Abstract
Background
Studies demonstrate an increase in radiation exposure with transradial approach (TRA) when compared with transfemoral approach (TFA) for coronary angiography. Given the learning curve associated with TRA, it is not known if this increased radiation exposure to patients is seen when procedures are performed by experienced operators.
Methods
We retrospectively evaluated 1,696 patients who underwent coronary angiography with or without percutaneous coronary intervention (PCI) by experienced operators at a tertiary center from October 2010 to June 2011. Experienced operators were defined as those that perform >75 PCIs/year with >95% of cases performed using the TRA or TFA approach for ≥5 years. The outcomes of interest were dose area product (DAP) and fluoroscopy time (FT).
Results
Of the 1,696 patients, 1,382 (81.5%) were performed by experienced femoral operators using TFA and 314 (18.5%) were performed by experienced radial operators using TRA. Most of these cases (65.4%) were diagnostic only (870 TFA and 240 TRA) with both DAP (6040 [3210–8786] vs 5019 [3377–6869] μGy·m2, P = .003] and FT [6.2 [4.0–10.3] vs 3.3 [2.6–5.0] minutes, P < .001) significantly higher using TRA versus TFA. For procedures involving PCI, despite similar baseline patient, procedural and lesion characteristics, DAP and FT remained significantly higher using TRA versus TFA (19,649 [11,996–25,929] vs 15,395 [10,078–21,617] μGy·m2, P = .02 and 22.1 [13.3–31.0] vs. 13.8 [9.8–20.3] minutes, P < .001).
Conclusions
In a contemporary cohort of patients undergoing coronary angiography by experienced operators, TRA was associated with higher radiation exposure when compared with TFA.
Coronary angiography and interventions under fluoroscopic guidance expose both the patient and operator to variable amounts of radiation. The dose of radiation exposure depends on the duration of the procedure, operator technique, as well as independent patient and lesion characteristics.1 Studies have shown that radiation exposure depends, in part, on the approach (transradial vs transfemoral) to the procedure. Efforts to minimize radiation exposure are of paramount importance.2
There is a growing trend to perform cardiac catheterization procedures utilizing the transradial approach (TRA) due to recent data demonstrating improved outcomes with decreased bleeding and access-site complications when compared to the transfemoral approach (TFA) using unfractionated heparin and glycoprotein IIb/IIIa inhibitors.3–6 However, TRA has also been shown to be associated with longer procedural and fluoroscopy times, with increased exposure to radiation.7,8 TRA has a high learning curve for both diagnostic coronary angiograms and percutaneous coronary interventions (PCI) and therefore requires training and experience. It has been shown that operator experience matters both for reducing the number of access site crossovers9 and in improving outcomes with transradial procedures.3 It is however, not known if radiation exposure is similar to that of TFA when procedures are performed by experienced operators.
Methods
Study design and patient population
The present study is a retrospective analysis of patients who underwent coronary angiography with or without PCI using TRA or TFA by experienced radial (n = 6) and femoral (n = 8) operators, respectively, and had radiation dose data available (n = 1,696) at a tertiary care center from October 2010 to June 2011. The radial operators in this study have lifetime experience with TRA in excess of 1300 cases (operators 1 and 2 report approximately 6,400 cases; operator 3, 2,150 cases; operator 4, 1,500 cases; operator 5, 1,400 cases; and operator 6, 1,300 cases) and perform procedures at multiple institutions. All radial and femoral operators included in this study perform more than 95% of their cases using TRA or TFA only, respectively. Cases involving any additional procedure, such as peripheral angiography or right heart catheterization were excluded. This study was approved by the institutional review board at New York University School of Medicine.
Variables of interest
Baseline patient and procedural characteristics, and operator involvement in each case was abstracted from a review of electronic patient medical records, including cardiac catheterization reports. Baseline lesion characteristics and clinical outcomes were obtained from the institutional database reported to the National Cardiovascular Data Registry. The primary outcome of interest was dose area product (DAP), which reflects both the dose of radiation administered and the area on the patient it is administered to. This is a continuous variable measured in microgray meter squared (μGym2). Secondary outcome were fluoroscopy time (FT) measured in minutes, which reflects the length of time the patient and operator are exposed to radiation; and total dose, measured in milligray (mGy), administered from the angiography system. These parameters of radiation exposure and the number of exposures (number of scenes recorded for review) were obtained from built-in software in the Siemens cardiac angiography system. These measurements are automated and an imaging technology specialist calibrates the device quarterly to ensure reliability.
Coronary angiography and intervention
Approach to coronary angiography and intervention, including access site, type of catheters used, and camera angles during fluoroscopy and cinematography, as well as approach to radiation safety, including use of devices known to reduce radiation scatter, collimation, and magnification, were per individual operator practice. However, every effort is routinely made to reduce radiation exposure in both groups and some features were standard. The interventional rooms are equipped with a ceiling-mounted lead glass screen and table shield systems. For both cases using TFA and those using TRA, conscious sedation is administered prior to arterial puncture and contrast is administered using an automated injector (MEDRAD, MEDRAD Inc, Pittsburgh, PA). For cases using TFA, 6F sheaths and catheters are used for diagnostic angiograms, 500 U of unfractionated heparin is administered through the sheath, and femoral angiography is performed. For cases using TRA, 5 Fr sheaths and catheters are used for diagnostic angiograms and a cocktail with 100 μg nitroglycerin, 2.5 mg verapamil, and 2500 U of unfractionated heparin is administered through the sheath. Routine radial angiography is not performed, unless there was difficulty in advancing a wire or a catheter.
Statistical analysis
Patients were grouped into TRA cases performed by experienced radial operators (n = 314) and TFA cases performed by experienced femoral operators (n = 1,382) in the diagnostic coronary angiogram only and PCI cohorts. The PCI cohort includes both ad-hoc and planned PCI cases. Differences in baseline characteristics were evaluated by χ2 test for categorical variables. Normality was examined using histograms, quantile-quantile plots and Shapiro-Wilk test. Normally and non-normally distributed continuous variables were analyzed by independent-samples t test and Mann-Whitney U test, respectively. Primary and secondary outcomes were not normally distributed and, therefore, are presented as median [interquartile range] and compared with the Mann-Whitney U test. Statistical analysis was conducted using the Statistical Package for Social Sciences software, version 19.0 (SPSS, Chicago, IL). Statistical significance was tested using a 2-sided α level of .05.
Sensitivity analyses
Cardiac catheterization procedures were performed at an academic institution which allows for a junior cardiology fellow to meaningfully participate during diagnostic procedures. As a result, a prespecified sensitivity analysis was performed in the diagnostic cohort excluding cases involving a junior fellow, leaving cases performed only by an experienced operator. In addition, after noting a significantly higher use of left-sided access in the TRA compared with TFA group in the diagnostic cohort, a second sensitivity analysis was performed. Left-sided access is not routinely used by the operators in this study and therefore reflect either underlying difficulty with access or, in the case of radial procedures, a plan to cannulate the left internal mammary artery in patients with a history of coronary artery bypass grafts (CABG). As a result, cases either using left-sided access or involving CABG were excluded from both groups for the second sensitivity analysis. After noting a marginally higher use of pressure wire in the TRA group in the PCI cohort, a sensitivity analysis was performed excluding cases utilizing pressure wire or intravascular ultrasound (IVUS) from the TRA and TFA groups.
No extramural funding was used to support this work. The authors are solely responsible for the design and conduct of this study, all study analyses and drafting and editing of the manuscript.
Results
Diagnostic coronary angiogram only cohort
Baseline characteristics
Baseline characteristics of the diagnostic coronary angiogram only cohort are shown in Table I. The TRA (n = 240) and TFA (n = 870) groups consisted predominately of men (61% and 60%) with a median age of 66 and 65 years, respectively. Left-sided access was utilized in 14% of cases in the TRA group and 2% in the TFA group (P < .001), while 35% of TRA cases and 23% of TFA cases had a junior fellow present (P < .001). A 6.3% increase in the number of exposures and 6.7% increase in the amount of contrast was noted in the TFA compared with the TRA group (P = .007 and P = .009, respectively). In addition, a 5F universal catheter was used to perform 25% of the diagnostic coronary angiograms in the TRA group.
Table I.
Baseline characteristics of patients undergoing TRA versus TFA by experienced radial and femoral operators, respectively, in the diagnostic coronary angiography cohort
| Total cohort | Radial (n = 240) | Femoral (n = 870) | P |
|---|---|---|---|
| Age (y) | 66.0 + 11.8 | 64.5 + 12.6 | .10 |
| Men (%) | 60.8 | 59.7 | .77 |
| Body mass index (kg/m2) | 28.8 + 6.8 | 29.5 + 6.2 | .16 |
| Left-sided access (%) | 14.2 | 2.3 | <.001 |
| Assessment of grafts (%) | 10.0 | 8.5 | .52 |
| Assessment of AV or LV function (%) | 51.3 | 56.6 | .16 |
| Use of IVUS (%) | 1.3 | 2.1 | .59 |
| Use of pressure wire (%) | 0.8 | 2.6 | .14 |
| No. of exposures | 8.0 + 4.4 | 8.5 + 3.4 | .007 |
| Total Contrast use (mL) | 75 [55–101] | 80 [64–104] | .009 |
| Junior fellow present (%) | 34.6 | 22.5 | <.001 |
| After exclusion of cases where a junior fellow is present: | Radial (n = 157) | Femoral (n = 674) | |
|
| |||
| Age (y) | 65.3 + 11.5 | 64.8 + 12.5 | .68 |
| Men (%) | 61.8 | 59.1 | .59 |
| Body mass index (kg/m2) | 28.7 + 6.3 | 29.4 + 6.1 | .22 |
| Left-sided access (%) | 14.6 | 2.4 | <.001 |
| Assessment of grafts (%) | 10.8 | 9.9 | .77 |
| Assessment of AV or LV function (%) | 49.7 | 57.4 | .09 |
| Use of IVUS (%) | 1.9 | 2.4 | 1.00 |
| Use of pressure wire (%) | 0.6 | 3.1 | .10 |
| No. of exposures | 8.3 + 4.5 | 8.6 + 3.6 | .04 |
| Contrast use (mL) | 75 [55–107] | 80 [65–104] | .53 |
|
| |||
| After additional exclusion of cases with left-sided access or assessment of coronary artery bypass grafts: | Radial (n = 132) | Femoral (n = 595) | |
| Age (years) | 64.8 + 11.6 | 63.8 + 12.5 | .43 |
| Men (%) | 59.1 | 56.6 | .63 |
| Body mass index (kg/m2) | 28.6 + 6.5 | 29.5 + 6.2 | .12 |
| Assessment of AV or LV function (%) | 56.1 | 59.2 | .56 |
| Use of IVUS (%) | 0.8 | 2.5 | .33 |
| Use of pressure wire (%) | 0.8 | 3.2 | .15 |
| No. of exposures | 7.6 + 4.0 | 8.1 + 2.5 | .007 |
| Contrast use (mL) | 70 [51–94] | 80 [65–100] | .001 |
AV, Aortic valve; LV, left ventricular.
Data shown as mean ± SD or median [interquartile range].
Outcomes
In the diagnostic coronary angiogram only cohort, all measures of radiation exposure, including DAP, FT, and total dose, were significantly higher (20.3%, 87.9%, and 20.2% higher, respectively) in the TRA compared with TFA groups (Figure 1).
Figure 1.
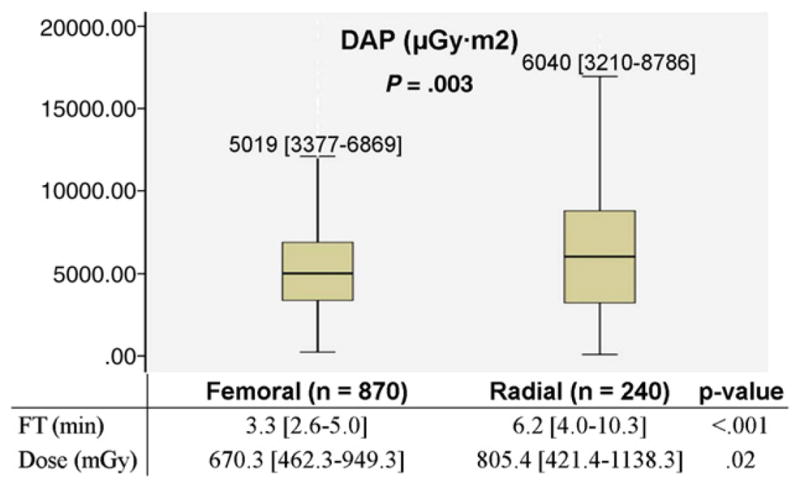
Radiation exposure between patients undergoing TRA versus TFA, in the diagnostic coronary angiography only cohort.
Sensitivity analyses
Baseline characteristics of the diagnostic cohort after exclusion of cases where a junior fellow was present (n = 279) are shown in Table I. The significance was somewhat attenuated but the radiation exposure remained significantly higher in the TRA group when compared with the TFA group for all parameters tested (Figure 2). Compared with cases where a junior fellow was present, in cases where there was no junior fellow involvement, median DAP decreased by 3.9% in the TRA group and 0.6% in the TFA group. In addition, median FT decreased by 8% in the TRA group and 3% in the TFA group. There was minimal change in median total dose in both groups.
Figure 2.
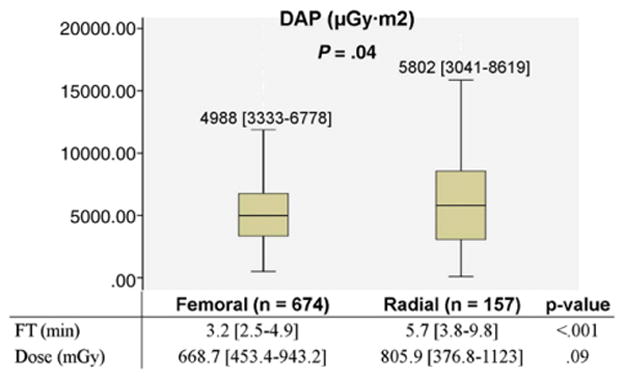
Exploratory analysis of radiation exposure between patients undergoing TRA versus TFA in the diagnostic coronary angiography only cohort after exclusion of cases where a junior fellow was present.
Baseline characteristics of the diagnostic cohort after the additional exclusion of left-sided access and CABG cases (n = 104) are shown in Table I. The different measures of radiation exposure were still numerically higher in the TRA compared with TFA group, although not all were statistically significant. Median DAP was 6.5% higher and median total dose was 4.3% higher in the TRA compared with TFA group, but this was not significantly significant (P = .28 and P = .52, respectively). However, TRA was associated with a 77.4% higher FT when compared with TFA (P < .001) (Figure 3).
Figure 3.
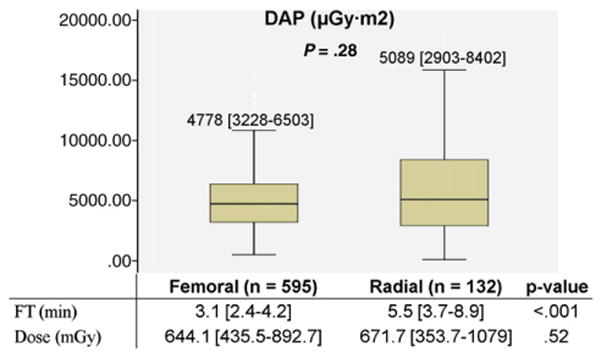
Exploratory analysis of radiation exposure between patients undergoing TRA versus TFA in diagnostic coronary angiography only cohort after additional exclusion of cases with left-sided access or assessment of coronary artery bypass grafts.
PCI cohort
Baseline characteristics
Baseline characteristics of the PCI cohort are shown in Table II. The TRA (n = 74) and TFA (n = 512) groups were predominately elective ad-hoc PCI cases. Patient and procedural characteristics were generally well-balanced between the TRA and TFA groups, with the exception of a non-significant trend towards higher proportion of cases using pressure wire in the TRA compared with TFA group. Overall, procedural complications were low in both groups.
Table II.
Baseline characteristics of patients undergoing TRA versus TFA by experienced radial and femoral operators, respectively, in percutaneous coronary intervention cohort
| Radial (n = 74) | Femoral (n = 512) | P | |
|---|---|---|---|
| Age (y) | 67.5 + 10.1 | 66.3 + 11.0 | .39 |
| Men (%) | 67.6 | 73.4 | .33 |
| Body mass index (kg/m) | 28.6 + 6.3 | 29.4 + 6.1 | .28 |
| Status of case (%) | .40 | ||
| Elective | 79.7 | 73.4 | |
| Urgent | 18.9 | 22.9 | |
| Emergent | 1.4 | 3.7 | |
| Cardiogenic shock (%) | 0.0 | 0.2 | 1.00 |
| Left-sided access (%) | 10.8 | 7.6 | .36 |
| Staged PCI (%) | 10.8 | 14.3 | .48 |
| Assessment of grafts (%) | 1.4 | 4.9 | .23 |
| Assessment of AV or LV function (%) | 36.5 | 37.5 | .90 |
| Use of IVUS (%) | 8.1 | 12.3 | .34 |
| Use of pressure wire (%) | 6.8 | 2.5 | .06 |
| No. of vessels intervened (%) | .58 | ||
| 1 vessel | 94.6 | 91.2 | |
| 2 vessels | 5.4 | 8.4 | |
| No. of stents deployed (%) | .27 | ||
| 1 stent | 66.2 | 62.3 | |
| 2 stents | 24.3 | 21.5 | |
| 3 stents | 8.1 | 7.2 | |
| Graft lesion (%) | 1.4 | 4.9 | .23 |
| Bifurcation lesion (%) | 13.5 | 7.6 | .11 |
| Calcification (%) | 12.2 | 10.4 | .69 |
| Rotational atherectomy (%) | 9.5 | 6.1 | .31 |
| Chronic total occlusion (%) | 8.1 | 3.7 | .11 |
| Long lesion (>33mm) (%) | 8.1 | 10.0 | .83 |
| Class C lesion (%) | 27.0 | 34.0 | .29 |
| Procedural success (%) | 98.6 | 98.0 | 1.00 |
| No. of exposures | 21 [16–28] | 21 [17–28] | .57 |
| Contrast use (mL) | 216 [149–288] | 195 [153–257] | .23 |
| Complications | |||
| Intraprocedural perforation (%) | 1.4 | 0.2 | .24 |
| Intraprocedural flow-limiting dissection (%) | 1.4 | 0.2 | .24 |
| Periprocedural stroke (%) | 0.0 | 0.2 | 1.00 |
| Periprocedural myocardial infarction (%) | 0.0 | 0.0 | 1.00 |
| Tamponade (%) | 0.0 | 0.2 | 1.00 |
| Bleeding within 72 h of procedure (%) | 0.0 | 0.2 | 1.00 |
| Other vascular complication (%) | 0.0 | 0.0 | — |
AV, Aortic valve; LV, left ventricular.
Data shown as mean ± SD or median [interquartile range].
Outcomes
In this PCI cohort, all measures of radiation exposure, including DAP, FT, and total dose, were significantly higher (27.6%, 60.1%, and 24.8% higher, respectively) in the TRA compared with TFA groups (Figure 4). The proportion of cases with FT >60 minutes was low in both groups and not significantly different. While the proportion of cases with total dose >3Gy was significantly higher in the TRA compared with TFA group, there was no significant difference in the proportion of cases with total dose >5Gy.
Figure 4.
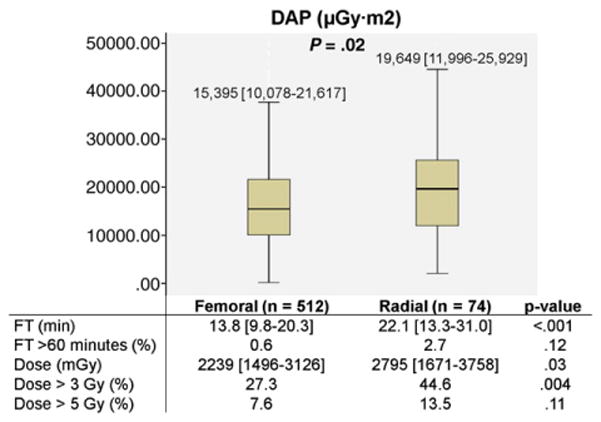
Radiation exposure between patients undergoing TRA versus TFA in percutaneous coronary intervention cohort.
Sensitivity analyses
After exclusion of cases where pressure wire or IVUS was used in the PCI cohort (n = 87), baseline characteristics of the PCI cohort remained similar between the TRA (n = 63) and TFA (n = 436) groups. The significance was somewhat attenuated but DAP (18,298 [11,976–25,071] vs 15,084 [10,061–21,260], P = .04), FT (20.7 [13.1–29.4] vs 13.8 [9.7–20.5], P < .001), and total dose (2638 [1612–3694] vs 2193 [1493–3076], P = .08) remained higher in the TRA vs TFA group. Compared with the overall cohort, in cases where there was no use of pressure wire or IVUS, median DAP decreased by 6.9% in the TRA group and 2.0% in the TFA group. In addition, median FT decreased by 6.3% in the TRA group and 0% in the TFA group, whereas median total dose decreased by 5.6% in the TRA group and 2.1% in the TFA group.
Discussion
This analysis demonstrates that radiation exposure during coronary angiography with or without PCI is higher with TRA when compared with TFA even when performed by experienced operators.
Operator volume and experience does affect outcomes when associated with transradial procedures. Subgroup analysis of the large multicenter randomized RIVAL study demonstrated a benefit in major adverse cardiovascular outcomes of TRA over TFA in patients presenting with ST-segment elevation myocardial infarction and those treated at high-volume centers when the predominant adjunctive therapy used during PCI was unfractionated heparin/glycoprotein IIb/IIIa inhibitors.3 One observational cohort study demonstrated case volume to not only significantly correlate with decreased rates of PCI failure but decreased fluoroscopy time as well, suggesting the need for a case volume of 50 to 100 transradial cases to be considered an experienced operator.10 Another study demonstrated lower procedural success rates (8% less) with all-comer TRA compared with TFA operators and longer fluoroscopic times (82% higher) in TRA cases performed by inexperienced operators compared with TRA cases performed by operators with at least 100 previous procedures performed using TRA.11 The current study includes radial operators who have a lifetime TRA experience of at least 1300 cases and perform more than 95% of their cases using TRA, thereby representing radial operators who are experienced with this approach.
In the current era of increased use of cardiac imaging studies and resulting increased annual radiation exposure, it has become important to note the risk of radiation from coronary angiography and PCI when assessing the risk-benefit ratio of the procedure to a particular patient.12 Adverse side effects of prolonged fluoroscopic procedures and increased radiation exposure over time include dermatologic burns for the patient and increased risk of malignancy to both patients and operators.2 Measures must be taken to reduce radiation exposure including keeping the camera as close to the patient as possible and minimizing camera angulation to reduce radiation scatter, use of collimation and less magnification whenever possible, and use of appropriate shielding. Efforts were made to reduce radiation exposure in both groups by the operators in this study. Variables inherent to TRA and differ compared with TFA is the use of a 5Fr universal catheter in 25% of diagnostic TRA cases and the use of 5Fr catheters in 100% of diagnostic TRA cases (compared with the routine use of 6Fr catheters in diagnostic TFA cases). In the PCI cohort for this study, the proportion of cases using a total dose of more than 3Gy or more than 5Gy is observed to be high and, similar to other radiation parameters, higher in the TRA compared with TFA group, reflecting perhaps the complex case selections for both the groups tested. However, baseline characteristics are not noted to be significantly different in these 2 groups.
Multiple studies have demonstrated higher radiation exposure associated with TRA compared with TFA. One observational cohort study evaluated 928 patients who underwent diagnostic coronary angiograms via TFA (n = 734) or TRA (n = 194) and demonstrated FT to be 58% higher in the TRA compared with TFA group.13 They repeated the analysis with a subgroup of experienced TRA operators and showed FT to be 29% higher in the TRA compared with TFA group. Our results are consistent with this study showing increased FT and radiation exposure with TRA even with experienced operators. A larger study of 5,954 diagnostic coronary angiograms performed at a tertiary cardiac center demonstrated a significant 23% increase in radiation dose with TRA compared with TFA.8 Although the study was performed at a high volume center, 16 operators were examined in this study and all were noted to have some experience in both the radial and femoral approach, but no parameters were used to define operator experience. The current study is one of the few larger studies to focus on a group of experienced operators who perform more than 95% of their cases using either TRA or TFA for cardiac catheterization. The current study also examines DAP as the primary outcome of interest, a better correlate to patient radiation skin dose than FT.14
One study did randomize elective cases performed by an experienced transradial operator to either TRA or TFA; however, the study evaluated only one operator.15 This operator demonstrated a significant 18% increase in FT and 15% increase in DAP with TRA when performing diagnostic coronary angiograms (n = 195), and no difference in radiation exposure with PCI (n = 102). A more recent study demonstrated that selected procedures performed by the radial route were not associated with higher radiation exposure when compared with those performed by the femoral route.16 In this large retrospective analysis, however, there were 6 interventional cardiologists that performed cases using both the radial and femoral approaches. Therefore, the operators decided the approach for these selected cases based on clinical characteristics of the patient, whereas in the current study, the operators were dedicated radial or dedicated femoral operators, and the analysis presented here represents an all-comers population undergoing transradial or transfemoral coronary angiography with or without PCI.
Some studies have shown that TRA via the left radial artery is associated with shorter procedure times and lower radiation exposure due to less tortuosity of the left subclavian artery.17–20 However, the right radial artery is routinely used in clinical practice due to feasibility with room setup and familiarity of manipulating the catheter from the right side as in the femoral approach. In addition, leaning over the patient to manipulate catheters through the left radial artery may be uncomfortable and cause back strain for operators.5 The default approach for the radial operators in the current study was the right radial artery, with the left radial artery only used in the 14% of cases. Left-sided access is used by this group of radial operators when the left internal mammary artery is to be assessed or there is known difficulty in access and approach from the right radial artery. Although the TALENT study, a randomized dual-center study of 1540 patients undergoing left or right radial artery coronary procedures, demonstrated that left radial artery access was associated with lower DAP and FT compared to right radial artery access in the diagnostic only group, there was no difference noted in patients undergoing PCI.20 Furthermore, subgroup analyses demonstrated the benefit of left radial artery access was notable in patients older than 70 years and inexperienced operators. Being older than 70 years was also an independent predictor of subclavian tortuosity and emphasizes the importance of incorporating patient characteristics, in addition to operator experience, when choosing approach. Whether the routine use of the left radial artery results in radiation exposure similar to that associated with TFA remains unknown.
Limitations
There are several limitations with the present study. This is a retrospective analysis from a single center, and, as a result, there may be unmeasured confounding variables. In addition, the sample size is relatively small, and there is a greater proportion of TFA compared with TRA cases given that all of the radial operators compared with 3 out of the 8 femoral operators represented in this analysis perform procedures at multiple institutions. Data from cases performed at other institutions are not available. However, there are 6 experienced radial and 8 experienced femoral operators represented in this study, and cases with concomitant right heart catheterization or any peripheral angiography were excluded (a few of the radial operators in this study perform peripheral procedures using TRA). Lastly, direct radiation exposure to the patient and operator, as measured by dosimeter, were not recorded. DAP is chosen as the primary outcome in this analysis, however, due to its more accurate correlation with patient radiation skin dose than other automated parameters of radiation exposure.14
Conclusions
In conclusion, in a contemporary cohort of patients undergoing coronary angiography by experienced operators, TRA was associated with higher radiation exposure when compared with TFA. Although transradial procedures may have other advantages (reduced access site complications/bleeding), the amount of radiation administered should be borne in mind while caring for such patients.
Acknowledgments
The results of this study were presented at an oral abstract presentation at EuroPCR 2012. Binita Shah was partially funded by an NIH/NHLBI grant (T32HL098129).
References
- 1.Mahesh M. Fluoroscopy: patient radiation exposure issues. Radiographics. 2001;21:1033–45. doi: 10.1148/radiographics.21.4.g01jl271033. [DOI] [PubMed] [Google Scholar]
- 2.Andreassi MG, Cioppa A, Manfredi S, et al. Acute chromosomal DNA damage in human lymphocytes after radiation exposure in invasive cardiovascular procedures. Eur Heart J. 2007;28:2195–9. doi: 10.1093/eurheartj/ehm225. [DOI] [PubMed] [Google Scholar]
- 3.Jolly SS, Yusuf S, Cairns J, et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomized, parallel group, multicenter trial. Lancet. 2011;377:1409–20. doi: 10.1016/S0140-6736(11)60404-2. [DOI] [PubMed] [Google Scholar]
- 4.Pristipino C, Trani C, Nazzaro MS, et al. Major improvement of percutaneous cardiovascular procedure outcomes with radial artery catheterization: results from the PREVAIL study. Heart. 2009;95:476–82. doi: 10.1136/hrt.2008.150714. [DOI] [PubMed] [Google Scholar]
- 5.Rao S, Cohen MG, Kandzari DE, et al. The transradial approach to percutaneous coronary intervention: historical perspective, current concepts, and future directions. J Am Coll Cardiol. 2010;55:2187–95. doi: 10.1016/j.jacc.2010.01.039. [DOI] [PubMed] [Google Scholar]
- 6.Joyal D, Bertrand OF, Rinfret S, et al. Meta-analysis of ten trials on the effectiveness of the radial versus the femoral approach in primary percutaneous coronary intervention. Am J Cardiol. 2012;109:813–8. doi: 10.1016/j.amjcard.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 7.Brueck M, Bandorski D, Kramer W, et al. A randomized comparison of transradial versus transfemoral approach for coronary angiography and angioplasty. J Am Coll Cardiol Intv. 2009;2:1047–54. doi: 10.1016/j.jcin.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 8.Mercuri M, Mehta S, Xie C, et al. Radial artery access as a predictor of increased radiation exposure during a diagnostic cardiac catheterization procedure. J Am Coll Cardiol Intv. 2011;4:347–52. doi: 10.1016/j.jcin.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 9.Burzotta F, Trani C, Mazzari MA, et al. Vascular complications and access crossover in 10,676 transradial percutaneous coronary procedures. Am Heart J. 2012;163:230–8. doi: 10.1016/j.ahj.2011.10.019. [DOI] [PubMed] [Google Scholar]
- 10.Ball WT, Sharieff W, Jolly SS, et al. Characterization of operator learning curve for transradial coronary interventions. Circ Cardiovasc Interv. 2011 Aug;4:336–41. doi: 10.1161/CIRCINTERVENTIONS.110.960864. [DOI] [PubMed] [Google Scholar]
- 11.Looi JL, Cave A, El-Jack S. Learning curve in transradial coronary angiography. Am J Cardiol. 2011;108:1092–5. doi: 10.1016/j.amjcard.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 12.Smith-Bindman R, Miglioretti DL, Johnson E, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996–2010. JAMA. 2012;307:2400–9. doi: 10.1001/jama.2012.5960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farman MT, Khan NU, Sial JA, et al. Comparison of fluoroscopy time during coronary angiography and interventions by radial and femoral routes—can we decrease the fluoroscopy time with increased experience? An observational study. Anadolu Kardiyol Derg. 2011;11:607–12. doi: 10.5152/akd.2011.163. [DOI] [PubMed] [Google Scholar]
- 14.Chida K, Saito H, Otani H, et al. Relationship between fluoroscopic time, dose–area product, body weight, and maximum radiation skin dose in cardiac interventional procedures. Am J Roentgenol. 2006;186:774–8. doi: 10.2214/AJR.04.1653. [DOI] [PubMed] [Google Scholar]
- 15.Lange HW, von Boetticher H. Randomized comparison of operator radiation exposure during coronary angiography and intervention by radial or femoral approach. Catheter Cardiovasc Interv. 2006;67:12–6. doi: 10.1002/ccd.20451. [DOI] [PubMed] [Google Scholar]
- 16.Kuipers G, Delewi R, Velders XL, et al. Radiation exposure during percutaneous coronary interventions and coronary angiograms performed by the radial compared with the femoral route. J Am Coll Cardiol Intv. 2012;5:752–7. doi: 10.1016/j.jcin.2012.03.020. [DOI] [PubMed] [Google Scholar]
- 17.Cha KS, Kim MH, Kim HJ. Prevalence and clinical predictors of severe tortuosity of right subclavian artery in patients undergoing transradial coronary angiography. Am J Cardiol. 2003;92:1220–2. doi: 10.1016/j.amjcard.2003.07.038. [DOI] [PubMed] [Google Scholar]
- 18.Dehghani P, Mohammad A, Bajaj R, et al. Mechanism and predictors of failed transradial approach for percutaneous coronary interventions. J Am Coll Cardiol Intv. 2009;2:1057–64. doi: 10.1016/j.jcin.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 19.Pelliccia F, Trani C, Biondi-Zoccai GGL, et al. Comparison of the feasibility and effectiveness of transradial coronary angiography via right versus left radial artery approaches (from the PREVAIL study) Am J Cardiol. 2012;110:771–5. doi: 10.1016/j.amjcard.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 20.Sciahbasi A, Romagnoli E, Burzotta F, et al. Transradial approach (left vs right) and procedural times during percutaneous coronary procedures: TALENT study. Am Heart J. 2011;161:172–9. doi: 10.1016/j.ahj.2010.10.003. [DOI] [PubMed] [Google Scholar]


