of IL-10148. Similarly, the administration of a single dose of H. pylori DNA reduced sodium dextran sulfate (DSS)-induced colitis, in both acute and chronic experimental settings83. With respect to asthma, murine infection with H. pylori efficiently prevents ovalbumin- or house dust mite-induced allergic airway inflammation133. Infected mice are protected against airway hyper-responsiveness (measured after methacholine exposure), as well as tissue inflammation and goblet cell metaplasia, and exhibit reduced pulmonary and bronchoalveolar infiltration of eosinophils, Th2 cells and Th17 cells133. Asthma protection could be attributed to H. pylori-induced, highly suppressive Tregs, which accumulate in the lungs of infected mice and block allergen-specific effector T-cell responses (see figure). In line with thisobservation, the adoptive transfer of mesenteric lymph node (MLN)-derived CD25+ Tregs from infected donors is sufficient to protect naive recipients against asthma133. The induction of H. pylori-specific Tregs with suppressive properties in turn involves tolerogenic DCs98, which presumably encounter H. pylori or its tolerizing persistence determinants in the gastric mucosa and then home to the MLNs for T-effector and Treg-cell priming. The suppression of both asthma and colitis is believed to require (DC and/or Treg-derived) IL-10 (see the figure).
Figure for text box 3. H. pylori exerts systemic immunomodulatory effects.
H. pylori exclusively inhabits the gastric mucosa but it also has systemic immunomodulatory effects that manifest in the airways and lower gastrointestinal tract. Tissue-resident DCs can sample H. pylori antigens in the gastric mucosa and subsequently migrate to the stomach-draining and mesenteric lymph nodes (MLNs), where they prime T-cell (in particular Treg) responses. Alternatively, soluble antigens can be transported via the lymph to the MLNs for presentation by resident DC populations. MLN-derived, H. pylori-specific Tregs enter the circulation and accumulate not only in the gastric mucosa, but also at other mucosal surfaces of the body, such as those of the airways and lower bowel. According to current models, ‘pathogenic’ effector T-cell populations (allergen-specific Th17 and Th2 cells and colitogenic Th1 and Th17 cells) are suppressed by H. pylori-specific Tregs via soluble mediators (such as IL-10) and contact-dependent mechanisms. Th1/2/17, T-helper cell subsets; Treg, regulatory T-cell.
Summary (online only, 6 bullet points, 1-2 sentences each).
-Helicobacter pylori persistently colonizes the gastric mucosa of humans, infecting roughly every other individual worldwide. The prevalence of H. pylori is decreasing in most parts of the developed world due to improved sanitation, reduced transmission and more frequent use of antibiotics in childhood.
-As a consequence of the loss of H. pylori from Western societies, the incidence of peptic ulcer disease and of gastric cancer has decreased continuously in populations affected by this trend. At the same time, allergies and chronic inflammatory disorders have become more common; epidemiological and experimental evidence suggests an inverse causal association between the loss of H. pylori and the rise in these immunological disorders.
-The initial colonization of the hostile environment of the gastric mucosa requires specific adaptations: these include flagella-based motility, production of urease enzyme, chemotaxis and helical cell shape.
-To establish persistent infection, H. pylori has evolved to avoid recognition by pattern recognition receptors of the innate immune system, and to preferentially activate receptors coupling to anti-inflammatory signaling pathways. Its pathogen-associated molecular patterns are substantially less bioactive than those of related gram-negative enteropathogens.
-Another H. pylori persistence strategy involves the prevention and manipulation of T-cell-mediated adaptive immunity. Specific virulence factors are produced by all strains of H. pylori to block T-cell activation, proliferation and effector functions, and to preferentially induce T-regulatory over T-effector responses. Asymptomatic carriers are more likely to preferentially generate Treg responses and to harbor dense H. pylori populations than patients with peptic ulcer disease.
-H. pylori causes gastric disease due to its production of vacuolating cytotoxin and a pathogenicity island-encoded type IV secretion system; both virulence determinants act in concert to promote the production of pro-inflammatory cytokines, to disrupt cell polarity and to cause tissue damage. The advantage for the bacteria of the production of these virulence determinants remains poorly understood, and may involve improved iron acquisition or enhanced transmission.
Acknowledgements
Work in the laboratories of NRS and AM is supported by grants AI054423 and AI094839 from the US National Institutes of Health to NRS and grants from the Swiss and Zurich Cantonal Cancer Leagues, the Gebert-Rüf Foundation and the Swiss National Science Foundation to AM. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of these funding agencies.
Glossary Terms
- mucosa-associated lymphoid tissue (MALT) lymphoma
A cancer originating from marginal zone B cells of mucosa-associated lymphoid tissue. H. pylori infection-associated MALT lymphomas can often be treated with H. pylori eradication therapy which eliminates the antigenic driver of proliferation.
- gastric adenocarcinoma
A malignant epithelial tumor originating from the glandular epithelium of the stomach.
- Type IV secretion system (T4SS)
A Gram-negative bacterial contact dependent specialized secretion system evolutionarily related to the Agrobacterium tumefaciens transforming plasmid pilus. These multi-subunit molecular machines deliver proteins and/or protein-DNA complexes from the bacterial cytoplasm, across the bacterial cell wall (inner membrane, periplasm, outer membrane), and across a target eukaryotic cell plasma membrane to the target cell cytosol.
- SOS response
A coordinated transcriptional response to DNA damage extensively characterized in E. coli which is initiated by activation of RecA through binding to damaged DNA, resulting in inhibition of cell cycle progression and increased expression of DNA repair proteins and mutagenic DNA polymerases.
- natural competence
Ability to take up extracellular DNA and recombine it into the bacterial chromosome.
- gene conversion
An intragenomic recombination event where gene sequences at one position in the genome are replaced with homologous sequence encoded at a different location.
- slipped strand mispairing
A mutagenic process that can occur during DNA replication of dinucleotide or homopolymeric repeats due to mispairing of complementary bases.
- pathogenicity island
Genomic islands that often encode virulence determinants and are typically acquired by horizontal transfer.
- cell polarity
Epithelial cells form connections between cells that restrict free diffusion both within the membrane and between cells resulting in an apical surface oriented towards the lumen and a baso-lateral surface oriented towards the underlying submucosa.
- polarized cell culture model
a monolayer of cultured epithlial cells that form tight junctions, usually grown on filters that allow the apical and basolateral compartments to be accessed separately.
- transcytosis
Movement of molecules across an epithelial cell, including uptake from the apical compartment space and delivery to the baso-lateral compartment.
- transmission electron microscopy
A microscopy technique that transmits a beam of electrons through an ultra thin specimen and is capable of imaging at much higher resolution than light microscopy.
- field emission scanning EM
An electron microscopy technique where an image is produced by scanning the sample with a focused beam of electrons using a field emission gun which generates a smaller diameter beam.
- evolved VgrG subunits
Type VI secretion system subunits that have both a structural role in formation of the secretion apparatus and an effector function upon delivery into host cells.
- fibronectin
an extracellular matrix protein that bind integrins.
- sterilizing immunity
Protective immunity that results in complete clearance of the pathogen, i.e. to below the detection limit, as opposed to a mere reduction in colonization levels.
- adjuvants
pharmacological or immunological agents that are added to vaccine formulations to improve their immunogenicity.
- gastroesophageal reflux disease (GERD)
also called acid reflux disease, refers to mucosal damage caused by stomach acid flowing back from the stomach into the esophagus
- Methacholine
muscarinic receptor agonist that is clinically used to diagnose bronchial hyperreactivity, a hallmark of asthma and of chronic obstructive pulmonary disease. The methacholine challenge test involves inhalation of aerosolized methacholine, which leads to bronchoconstriction.
- pathogen-associated molecular patterns (PAMPs)
molecules with shared molecular motifs that are conserved among certain classes of microbes and detected by innate immune receptors; examples include LPS, lipoteichoic acid, flagellins, double stranded RNA and hypomethylated CpG dinucleotides.
- pattern recognition receptors (PRRs)
surface-localized, endosomal or cytoplasmic receptors expressed by innate immune cells that recognize pathogen-associated or damage-associated molecular patterns; PRRs are classified according to their ligand specificity, function, localization and/or evolutionary relationships.
- dendritic cells (DCs)
innate immune cells of characteristic morphology that serve as antigen- presenting cells; immature DCs constantly sample their environment for invading microorganisms, which are phagocytosed and their antigens processed and presented to T-cells upon migration to lymphoid organs.
- type I interferons
synonymous with IFN-α and IFN-β; cytokines that are expressed by many leukocytes, with especially large quantities derived from plasmacytoid dendritic cells. They have an important role in anti-viral defenses through their activity on NK cells and macrophages.
- MyD88 (Myeloid differentiation primary response gene 88)
cytplasmic adaptor protein that couples ligand-activated TLRs (except TLR3) to downstream signaling pathways ultimately leading to NF-κB activation.
- damage-associated molecular patterns (DAMPs)
also referred to as danger-associated molecular patterns, are factors produced under inflammatory conditions of non-infectious origin or by damaged or stressed tissues. Examples include proteins (e.g. heat shock proteins, S100 proteins), other macromolecules (extracellular or cytoplasmic DNA), ATP, adenosine and uric acid crystals.
- inflammasomes
large cytoplasmic multiprotein complexes that sense microbial infections or danger molecules and initiate auto-proteolytic cleavage of caspase-1, and the subsequent processing and release of pro-inflammatory cytokines, namely IL-1β and IL-18. Various types of inflammasomes can be distinguished based on the Nod-like receptor involved in their activation.
- outer membrane vesicles (OMVs)
also referred to as ‘blebs’, are shed from the outer membrane by Gram-negative bacteria during normal growth, and have been reported to enter and transport virulence factors into host cells. OMVs contain numerous components of the bacterial cell wall, including peptidoglycan.
- regulatory T-cell (Treg)
a subpopulation of mostly CD4+ T cells that suppress immune responses by other cells, maintain self-tolerance and immune homeostasis, and prevent auto-immunity and excessive immunopathology. The lineage-defining transcription factor of Tregs is FoxP3.
- polarized T-effector cell subsets
upon activation via their T-cell receptor, T cells may differentiate into one of several T-helper subtypes, including Th1, Th2 and Th17 cells, which differ in their lineage-defining transcription factors and cytokine expression profiles. The cytokine cocktail provided by the antigen-presenting cell during T-cell activation determines Th subset polarization/ differentiation.
- Ras signalling pathway
Ras is the prototypical member of the Ras superfamily of small GTPases; Ras-regulated signalling pathways control a variety of cellular processes including actin cytoskeletal rearrangements, proliferation, differentiation, cell adhesion, apoptosis, and cell migration. Ras and Ras-related proteins are often deregulated in cancers.
- naive T-cells
T-cells that have not yet come in contact with their cognate antigen
Biography
Anne Müller
Anne Müller studies the pathogenesis of Helicobacter-induced gastric cancer and gastric lymphoma. Additional research interests include H. pylori virulence factors, persistence mechanisms and innate immune recognition. She received her Ph.D. in 2000 at the Max Planck Institute of Infection Biology, Berlin, Germany, and then moved to the laboratory of Stanley Falkow at Stanford University, California, to pursue postdoctoral research on Helicobacter-host interactions. She has been an independent researcher and Faculty member at the Institute of Molecular Cancer Research, University of Zürich, Switzerland, since 2006.
Mara L. Hartung
Mara L. Hartung studied biology at the University of Tübingen, Germany. She is currently pursuing her doctoral studies at the Institute of Molecular Cancer Research, University of Zürich, Switzerland. Her research focuses on investigating the mechanism of DNA damage inflicted on gastric epithelial cells by H. pylori and the implications of this process for gastric carcinogenesis.
Nina Salama
Nina Salama investigates H. pylori pathogenesis with a focus on bacterial determinants that promote persistent colonization. Current insterests include generation and consequeces of helical cell morphology, genetic variation during chronic colonization, mechanisms of transmission and H. pylori interactions with other bacteria and tissues in the upper gastrointestinal tract. She received her Ph.D. in 1995 at the University of California, Berkely, and then moved to the laboratory of Stanley Falkow at Stanford University, California, to pursue postdoctoral research on Helicobacter pylori bacterial genetics. She has been an independent research and Faculty member at the Fred Hutchinson Cancer Research Center and Affiliate Professor of Microbiology at the University of Washington in Seattle Washington, since 2001.
Footnotes
Competing interests
The authors declare that no conflicts of interest exist.
References
- 1.Wroblewski LE, Peek RM, Jr., Wilson KT. Helicobacter pylori and gastric cancer: factors that modulate disease risk. Clin Microbiol Rev. 2010;23:713–39. doi: 10.1128/CMR.00011-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bik EM, et al. Molecular analysis of the bacterial microbiota in the human stomach. Proc Natl Acad Sci U S A. 2006;103:732–7. doi: 10.1073/pnas.0506655103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Palframan SL, Kwok T, Gabriel K. Vacuolating cytotoxin A (VacA), a key toxin for Helicobacter pylori pathogenesis. Front Cell Infect Microbiol. 2012;2:92. doi: 10.3389/fcimb.2012.00092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schreiber S, et al. Rapid loss of motility of Helicobacter pylori in the gastric lumen in vivo. Infect Immun. 2005;73:1584–9. doi: 10.1128/IAI.73.3.1584-1589.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vaishnava S, et al. The antibacterial lectin RegIIIgamma promotes the spatial segregation of microbiota and host in the intestine. Science. 2011;334:255–8. doi: 10.1126/science.1209791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Montecucco C, Rappuoli R. Living dangerously: how Helicobacter pylori survives in the human stomach. Nat Rev Mol Cell Biol. 2001;2:457–66. doi: 10.1038/35073084. [DOI] [PubMed] [Google Scholar]
- 7.Celli JP, et al. Rheology of gastric mucin exhibits a pH-dependent sol-gel transition. Biomacromolecules. 2007;8:1580–6. doi: 10.1021/bm0609691. [DOI] [PubMed] [Google Scholar]
- 8.Celli JP, et al. Helicobacter pylori moves through mucus by reducing mucin viscoelasticity. Proc Natl Acad Sci U S A. 2009;106:14321–6. doi: 10.1073/pnas.0903438106. [Showed that H. pylori is immobilized by gastric mucin gel at low pH, but in the presence of urea induces a pH-dependent gel-to-solution transition that allows the bacterium to swim freely.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Howitt MR, et al. ChePep Controls Helicobacter pylori Infection of the Gastric Glands and Chemotaxis in the Epsilonproteobacteria. MBio. 2011;2 doi: 10.1128/mBio.00098-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rolig AS, Carter JE, Ottemann KM. Bacterial chemotaxis modulates host cell apoptosis to establish a T-helper cell, type 17 (Th17)-dominant immune response in Helicobacter pylori infection. Proc Natl Acad Sci U S A. 2011;108:19749–54. doi: 10.1073/pnas.1104598108. [Demonstrated that chemotaxis promotes interactions between the bacteria and epithelium that drive pro-inflammatory Th17 responses.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rolig AS, Shanks J, Carter JE, Ottemann KM. Helicobacter pylori requires TlpD-driven chemotaxis to proliferate in the antrum. Infect Immun. 2012;80:3713–20. doi: 10.1128/IAI.00407-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Terry K, Williams SM, Connolly L, Ottemann KM. Chemotaxis plays multiple roles during Helicobacter pylori animal infection. Infect Immun. 2005;73:803–11. doi: 10.1128/IAI.73.2.803-811.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bonis M, Ecobichon C, Guadagnini S, Prevost MC, Boneca IG. A M23B family metallopeptidase of Helicobacter pylori required for cell shape, pole formation and virulence. Mol Microbiol. 2010;78:809–19. doi: 10.1111/j.1365-2958.2010.07383.x. [One of two papers that identified cell wall enzymes that reduce crosslinking in the cells wall that promote helical cell shape and that helical shape promotes efficient stomach colonization.] [DOI] [PubMed] [Google Scholar]
- 14.Sycuro LK, et al. Peptidoglycan crosslinking relaxation promotes Helicobacter pylori's helical shape and stomach colonization. Cell. 2010;141:822–33. doi: 10.1016/j.cell.2010.03.046. [One of two papers that identified cell wall enzymes that reduce crosslinking in the cells wall that promote helical cell shape and that helical shape promotes efficient stomach colonization.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sycuro LK, et al. Multiple peptidoglycan modification networks modulate Helicobacter pylori's cell shape, motility, and colonization potential. PLoS Pathog. 2012;8:e1002603. doi: 10.1371/journal.ppat.1002603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Williams SM, et al. Helicobacter pylori chemotaxis modulates inflammation and bacterium-gastric epithelium interactions in infected mice. Infect Immun. 2007;75:3747–57. doi: 10.1128/IAI.00082-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sayi A, et al. The CD4+ T cell-mediated IFN-gamma response to Helicobacter infection is essential for clearance and determines gastric cancer risk. J Immunol. 2009;182:7085–101. doi: 10.4049/jimmunol.0803293. [Revealed that T-cell responses to H. pylori promote clearance on the one hand, and immunopathology on the other, thus complicating vaccination development.] [DOI] [PubMed] [Google Scholar]
- 18.Gobert AP, et al. Helicobacter pylori arginase inhibits nitric oxide production by eukaryotic cells: a strategy for bacterial survival. Proc Natl Acad Sci U S A. 2001;98:13844–9. doi: 10.1073/pnas.241443798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang G, Alamuri P, Maier RJ. The diverse antioxidant systems of Helicobacter pylori. Mol Microbiol. 2006;61:847–60. doi: 10.1111/j.1365-2958.2006.05302.x. [DOI] [PubMed] [Google Scholar]
- 20.Dorer MS, Sessler TH, Salama NR. Recombination and DNA repair in Helicobacter pylori. Annu Rev Microbiol. 2011;65:329–48. doi: 10.1146/annurev-micro-090110-102931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chaturvedi R, et al. Spermine oxidase mediates the gastric cancer risk associated with Helicobacter pylori CagA. Gastroenterology. 2011;141:1696–708. e1–2. doi: 10.1053/j.gastro.2011.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Touati E, et al. Chronic Helicobacter pylori infections induce gastric mutations in mice. Gastroenterology. 2003;124:1408–19. doi: 10.1016/s0016-5085(03)00266-x. [DOI] [PubMed] [Google Scholar]
- 23.Dorer MS, Fero J, Salama NR. DNA damage triggers genetic exchange in Helicobacter pylori. PLoS Pathog. 2010;6:e1001026. doi: 10.1371/journal.ppat.1001026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Orillard E, Radicella JP, Marsin S. Biochemical and cellular characterization of Helicobacter pylori RecA, a protein with high-level constitutive expression. J Bacteriol. 2011;193:6490–7. doi: 10.1128/JB.05646-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dorer MS, Cohen IE, Sessler TH, Fero J, Salama NR. Natural Competence Promotes Helicobacter pylori Chronic Infection. Infect Immun. 2012 doi: 10.1128/IAI.01042-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aras RA, Kang J, Tschumi AI, Harasaki Y, Blaser MJ. Extensive repetitive DNA facilitates prokaryotic genome plasticity. Proc Natl Acad Sci U S A. 2003;100:13579–84. doi: 10.1073/pnas.1735481100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aras RA, et al. Plasticity of repetitive DNA sequences within a bacterial (Type IV) secretion system component. J Exp Med. 2003;198:1349–60. doi: 10.1084/jem.20030381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barrozo RM, et al. Functional Plasticity in the Type IV Secretion System of Helicobacter pylori. PLoS Pathog. 2013;9:e1003189. doi: 10.1371/journal.ppat.1003189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alm RA, et al. Comparative genomics of Helicobacter pylori: analysis of the outer membrane protein families. Infect Immun. 2000;68:4155–68. doi: 10.1128/iai.68.7.4155-4168.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Colbeck JC, Hansen LM, Fong JM, Solnick JV. Genotypic profile of the outer membrane proteins BabA and BabB in clinical isolates of Helicobacter pylori. Infect Immun. 2006;74:4375–8. doi: 10.1128/IAI.00485-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hennig EE, Allen JM, Cover TL. Multiple chromosomal loci for the babA gene in Helicobacter pylori. Infect Immun. 2006;74:3046–51. doi: 10.1128/IAI.74.5.3046-3051.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Solnick JV, Hansen LM, Salama NR, Boonjakuakul JK, Syvanen M. Modification of Helicobacter pylori outer membrane protein expression during experimental infection of rhesus macaques. Proc Natl Acad Sci U S A. 2004;101:2106–11. doi: 10.1073/pnas.0308573100. [First demonstration of gene conversion as a mechanism for phase variation of adhesin expression during experimental infection.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ilver D, et al. Helicobacter pylori adhesin binding fucosylated histo-blood group antigens revealed by retagging. Science. 1998;279:373–7. doi: 10.1126/science.279.5349.373. [DOI] [PubMed] [Google Scholar]
- 34.Kawai M, et al. Evolution in an oncogenic bacterial species with extreme genome plasticity: Helicobacter pylori East Asian genomes. BMC Microbiol. 2011;11:104. doi: 10.1186/1471-2180-11-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mahdavi J, et al. Helicobacter pylori SabA adhesin in persitent infection and chronic inflammation. Science. 2002;297:573–8. doi: 10.1126/science.1069076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Talarico S, Whitefield SE, Fero J, Haas R, Salama NR. Regulation of Helicobacter pylori adherence by gene conversion. Mol Microbiol. 2012 doi: 10.1111/j.1365-2958.2012.08073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Styer CM, et al. Expression of the BabA adhesin during experimental infection with Helicobacter pylori. Infect Immun. 2010;78:1593–600. doi: 10.1128/IAI.01297-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goodwin AC, et al. Expression of the Helicobacter pylori adhesin SabA is controlled via phase variation and the ArsRS signal transduction system. Microbiology. 2008;154:2231–40. doi: 10.1099/mic.0.2007/016055-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Salaun L, Ayraud S, Saunders NJ. Phase variation mediated niche adaptation during prolonged experimental murine infection with Helicobacter pylori. Microbiology. 2005;151:917–23. doi: 10.1099/mic.0.27379-0. [DOI] [PubMed] [Google Scholar]
- 40.Kao CY, Sheu SM, Sheu BS, Wu JJ. Length of thymidine homopolymeric repeats modulates promoter activity of sabA in Helicobacter pylori. Helicobacter. 2012;17:203–9. doi: 10.1111/j.1523-5378.2012.00936.x. [DOI] [PubMed] [Google Scholar]
- 41.Covacci A, et al. Molecular characterization of the 128-kDa immunodominant antigen of Helicobacter pylori associated with cytotoxicity and duodenal ulcer. Proc Natl Acad Sci U S A. 1993;90:5791–5. doi: 10.1073/pnas.90.12.5791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tummuru MK, Cover TL, Blaser MJ. Cloning and expression of a high-molecular-mass major antigen of Helicobacter pylori: evidence of linkage to cytotoxin production. Infect Immun. 1993;61:1799–809. doi: 10.1128/iai.61.5.1799-1809.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Murata-Kamiya N. Pathophysiological functions of the CagA oncoprotein during infection by Helicobacter pylori. Microbes Infect. 2011;13:799–807. doi: 10.1016/j.micinf.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 44.Ohnishi N, et al. Transgenic expression of Helicobacter pylori CagA induces gastrointestinal and hematopoietic neoplasms in mouse. Proc Natl Acad Sci U S A. 2008;105:1003–8. doi: 10.1073/pnas.0711183105. [Using transgenic expression showed that CagA can behave as an oncogene.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yamazaki S, et al. The CagA protein of Helicobacter pylori is translocated into epithelial cells and binds to SHP-2 in human gastric mucosa. J Infect Dis. 2003;187:334–7. doi: 10.1086/367807. [DOI] [PubMed] [Google Scholar]
- 46.Tsugawa H, et al. Reactive Oxygen Species-Induced Autophagic Degradation of Helicobacter pylori CagA Is Specifically Suppressed in Cancer Stem-like Cells. Cell Host Microbe. 2012;12:764–77. doi: 10.1016/j.chom.2012.10.014. [Defined a molecular interaction by which certain alleles of VacA attenuate CagA activity in cells through autophagy dependent degradation. These results provide a possible mechanism for the observed association between carriage of CagA and VacA s1m1 alleles. Additionally the identification of stem-like cells that are resistant to VacA s1m1 autophagy induction indicate a possible CagA-dependent cancer precursor.] [DOI] [PubMed] [Google Scholar]
- 47.Ishimoto T, et al. CD44 variant regulates redox status in cancer cells by stabilizing the xCT subunit of system xc(-) and thereby promotes tumor growth. Cancer Cell. 2011;19:387–400. doi: 10.1016/j.ccr.2011.01.038. [DOI] [PubMed] [Google Scholar]
- 48.Oh JD, Karam SM, Gordon JI. Intracellular Helicobacter pylori in gastric epithelial progenitors. Proc Natl Acad Sci U S A. 2005;102:5186–91. doi: 10.1073/pnas.0407657102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hayashi T, Morohashi H, Hatakeyama M. Bacterial EPIYA effectors - Where do they come from? What are they? Where are they going? Cell Microbiol. 2012;15:377–85. doi: 10.1111/cmi.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mueller D, et al. c-Src and c-Abl kinases control hierarchic phosphorylation and function of the CagA effector protein in Western and East Asian Helicobacter pylori strains. J Clin Invest. 2012;122:1553–66. doi: 10.1172/JCI61143. [Mutational analysis demonstrating that Src and Abl family kinases phosphorylate CagA sequentially and in a tightly controlled fashion.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Israel DA, et al. Helicobacter pylori strain-specific differences in genetic content, identified by microarray, influence host inflammatory responses. J Clin Invest. 2001;107:611–20. doi: 10.1172/JCI11450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Arnold IC, et al. Tolerance rather than immunity protects from Helicobacter pylori-induced gastric preneoplasia. Gastroenterology. 2011;140:199–209. doi: 10.1053/j.gastro.2010.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Philpott DJ, et al. Reduced activation of inflammatory responses in host cells by mouse-adapted Helicobacter pylory isolates. Cell Microbiol. 2002;4:285–96. doi: 10.1046/j.1462-5822.2002.00189.x. [DOI] [PubMed] [Google Scholar]
- 54.Tan S, Noto JM, Romero-Gallo J, Peek RM, Jr., Amieva MR. Helicobacter pylori perturbs iron trafficking in the epithelium to grow on the cell surface. PLoS Pathog. 2011;7:e1002050. doi: 10.1371/journal.ppat.1002050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Terradot L, Waksman G. Architecture of the Helicobacter pylori Cag-type IV secretion system. FEBS J. 2011;278:1213–22. doi: 10.1111/j.1742-4658.2011.08037.x. [DOI] [PubMed] [Google Scholar]
- 56.Christie PJ, Atmakuri K, Krishnamoorthy V, Jakubowski S, Cascales E. Biogenesis, architecture, and function of bacterial type IV secretion systems. Annu Rev Microbiol. 2005;59:451–85. doi: 10.1146/annurev.micro.58.030603.123630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chandran V, et al. Structure of the outer membrane complex of a type IV secretion system. Nature. 2009;462:1011–5. doi: 10.1038/nature08588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fischer W, et al. Systematic mutagenesis of the Helicobacter pylori cag pathogenicity island: essential genes for CagA translocation in host cells and induction of interleukin-8. Mol Microbiol. 2001;42:1337–48. doi: 10.1046/j.1365-2958.2001.02714.x. [DOI] [PubMed] [Google Scholar]
- 59.Pham KT, et al. CagI is an essential component of the Helicobacter pylori Cag type IV secretion system and forms a complex with CagL. PLoS One. 2012;7:e35341. doi: 10.1371/journal.pone.0035341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rohde M, Puls J, Buhrdorf R, Fischer W, Haas R. A novel sheathed surface organelle of the Helicobacter pylori cag type IV secretion system. Mol Microbiol. 2003;49:219–34. doi: 10.1046/j.1365-2958.2003.03549.x. [DOI] [PubMed] [Google Scholar]
- 61.Tanaka J, Suzuki T, Mimuro H, Sasakawa C. Structural definition on the surface of Helicobacter pylori type IV secretion apparatus. Cell Microbiol. 2003;5:395–404. doi: 10.1046/j.1462-5822.2003.00286.x. [DOI] [PubMed] [Google Scholar]
- 62.Kwok T, et al. Helicobacter exploits integrin for type IV secretion and kinase activation. Nature. 2007;449:862–6. doi: 10.1038/nature06187. [First demonstration that CagL can interact with integrins and plays multiple roles in CagA secretion and Cag T4SS dependent pathologic effects on host cells.] [DOI] [PubMed] [Google Scholar]
- 63.Conradi J, et al. An RGD Helper Sequence in CagL of Helicobacter pylori Assists in Interactions with Integrins and Injection of CagA. Front Cell Infect Microbiol. 2012;2:70. doi: 10.3389/fcimb.2012.00070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shaffer CL, et al. Helicobacter pylori exploits a unique repertoire of type IV secretion system components for pilus assembly at the bacteria-host cell interface. PLoS Pathog. 2011;7:e1002237. doi: 10.1371/journal.ppat.1002237. [Developed robust methods to visualize Cag T4SS pili revealing that CagA secretion and Cag pilus formation can be uncoupled.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jimenez-Soto LF, et al. Helicobacter pylori type IV secretion apparatus exploits beta1 integrin in a novel RGD-independent manner. PLoS Pathog. 2009;5:e1000684. doi: 10.1371/journal.ppat.1000684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kaplan-Turkoz B, et al. Structural insights into Helicobacter pylori oncoprotein CagA interaction with beta1 integrin. Proc Natl Acad Sci U S A. 2012;109:14640–5. doi: 10.1073/pnas.1206098109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gorrell RJ, et al. A novel NOD1- and CagA-independent pathway of interleukin-8 induction mediated by the Helicobacter pylori type IV secretion system. Cell Microbiol. 2012 doi: 10.1111/cmi.12055. [DOI] [PubMed] [Google Scholar]
- 68.Saha A, Backert S, Hammond CE, Gooz M, Smolka AJ. Helicobacter pylori CagL activates ADAM17 to induce repression of the gastric H, K-ATPase alpha subunit. Gastroenterology. 2010;139:239–48. doi: 10.1053/j.gastro.2010.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tegtmeyer N, et al. A small fibronectin-mimicking protein from bacteria induces cell spreading and focal adhesion formation. J Biol Chem. 2010;285:23515–26. doi: 10.1074/jbc.M109.096214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wiedemann T, et al. Helicobacter pylori CagL dependent induction of gastrin expression via a novel alphavbeta5-integrin-integrin linked kinase signalling complex. Gut. 2012;61:986–96. doi: 10.1136/gutjnl-2011-300525. [DOI] [PubMed] [Google Scholar]
- 71.Moran AP, Lindner B, Walsh EJ. Structural characterization of the lipid A component of Helicobacter pylori rough- and smooth-form lipopolysaccharides. J Bacteriol. 1997;179:6453–63. doi: 10.1128/jb.179.20.6453-6463.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cullen TW, et al. Helicobacter pylori versus the host: remodeling of the bacterial outer membrane is required for survival in the gastric mucosa. PLoS Pathog. 2012;7:e1002454. doi: 10.1371/journal.ppat.1002454. [First description of the H. pylori phosphatases that are responsible for the modification of lipid A that allows escape from TLR4 recognition and mouse colonization.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ishihara S, et al. Essential role of MD-2 in TLR4-dependent signaling during Helicobacter pylori-associated gastritis. J Immunol. 2004;173:1406–16. doi: 10.4049/jimmunol.173.2.1406. [DOI] [PubMed] [Google Scholar]
- 74.Kawahara T, et al. Type I Helicobacter pylori lipopolysaccharide stimulates toll-like receptor 4 and activates mitogen oxidase 1 in gastric pit cells. Infect Immun. 2001;69:4382–9. doi: 10.1128/IAI.69.7.4382-4389.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yokota S, et al. Highly-purified Helicobacter pylori LPS preparations induce weak inflammatory reactions and utilize Toll-like receptor 2 complex but not Toll-like receptor 4 complex. FEMS Immunol Med Microbiol. 2007;51:140–8. doi: 10.1111/j.1574-695X.2007.00288.x. [DOI] [PubMed] [Google Scholar]
- 76.Smith SM, et al. Tribbles 3: a novel regulator of TLR2-mediated signaling in response to Helicobacter pylori lipopolysaccharide. J Immunol. 2011;186:2462–71. doi: 10.4049/jimmunol.1000864. [DOI] [PubMed] [Google Scholar]
- 77.Rad R, et al. Extracellular and intracellular pattern recognition receptors cooperate in the recognition of Helicobacter pylori. Gastroenterology. 2009;136:2247–57. doi: 10.1053/j.gastro.2009.02.066. [Comprehensive analysis of innate immune recognition of H. pylori using dendritic cells from gene- targeted mice lacking various combinations of PRRs.] [DOI] [PubMed] [Google Scholar]
- 78.Sayi A, et al. TLR-2-activated B cells suppress Helicobacter-induced preneoplastic gastric immunopathology by inducing T regulatory-1 cells. J Immunol. 2011;186:878–90. doi: 10.4049/jimmunol.1002269. [DOI] [PubMed] [Google Scholar]
- 79.Gewirtz AT, et al. Helicobacter pylori flagellin evades toll-like receptor 5-mediated innate immunity. J Infect Dis. 2004;189:1914–20. doi: 10.1086/386289. [DOI] [PubMed] [Google Scholar]
- 80.Andersen-Nissen E, et al. Evasion of Toll-like receptor 5 by flagellated bacteria. Proc Natl Acad Sci U S A. 2005;102:9247–52. doi: 10.1073/pnas.0502040102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Otani K, et al. Toll-like receptor 9 signaling has anti-inflammatory effects on the early phase of Helicobacter pylori-induced gastritis. Biochem Biophys Res Commun. 2012;426:342–9. doi: 10.1016/j.bbrc.2012.08.080. [DOI] [PubMed] [Google Scholar]
- 82.Owyang SY, Luther J, Owyang CC, Zhang M, Kao JY. Helicobacter pylori DNA's anti-inflammatory effect on experimental colitis. Gut Microbes. 2012;3:168–71. doi: 10.4161/gmic.19181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Luther J, et al. Helicobacter pylori DNA decreases pro-inflammatory cytokine production by dendritic cells and attenuates dextran sodium sulphate-induced colitis. Gut. 2011;60:1479–86. doi: 10.1136/gut.2010.220087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Luther J, Dave M, Higgins PD, Kao JY. Association between Helicobacter pylori infection and inflammatory bowel disease: a meta-analysis and systematic review of the literature. Inflamm Bowel Dis. 2010;16:1077–84. doi: 10.1002/ibd.21116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gringhuis SI, den Dunnen J, Litjens M, van der Vlist M, Geijtenbeek TB. Carbohydrate-specific signaling through the DC-SIGN signalosome tailors immunity to Mycobacterium tuberculosis, HIV-1 and Helicobacter pylori. Nat Immunol. 2009;10:1081–8. doi: 10.1038/ni.1778. [DOI] [PubMed] [Google Scholar]
- 86.Gringhuis SI, et al. C-type lectin DC-SIGN modulates Toll-like receptor signaling via Raf-1 kinase-dependent acetylation of transcription factor NF-kappaB. Immunity. 2007;26:605–16. doi: 10.1016/j.immuni.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 87.Strowig T, Henao-Mejia J, Elinav E, Flavell R. Inflammasomes in health and disease. Nature. 2012;481:278–86. doi: 10.1038/nature10759. [DOI] [PubMed] [Google Scholar]
- 88.Kim YG, et al. The cytosolic sensors Nod1 and Nod2 are critical for bacterial recognition and host defense after exposure to Toll-like receptor ligands. Immunity. 2008;28:246–57. doi: 10.1016/j.immuni.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 89.Broz P, Monack DM. Molecular mechanisms of inflammasome activation during microbial infections. Immunol Rev. 2011;243:174–90. doi: 10.1111/j.1600-065X.2011.01041.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Viala J, et al. Nod1 responds to peptidoglycan delivered by the Helicobacter pylori cag pathogenicity island. Nat Immunol. 2004;5:1166–74. doi: 10.1038/ni1131. [DOI] [PubMed] [Google Scholar]
- 91.Kaparakis M, et al. Bacterial membrane vesicles deliver peptidoglycan to NOD1 in epithelial cells. Cell Microbiol. 2009;12:372–85. doi: 10.1111/j.1462-5822.2009.01404.x. [DOI] [PubMed] [Google Scholar]
- 92.Hutton ML, et al. Helicobacter pylori exploits cholesterol-rich microdomains for induction of NF-kappaB-dependent responses and peptidoglycan delivery in epithelial cells. Infect Immun. 2010;78:4523–31. doi: 10.1128/IAI.00439-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Allison CC, Kufer TA, Kremmer E, Kaparakis M, Ferrero RL. Helicobacter pylori induces MAPK phosphorylation and AP-1 activation via a NOD1-dependent mechanism. J Immunol. 2009;183:8099–109. doi: 10.4049/jimmunol.0900664. [DOI] [PubMed] [Google Scholar]
- 94.Grubman A, et al. The innate immune molecule, NOD1, regulates direct killing of Helicobacter pylori by antimicrobial peptides. Cell Microbiol. 2009;12:626–39. doi: 10.1111/j.1462-5822.2009.01421.x. [DOI] [PubMed] [Google Scholar]
- 95.Watanabe T, et al. NOD1 contributes to mouse host defense against Helicobacter pylori via induction of type I IFN and activation of the ISGF3 signaling pathway. J Clin Invest. 2010;120:1645–62. doi: 10.1172/JCI39481. [Description of a new signaling pathway linking NOD1 activation by H. pylori to type I IFN production and infection control.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hitzler I, et al. Caspase-1 Has Both Proinflammatory and Regulatory Properties in Helicobacter Infections, Which Are Differentially Mediated by Its Substrates IL-1beta and IL-18. J Immunol. 2012;188:3594–602. doi: 10.4049/jimmunol.1103212. [DOI] [PubMed] [Google Scholar]
- 97.Tomita T, et al. Expression of Interleukin-18, a Th1 cytokine, in human gastric mucosa is increased in Helicobacter pylori infection. J Infect Dis. 2001;183:620–7. doi: 10.1086/318541. [DOI] [PubMed] [Google Scholar]
- 98.Oertli M, et al. DC-derived IL-18 drives Treg differentiation, murine Helicobacter pylori-specific immune tolerance, and asthma protection. J Clin Invest. 2012;122:1082–96. doi: 10.1172/JCI61029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tu S, et al. Overexpression of interleukin-1beta induces gastric inflammation and cancer and mobilizes myeloid-derived suppressor cells in mice. Cancer Cell. 2008;14:408–19. doi: 10.1016/j.ccr.2008.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.El-Omar EM, et al. Interleukin-1 polymorphisms associated with increased risk of gastric cancer. Nature. 2000;404:398–402. doi: 10.1038/35006081. [DOI] [PubMed] [Google Scholar]
- 101.Benoit BN, et al. Role of ASC in the mouse model of Helicobacter pylori infection. J Histochem Cytochem. 2009;57:327–38. doi: 10.1369/jhc.2008.952366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Akhiani AA, et al. Protection against Helicobacter pylori infection following immunization is IL-12-dependent and mediated by Th1 cells. J Immunol. 2002;169:6977–84. doi: 10.4049/jimmunol.169.12.6977. [DOI] [PubMed] [Google Scholar]
- 103.Akhiani AA, Schon K, Franzen LE, Pappo J, Lycke N. Helicobacter pylori-specific antibodies impair the development of gastritis, facilitate bacterial colonization, and counteract resistance against infection. J Immunol. 2004;172:5024–33. doi: 10.4049/jimmunol.172.8.5024. [DOI] [PubMed] [Google Scholar]
- 104.Ermak TH, et al. Immunization of mice with urease vaccine affords protection against Helicobacter pylori infection in the absence of antibodies and is mediated by MHC class II-restricted responses. J Exp Med. 1998;188:2277–88. doi: 10.1084/jem.188.12.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Velin D, Bachmann D, Bouzourene H, Michetti P. Mast cells are critical mediators of vaccine-induced Helicobacter clearance in the mouse model. Gastroenterology. 2005;129:142–55. doi: 10.1053/j.gastro.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 106.Velin D, et al. Interleukin-17 is a critical mediator of vaccine-induced reduction of Helicobacter infection in the mouse model. Gastroenterology. 2009;136:2237–2246. e1. doi: 10.1053/j.gastro.2009.02.077. [DOI] [PubMed] [Google Scholar]
- 107.Hitzler I, Oertli M, Becher B, Agger EM, Müller A. Dendritic Cells Prevent Rather Than Promote Immunity Conferred by a Helicobacter Vaccine Using a Mycobacterial Adjuvant. Gastroenterology. 2011;141:186–96. doi: 10.1053/j.gastro.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 108.Shi Y, et al. Helicobacter pylori-induced Th17 responses modulate Th1 cell responses, benefit bacterial growth, and contribute to pathology in mice. J Immunol. 2010;184:5121–9. doi: 10.4049/jimmunol.0901115. [DOI] [PubMed] [Google Scholar]
- 109.Stoicov C, et al. T-bet knockout prevents Helicobacter felis-induced gastric cancer. J Immunol. 2009;183:642–9. doi: 10.4049/jimmunol.0900511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gebert B, Fischer W, Weiss E, Hoffmann R, Haas R. Helicobacter pylori vacuolating cytotoxin inhibits T lymphocyte activation. Science. 2003;301:1099–102. doi: 10.1126/science.1086871. [DOI] [PubMed] [Google Scholar]
- 111.Sundrud MS, Torres VJ, Unutmaz D, Cover TL. Inhibition of primary human T cell proliferation by Helicobacter pylori vacuolating toxin (VacA) is independent of VacA effects on IL-2 secretion. Proc Natl Acad Sci U S A. 2004;101:7727–32. doi: 10.1073/pnas.0401528101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sewald X, et al. Integrin subunit CD18 Is the T-lymphocyte receptor for the Helicobacter pylori vacuolating cytotoxin. Cell Host Microbe. 2008;3:20–9. doi: 10.1016/j.chom.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 113.Sewald X, Jimenez-Soto L, Haas R. PKC-dependent endocytosis of the Helicobacter pylori vacuolating cytotoxin in primary T lymphocytes. Cell Microbiol. 2010;13:482–96. doi: 10.1111/j.1462-5822.2010.01551.x. [DOI] [PubMed] [Google Scholar]
- 114.Gerhard M, et al. A secreted low-molecular-weight protein from Helicobacter pylori induces cell-cycle arrest of T cells. Gastroenterology. 2005;128:1327–39. doi: 10.1053/j.gastro.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 115.Schmees C, et al. Inhibition of T-cell proliferation by Helicobacter pylori gamma-glutamyl transpeptidase. Gastroenterology. 2007;132:1820–33. doi: 10.1053/j.gastro.2007.02.031. [DOI] [PubMed] [Google Scholar]
- 116.Oertli M, et al. Helicobacter pylori gamma-glutamyl transpeptidase and vacuolating cytotoxin promote gastric persistence and immune tolerance. Proc Natl Acad Sci U S A. 2013;110:3047–52. doi: 10.1073/pnas.1211248110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kao JY, et al. Helicobacter pylori immune escape is mediated by dendritic cell-induced Treg skewing and Th17 suppression in mice. Gastroenterology. 2010;138:1046–54. doi: 10.1053/j.gastro.2009.11.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kim JM, et al. Stimulation of dendritic cells with Helicobacter pylori vacuolating cytotoxin negatively regulates their maturation via the restoration of E2F1. Clin Exp Immunol. 2011;166:34–45. doi: 10.1111/j.1365-2249.2011.04447.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lundgren A, et al. Mucosal FOXP3-expressing CD4+ CD25high regulatory T cells in Helicobacter pylori-infected patients. Infect Immun. 2005;73:523–31. doi: 10.1128/IAI.73.1.523-531.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Lundgren A, Suri-Payer E, Enarsson K, Svennerholm AM, Lundin BS. Helicobacter pylori-specific CD4+ CD25high regulatory T cells suppress memory T-cell responses to H. pylori in infected individuals. Infect Immun. 2003;71:1755–62. doi: 10.1128/IAI.71.4.1755-1762.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lundgren A, Trollmo C, Edebo A, Svennerholm AM, Lundin BS. Helicobacter pylori-specific CD4+ T cells home to and accumulate in the human Helicobacter pylori-infected gastric mucosa. Infect Immun. 2005;73:5612–9. doi: 10.1128/IAI.73.9.5612-5619.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Robinson K, et al. Helicobacter pylori-induced peptic ulcer disease is associated with inadequate regulatory T cell responses. Gut. 2008;57:1375–85. doi: 10.1136/gut.2007.137539. [Study demonstrating that asymptomatic carriers predominantly launch Treg responses to H. pylori infection, whereas patients with peptic ulcer disease generate T-effector responses.] [DOI] [PubMed] [Google Scholar]
- 123.Harris PR, et al. Helicobacter pylori gastritis in children is associated with a regulatory T-cell response. Gastroenterology. 2008;134:491–9. doi: 10.1053/j.gastro.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 124.Ismail HF, Fick P, Zhang J, Lynch RG, Berg DJ. Depletion of neutrophils in IL-10(−/−) mice delays clearance of gastric Helicobacter infection and decreases the Th1 immune response to Helicobacter. J Immunol. 2003;170:3782–9. doi: 10.4049/jimmunol.170.7.3782. [DOI] [PubMed] [Google Scholar]
- 125.Salama NR, Otto G, Tompkins L, Falkow S. Vacuolating cytotoxin of Helicobacter pylori plays a role during colonization in a mouse model of infection. Infect Immun. 2001;69:730–6. doi: 10.1128/IAI.69.2.730-736.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chevalier C, Thiberge JM, Ferrero RL, Labigne A. Essential role of Helicobacter pylori gamma-glutamyltranspeptidase for the colonization of the gastric mucosa of mice. Mol Microbiol. 1999;31:1359–72. doi: 10.1046/j.1365-2958.1999.01271.x. [DOI] [PubMed] [Google Scholar]
- 127.Blaser MJ, Falkow S. What are the consequences of the disappearing human microbiota? Nat Rev Microbiol. 2009;7:887–94. doi: 10.1038/nrmicro2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Amberbir A, et al. Effects of Helicobacter pylori, geohelminth infection and selected commensal bacteria on the risk of allergic disease and sensitization in 3-year-old Ethiopian children. Clin Exp Allergy. 2011 doi: 10.1111/j.1365-2222.2011.03831.x. [DOI] [PubMed] [Google Scholar]
- 129.Blaser MJ, Chen Y, Reibman J. Does Helicobacter pylori protect against asthma and allergy? Gut. 2008;57:561–7. doi: 10.1136/gut.2007.133462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Chen Y, Blaser MJ. Inverse associations of Helicobacter pylori with asthma and allergy. Arch Intern Med. 2007;167:821–7. doi: 10.1001/archinte.167.8.821. [DOI] [PubMed] [Google Scholar]
- 131.Chen Y, Blaser MJ. Helicobacter pylori colonization is inversely associated with childhood asthma. J Infect Dis. 2008;198:553–60. doi: 10.1086/590158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Reibman J, et al. Asthma is inversely associated with Helicobacter pylori status in an urban population. PLoS One. 2008;3:e4060. doi: 10.1371/journal.pone.0004060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Arnold IC, et al. Helicobacter pylori infection prevents allergic asthma in mouse models through the induction of regulatory T cells. J Clin Invest. 2011;121:3088–3093. doi: 10.1172/JCI45041. [First experimental evidence documenting a protective effect of H. pylori infection in allergic asthma.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Hayashi T, et al. Tertiary structure-function analysis reveals the pathogenic signaling potentiation mechanism of Helicobacter pylori oncogenic effector CagA. Cell Host Microbe. 2012;12:20–33. doi: 10.1016/j.chom.2012.05.010. [Using a combination of NMR, X-ray crystallography, modeling and mutational analysis revealed molecular mechanisms by which CagA interacts with multiple cellular targets.] [DOI] [PubMed] [Google Scholar]
- 135.Murata-Kamiya N, Kikuchi K, Hayashi T, Higashi H, Hatakeyama M. Helicobacter pylori exploits host membrane phosphatidylserine for delivery, localization, and pathophysiological action of the CagA oncoprotein. Cell Host Microbe. 2010;7:399–411. doi: 10.1016/j.chom.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 136.Olbermann P, et al. A global overview of the genetic and functional diversity in the Helicobacter pylori cag pathogenicity island. PLoS Genet. 2010;6:e1001069. doi: 10.1371/journal.pgen.1001069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.de Sablet T, et al. Phylogeographic origin of Helicobacter pylori is a determinant of gastric cancer risk. Gut. 2011;60:1189–95. doi: 10.1136/gut.2010.234468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Yeh YC, et al. H. pylori cagL amino acid sequence polymorphism Y58E59 induces a corpus shift of gastric integrin alpha5beta1 related with gastric carcinogenesis. Mol Carcinog. 2011;50:751–9. doi: 10.1002/mc.20753. [DOI] [PubMed] [Google Scholar]
- 139.Rizzato C, et al. Variations in Helicobacter pylori cytotoxin-associated genes and their influence in progression to gastric cancer: implications for prevention. PLoS One. 2012;7:e29605. doi: 10.1371/journal.pone.0029605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Rupnow MF, Chang AH, Shachter RD, Owens DK, Parsonnet J. Cost-effectiveness of a potential prophylactic Helicobacter pylori vaccine in the United States. J Infect Dis. 2009;200:1311–7. doi: 10.1086/605845. [DOI] [PubMed] [Google Scholar]
- 141.Muller A, Solnick JV. Inflammation, immunity, and vaccine development for Helicobacter pylori. Helicobacter. 2011;16(Suppl 1):26–32. doi: 10.1111/j.1523-5378.2011.00877.x. [DOI] [PubMed] [Google Scholar]
- 142.Czinn SJ, Blanchard T. Vaccinating against Helicobacter pylori infection. Nat Rev Gastroenterol Hepatol. 2011;8:133–40. doi: 10.1038/nrgastro.2011.1. [DOI] [PubMed] [Google Scholar]
- 143.Aebischer T, et al. Correlation of T cell response and bacterial clearance in human volunteers challenged with Helicobacter pylori revealed by randomised controlled vaccination with Ty21a-based Salmonella vaccines. Gut. 2008;57:1065–72. doi: 10.1136/gut.2007.145839. [First human vaccine trial in which volunteers were challenged with live H. pylori; provided first human evidence that T-cells are required for H. pylori infection control.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Malfertheiner P, et al. Safety and immunogenicity of an intramuscular Helicobacter pylori vaccine in noninfected volunteers: a phase I study. Gastroenterology. 2008;135:787–95. doi: 10.1053/j.gastro.2008.05.054. [DOI] [PubMed] [Google Scholar]
- 145.Linz B, et al. An African origin for the intimate association between humans and Helicobacter pylori. Nature. 2007;445:915–8. doi: 10.1038/nature05562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Howson CP, Hiyama T, Wynder EL. The decline in gastric cancer: epidemiology of an unplanned triumph. Epidemiol Rev. 1986;8:1–27. doi: 10.1093/oxfordjournals.epirev.a036288. [DOI] [PubMed] [Google Scholar]
- 147.Herbarth O, et al. Helicobacter pylori colonisation and eczema. J Epidemiol Community Health. 2007;61:638–40. doi: 10.1136/jech.2006.046706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Higgins PD, et al. Prior Helicobacter pylori infection ameliorates Salmonella typhimurium-induced colitis: Mucosal crosstalk between stomach and distal intestine. Inflamm Bowel Dis. 2010 doi: 10.1002/ibd.21489. [DOI] [PMC free article] [PubMed] [Google Scholar]