Abstract
Exercise stresses the pulmonary circulation through increases in cardiac output () and left atrial pressure. Invasive as well as noninvasive studies in healthy volunteers show that the slope of mean pulmonary artery pressure (mPAP)–flow relationships ranges from 0.5 to 3 mm Hg⋅min⋅L−1. The upper limit of normal mPAP at exercise thus approximates 30 mm Hg at a of less than 10 L⋅min−1 or a total pulmonary vascular resistance at exercise of less than 3 Wood units. Left atrial pressure increases at exercise with an average upstream transmission to PAP in a close to one-for-one mm Hg fashion. Multipoint PAP–flow relationships are usually described by a linear approximation, but present with a slight curvilinearity, which is explained by resistive vessel distensibility. When mPAP is expressed as a function of oxygen uptake or workload, plateau patterns may be observed in patients with systolic heart failure who cannot further increase at the highest levels of exercise. Exercise has to be dynamic to avoid the increase in systemic vascular resistance and abrupt changes in intrathoracic pressure that occur with resistive exercise and can lead to unpredictable effects on the pulmonary circulation. Postexercise measurements are unreliable because of the rapid return of pulmonary vascular pressures and flows to the baseline resting state. Recent studies suggest that exercise-induced increase in PAP to a mean higher than 30 mm Hg may be associated with dyspnea-fatigue symptomatology.
Keywords: pulmonary circulation, pulmonary vascular resistance, pulmonary arterial compliance, cardiac output, exercise capacity
After catheterization of the heart had been introduced as a diagnostic tool by Cournand and his colleagues in the 1940s (1), it was realized that many diseases are associated with elevated pressures in the pulmonary circulation and that this can be a cause of dyspnea and fatigue. The questions asked at that time were about the critical levels of pulmonary artery pressures (PAP) that would be of clinical relevance and whether differences in mechanisms of increased PAP might matter. Wood defined limits of normal based on catheterizations of the heart in 60 healthy subjects at the Brompton hospital, which showed PAP ranging from 8/2 to 28/14 mm Hg, with values never exceeding 30/15, mean 20 mm Hg (2). Consequently, he believed that “serious pulmonary hypertension” usually would be associated with much higher pressures. This view was the basis for defining resting pulmonary hypertension as a mean PAP (mPAP) higher than 25 mm Hg, thus with a safety margin of at least 5 mm Hg above the upper limit of normal (3, 4), still agreed upon at the most recent 2008 expert consensus conference held in Dana Point, California (5). Wood and his contemporaries extrapolated the Poiseuille-Hagen notion of resistance as a ratio between a driving pressure and flow to the pulmonary circulation. Pulmonary vascular resistance (PVR) was defined as the ratio of the difference between mPAP and left atrial pressure (LAP) divided by cardiac output ().
The simple use of the PVR equation rewritten as
was at the basis of the hemodynamic classification of pulmonary hypertension being caused either by an increased , an increased LAP, or an increased resistance, and identification of associated causal conditions (2). As it was already known that increases linearly with increased Vo2 or workload (6), it was also realized that PAP could remain within limits of normal at rest but briskly increase with exercise in the presence of increased resistance, such as in chronic obstructive lung disease (7) or increased LAP due to left heart failure or mitral stenosis (8).
The early hemodynamic exercise studies in normal subjects showed that LAP remained within normal limits and that mPAP did not increase “a great deal” (3). Accordingly, exercise-induced pulmonary hypertension was defined by an mPAP higher than 30 mm Hg (3, 4). Again, this was understood as a reasonable threshold for pathological values, not strictly an upper limit of normal. Like for the cut-off value of 25 mm Hg at rest, a safety margin was considered, taking into account possible errors of ±2 mm Hg on invasive measurements of vascular pressures with fluid-filled catheters (3). However, participants at the expert consensus conference in Dana Point believed that this cut-off value was not sufficiently supported by the data reported in the literature and therefore decided to omit exercise from any diagnostic criteria for pulmonary hypertension (5).
In the following sections we provide a historical perspective on use of exercise to probe pulmonary vascular disease as well as a summary of recent advancements in invasive and noninvasive measurements that establish the functional significance of PAP responses to exercise.
The Limits of Normal of the Pulmonary Circulation at Exercise
The first catheterizations of the right heart in normal humans during exercise were reported in the late 1940s. The results showed a small increase, no change, or sometimes a decrease in mPAP as was increased with moderate levels of exercise (9, 10). In 1950, Cournand and colleagues observed a sharp increase in mPAP when was increased to 3.5 times the resting value (11). A similar sharp rise in mPAP at flows above 350% of normal was reported a few years later in isolated perfused lungs (12). However, subsequent studies repeatedly reported a linear increase in mPAP as a function of flow in isolated perfused lungs as well as in intact human beings studied using the unilateral balloon occlusion technique (to double the flow in the contralateral lung) and/or exercise. In his review about pulmonary hemodynamics at exercise published in 1969, Fowler concluded that mPAP–flow relationships are generally best described by a linear approximation until the highest physiologically possible flows, and that previously reported take-off patterns, or disproportionate increase in PAP at the highest flows, were probably explained by a deterioration of the experimental preparation in isolated perfused lung studies and either methodological problems or diastolic dysfunction with an increase in LAP in intact human studies (13).
In 1989, Reeves, Dempsey, and Grover reviewed the published data on invasive pulmonary hemodynamic measurements during exercise in normal subjects (14). They collected 196 measurements in the supine position in 91 subjects (63 men and 28 women from six previous studies) analyzed by Vo2 in steps of 50 or 1,000 ml/min as workload was increased. For each step of Vo2, there were no differences in PAP measurements between men and women, so that the data were pooled in the analysis. They also retrieved a total of 104 measurements in 24 subjects (23 men and 1 woman, from four previous studies and unpublished data from Wagner and Moon) who performed incremental upright exercise. This analysis established that supine exercise is associated with a slight decrease in PVR, which is explained by the distensibility of pulmonary resistive vessels in fully recruited lungs in West’s zone III. In the upright position, the resting PVR was found to be higher, but the exercise PVR was the same and decreased similarly. This is explained by initial derecruitment caused by a lower (via decreased venous return). A higher resting PVR accounts for more marked and hyperbolic decrease of PVR at exercise reported in upright subjects (14).
Reeves and colleagues were able to find measurements at rest and at least two levels of exercise in 63 subjects (including 21 women) so that they could calculate linear regressions relating mPAP to in each of them. On average, each liter per minute of increase in was accompanied by 1 mm Hg increase in mPAP in young adult men and women. Aging to 60 to 80 years was found to be associated with a more than doubling of the slope of mPAP– relationships, to an average of 2.5 mm Hg⋅min⋅L−1.
A more recent review of the literature of invasive pulmonary hemodynamic data in normal subjects conducted by Kovacs and colleagues confirmed these data (15). Invasive measurements of PVR were found in only 13 subjects aged more than 50 years. The review otherwise confirmed an only moderate decrease in PVR at exercise, which was, however, less important or absent in older subjects, and slopes of mPAP– of approximately 1 mm Hg⋅min⋅L−1 in subjects of less than 50 years (15).
As noninvasive measurements allow for an easier recruitment of healthy subjects, the problem with defining the limits of normal of the pulmonary circulation during exercise was revisited using a noninvasive Doppler echocardiographic approach. mPAP was estimated from the maximum velocity of tricuspid regurgitation, LAP from the ratio of mitral flow and annulus E/E′ waves, and was calculated from the left ventricular outflow velocity–time integral (16). In an initial study on 25 healthy subjects aged 35 ± 14 years exercised to a maximum workload of 170 ± 51 W (mean ± SD), the slope of mPAP– was 1.4 ± 0.6 mm Hg⋅min⋅L−1, suggesting a normal range (defined as mean − 2 SD to mean + 2 SD) from 0.2 to 2.6 mm Hg⋅min⋅L−1 (17). This is very similar to previously reported invasive hemodynamic studies (14, 15). The authors repeated the measurements and derived calculations in a population of 56 healthy male and 57 healthy female volunteers aged 19 to 63 years (18). Peak exercise was associated with mPAP of 33 ± 7 mm Hg and of 18 ± 5 L⋅min −1. The slope of mPAP– relationships was 1.5 ± 0.5 mm Hg⋅min⋅L−1, thus defining the limits of normal from 0.5 to 2.5 mm Hg⋅min⋅L−1. The authors acknowledged that these measurements require the highest levels of skill and training, so that it is not known whether noninvasive stress echocardiography of the pulmonary circulation may be generally applicable. Also, more data are needed on the effects of aging.
Even though mPAP– plots can be described by a linear adjustment, inspection of a sufficient number of mPAP– coordinates discloses a slight curvilinearity (19). This is explained by the distensibility of pulmonary resistive vessels and adds to the effects of vascular recruitment to decrease PVR at exercise (14). In vitro measurements of pulmonary vascular distensibility (α) reveal (on average) a 2% change in diameter per mm Hg of mean pressure, and this value is remarkably constant over a wide range of animal species (19, 20). The same α of 2%/mm Hg explains essentially all of the natural curvilinearity of multipoint mPAP– relationships, so that the relationships between mPAP, , and LAP can be described by the equation:
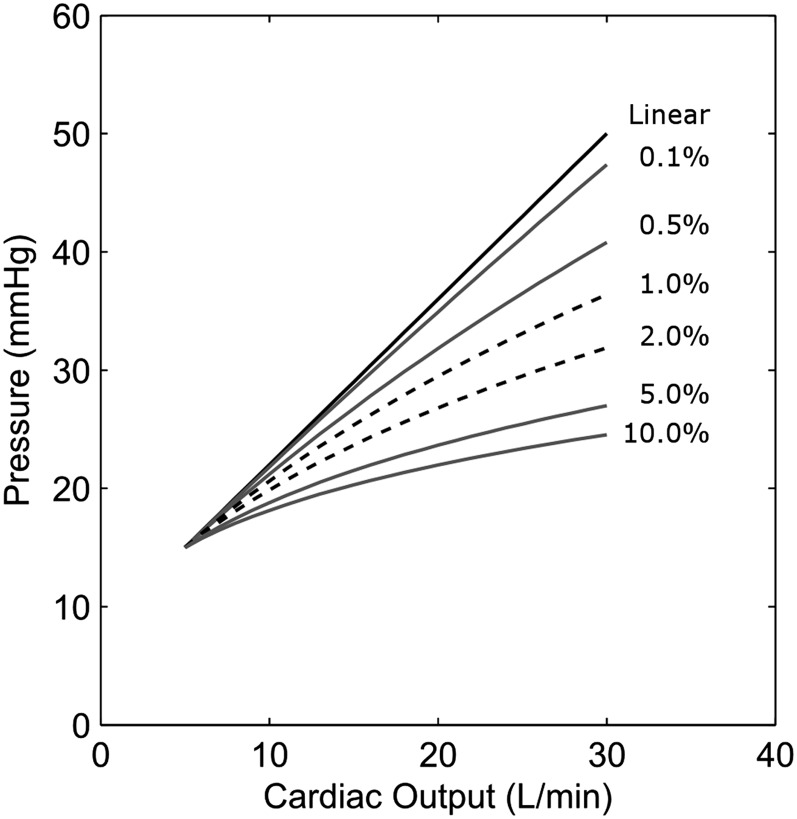
where R0 is total pulmonary vascular resistance. This equation is more complicated than the traditional PVR equation, and an α of 2%/mm Hg pressure may not seem substantial. We therefore modeled the effects of increasing α from 0.1 to 10% on the relationships between mPAP and at LAP maintained constant, as compared with the same relationships predicted by the “linear” model. The results are illustrated in Figure 1. It is apparent that a normal value of 2% markedly decreases mPAP at high levels of and that a decrease in α from 2 to 0.1% greatly increases mPAP at exercise.
Figure 1.
Modeled mean pulmonary artery pressure–flow relationships at progressively increased pulmonary vascular distensibility expressed as % increase in diameter per mm Hg pressure (or α). α is normally less than 2%/mm Hg. A slight increase in vascular distensibility may result in marked decrease in pulmonary artery pressures at exercise.
A recalculation of α from multipoint mPAP– relationships measured in a small number of young adult volunteers in normoxia and in hypobaric hypoxia revealed a value of 2%/mm Hg, which tended to decrease in hypoxia (19). The same calculation of α on the basis of exercise stress echocardiographic measurements in 113 normal volunteers in normoxia revealed an α of 1.3 ± 1.0%/mm Hg. In this study, maximum workload and were higher in men than in women (P < 0.05), but mPAP– relationships were not different. However, women had a higher α (1.6 ± 1.3 vs. 1.1 ± 0.6%/mm Hg; P < 0.05). In addition, the average mPAP– slope was higher and α lower in subjects older than 50 years, even though the study did not include very old subjects (18).
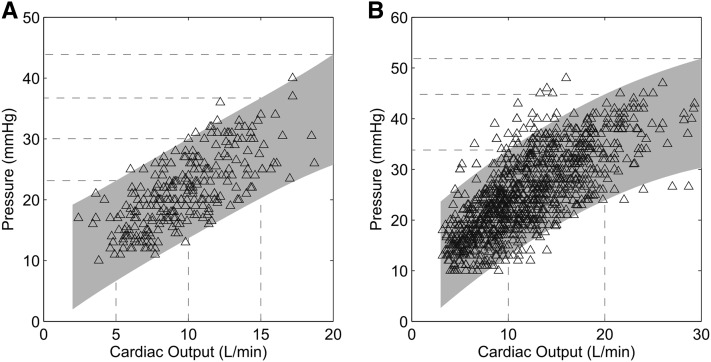
A rigorous reevaluation of the upper limits of normal from the noninvasive measurements reported by Argiento and colleagues (17) indicates the upper limits of normal of mPAP at exercise of 34 mm Hg at a less than 10 L/min, 45 mm Hg at a greater than 10 and less than 20 L/min, and 52 mm Hg at a greater than 20 and less than 30 L/min (Figure 2). These values are in agreement with those previously reported in invasive studies. Because of the uncertainty about the accuracy and precision of echocardiographic measurements of the pulmonary circulation at exercise (16), we analyzed multipoint mPAP– relationships measured at right heart catheterization of 24 normal subjects (15 men and 9 women, aged 54 ± 16 yr) referred to the Massachusetts General Hospital for unexplained dyspnea. These subjects qualified as healthy, as their exercise capacity was normal and no cardiac, pulmonary, or systemic disease accounting for dyspnea could be found. Twenty of them have been reported previously as normal control subjects (21). In these subjects, maximum workload was 138 ± 46 W, mPAP was 15 ± 3 mm Hg at rest and 28 ± 5 at maximum exercise, and was 5.2 ± 1.2 at rest and 13.8 ± 2.5 L⋅min at maximum exercise. The availability of 11 ± 2 minute-by-minute mPAP– measurements per subject during exercise (total of 269 measurements) permitted precise evaluation of pressure–flow relationships and pulmonary vascular distensibility. The slope of mPAP– was 1.5 ± 0.3 mm Hg⋅min⋅L−1, and α was 1.4 ± 0.5% mm Hg−1 (Figure 2). These values are remarkably similar to those of noninvasive echocardiographic studies. Furthermore, in this limited-size healthy-subject group, α was higher in women (n = 9) compared with men (n = 15) (1.6 ± 0.5 vs. 1.3 ± 0.4 mm Hg−1) and decreased in older subjects (1.6 ± 0.5 < 50 yr [n = 9] vs. 1.2 ± 0.4 mm Hg−1 > 50 yr [n = 15]), also very much in keeping with noninvasive measurements.
Figure 2.
(A) Mean pulmonary artery pressure (mPAP)– relationships at rest and at progressively increased workloads in normal subjects measured by echocardiography (n = 113). (B) mPAP– relationships at rest and at progressively increased workloads in normal subjects measured by right heart catheterization (n = 24). The prediction bands are shown by the shaded areas. mPAP at values of 10, 20, and 30 L/min are shown by the stippled lines. There was a good agreement on limits of normal between noninvasive and invasive measurements. Upper limits of normal are estimated as a slope of linearized mPAP– of 3 mm Hg⋅min⋅L−1 or mPAP less than 30 mm Hg at a less than 10 L⋅min−1. Adapted by permission from Reference 16.
It can be seen from these noninvasive and invasive measurements that an mPAP of 30 mm Hg remains an acceptable approximation upper limit of normal at exercise as long as remains below 10 L⋅min−1.
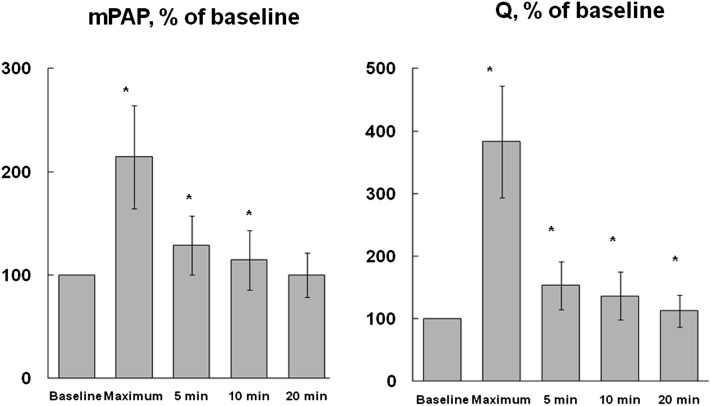
Another important aspect of these studies is that mPAP and rapidly return to resting values, essentially within the first 5 minutes of recovery (17). This is illustrated in Figure 3. Rapid return to normal of pulmonary vascular pressures and flows decreases the relevance of postexercise measurements as a reflection of exercise-induced changes (8).
Figure 3.
Changes in mean pulmonary artery pressure (mPAP) and at maximum exercise and after 5, 10, and 20 minutes’ recovery in 25 healthy subjects. Both mPAP and are almost back to baseline 5 minutes after maximum exercise. Reprinted by permission from Reference 17.
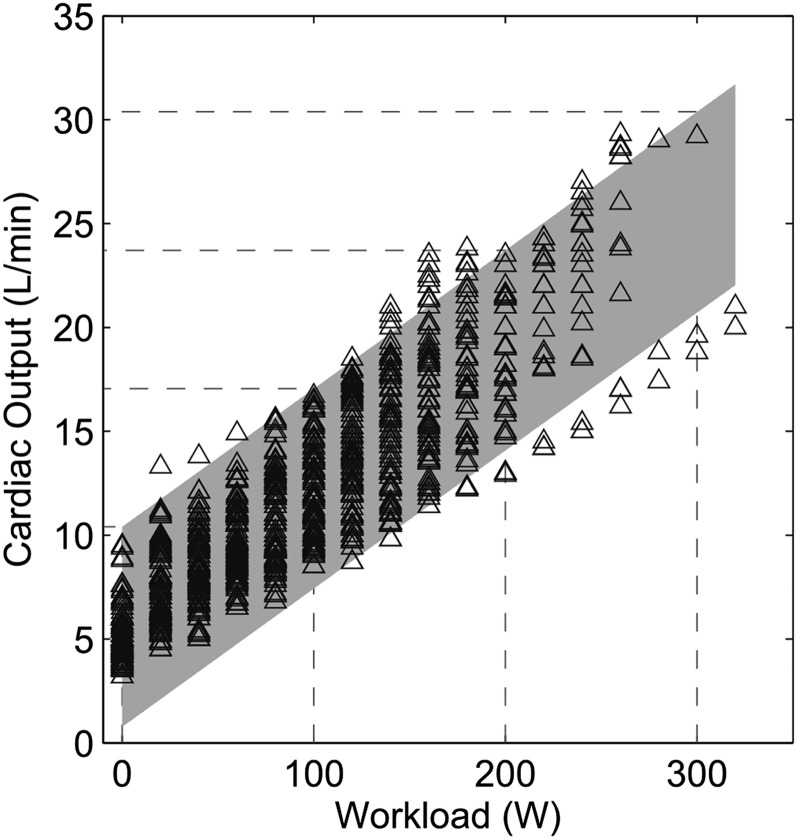
On the other hand, as illustrated in Figure 4, the workload– relationship is quite variable. It is therefore preferable to express mPAP at exercise as a function of rather than of workload to define the functional state of the pulmonary circulation.
Figure 4.
Cardiac output versus workload (W) relationships at exercise. There is wide range of cardiac output values at any given workload. Reprinted by permission from Reference 18.
In summary, both invasive and noninvasive studies show a large interindividual variation of mPAP– relationships, with SDs in the order of the means, which makes it difficult to estimate the limits of normal. Available studies until now have been too limited in size. This is particularly true for older subjects. Noninvasive approaches allow for the recruitment of larger numbers but may be less reliable than “gold standard” invasive measurements. With all these limitations in mind, it appears that a reasonable upper limit of normal of mPAP– relationships is 3 mm Hg⋅min⋅L−1, corresponding to a maximum exercise total PVR of 3 Wood units. Further studies will show if this limit has to be increased in older healthy subjects and for what age range this might be.
Left Atrial Pressure
Until the 1980s, the opinion prevailed that LAP does not change during exercise (3). However, Bevegaard and colleagues had reported an increase in wedge PAP (PAW) up to 25 mm Hg in exercising athletes (22), whereas Granath and colleagues had observed PAW over 30 mm Hg in exercising elderly subjects (23, 24). This increase in PAW with exercise has been repeatedly confirmed and found to be strongly correlated to right atrial pressure (RAP), even though RAP increases less than PAW (25–27). In their analysis of the pulmonary vascular pressure–flow relationships from at least three points during exercise, Reeves and colleagues found a linear increase in PAW with , with a high correlation between these measurements during either supine or upright exercise, and slopes very close to one, suggesting a one-for-one mm Hg upstream transmission of changes in LAP to changes in mPAP (14). This was subsequently confirmed by Lewis and colleagues (21).
There has been discussion as to whether these observations are valid in the presence of higher intrathoracic pressure swings at exercise, particularly regarding the reliability of the estimation of LAP from PAW. However, positive and negative intrathoracic pressures at high levels of ventilation likely cancel each other out in normal subjects, and LAP is probably correctly estimated by a PAW in zone III lungs at high levels of (14). Previous studies have reported a good agreement between PAW and LAP prospectively measured over a wide range of pressures at exercise (8, 28), even though this is not always confirmed in current retrospective quality-control studies (29).
As for the cause of increased PAW or LAP at exercise, this is likely explained by the left ventricle (LV) using the Starling mechanism matching of its flow output to peripheral demand (25). Left ventricular diastolic compliance decreases with increasing diastolic volume, which reaches a maximum at mild to moderate levels of exercise (30). This is due to the intrinsic mechanical properties of the LV, with contribution of competition for space with the right ventricle within the relatively nondistensible pericardium and possible sympathetic nervous system activation. Elite endurance athletes present with parallel increases of LAP and RAP, which occur at higher levels of exercise than in less well trained or sedentary subjects (25), suggesting that pericardial constraint is acting in the elite athletes at very high levels of exercise but not the latter group. This theory is supported by studies on athletic animals showing that when the pericardium is removed, peak end-diastolic volume, stroke volume, and maximal oxygen uptake are increased (31).
Given the hyperbolic relationship between diastolic ventricular pressure and volumes, it is curious that available data rather suggest a linear relationship between PAW and during exercise (14). A possible explanation for this apparent paradox is in the limited number of individual PAW– and mPAP– coordinates reported, making adequate linearity testing difficult. This issue was addressed by Stickland and colleagues in an invasive study in healthy athletes (26). Neither PAW nor RAP increased above normal before Vo2 values of approximately 30 ml⋅kg−1⋅min−1, corresponding to in the range of 20 L⋅min−1. Above this level of exercise, both PAW and RAP increased rapidly in the less-fit subjects but was very much delayed in the fittest subjects, in whom, as expected, stroke volume continued to increase.
Although Stickland and colleagues favored the hypothesis that elite athletes present with a lesser increase in mPAP because of a higher LV compliance, La Gerche and colleagues recently added the notion of the individual variability in exercise-induced decrease in PVR (32). They found that the lowest exercise PVR was associated with pulmonary shunting of agitated contrast, which could be explained by more pronounced vascular distension. They also found that lower exercise PVR and shunting of agitated contrast were associated with lower brain natriuretic peptide levels, in keeping with the notion that more pulmonary vascular distension would allow for lesser right ventricle loading conditions at high .
Argiento and colleagues calculated LAP from transmitral mitral Doppler and mitral annulus tissue Doppler ratio of E and E′ waves in normal exercising individuals and could not find a significant change over a range of Qs from 10 to 26 L⋅min−1, mean 18 L⋅min−1 (17, 18). Although the measurement has been validated during exercise (33), the authors wondered if this negative result might have been artifactual or related to the fact that most subjects did not exercise at levels high enough to be associated with a significant increase in LAP (18).
In summary, on the basis of available exercise measurements in normal subjects, it appears that both mPAP and LAP increase in a broadly linear fashion with . A slight curvilinearity is disclosed by attentive examination of multipoint mPAP– plots.
Exercise Stress Tests for the Detection of Early or Latent Pulmonary Hypertension
Recommendations derived from the 2008 Dana Point conference warned against invasive as well as noninvasive exercise stress testing for early detection of pulmonary hypertension, because of insufficient evidence (34–36). However, more recent recommendations of European and North American societies of echocardiography include exercise stress testing for the detection of pulmonary hypertension in subjects with unexplained dyspnea or valvular heart disease (37). More data are currently being gathered as concepts evolve (16).
An overview of studies of exercise stress tests of the pulmonary circulation for detection of abnormal responses is presented in Table 1. Methods and approaches were highly variable. Some studies relied on Doppler echocardiographic determination of a systolic PAP (sPAP) from maximum velocities of tricuspid regurgitant jets. Abnormal responses were defined by an sPAP greater than 40 mm Hg during exercise (38–41), an sPAP 46 mm Hg immediately after exercise (42), or a postexercise increase in sPAP by greater than 20 mm Hg (43). The measurements were sometimes combined with a determination of maximum oxygen uptake (Vo2max) (41) and eventually confirmed at right heart catheterization in a proportion of patients (41, 43, 44). Some studies added detailed echocardiographic analysis of left ventricular structure and function (42) or lung function tests (43). Some reported on sPAP and measured at several levels of exercise, which appeared to refine the diagnosis of abnormal responses. There were patients with systemic sclerosis with increased slopes of mPAP– but unremarkable maximum sPAP because of a lower exercise capacity (44). A decreased α coefficient was calculated from multipoint mPAP– plots in a small preliminary study on asymptomatic carriers of a bone morphogenetic protein receptor–2 mutation, which is associated with a high risk of idiopathic pulmonary arterial hypertension (PAH) (45).
TABLE 1.
REVIEW OF EXERCISE STRESS STUDIES OF THE PULMONARY CIRCULATION IN PATIENTS WITH UNEXPLAINED DYSPNEA WITH OR WITHOUT RISK FACTORS OF PULMONARY ARTERIAL HYPERTENSION
| Risk Factor | n | Exercise Measurement | Method | Reference |
| HAPE | 9 | sPAP > 40 mm Hg | Echo | Grünig and colleagues (38) |
| PAH relative | 52 | sPAP > 40 mm Hg | Echo | Grünig and colleagues (39) |
| SSc | 24 | sPAP > 40 mm Hg, mPAP– | Echo | Huez and colleagues (44) |
| SSc | 54 | ↑ sPAP > 20 mm Hg post Ex | Echo | Steen and colleagues (43) |
| Dyspnea | 78 | mPAP > 30 mm Hg, Vo2max | RHC | Tolle and colleagues (47) |
| PAH relative | 291 | sPAP > 40 mm Hg | Echo | Grünig and colleagues (40) |
| SSc | 29 | mPAP– | Echo/RHC | Kovacs and colleagues (48) |
| SSc | 52 | sPAP > 40 mm Hg, Vo2max | Echo/RHC | Kovacs and colleagues (41) |
| SSc | 57 | mPAP > 30, TPG > 15 mm Hg | RHC | Saggar and colleagues (46) |
| SSc | 172 | sPAP > 46 mm Hg post Ex | Echo | D'Alto and colleagues (42) |
| CHF | 60 | mPAP– mPAP–W | RHC | Lewis and colleagues (21) |
| Dyspnea, CTEPH | 38 | mPAP > 30 mm Hg | RHC | Whyte and colleagues (49) |
| COPD | 98 | PAP– or PAP–W | RHC | Mykland Hilde and colleagues (54) |
Definition of abbreviations: CHF = congestive heart failure; CTEPH = chronic thromboembolic pulmonary hypertension; echo = echocardiography; Ex = exercise; HAPE = high-altitude pulmonary edema; mPAP = mean pulmonary artery pressure; PAH = pulmonary arterial hypertension; RHC = right heart catheterization; sPAP = systolic pulmonary artery pressure; SSc = systemic sclerosis; TPG = transpulmonary pressure gradient; W = workload.
Invasive studies showed that increased LAP could be a common cause of increased PAP at exercise, particularly in patients with systemic sclerosis (41, 43, 46). Invasive measurements of PAP, , PAW, and Vo2 have improved the understanding of the role of increased PAW as a cause of increased PAP in patients with heart failure (16), suggested that increased slopes of mPAP– or mPAP–workload associated with exercise intolerance (47), and shown that high PAP associated with excessive dyspnea at exercise may be predicted by high-normal resting mPAP in a substantial proportion of patients (48, 49).
Although the exercise stress test based solely on sPAP and workload measurements has shown interest in screening programs, the approach is not satisfactory because PAP is a flow-dependent variable, and the achieved at a given workload varies from one subject to another (8, 18) (Figure 4). Furthermore, the maximum velocity of tricuspid regurgitation is dependent on stroke volume, so that an sPAP higher than 40 to 44 mm Hg, generally accepted at the upper limit of normal at exercise in a general population (38–41), is easily exceeded by exercising athletes (17, 18, 50, 51). Furthermore, sPAP increases with aging and body weight in relation to decreased left ventricular diastolic compliance and associated increase in LAP (52).
How often abnormally increased mPAP at exercise can simply be predicted by upper limit of normal or borderline resting values has not been thoroughly evaluated. However, isolated resting measurements may be more prone to errors in the evaluation of the resistive properties of the pulmonary circulation than multipoint pressure–flow relationships because of the already discussed inherent limitations of isolated PVR calculations (14, 19, 20). Furthermore, exercise-induced pulmonary vasoconstriction, upstream transmission of LAP, and increased intrathoracic pressures are obvious causes of increased slopes of mPAP– relationships (2, 7). Accordingly, “out of proportion” increases in mPAP have been reported in subjects acutely or chronically exposed to environmental hypoxia (53) or in patients with either chronic lung diseases (7, 54) or left heart conditions (2, 8, 21, 29). Patients with chronic obstructive lung diseases are particularly prone to develop dynamic hyperinflation with predominantly positive intrathoracic pressures at exercise, which increases the slope of mPAP– (55).
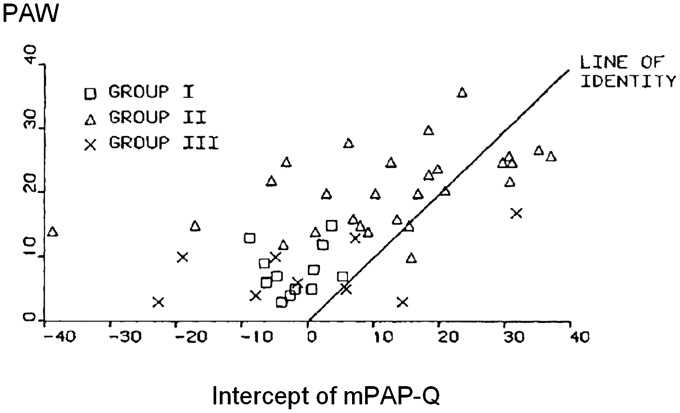
Exercise-induced pulmonary vasoconstriction, increased intrathoracic pressures, or upstream transmission of exercise-induced increase in LAP may be disclosed by negative extrapolated pressure intercepts of (mPAP-PAW)– relationships caused by “out of proportion” increase in mPAP at the highest levels of flow (56–58). This is illustrated in Figure 5, drawn from mPAP and PAW measurements at several levels of flow in patients with advanced left heart failure (groups I and II) or resting pulmonary vascular disease (group III) (56). The zero-flow intercept of (mPAP-PAW)– plots represents the lowest inflow pressure of the pulmonary circulation required to generate a pulmonary blood flow and thus cannot be lower than LAP or PAW taken as the outflow pressure of the pulmonary circulation (56–58). Patients with severe pulmonary hypertension may be prone to exercise-induced pulmonary vasoconstriction because of the combined effects of decreased mixed venous Po2, acidosis, and sympathetic nervous system activation (58). This problem might possibly be avoided by using low-dose dobutamine to increase (58), but there are no reported data to assess this alternative approach to multipoint mPAP– relationships.
Figure 5.
Negative extrapolated pressure intercepts of mean pulmonary artery pressure (mPAP)–flow plots in patients with left heart failure. Group I and II: patients with left ventricular conditions and mPAP less than or greater than 19 mm Hg, respectively. Group III: pulmonary vascular disease. Extrapolated pressure intercepts of mPAP– plots lower than left atrial pressure suggest pulmonary vasoconstriction at high pressures or flows. PAW = pulmonary artery wedge pressure. Reprinted by permission from Reference 56.
Exercise to increase has to be dynamic. Resistive exercise is associated with increased systemic vascular resistance and intrathoracic pressure changes with unpredictable effects on the pulmonary circulation (59). Another important issue is in the timing of the measurements. As already mentioned, the postexercise return to normal of PAP and is rapid, with values almost back to baseline after only a few minutes’ rest (17). Finally, even though Vo2 and workload are linearly related to (6), the measurements cannot be used as surrogates to define the functional state of the pulmonary circulation because the linearity of the relationship is lost at high levels of exercise in heart failure (8, 21) and because the mechanical efficiency of the work varies considerably from one subject to another (17).
The issue is often raised that echocardiographic measurements of the pulmonary circulation would be inaccurate. Several studies have reported on good correlations between pulmonary vascular pressures and flows measured at echocardiography and right heart catheterization (16, 37). However, correlation coefficients largely reflect the variability of the subjects being measured. If one measurement is always twice as big as the other, they are highly correlated but do not agree. Bland and Altman addressed this problem by designing difference versus average plots, to derive the bias, or the difference between the means, and whether it is constant over the range of measurements, and the limits of agreement, or the range of possible errors (60). Thus in the Bland and Altman analysis, the bias informs about accuracy, and the limits of agreement inform about precision. Two previous studies concluded about insufficient accuracy of echocardiography compared with catheterization for the assessment of pulmonary hypertension (61, 62). However, the Bland and Altman plots showed almost no bias but large limits of agreement, rather indicating good accuracy but insufficient precision. Similar results have been reported for measurements by thermodilution compared with the direct Fick method (63) or for PAW compared with direct measurements of LAP (30). Insufficient precision may be in part related to spontaneous physiologic variations. For example, patients with PAH may present with spontaneous variations in up to 22% for mPAP and 36% for PVR (64). It can thus be safely stated that echocardiography of the pulmonary circulation allows for accurate measurements and that the method is valid for population studies. However, insufficient precision may limit the application of the measurements for individual diagnostic purposes. Measurements below or above cut-off values must therefore always be confronted with internal or invasively obtained controls and interpreted with caution in the context of a clinical probability.
Conclusions
Exercise stress tests of the pulmonary circulation have always been part of the diagnosis of pulmonary hypertension as a hemodynamic abnormality. The approach has allowed identification of patients with normal or marginally increased mPAP at rest but with symptomatic increases in mPAP at exercise, related to either increased resistance or increased left atrial pressure. Although this differential diagnosis is of obvious therapeutic relevance, guidelines about exercise stress studies of the pulmonary circulation have not been developed until now for lack of robust evidence allowing for a consensus on clearly defined cut-off values. Matters are further complicated by the physiological variability and interdependency of pulmonary inflow and outflow pressures and .
However, at this stage and in view of recent years’ advances brought about by invasive as well as noninvasive studies, it should be possible to reach a consensus on the following statements:
An exercise-induced increase in mPAP greater than 30 mm Hg at a less than 10 L/min corresponds to a diagnosis of exercise-induced pulmonary hypertension.
Exercise stress hemodynamic investigations should report on measurements of the components of the PVR equation, that is, mPAP, LAP (or PAW), and , to allow for a differential diagnosis of pulmonary vascular disease versus left heart failure.
The limits of normal of mPAP– relationships range from 0.5 to 3.0 mm Hg⋅min⋅L−1.
A slope of mPAP– greater than 3.0 mm Hg⋅min⋅L−1 corresponds to a diagnosis of exercise-induced pulmonary hypertension.
Measurements are preferably invasive but are possible using Doppler echocardiography provided invasive control measurements are performed in case of doubt.
In agreement with a recent editorial (65), it is suggested that more research is needed in the following directions:
Improved definition of physical activity–, age-, and sex-related limits of normal of the pulmonary circulation at exercise
Improved validation of noninvasive methods for the study of the pulmonary circulation during exercise
Further exploration of the impact of exercise-induced pulmonary hypertension on exercise capacity as defined by a whole range of gas exchange and ventilatory variables at cardiopulmonary exercise testing
Measurements of right ventricular function at exercise
Natural history and effects of targeted therapies in patients with exercise-induced pulmonary hypertension in the absence of identifiable left heart or lung disease, thus possibly corresponding to early-stage PAH
Footnotes
Supported by National Institutes of Health grant NIH-K23HL091106 (G.D.L.), Fonds de la Recherche Scientifique Medicale-3.4637.09 (R.N.), Actelion Chair (R.N.), Pfizer Aspire Award (G.D.L.), Marie Curie postdoctoral grant, European Respiratory Society (R.V.).
Author Contributions: R.N., R.V., B.P.D., Rajeev Saggar, Rajan Saggar, J.-L.V., G.D.L.: analysis and interpretation of data, revision of drafted article, final approval; R.N., R.V., B.P.D., G.D.L.: acquisition of data; R.N.: successive drafts of the article.
CME will be available for this article at http://ajrccm.atsjournals.org or at http://cme.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.201211-2090CI on January 24, 2013
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Cournand A, Bloomfield RA, Lauson HD. Double lumen catheter for intravenous and intracardiac blood sampling and pressure recording. Proc Soc Exp Biol Med 1945;60:73–75 [DOI] [PubMed] [Google Scholar]
- 2.Wood P. Pulmonary hypertension with special reference to the vasoconstrictive factor. Br Heart J 1958;20:557–570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fishman AP. Pulmonary circulation. In: American Physiology Society handbook of physiology: section 3. The respiratory system. Circulation and nonrespiratory functions. Vol 1. Bethesda MD: American Physiology Society; 1985. pp. 93–166.
- 4.Rich S, Dantzker DR, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, Fishman AP, Goldring RM, Groves BM, Koerner SK. Primary pulmonary hypertension. A national prospective study. Ann Intern Med 1987;107:216–223 [DOI] [PubMed] [Google Scholar]
- 5.Badesch DB, Champion HC, Sanchez MA, Hoeper MM, Loyd JE, Manes A, McGoon M, Naeije R, Olschewski H, Oudiz RJ, et al. Diagnosis and assessment of pulmonary arterial hypertension. J Am Coll Cardiol 2009;54:S55–S66 [DOI] [PubMed] [Google Scholar]
- 6.Hall JE, Guyton AC. Textbook of medical physiology, 12th ed. Philadelphia, PA: Saunders Elsevier; 2011.
- 7.Weitzenblum E. Chronic cor pulmonale. Heart 2003;89:225–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borlaug BA, Nishimura RA, Sorajja P, Lam CSP, Redfield M. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ Heart Fail 2010;3:588–595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hickman JB, Cargill WH. Effect of exercise on cardiac output and pulmonary artery pressure in normal persons and in patients with cardiovascular disease and pulmonary emphysema. J Clin Invest 1948;27:10–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riley RL, Himmelstein A, Motley HL, Weiner H, Cournand A. Studies of the pulmonary circulation at rest and during exercise in normal individuals and in patients with chronic pulmonary disease. Am J Physiol 1948;152:372–382 [DOI] [PubMed] [Google Scholar]
- 11.Cournand A, Riley RL, Himmelstein A, Austrial R. Pulmonary circulation and alveolar ventilation-perfusion relationships after pneumonectomy. J Thorac Surg 1950;19:80–116 [PubMed] [Google Scholar]
- 12.Lategola MT. Pressure-flow relationships in the dog lung during acute subtotal vascular occlusion. Am J Physiol 1958;192:613–619 [DOI] [PubMed] [Google Scholar]
- 13.Fowler NO. The normal pulmonary arterial pressure-flow relationships during exercise. Am J Med 1969;47:1–6 [DOI] [PubMed] [Google Scholar]
- 14.Reeves JT, Dempsey JA, Grover RF. Pulmonary circulation during exercise. : Pulmonary vascular physiology and physiopathology. Weir EK, Reeves JT, New York: Marcel Dekker; 1989. 107–133 [Google Scholar]
- 15.Kovacs G, Olschewski A, Berhold A, Oschewski H. Pulmonary vascular resistance during exercise in normal subjects: a systematic review. Eur Respir J 2012;39:319–328 [DOI] [PubMed] [Google Scholar]
- 16.Bossone E, D’Andrea A, D’Alto M, Citro R, Argiento P, Ferrara F, Cittadini A, Rubenfire M, Naeije R. Echocardiography in pulmonary arterial hypertension: from diagnosis to prognosis. J Am Soc Echocardiogr 26:1–14. [DOI] [PubMed]
- 17.Argiento P, Chesler N, Mulè M, D’Alto M, Bossone E, Unger P, Naeije R. Exercise stress echocardiography for the study of the pulmonary circulation. Eur Respir J 2010;35:1273–1278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Argiento P, Vanderpool RR, Mule M, Russo MG, D’Alto M, Bossone E, Chesler NC, Naeije R. Exercise stress echocardiography of the pulmonary circulation: limits of normal and sex differences. Chest 2012;142:1158–1165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reeves JT, Linehan JH, Stenmark KR. Distensibility of the normal human lung circulation during exercise. Am J Physiol Lung Cell Mol Physiol 2005;288:L419–L425 [DOI] [PubMed] [Google Scholar]
- 20.Linehan JH, Haworth ST, Nelin LD, Krenz GS, Dawson CA. A simple distensible model for interpreting pulmonary vascular pressure-flow curves. J Appl Physiol 1992;73:987–994 [DOI] [PubMed] [Google Scholar]
- 21.Lewis GD, Murphy RM, Shah RV, Pappagianopoulos PP, Malhotra R, Bloch KD, Systrom DM, Semigran MJ. Pulmonary vascular response patterns during exercise in left ventricular systolic dysfunction predict exercise capacity and outcomes. Circ Heart Fail 2011;4:276–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bevegaard S, Holmgren A, Jonsson B. Circulatory studies in well trained athletes at rest and during heavy exercise, with special reference to stroke volume and the influence of body position. Acta Physiol Scand 1963;57:26–50 [DOI] [PubMed] [Google Scholar]
- 23.Granath A, Jonsson B, Strandell T. Circulation in healthy old men, studied by right heart catheterization at rest and during exercise in supine and sitting position. Acta Med Scand 1964;176:425–446 [DOI] [PubMed] [Google Scholar]
- 24.Granath A, Strandell T. Relationships between cardiac output, stroke volume, and intracardiac pressures at rest and during exercise in supine position and some anthropometric data in healthy old men. Acta Med Scand 1964;176:447–466 [DOI] [PubMed] [Google Scholar]
- 25.Reeves JT, Groves BM, Cymerman A, Sutton JR, Wagner PD, Turkevich D, Houston CS. Operation Everest II: cardiac filling pressures during cycle exercise at sea level. Respir Physiol 1990;80:147–154 [DOI] [PubMed] [Google Scholar]
- 26.Stickland MK, Welsh RC, Petersen SR, Tyberg JV, Anderson WD, Jones RL, Taylor DA, Bouffard M, Haykowsky MJ. Does fitness level modulate the cardiovascular hemodynamic response to exercise? J Appl Physiol 2006;100:1895–1901 [DOI] [PubMed] [Google Scholar]
- 27.Naeije R, Mélot C, Niset G, Delcroix M, Wagner PD. Improved arterial oxygenation by a pharmacological increase in chemosensitivity during hypoxic exercise in normal subjects. J Appl Physiol 1993;74:1666–1671 [DOI] [PubMed] [Google Scholar]
- 28.Thadani U, Parker JO. Hemodynamics at rest and during supine and sitting exercise in normal subjects. Am J Cardiol 1978;41:52–59 [DOI] [PubMed] [Google Scholar]
- 29.Halpern SD, Taichman DB. Misclassification of pulmonary hypertension due to reliance on pulmonary capillary wedge pressure rather than left ventricular end-diastolic pressure. Chest 2009;136:37–43 [DOI] [PubMed] [Google Scholar]
- 30.Sullivan MJ, Cobb FR, Higginbotham MB. Stroke volume increases by similar mechanisms during upright exercise in men and women. Am J Cardiol 1991;67:1405–1412 [DOI] [PubMed] [Google Scholar]
- 31.Stray-Gunderson J, Musch TI, Haidot GC, Swain DP, Ordway GA, Mitchell JH. The effects of pericardiectomy on maximal oxygen consumption and maximal cardiac output in untrained dogs. Circ Res 1986;58:523–530 [DOI] [PubMed] [Google Scholar]
- 32.La Gerche A, MacIsaac AL, Burns AT, Mooney DJ, Inder WJ, Voigt JU, Heidbüchel H, Prior DL. Pulmonary transit of agitated contrast is associated with enhanced pulmonary vascular reserve and right ventricular function at exercise. J Appl Physiol 2010;109:1307–1317 [DOI] [PubMed] [Google Scholar]
- 33.Talreja DR, Nishimura RA, Oh JK. Estimation of left ventricular filling pressure with exercise by Doppler echocardiography in patients with normal systolic function: a simultaneous echocardiographic-cardiac catheterization study. J Am Soc Echocardiogr 2007;20:477–479 [DOI] [PubMed] [Google Scholar]
- 34.Galiè N, Hoeper MM, Humbert M, Torbicki A, Vachiery JL, Barbera JA, Beghetti M, Corris P, Gaine S, Gibbs JS, et al. ; The Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS) endorsed by the International Society of Heart and Lung Transplantation (ISHLT) Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J 2009;30:2493–2537 [DOI] [PubMed] [Google Scholar]
- 35.Galiè N, Hoeper MM, Humbert M, Torbicki A, Vachiery JL, Barbera JA, Beghetti M, Corris P, Gaine S, Gibbs JS, et al. ; The Task Force for Diagnosis and Treatment of Pulmonary Hypertension of European Society of Cardiology (ESC) and the European Respiratory Society (ERS) endorsed by the International Society of Heart and Lung Transplantation (ISHLT). Guidelines for the diagnosis and treatment of pulmonary hypertension Eur Respir J 2009;34:1219–1263 [DOI] [PubMed] [Google Scholar]
- 36.McLaughlin McLaughlin VV, Archer SL, Badesch DB, Barst RJ, Farber HW, Lindner JR, Mathier MA, McGoon MD, Park MH, Rosenson RS, et al. ACCF/AHA 2009 expert consensus document on pulmonary hypertension. A report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association. Circulation 2009;119:2250–2294 [DOI] [PubMed] [Google Scholar]
- 37.Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography, endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 2010;23:685–771 [DOI] [PubMed] [Google Scholar]
- 38.Grünig E, Mereles D, Hildebrandt W, Swenson ER, Kübler W, Kuecherer H, Bärtsch P. Stress Doppler echocardiography for identification of susceptibility to high altitude pulmonary edema. J Am Coll Cardiol 2000;35:980–987 [DOI] [PubMed] [Google Scholar]
- 39.Grünig E, Janssen B, Mereles D, Barth U, Borst MM, Vogt IR, Fischer C, Olschewski H, Kuecherer HF, Kübler W. Abnormal pulmonary artery pressure response in asymptomatic carriers of primary pulmonary hypertension gene. Circulation 2000;102:1145–1150 [DOI] [PubMed] [Google Scholar]
- 40.Grünig E, Weissmann S, Ehlken N, Fijalkowska A, Fischer C, Fourme T, Galié N, Ghofrani A, Harrison RE, Huez S, et al. Stress-Doppler-echocardiography in relatives of patients with idiopathic and familial pulmonary arterial hypertension: results of a multicenter European analysis of pulmonary artery pressure response to exercise and hypoxia. Circulation 2009;119:1747–1757 [DOI] [PubMed] [Google Scholar]
- 41.Kovacs G, Maier R, Aberer E, Brodmann M, Scheidl S, Hesse C, Troester N, Salmhofer W, Stauber R, Fuerst FC, et al. Assessment of pulmonary arterial pressure during exercise in collagen vascular disease: echocardiography vs right-sided heart catheterization. Chest 2010;38:270–278 [DOI] [PubMed] [Google Scholar]
- 42.D’Alto M, Ghio S, D’Andrea A, Pazzano AS, Argiento P, Camporotondo R, Allocca F, Scelsi L, Cuomo G, Caporali R, et al. Inappropriate exercise-induced increase in pulmonary artery pressure in patients with systemic sclerosis. Heart 2011;97:112–117 [DOI] [PubMed] [Google Scholar]
- 43.Steen V, Chou M, Shanmugam V, Mathias M, Kuru T, Morrissey R. Exercise-induced pulmonary arterial hypertension in patients with systemic sclerosis. Chest 2008;134:146–151 [DOI] [PubMed] [Google Scholar]
- 44.Huez S, Roufosse F, Vachièry JL, Pavelescu A, Derumeaux G, Wautrecht JC, Cogan E, Naeije R. Isolated right ventricular dysfunction in systemic sclerosis: latent pulmonary hypertension? Eur Respir J 2007;30:928–936 [DOI] [PubMed] [Google Scholar]
- 45.Pavelescu A, Vanderpool R, Vachiéry JL, Grunig E, Naeije R. Echocardiography of pulmonary vascular function in asymptomatic carriers of BMPR2 mutations. Eur Respir J 2012;40:1287–1289 [DOI] [PubMed] [Google Scholar]
- 46.Saggar R, Khanna D, Furst DE, Shapiro S, Maranian P, Belperio JA, Chauhan N, Clements P, Gorn A, Weigt SS, et al. Exercise-induced pulmonary hypertension associated with systemic sclerosis. Four distinct entities. Arthritis Rheum 2010;62:3741–3750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tolle JJ, Waxman AB, Van Horn TL, Pappagianopoulos PP, Systrom DM. Exercise-induced pulmonary arterial hypertension. Circulation 2008;118:2183–2189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kovacs G, Maier R, Aberer E, Brodmann M, Scheidl S, Tröster N, Hesse C, Salmhofer W, Graninger W, Gruenig E, et al. Borderline pulmonary arterial pressure is associated with decreased exercise capacity in scleroderma. Am J Respir Crit Care Med 2009;181:881–886 [DOI] [PubMed] [Google Scholar]
- 49.Whyte K, Hoette S, Herve P, Montani D, Jaïs X, Parent F, Savale L, Natali D, O’Callaghan DS, Garcia G, et al. The association between resting and mild-to-moderate exercise pulmonary artery pressure. Eur Respir J 2012;39:313–318 [DOI] [PubMed] [Google Scholar]
- 50.Bossone E, Rubenfire M, Bach DS, Ricciardi M, Armstrong WF. Range of tricuspid regurgitation velocity at rest and during exercise in normal adult men: implications for the diagnosis of pulmonary hypertension. J Am Coll Cardiol 1999;33:1662–1666 [DOI] [PubMed] [Google Scholar]
- 51.D’Andrea A, Naeije R, D’Alto M, Argiento P, Golia E, Cocchia R, Riegler L, Scarafile R, Limongelli G, Di Salvo G, et al. Range of pulmonary artery systolic pressure among highly trained athletes. Chest 2011;139:788–794 [DOI] [PubMed] [Google Scholar]
- 52.McQuillan BM, Picard MH, Leavitt M, Weyman AE. Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation 2001;104:2797–2802 [DOI] [PubMed] [Google Scholar]
- 53.Groepenhoff H, Overbeek MJ, Mulè M, van der Plas M, Argiento P, Villafuerte FC, Beloka S, Faoro V, Macarlupu JL, Guenard H, et al. Exercise pathophysiology in patients with chronic mountain sickness. Chest 2012;142:877–884 [DOI] [PubMed] [Google Scholar]
- 54.Mykland Hilde JM, Skjorten I, Hansteen V, Melsom MN, Hisdal J, Humerfelt S, Steine K. Hemodynamic responses to exercise in patients with COPD. Eur Respir J (In press) [DOI] [PubMed]
- 55.Naeije R, Boerrigter BG. Pulmonary hypertension at exercise in COPD: does it matter? Eur Respir J (In press) [DOI] [PubMed]
- 56.Janicki JS, Weber KT, Likoff MJ, Fishman AP. The pressure-flow response of the pulmonary circulation in patients with heart failure and pulmonary vascular disease. Circulation 1985;72:1270–1278 [DOI] [PubMed] [Google Scholar]
- 57.Naeije R, Lipski A, Abramowicz M, Lejeune P, Mélot C, Antoine M, De Smet JM, Leclerc JL, Primo G. Nature of pulmonary hypertension in congestive heart failure. Effects of cardiac transplantation. Am J Respir Crit Care Med 1994;147:881–887 [DOI] [PubMed] [Google Scholar]
- 58.Kafi SA, Mélot C, Vachiéry JL, Brimioulle S, Naeije R. Partitioning of pulmonary vascular resistance in primary pulmonary hypertension. J Am Coll Cardiol 1998;31:1372–1376 [DOI] [PubMed] [Google Scholar]
- 59.MacDougall JD, McKelvie RS, Moroz DE, Sale DG, McCartney N, Buick F. Factors affecting blood pressure during heavy weight lifting and static contractions. J Appl Physiol 1992;73:1590–1597 [DOI] [PubMed] [Google Scholar]
- 60.Bland JM, Altman DG. Statistical methods for assessing agreement between two different methods of clinical measurement. Lancet 1986;1:307–310 [PubMed] [Google Scholar]
- 61.Fisher MR, Forfia PR, Chamera E, Housten-Harris T, Champion HC, Girgis RE, Corretti MC, Hassoun PM. Accuracy of Doppler echocardiography in the hemodynamic assessment of pulmonary hypertension. Am J Respir Crit Care Med 2009;179:615–621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rich JD, Shah SJ, Swamy RS, Kamp A, Rich S. Inaccuracy of Doppler echocardiographic estimates of pulmonary artery pressures in patients with pulmonary hypertension. Chest 2011;139:988–993 [DOI] [PubMed] [Google Scholar]
- 63.Hoeper MM, Maier R, Tongers J, Niedermeyer J, Hohlfeld JM, Hamm M, Fabel H. Determination of cardiac output by the Fick method, thermodilution, and acetylene rebreathing in pulmonary hypertension. Am J Respir Crit Care Med 1999;160:535–541 [DOI] [PubMed] [Google Scholar]
- 64.Rich S, D’Alonzo GE, Dantzker DR, Levy PS. Magnitude and implications of spontaneous hemodynamic variability in primary pulmonary hypertension. Am J Cardiol 1985;55:159–163 [DOI] [PubMed] [Google Scholar]
- 65.Saggar R, Lewis GD, Systrom DM, Champion DM, Naeije R, Saggar R. Pulmonary vascular response to exercise: a hemodynamic observation. Eur Respir J 2012;39:231–234 [DOI] [PubMed] [Google Scholar]