Summary
China has seen the largest human migration in history, and the country's rapid urbanisation has important consequences for public health. A provincial analysis of its urbanisation trends shows shifting and accelerating rural-to-urban migration across the country and accompanying rapid increases in city size and population. The growing disease burden in urban areas attributable to nutrition and lifestyle choices is a major public health challenge, as are troubling disparities in health-care access, vaccination coverage, and accidents and injuries in China's rural-to-urban migrant population. Urban environmental quality, including air and water pollution, contributes to disease both in urban and in rural areas, and traffic-related accidents pose a major public health threat as the country becomes increasingly motorised. To address the health challenges and maximise the benefits that accompany this rapid urbanisation, innovative health policies focused on the needs of migrants and research that could close knowledge gaps on urban population exposures are needed.
Introduction
In the past three decades, China has seen the largest human migration in history, leading to a rise in urban population from 191 million in 1980, to 622 million in 2009—an increase driven largely by rural-to-urban migration.1 China's urban population as a share of the total population is growing rapidly,2 and an additional 200 million rural-to-urban migrants are anticipated during the next 10 years.3 In 2011, the proportion of China's population classified as urban reached 51%, thereby overtaking the rural proportion for the first time.4 With decades of rapid urbanisation still ahead, the health consequences of this trend are of utmost importance for China's population. Health benefits will probably continue to accrue to urban populations, who have better access to health services and education and higher incomes than do their rural counterparts. However, urbanisation will continue to increase population exposure to major risk factors for disease, especially those that relate to the challenging environmental and social conditions (eg, environmental pollution and physical inactivity) that dominate China's large cities. As the country urbanises, the degree of transition to western-style diets and sedentary lifestyles, the trend in outdoor air pollution, and progress in prevention of accidents are important factors that will affect the future health of China's population.
In this Review, we use the criteria that defined urban in China's 2000 census—ie, more than 1500 people per km2, with qualifiers.5 We examine the growth of urban areas, including both geographical expansion and rise in population density within urban areas. Although a dichotomous rural–urban classification has been widely used in China and elsewhere, we discuss work that has attempted to classify areas along a range of so-called urbanicity by use of metrics that capture key aspects of the process of urbanisation.6, 7, 8
Urbanisation
The urban population in China has more than tripled in the past three decades and the number of cities with populations of more than 500 000 people rose from 40 in 1978, to 140 in 2007.9 Furthermore, the rate of urbanisation is accelerating.1 Similar scales of urbanisation took hundreds of years to complete in developed countries. The speed and scale of China's urban growth has been driven by many important factors such as economic reforms in the late 1970s, within-country migration policies, increasing urban–rural income disparities, surplus agricultural labourers, and conversion of farmland for urban use.9
The drivers of migration are often described as push or pull factors (panel ) on the basis of theoretical work.10 This framework has been used to examine the determinants of rural-to-urban migration in China,11 and several especially important factors have been identified—eg, surplus rural labour force (push factor), environmental stress (push factor), and peer relations (pull factor). High quality health care as a pull factor driving migration to urban areas has not been addressed, but is unlikely to be a strong driver in view of the challenges that rural migrants have faced over the past two decades with access to health insurance and affordable care in urban areas.
Panel. Economic, social, and environmental push and pull factors driving migration in China.
Push factors
Economic
-
•
Agricultural failure
-
•
Income variability
-
•
Surplus labourers
-
•
Loss of employment
Social
-
•
Ethnic or other discrimination
-
•
Displeasure with traditional lifestyle
Environmental
-
•
Administrative displacement (eg, Three Gorges Dam)
-
•
Drought or flood
-
•
Disaster (eg, 2008 Wenchuan earthquake)
-
•
Resource depletion (eg, soil erosion), especially in resource-dependent communities (eg, lumber communities)
-
•
Loss of land, conversion of farmland
Pull factors
Economic
-
•
Prospects for high income and remittance
-
•
Job opportunities
-
•
Improved housing
-
•
Health care
Social
-
•
Marriage prospects
-
•
Educational opportunities
-
•
Children, siblings, spouse, or other relatives
Environmental
-
•
Resource discovery (eg, mining find)
Urban population growth in China is characterised by rural-to-urban migration and, to a lesser extent, in-situ urbanisation of rural areas and natural population growth. Nearly 40% of people living in urban areas are migrants, with migrant populations numbering roughly 260 million.1 To accommodate this massive influx and natural population growth within cities, China's urban area has increased rapidly (figure 1 ), with large areas of farmlands converted to urban use—ie, in-situ urbanisation. Historically, this expansion of urban area has been concentrated along the eastern coast, but in the past decade rapid growth has occurred in inland provinces, such as Sichuan.
Figure 1.
China's urban area expansion from 1990 to 2010
The area of China's largest 654 cities was estimated from Landsat Thematic Mapper and Enhanced Thematic Mapper Plus imagery acquired in 1990, 2000, and 2010. Urban area in each province was estimated as the sum of the areas of the individual cities in that province. The large map depicts the size of urban areas in 2010, whereas the two smaller maps are for 1990 and 2000. The pillar in each province represents the ratio of the growth of urban area in that province between 1990 and 2000, to growth between 2000 and 2010. The height of the scale bar is equivalent to a 1·5-times change in area within that period. Data from Wang and colleagues, 2011.12
China's permanent residence registry system (called hukou in Chinese) has had an especially strong effect on the country's urban growth. The system records the residential location of every citizen and divides registered residents into agricultural and non-agricultural groups. People who live in cities hold non-agricultural hukou, whereas farmers and other rural residents hold agricultural hukou. The advantages for those holding non-agricultural hukou in cities are many, and include access to health care, education for children, and housing benefits. To switch official residency to non-agricultural hukou remains difficult. Nearly a fifth of China's total population hold hukou for locations other than where they live—ie, they are migrants.
Urbanisation is closely linked to economic development, with urbanisation driven by and driving economic growth (appendix).13 In China, economic opportunities are a strong pull factor stimulating migration. An important economic effect of migration is to provide a large labour pool for productive activities in urban areas (appendix). Despite the speed and scale of Chinese urbanisation, the process has been distinguished by the absence of widespread proliferation of urban slums seen commonly in expanding urban areas in other developing country settings. This success is partly due to China's governmental commitment to the expansion of housing and basic infrastructure in urban areas.13 Since the 1950s, the government has invested heavily in the construction of housing for urban workers, a practice that has been adopted by private enterprises including large factories and construction companies that draw migrant populations.14, 15 Additionally, as urban boundaries expand, rural villages are subsumed and their rural-turned-urban populations often turn to renting property as an alternative source of income, providing additional housing options for migrant populations.16 Although these activities have restricted the growth of large-scale urban and periurban slums, substandard housing is a major issue, particularly for rural-to-urban migrants without urban hukou, many of whom live in crowded, substandard conditions.
Health and urbanisation
Urbanisation offers opportunities for improvements in population health in China (such as access to improved health care and basic infrastructure) and substantial health risks including air pollution, occupational and traffic hazards, and the risks conferred by changing diets and activity. The pathways through which urbanisation affects health are complex and multifactorial. First, the urban environment itself poses chemical, biological, and physical hazards, which can lead to injury and illness in urban residents. Second, urbanisation triggers changes in occupational activities, socioeconomic status, and social structures that can promote illnesses such as neuropsychiatric disorders, cardiovascular disease, and other non-communicable chronic diseases in both urban and rural populations. Third, the massive rural-to-urban migration that accompanies urbanisation has created particular challenges for health-care delivery in highly mobile and often undocumented populations in China. Finally, urbanisation has connected previously isolated locations through rural-to-urban migration and short-term travel for commerce and recreation, with implications for the spread of communicable infections across the country.
Health-care delivery to rural-to-urban migrants
Urbanisation has long been a major force driving health-care policy in China. Concern about the health of rural-to-urban migrants in the early stages of the country's mass urbanisation was restricted to perceived threats posed by migrants, such as the possibility that this so-called floating population would evade the one-child policy17 and contribute to the introduction of traditional rural infectious diseases to cities.18 Migrant workers consistently underuse health services both in their origin communities and in their destination cities, creating potential short-term and long-term health problems. A large study in Shenzhen—one of the top destinations for migrant workers in China (appendix)—showed that 55% of migrant workers were uninsured, and 62% of migrant workers who reported illness did not visit a doctor.19
China's development strategy shifted to accept and promote migration to urban areas as important for stimulation of economic growth, and several major cities have initiated policies to address the major health issues facing migrants. In the 1990s, Beijing introduced policies intended to regulate the migrant population by, among other things, requiring that migrant workers had certification that they were in good health before they could legally work.20 This policy was tested during the severe acute respiratory syndrome (SARS) outbreak in 2003, when management of migrant workers became crucial for containment of the epidemic in the city.20 In 2006, Beijing changed its approach, dropped the requirement for health certification, and offered basic health-care services through community health-service centres, along with free diagnosis and treatment for tuberculosis and HIV/AIDS.20 Children of migrant workers were offered health-care services equal to those of registered urban citizens.20
Progress has been slow, however, in the improvement of urban health-care access elsewhere. In 2006, only 28% of the urban population were covered by the Basic Health Insurance Scheme, which is the main urban health-care insurance scheme.21, 22 The main reason for this low coverage was that the scheme did not cover informal sector workers and migrant workers.21, 22 Positively, the Ministry of Health announced a pilot project in 2010, modelled on the Beijing programme, that aims to provide health-care services and health education to migrant workers in 65 major cities and counties in 29 provinces.23
The challenges of health-care delivery to rural-to-urban migrants are made especially clear by China's childhood immunisation programmes, which have been substantially complicated by urbanisation. Since the early 1970s, the Planned Immunisation Programme has provided basic vaccines for tuberculosis, diphtheria, pertussis, tetanus, poliomyelitis, and measles; hepatitis B was added in 1992. Since 2005, the programme has offered nine vaccines free of charge to all neonates and infants nationwide, and coverage has increased strikingly in both urban and rural areas. Much progress has been made towards closing the urban–rural gap in coverage. For instance, in 1993, hepatitis B vaccination coverage was less than 50% in nearly all rural communities, whereas it was over 90% in urban areas.24 By contrast, in 2006, hepatitis B vaccination coverage reached 95% in urban neonates and exceeded 80% in most rural areas.25 Despite this progress, the mass rural-to-urban migration over the past two decades has resulted in a troubling trend whereby immunisation coverage in the children of migrants is less extensive than in both their urban and rural counterparts.26, 27, 28, 29 For example, in the Pearl River Delta region of Guangdong Province—which is a major destination for migrant workers (appendix)—average full-dose coverage for tuberculosis, diphtheria, pertussis, tetanus, poliomyelitis, measles, and hepatitis B in the children of migrant workers was estimated to be less than 60%.26 In less developed migrant destinations, such as Guigang City in Guangxi, the full-dose coverage was less than 20%, except for tuberculosis (36%).27 China has addressed these troubling trends by establishing community health-service centres in urban areas to provide basic post-birth immunisation, among other services, but they have been underused by migrant workers. Little awareness of immunisation among migrant parents, the costs associated with inoculation,26, 27 frequent job-related changes of residence,28 and births that violate the one-child policy have been cited as important factors driving low immunisation coverage in their children. To strengthen immunisation programmes to reach this population is now a high priority for China's health policy makers.
The absence of continuous health-care coverage of rural-to-urban migrants puts many at risk of a dual infectious disease burden. Migrants can be exposed to pathogens associated with rural poverty (eg, soil-transmitted helminths) and diseases associated with crowded, urban environments (eg, tuberculosis). For example, parasitic diseases such as schistosomiasis and helminth infections are common in poor rural areas of southwestern and central China, home to more than half of the country's migrant workers. Rural residents are examined and treated regularly by local specialist health agencies (eg, anti-schistosomiasis stations), but infected migrant workers often go undiagnosed and untreated in their urban homes, leading to morbidity and raising the risk of reintroduction of diseases into previously controlled rural areas when workers return home to visit.30 Furthermore, a study in Beijing showed that the crowded working and living conditions of migrant workers might put them at higher risk of tuberculosis infection than permanent residents.31 Urban environments might be associated with an increased risk of sexually transmitted infections, because high-risk sexual behaviours are more common and the prevalence of sexually transmitted infections is higher in rural-to-urban migrants than in their rural counterparts.32
Changing lifestyles and non-communicable disease
Urbanisation has led to changes in patterns of human activity, diet, and social structures in China, with profound implications for non-communicable diseases—eg, diabetes, cardiovascular disease, cancer, and neuropsychiatric disorders. He and colleagues' study33 in a geographically and socially isolated ethnic minority group in southwest China provided early evidence of the effect of urbanisation on chronic disease; age-related increases in blood pressure were greater in individuals who had moved to urban areas than in those who remained in rural villages.33 Since then, researchers have suggested that Chinese urban environments promote lifestyles that place people at risk of hypertension and obesity—risk factors for many non-communicable diseases.
Occupational physical activity is less common in urbanised areas than in rural, agricultural regions and—when compounded with the declines in physical activity that accompany motorised transport and labour-saving household appliances that are common in urban areas—this deficit in energy expenditure is unlikely to be compensated for through leisure physical activities.34, 35 Although the consumption of animal protein and the proportion of calories derived from fat have increased throughout China, individuals living in urbanised areas consume greater amounts of dietary fat than do their rural counterparts.36, 37 In view of the changes in diet and physical activity, that the age-adjusted prevalence of adult hypertension and childhood overweight and obesity in urban areas is roughly double the rates in rural areas is unsurprising.38, 39
Urbanisation-associated changes in diet and physical activity have been accompanied by a rise in cancer in China, and differences in cancer mortality between rural and urban areas have long been reported.40 In Shanghai, the 3 year incidence of gastrointestinal and hormonal cancers—particularly cancers of the colon, kidney, gallbladder, breast, and uterus—has risen substantially since the 1970s, and nationally these incidences are higher in urban areas than in rural areas.41, 42 Increasing evidence exists that obesity, excess calorific intake, and declines in physical activity are carcinogenic.43, 44 The delayed onset of childbirth and reductions in the number of offspring could contribute to the rise in breast cancer incidence. Cancer survival in China is higher in urban than in rural areas, and low-income, poorly educated individuals are more likely to be diagnosed with late-stage cancers than with early-stage cancers.45, 46 These disparities point to the need for expanded access to cancer screening and treatment for poor populations and undeveloped regions outside urban areas.
As urbanisation continues in China, chronic diseases could become less concentrated in urban areas. Worldwide, the urban–rural gap in the distribution of overweight and hypertension diminishes with increasing country-level wealth and development.47, 48 Similarly, obesity, hypertension, physical inactivity, and high intake of dietary fat are more prevalent in towns and cities in China, but the difference in their prevalence between urban and rural areas has declined as the economy has expanded.8 The drivers of these trends are not well understood. Possibly, the rise in these risk factors in rural areas is an indirect result of urbanisation. For example, increased socioeconomic status in rural residents resulting from financial support from family members in urban areas, could affect a rural family's agricultural activities and ability to purchase processed foods. Rural areas can become increasingly urbanised over time and can acquire characteristics of urban environments that promote chronic disease. Longitudinal examination of an area's urbanicity in relation to risk factors for chronic disease could potentially identify specific characteristics of urban environments that promote non-communicable diseases. Efforts to reduce overweight and hypertension and their health sequelae should address the dietary changes and reductions in physical activity that have occurred in both urban and rural populations. The success of behavioural interventions to reduce obesity and hypertension-related chronic disease have been restricted, and structural interventions are necessary—eg, urban planning to promote active lifestyles and agricultural policies that promote healthy diets.49
Urbanisation can also promote neuropsychiatric disorders, which are a leading cause of disease burden in China—an estimated 17% of the adult population has one or more mental disorders.50 Urban environments present psychological stressors such as noise and social isolation,51 and Chinese migrant populations could be especially vulnerable to their effects. Generally, migrant populations have better physical health than their non-migrant peers, but rural-to-urban and urban-to-urban migrants in China report higher psychological distress than do non-migrating populations, a trend that lessens as the length of residence in the urban destination increases.52
Migrant populations could be vulnerable to discrimination and stigmatisation, and also might become stressed by finding work, housing, schools for their children, and health care without the protections and benefits afforded by hukou registration.53 Shifts in family structure as working-age adults leave rural areas have mental health consequences for those left behind, as has been noted in children left in rural villages by rural-to-urban migrant parents.54 Notably, the prevalence of mental illness is similar in rural and urban China, and depressive disorders and alcohol dependency are more prevalent in rural than in urban areas, which is not explained by differential access to treatment.50, 55 Whether rural depression and substance abuse are secondary effects of urbanisation, or urban environments have mental health protective effects remains unclear and warrants investigation. Mental health services that target migrant populations and other high-risk groups are urgently needed; only 5% of Chinese adults with a mental disorder have seen a mental health professional.50
Environmental and occupational risks in urban environments
Despite the massive increase in China's urban population, access to piped drinking water increased from 48% of the urban population in 1990, to nearly 94% in 2007.1 Provision of piped water, however, has not guaranteed access to safe urban water supplies and the burgeoning urban population is putting immense strain on municipal water suppliers. A 2006 survey56 of several thousand suppliers revealed that more than a quarter of municipal drinking water plants and more than half of private plants were not complying with monitoring requirements for water quality. Urbanisation is proceeding rapidly even though nearly half of China's major cities do not comply with health-based standards for drinking water.57
Water scarcity is a big challenge for China's urbanisation trajectory. Urban domestic water use per head has risen only slightly, despite the substantial rise in urban incomes, and the total urban water supply has remained somewhat constant.58 This consistency has largely been maintained by policies designed to reduce industrial urban water demand (eg, by moving industrial enterprises out of cities).58 Future growth, especially in areas where water is scarce, might push municipal suppliers to contaminated sources with worrying consequences for public health.59 Meanwhile, urban areas encroaching on rural communities will put pressure on nearby rural water supplies, which are less developed. To secure safe, reliable water supplies in line with future urban growth is one of the most pressing challenges for China's planners. In a country with one of the lowest per-head water supplies (less than 2156 m3 per head per year59), further investments in source protection, efficiency, and conservation are urgently needed.
China's air quality standards have been especially difficult to meet because of rapid urbanisation. Outdoor air pollution is associated with more than 400 000 premature deaths per year in China.60 Rapid increases in motor vehicle use—the number of vehicles in Beijing, for instance, grows by more than 1000 per day—and increased household energy consumption (mainly produced from coal) contribute to air pollution that far exceeds health standards in many cities.61 Vehicle emissions—including ozone and respirable particles—are major contributors to photochemical smog and spread from highly urbanised to nearby rural areas.59 Thus, the effect of urbanisation on outdoor air quality is seen well outside of China's large cities.
The burning of coal indoors in urban areas remains common despite attempts to reduce household use.59 This reliance on coal is partly because electricity and liquefied petroleum gas supplies can be erratic in rapidly urbanising areas with strained energy systems. By decreasing the number of households relying on coal and other solid fuels, indoor air pollution in China's rapidly growing cities could be greatly reduced.62 Clean household fuels and stringent vehicle emission standards would be important steps forward,63 especially since lung cancer incidence is higher in urban areas than in rural settings, despite higher rates of smoking in rural populations, a trend that could be explained partly by exposures to air pollutants.64, 65
Injury-related deaths (800 000 annually) are recognised as a substantial public health challenge in China.66 Over the past three decades, changes in transport modes, housing, and lifestyles have contributed to new patterns of accidents and injuries, and rapid urbanisation has had a key role in driving these trends, particularly traffic-related and occupational accidents and injuries.67 In urban areas, increasingly crowded roadways are shared by a mix of pedestrians and motorised and non-motorised vehicles that compete for road space. In the absence of separate rights of way, pedestrians and cyclists are put at heightened risk of accidents and injuries, especially at intersections.68 Slowing of traffic because of rising congestion in urban areas could have played a part in stabilisation or even reduction of traffic death rates,67 but traffic-related accidents and injuries remain the country's leading cause of injury-related deaths.66 Cyclists and pedestrians are especially at risk, and make up 60% of traffic-related deaths.66, 68 Such non-motorised transport is still used for as many as 40–55% of total trips taken in Beijing and Shanghai and a much higher proportion of journeys than that in smaller cities.68 Urban poor people—especially migrants—are most reliant on these non-motorised transport modes.68
Occupational accidents and injuries are a big concern, especially for migrants who have dangerous work environments, such as those in construction or heavy industry.69 In 2004, nearly all the 39 million construction workers in China were migrants.69 Migrant workers work nearly 50% longer hours, are less educated, and have less experience than non-migrant urban workers—all of which lead to increased risks of injuries.70 Although reliable data for occupational accident rates are unavailable, reports of work-related injuries (eg, pneumoconiosis, poisoning, and noise deafness) in migrant workers are common.71 A 2004 survey by the Ministry of Health recorded that 83% of township-based and village-based enterprises had unsafe working conditions and 16% of surveyed workers had occupational disease.72 An important corollary is that the children left behind when migrants move could also be at greater risk of accidents and injuries, partly because households with only one parent can have reduced capacity to supervise young children who are accident prone;73 more than 20 million such so-called left-behind children are estimated to exist in China.74
Ageing and urbanisation in China
Although China's population is following the worldwide trend (ie, ageing due to reduced fertility rates and increasing life expectancies), the country is unique in that government policy, namely the one-child policy, has had a key role (figure 2 ). Fertility rates have declined by nearly 70%, from 5·6 children per woman in 1950, to 1·8 children per woman in 2000.76 In 2005, life expectancy reached 73 years and the median age reached 32·6 years compared with 23·9 in 1950.76 These trends will have a pronounced effect on China's population, and will interact in important ways with urbanisation.
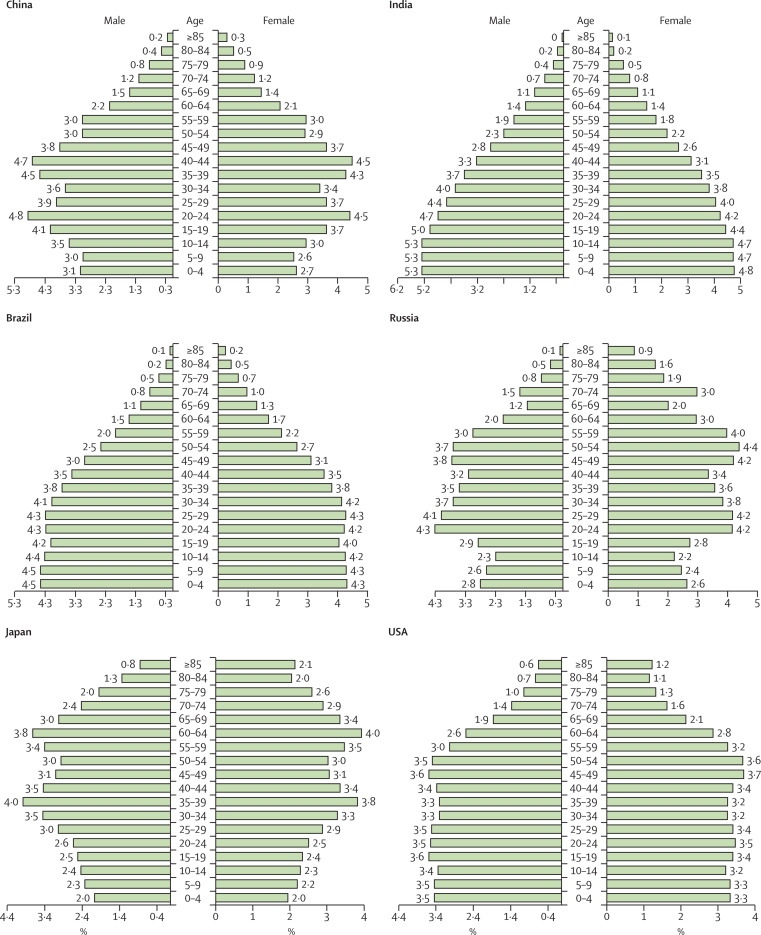
Figure 2.
Age distribution profiles of six countries in 2010
Data from US Census Bureau.75 Figures have been rounded up or rounded down as appropriate.
By 2050, China's median age is projected to be 49·8 years, higher than the projected median ages of the global population (37·8), India (38·6), USA (44·1), Brazil (45), and the European Union (47), and slightly less than that of Japan (52·5).76, 77 The proportion of the population 65 years of age and older in China reached 7·6% in 2005, and is projected to grow to 13·7% in 2025, and to 25% by 2050.76, 78 Partly because of urbanisation, trends of population ageing in China's urban and rural areas differ substantially. Urbanisation delays childbearing of urban migrants, and urbanites are likely to adhere more strictly to the one-child policy than rural dwellers.79 Thus, urban populations usually have low fertility rates,79 which, combined with longer life expectancy in urban areas, tend to yield rapidly ageing urban populations. However, both the push and pull factors driving urbanisation (panel) attract millions of young rural migrants into urban areas (more than 85% of migrants are younger than 40 years9), which greatly reduces the proportion of older urbanites. Because of the migration of young people to urban centres, people in rural areas are ageing rapidly. One study examining this effect showed that, in the absence of rural-to-urban migration, the proportion of the population older than 65 years would reach 25% in urban areas and 16% in rural areas by 2050. With migration included, the population older than 65 years would reach 21% in urban areas and 23% in rural areas in 2050, a substantially younger urban and older rural population, respectively.79
The rapid pace of ageing poses serious challenges for China, both now and in the future. In urban areas, data from 2000 show that 71% of the urban population older than 60 years reported pension benefits, and 12% had relied on social security.80 By contrast, in rural areas only 5% reported pension benefits, and 1·5% depended on social security, with most (about 85%) of the elderly population dependent on family support.80 The one-child policy has greatly reduced the number of children available to support ageing parents, and urbanisation has increased the geographical separation between adult children and their parents, restricting familial social support.76, 81 However, adult children who migrate and find work could provide increased economic support to their parents.82 The interaction between urbanisation and population ageing must be considered as China takes measures to reform its social security system. In particular, urgent attention is needed to strengthen rural social security—such as health-care and pension systems—and to develop innovative ways to increase support networks for rural elders in the absence of familial ties.
Research and policy needs
Untangling the causal web linking urbanisation and health needs a multidisciplinary approach, and metrics that capture the multidimensional process of rural-to-urban transformation show promise in the assessment of longitudinal changes in urbanicity and the subsequent health effects.6, 8, 83 These metrics have not been widely adopted or standardised, but as urbanisation continues, the social and environmental differences between rural and urban areas will also change. A framework that recognises an urban–rural overlap rather than an urban–rural dichotomy could help to identify key aspects of urbanisation that are protective of or detrimental to health. Furthermore, to account for the effects of urbanisation in rural areas is important. The pull of young adults to urban areas has profound effects on rural social structure, and increased connections between formerly isolated rural villages and cities can speed up the spread of infectious disease. Urban air and water pollution can extend to rural areas through environmental transport, whereas rural environmental pollution can reach urban areas—eg, when fresh produce contaminated by unsafe pesticides reaches urban markets. These pathways are complex and defy simple solutions, but need to be rigorously investigated to understand and respond to the health effects of urbanisation in China.
Importantly, air pollution, water quality, accidents, and other risks vary within cities, and disaggregated statistics that capture the differential exposures and health outcomes of populations within different urban areas are needed to assess efforts to mitigate risks and target interventions towards the populations bearing the greatest disease risks.84 Generation of these data will require extensive monitoring of urban environmental health risks, workplace injuries, and other factors. These monitoring activities should extend to periurban, suburban, and rural areas to assess the reach of typically urban environmental pollutants in rural areas. Systematic urban-mapping programmes, done with standardised protocols, would build capacity for effective research, urban planning, and policy making. In a country changing as rapidly as China, frequently updated urbanisation data are crucial to the country's future.
Policies to mitigate the adverse health effects of urbanisation need to meet the health-care needs of highly vulnerable populations, and must follow up these populations as they potentially transfer health-care burdens to rural areas—eg, when migrants return to their rural homes after sustaining disabling injuries or long-term illnesses. The provision of affordable health care to rural-to-urban migrants in urban areas irrespective of hukou status is urgently needed, and health-care providers must be aware of the dual urban–rural disease risks faced by these populations. Electronic medical record keeping, already common in many community hospitals in urban settings,85 could improve health-care continuity. The mobility of migrants has relevance for infectious diseases, which can potentially be transported long distances. Because migrants' use of health care is increasing, a key opportunity exists to reduce long-distance transmission by raising vaccination coverage and improving infectious-disease surveillance. Hospitals undertake real-time surveillance of reportable illnesses through China's internet-based Infectious Disease Reporting Information System—a powerful and robust system, provided that individuals with disease have sufficient access to health care.
The next decade of urbanisation in China will demand innovative health policies that address the needs of new urban residents while providing health services for people (especially older people and the very young) who remain in rural areas. Although China's rapid economic growth in the past two decades has brought many benefits, raised incomes, and pulled hundreds of millions out of poverty, the adverse health consequences of urbanisation pose major policy challenges and threaten to put additional pressure on the country's overstrained health services. Minimisation of these adverse effects, and indeed maximisation of the benefits, will require development of key infrastructure, improved awareness among policy makers of the health risks associated with urbanisation, and innovative policies on the part of urban planners and regulators to ensure safe and healthy urban life in China.
Search strategy and selection criteria
We searched China National Knowledge Infrastructure and Wanfang for Chinese language papers and PubMed for English language papers, using the medical subject heading terms “urbanization”, “migrant”, and “migration”, and the search terms “health”, “healthcare”, “hukou”, “infectious disease”, “chronic disease”, “mental health”, “nutrition”, “diabetes mellitus”, “obesity”, “cardiovascular diseases”, “injury”, and “vaccination”. We also searched for geographical terms such as “China” and province and municipality names. Searches included appropriate wild cards and truncation and we reviewed the references cited in relevant papers. We selected publications from the past 20 years and manually reviewed Chinese health, demography, and construction statistical yearbooks published over the past 20 years, and government reports published over the past 15 years.
Acknowledgments
Acknowledgments
We thank the China Medical Board for facilitating the manuscript. JVR is supported by the National Institute for Allergy and Infectious Disease (grant K01AI091864), by the National Institutes of Health/National Science Foundation Ecology of Infectious Disease Programme (grant 0622743), and by the Emory Global Health Institute Faculty Distinction Fund. PG is supported by the National High Technology Programme of China (grant 2009AA12200101). SL is supported partly by a National Institutes of Health/National Institute of Allergy and Infectious Diseases grant (R01AI068854) to the University of California, Berkeley, and by Public Health Preparedness for Infectious Diseases at the Ohio State University. EJC is supported by an American Recovery and Reinvestment Act supplement (grant R01AI068854-04S1) and by the National Institute for Allergy and Infectious Diseases (grant R01AI068854). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the paper. No payment was received by any of the co-authors for the preparation of this report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Contributors
JVR conceived and led the preparation of the report. All authors participated in data analysis, discussion, and writing of the report.
Conflicts of interest
We declare that we have no conflicts of interest.
Supplementary Material
References
- 1.NBSC . National statistics yearbook. National Bureau of Statistics of China; Beijing: 2010. [in Chinese]. [Google Scholar]
- 2.UN Department of Economic and Social Affairs, Population Division World population prospects. The 2010 Revision. http://esa.un.org/unpd/wpp/index.htm (accessed Oct 13, 2011).
- 3.Yusuf F, Saich T. China urbanizes: consequences, strategies and policies. The World Bank; Washington, DC: 2008. [Google Scholar]
- 4.National Bureau of Statistics of China China's total population and structural changes in 2011. http://www.stats.gov.cn/english/newsandcomingevents/t20120120_402780233.htm (accessed Jan 18, 2012).
- 5.Zhou YX, Ma LJC. China's urbanization levels: Reconstructing a baseline from the fifth population census. China Q. 2003;173:176–196. [Google Scholar]
- 6.Allender S, Foster C, Hutchinson L, Arambepola C. Quantification of urbanization in relation to chronic diseases in developing countries: a systematic review. J Urban Health. 2008;85:938–951. doi: 10.1007/s11524-008-9325-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dahly DL, Adair LS. Quantifying the urban environment: a scale measure of urbanicity outperforms the urban-rural dichotomy. Soc Sci Med. 2007;64:1407–1419. doi: 10.1016/j.socscimed.2006.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van de Poel E, O'Donnell O, Van Doorslaer E. Urbanization and the spread of diseases of affluence in China. Econ Hum Biol. 2009;7:200–216. doi: 10.1016/j.ehb.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Yeh A, Xu J, Liu K. China's post-reform urbanization: retrospect, policies and trends. United Nations Population Fund (UNFPA) and the International Institute for Environment and Development (IIED); New York: 2011. [Google Scholar]
- 10.Lee ES. A theory of migration. Demography. 1966;3:47–57. [Google Scholar]
- 11.Li B, Piachaud D. Urbanization and social policy in China. Asia-Pacific Dev J. 2006;13:1–26. [Google Scholar]
- 12.Wang L, Li C, Wang X, et al. China 1990–2010 satellite remote sensing mapping of urban expansion. Chin Sci Bull (in press).
- 13.United Nations Human Settlements Programme (UN Habitat) Cities for all: bridging the urban divide. Earthscan; London: 2010. [Google Scholar]
- 14.UN Human Settlements Programme (UN Habitat) The challenge of slums: global report on human settlements. Earthscan; London: 2003. [Google Scholar]
- 15.Wang YP, Wang YL, Wu JS. Housing migrant workers in rapidly urbanizing regions: a study of the Chinese model in Shenzhen. Housing Stud. 2010;25:83–100. [Google Scholar]
- 16.Liu Y, He S, Wu F, Webster C. Urban villages under China's rapid urbanization: unregulated assets and transitional neighbourhoods. Habitat Int. 2010;34:135–144. [Google Scholar]
- 17.Goldstein A, White M, Goldstein S. Migration, fertility, and state policy in Hubei Province, China. Demography. 1997;34:481–491. [PubMed] [Google Scholar]
- 18.Li MQ, Liu JJ, Ying K. An exploration of surveillance of early warning of intestinal infectious disease in suburban areas. Dis Surveill. 2006;21:57–58. (in Chinese). [Google Scholar]
- 19.Mou J, Cheng J, Zhang D, Jiang H, Lin L, Griffiths SM. Health care utilisation amongst Shenzhen migrant workers: does being insured make a difference? BMC Health Serv Res. 2009;9:214. doi: 10.1186/1472-6963-9-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fu H, He Q, Wang J. Background, evolution and trend of public health policy on Beijing floating population. Chin J Health Policy. 2008;1:47–50. (in Chinese). [Google Scholar]
- 21.Ramesh M, Wu X. Health policy reform in China: lessons from Asia. Soc Sci Med. 2009;68:2256–2262. doi: 10.1016/j.socscimed.2009.03.038. [DOI] [PubMed] [Google Scholar]
- 22.Hu S, Tang S, Liu Y, Zhao Y, Escobar ML, de Ferranti D. Reform of how health care is paid for in China: challenges and opportunities. Lancet. 2008;372:1846–1853. doi: 10.1016/S0140-6736(08)61368-9. [DOI] [PubMed] [Google Scholar]
- 23.General Office of Ministry of Health of China A notice of carrying out health care pilot projects for migrant workers. 2010. http://www.chinadhc.org/shownews.asp?id=299 (in Chinese, accessed June 11, 2011).
- 24.Cui F, Purha T, Hadler S, Liang X. Analysis on newborn hepatitis B immunization coverage and pregnant women hospital delivery rate in different regions. Chin J Vacc Immun. 2007;13:1–3. (in Chinese). [Google Scholar]
- 25.Zeng XJ, Yang G, Liao S. A study on the coverage, strategy and cost of hepatitis B vaccination in China, 1996. Zhonghua Liu Xing Bing Xue Za Zhi. 1998;19:277–281. (in Chinese). [PubMed] [Google Scholar]
- 26.Lin YJ, Lei RY, Luo YX. Analysis of immunization coverage rate and its influencing factor of floating children in Zhujiang Delta River Area of Guangdong Province. Chin J Vacc Immun. 2007;6:87–90. (in Chinese). [Google Scholar]
- 27.Qin XL, Li JL, Qin CW. Immunization of floating children in clustered areas of migrant workers and the influencing factors. J Appl Prev Med. 2007;13:155–156. (in Chinese). [Google Scholar]
- 28.Lin XD, Chen LP, Zheng XC, Li WC, Wang ZG, Deng ZJ. Analyses of factors influencing the coverage of national immunization program in migrant children. Chin J Child Health Care. 2011;19:51–53. (in Chinese). [Google Scholar]
- 29.Han YL, Wang JK, Gong WM. Management strategies on planned immunization of floating population. Occupation and Health. 2006;22:1277–1278. (in Chinese). [Google Scholar]
- 30.Huang YX, Manderson L. The social and economic context and determinants of schistosomiasis japonica. Acta Trop. 2005;96:223–231. doi: 10.1016/j.actatropica.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 31.Jia ZW, Jia XW, Liu YX. Spatial analysis of tuberculosis cases in migrants and permanent residents, Beijing, 2000–2006. Emerg Infect Dis. 2008;14:1413–1419. doi: 10.3201/1409.071543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang W, Wei C, Buchholz ME. Prevalence and risks for sexually transmitted infections among a national sample of migrants versus non-migrants in China. Int J STD AIDS. 2010;21:410–415. doi: 10.1258/ijsa.2009.008518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.He J, Klag MJ, Whelton PK. Migration, blood pressure pattern, and hypertension: the Yi Migrant Study. Am J Epidemiol. 1991;134:1085–1101. doi: 10.1093/oxfordjournals.aje.a116012. [DOI] [PubMed] [Google Scholar]
- 34.Monda KL, Gordon-Larsen P, Stevens J, Popkin BM. China's transition: the effect of rapid urbanization on adult occupational physical activity. Soc Sci Med. 2007;64:858–870. doi: 10.1016/j.socscimed.2006.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bauman A, Allman-Farinelli M, Huxley R, James WP. Leisure-time physical activity alone may not be a sufficient public health approach to prevent obesity–a focus on China. Obes Rev. 2008;9(suppl 1):119–126. doi: 10.1111/j.1467-789X.2007.00452.x. [DOI] [PubMed] [Google Scholar]
- 36.Popkin BM, Du S. Dynamics of the nutrition transition toward the animal foods sector in China and its implications: a worried perspective. J Nutr. 2003;133(suppl 2):3898S–3906S. doi: 10.1093/jn/133.11.3898S. [DOI] [PubMed] [Google Scholar]
- 37.Van de Poel E, O'Donnell O, Van Doorslaer E. Is there a health penalty of China's rapid urbanization? Health Econ. 2011 doi: 10.1002/hec.1717. published online Feb 21, 2011. [DOI] [PubMed] [Google Scholar]
- 38.Wu Y, Huxley R, Li L, the China NNHS Steering Committee, and the China NNHS Working Group Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation. 2008;118:2679–2686. doi: 10.1161/CIRCULATIONAHA.108.788166. [DOI] [PubMed] [Google Scholar]
- 39.Cui Z, Huxley R, Wu Y, Dibley MJ. Temporal trends in overweight and obesity of children and adolescents from nine provinces in China from 1991–2006. Int J Pediatr Obes. 2010;5:365–374. doi: 10.3109/17477166.2010.490262. [DOI] [PubMed] [Google Scholar]
- 40.Haynes R. Cancer mortality and urbanization in China. Int J Epidemiol. 1986;15:268–271. doi: 10.1093/ije/15.2.268. [DOI] [PubMed] [Google Scholar]
- 41.Jin F, Devesa SS, Chow WH. Cancer incidence trends in urban shanghai, 1972–1994: an update. Int J Cancer. 1999;83:435–440. doi: 10.1002/(sici)1097-0215(19991112)83:4<435::aid-ijc1>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 42.Ministry of Health of China . Health statistics yearbook 2008. Ministry of Health of China; Beijing: 2008. [Google Scholar]
- 43.World Cancer Research Fund/American Institute for Cancer Research . Food, nutrition, physical activity, and the prevention of cancer: a global perspective. AICR; Washington DC: 2007. [Google Scholar]
- 44.Gu D, He J, Duan X. Body weight and mortality among men and women in China. JAMA. 2006;295:776–783. doi: 10.1001/jama.295.7.776. [DOI] [PubMed] [Google Scholar]
- 45.Li J, Zhang BN, Fan JH. A nation-wide multicenter 10-year (1999-2008) retrospective clinical epidemiological study of female breast cancer in China. BMC Cancer. 2011;11:364. doi: 10.1186/1471-2407-11-364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sankaranarayanan R, Swaminathan R, Brenner H. Cancer survival in Africa, Asia, and Central America: a population-based study. Lancet Oncol. 2010;11:165–173. doi: 10.1016/S1470-2045(09)70335-3. [DOI] [PubMed] [Google Scholar]
- 47.Mendez MA, Monteiro CA, Popkin BM. Overweight exceeds underweight among women in most developing countries. Am J Clin Nutr. 2005;81:714–721. doi: 10.1093/ajcn/81.3.714. [DOI] [PubMed] [Google Scholar]
- 48.Leon DA. Cities, urbanization and health. Int J Epidemiol. 2008;37:4–8. doi: 10.1093/ije/dym271. [DOI] [PubMed] [Google Scholar]
- 49.Hu FB, Liu Y, Willett WC. Preventing chronic diseases by promoting healthy diet and lifestyle: public policy implications for China. Obes Rev. 2011;12:552–559. doi: 10.1111/j.1467-789X.2011.00863.x. [DOI] [PubMed] [Google Scholar]
- 50.Phillips MR, Zhang J, Shi Q. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001–05: an epidemiological survey. Lancet. 2009;373:2041–2053. doi: 10.1016/S0140-6736(09)60660-7. [DOI] [PubMed] [Google Scholar]
- 51.Krieger J, Higgins DL. Housing and health: time again for public health action. Am J Public Health. 2002;92:758–768. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chen J. Internal migration and health: re-examining the healthy migrant phenomenon in China. Soc Sci Med. 2011;72:1294–1301. doi: 10.1016/j.socscimed.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 53.Wang B, Li X, Stanton B, Fang X. The influence of social stigma and discriminatory experience on psychological distress and quality of life among rural-to-urban migrants in China. Soc Sci Med. 2010;71:84–92. doi: 10.1016/j.socscimed.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 54.Liu Z, Li X, Ge X. Left too early: the effects of age at separation from parents on Chinese rural children's symptoms of anxiety and depression. Am J Public Health. 2009;99:2049–2054. doi: 10.2105/AJPH.2008.150474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ma X, Xiang YT, Li SR. Prevalence and sociodemographic correlates of depression in an elderly population living with family members in Beijing, China. Psychol Med. 2008;38:1723–1730. doi: 10.1017/S0033291708003164. [DOI] [PubMed] [Google Scholar]
- 56.Zhang L. Investigation on drinking water safety in China in 2006. J Environ Health. 2007;24:595–597. (in Chinese). [Google Scholar]
- 57.SEPA . State of the Environment Report. State Environmental Protection Administration; Beijing, China: 2006. [Google Scholar]
- 58.Browder G, Xie S, Kim Y, Gu L, Fan M, Ehrhardt D. Stepping up: improving the performance of China's urban water utilities. World Bank; Washington, DC: 2007. [Google Scholar]
- 59.Zhang J, Mauzerall DL, Zhu T, Liang S, Ezzati M, Remais JV. Environmental health in China: progress towards clean air and safe water. Lancet. 2010;375:1110–1119. doi: 10.1016/S0140-6736(10)60062-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.World Bank . Cost of Pollution in China. World Bank; Washington, DC: 2007. [Google Scholar]
- 61.HEI . Health Effects of Outdoor Air Pollution in Developing Countries of Asia. Health Effects Institute; Boston, MA: 2004. [Google Scholar]
- 62.Zhang J, Smith KR. Household air pollution from coal and biomass fuels in China: measurements, health impacts, and interventions. Environ Health Perspect. 2007;115:848–855. doi: 10.1289/ehp.9479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Remais JV, Zhang J. Environmental lessons from China: finding promising policies in unlikely places. Environ Health Perspect. 2011;119:893–895. doi: 10.1289/ehp.1003024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang YX, Tao S, Shen HZ, Ma JM. Inhalation exposure to ambient polycyclic aromatic hydrocarbons and lung cancer risk of Chinese population. Proc Natl Acad Sci USA. 2009;106:21063–21067. doi: 10.1073/pnas.0905756106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhu YG, Ioannidis JP, Li H, Jones KC, Martin FL. Understanding and harnessing the health effects of rapid urbanization in China. Environ Sci Technol. 2011;45:5099–5104. doi: 10.1021/es2004254. [DOI] [PubMed] [Google Scholar]
- 66.Wang SY, Li YH, Chi GB. Injury-related fatalities in China: an under-recognised public-health problem. Lancet. 2008;372:1765–1773. doi: 10.1016/S0140-6736(08)61367-7. [DOI] [PubMed] [Google Scholar]
- 67.Hu G, Wen M, Baker TD, Baker SP. Road-traffic deaths in China, 1985–2005: threat and opportunity. Inj Prev. 2008;14:149–153. doi: 10.1136/ip.2007.016469. [DOI] [PubMed] [Google Scholar]
- 68.Pucher J, Peng ZR, Mittal N, Zhu Y, Korattyswaroopam N. Urban transport trends and policies in China and India: impacts of rapid economic growth. Transp Rev. 2007;27:379–410. [Google Scholar]
- 69.Chang D, Wang S. Status of occupational hygiene safety and health hazards and its intervention in migrant workers in China. China Occup Med. 2009;36:326–328. (in Chinese). [Google Scholar]
- 70.Du Y, Gregory R, Xin M. The impact of the guest worker system on poverty and wellbeing of migrant workers in urban China. In: Gaunaut RG, Song L, editors. The Turning Point in China's Economic Development. Asia Pacific Press; Canberra: 2006. pp. 172–202. [Google Scholar]
- 71.Ministry of Health of China . Ministry of Health communique: the situation of occupational disease prevention work in 2009. Ministry of Health of China; Beijing: 2010. [Google Scholar]
- 72.Yang QL, Li WD. Current issues on occupational health and control strategies. China Occup Med. 2004;31:58–59. (in Chinese). [Google Scholar]
- 73.Shen M, Yang S, Han J. Non-fatal injury rates among the “left-behind children” of rural China. Inj Prev. 2009;15:244–247. doi: 10.1136/ip.2008.019869. [DOI] [PubMed] [Google Scholar]
- 74.Duan C, Zhou F. Studies on left behind children in China. Popul Res. 2005;25:29–36. (in Chinese). [Google Scholar]
- 75.US Census Bureau . International Data Base. Department of Commerce; Washington, DC: 2011. [Google Scholar]
- 76.Chen F, Liu G. Population aging in China. In: Uhlenberg P, editor. International handbook of population aging. Springer; New York: 2009. pp. 152–172. [Google Scholar]
- 77.United Nations Population Division . World population prospects, the 2010 revision. United Nations Department of Economic and Social Affairs; New York: 2011. [Google Scholar]
- 78.Flaherty JH, Liu ML, Ding L. China: the aging giant. J Am Geriatr Soc. 2007;55:1295–1300. doi: 10.1111/j.1532-5415.2007.01273.x. [DOI] [PubMed] [Google Scholar]
- 79.Zeng Y, Vaupel JW. The impact of urbanization and delayed childbearing on population-growth and aging in China. Popul Dev Rev. 1989;15:425–445. [Google Scholar]
- 80.Wang DW. China's urban and rural old age security system: challenges and options. China World Econ. 2006;14:102–116. [Google Scholar]
- 81.Joseph AE, Phillips DR. Ageing in rural China: impacts of increasing diversity in family and community resources. J Cross Cult Gerontol. 1999;14:153–168. doi: 10.1023/a:1006658706496. [DOI] [PubMed] [Google Scholar]
- 82.Giles J, Wang D, Zhao C. Can China's rural elderly count on support from adult children? Implications of rural-to-urban migration. http://ssrn.com/abstract=1732389 (accessed Oct 13, 2011).
- 83.Jones-Smith JC, Popkin BM. Understanding community context and adult health changes in China: development of an urbanicity scale. Soc Sci Med. 2010;71:1436–1446. doi: 10.1016/j.socscimed.2010.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Moore M, Gould P, Keary BS. Global urbanization and impact on health. Int J Hyg Environ Health. 2003;206:269–278. doi: 10.1078/1438-4639-00223. [DOI] [PubMed] [Google Scholar]
- 85.Li Q, Li G. Status and expectation of individual healthcare record related standards. Chongqing Med. 2008;37:2398–2400. (in Chinese). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.